Published online Nov 19, 2025. doi: 10.5498/wjp.v15.i11.109566
Revised: June 24, 2025
Accepted: September 10, 2025
Published online: November 19, 2025
Processing time: 172 Days and 15.9 Hours
Dysfunctional beliefs about sleep may influence academic performance through their impact on sleep quality. Differences in chronotype can further moderate this relationship, particularly among students with irregular sleep patterns.
To examine the indirect effects of dysfunctional beliefs about sleep on academic performance through sleep quality while considering individual differences in chronotypes among medical students.
The participants were categorized by chronotype and administered the Dysfunctional Beliefs and Attitudes about Sleep Scale and the Pittsburgh Sleep Quality Index and reported their grade point averages (GPAs). Mediation analysis was performed to examine indirect pathways through sleep quality.
Dysfunctional sleep beliefs did not directly affect academic success but indirectly impaired GPA via reduced sleep quality, especially in evening-type students.
Chronotype moderates the relationship between sleep quality and academic performance, highlighting the need for targeted cognitive interventions.
Core Tip: This study investigated how dysfunctional beliefs about sleep indirectly affect academic achievement through sleep quality among medical students. The findings revealed that chronotype moderates this relationship, with evening-type students being particularly vulnerable to the negative effects of maladaptive sleep cognitions. By highlighting its role in mediating sleep quality, this study suggests that cognitive-behavioral interventions tailored to chronotype may improve both sleep and academic outcomes.
- Citation: Altınöz ŞT, Tarlacık LD, Engin E, Uzel Y, Doğan U, Altınöz AE. Unraveling the role of dysfunctional sleep beliefs: How chronotype shapes sleep quality and academic success in medical students. World J Psychiatry 2025; 15(11): 109566
- URL: https://www.wjgnet.com/2220-3206/full/v15/i11/109566.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i11.109566
Sleep is a fundamental biological process essential for cognitive, emotional, and physical functioning. One of the most influential factors regulating sleep-wake patterns is chronotype, which reflects individual variations in circadian rhythms[1-3]. Chronotype affects not only biological processes but also performance, lifestyle, and academic success[4,5].
Chronotypes are typically categorized into morning, evening, and intermediate types[1,6]. Morning-type individuals tend to be more productive during the early hours of the day, whereas evening-type individuals reach peak performance late at night[7]. Intermediate types show a more flexible pattern, balancing between the two[8]. This flexibility may support better adaptation in terms of sleep patterns and academic responsibilities[9].
Most research has emphasized the disadvantages faced by evening types due to the mismatch between their circadian rhythm and institutional demands[10-12]. Morning types are often seen as advantaged because of their alignment with conventional schedules[8,13-15]. However, these studies rarely consider cognitive or psychological factors that may mediate or moderate academic success. Accordingly, it is evident that the determinants of academic performance extend beyond circadian regulation alone, necessitating a more nuanced investigation into the interplay between endogenous biological rhythms and cognitive-academic functioning.
One such factor is dysfunctional sleep beliefs, which are increasingly recognized as cognitive contributors to poor sleep and decreased performance. These beliefs include rigid or unrealistic assumptions about sleep, such as “I must get 8 hours to function”, which can lead to anxiety and reduced sleep quality[16-19]. Studies have shown that dysfunctional beliefs about sleep correlate with lower sleep quality and indirectly correlate with poorer academic outcomes[20,21]. In particular, evening-type individuals appear more susceptible to the negative effects of these beliefs[22].
Understanding the impact of chronotype on individuals’ sleep beliefs could provide a more comprehensive framework for academic success. The findings emphasize that not only physiological regulation but also individuals’ cognitive and psychological states regarding sleep affect academic performance[20,21,23]. Interventions targeting dysfunctional sleep beliefs have been proposed to enhance both sleep quality and academic success and are considered critically important, especially for individuals under intense academic pressure, such as medical students[22,24]. Existing studies have yet to fully address how the effect of dysfunctional sleep beliefs on the relationship between sleep quality and academic success varies across different chronotypes.
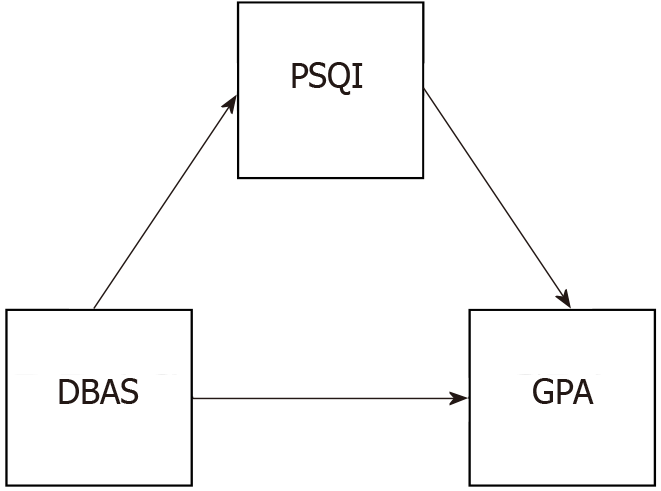
Therefore, this study aims to expand the literature by evaluating the impact of dysfunctional sleep beliefs on academic success through sleep quality across different chronotype groups. In this regard, the present study assessed the indirect effects of chronotype on academic success not only through biological rhythms but also through sleep beliefs and cognitive processes. This approach seeks to develop a more holistic understanding of the relationships between chronotype, sleep beliefs, and academic achievement. To this end, we developed the theoretical framework illustrated in Figure 1.
A total of 482 medical students participated in this study. The mean age of the participants was 22.31 years (SD = 1.94), with an age range of 18 to 26 years. Among the participants, 328 (68.1%) were female, 153 (31.7%) were male, and 1 (0.2%) identified as nonbinary. Regarding psychiatric diagnoses, 95 participants (19.7%) reported having an ongoing psychiatric condition, while 387 (80.2%) indicated that they did not have a psychiatric diagnosis. The average sleep duration of the participants was 7.37 hours (SD = 1.20).
Regarding medication use for sleep, regular use was reported by a small proportion of participants (1.1%), occasional use by some (7.7%), and the majority (91.2%) reported no medication use. In terms of daytime napping habits, 45.1% of participants reported taking daytime naps, while 54.9% stated that they did not nap during the day.
Concerning sleeping arrangements, some participants shared their bed with someone else (13.7%), whereas most did not (86.3%). Similarly, a minority shared their bedroom with others (30.8%), while the majority did not (69.2%).
Daily tea consumption was reported as follows: No tea consumption (13.7%), 1-3 cups per day (62.6%), 3-5 cups per day (13.7%), and more than 5 cups per day (9.9%). For coffee, the distribution was no coffee consumption (19.2%), 1-3 cups daily (72.5%), 3-5 cups daily (6.6%), and more than 5 cups daily (1.6%).
In terms of academic workload affecting sleep patterns, most participants reported that their study hours impacted their sleep schedules (59.3%), while 40.7% stated that they were unaffected. Finally, 31.3% of participants reported that they had experienced sleep problems, whereas 68.7% reported no such problems.
The data were collected using the Personal Information Form and the following scales prepared by the researchers.
Sociodemographic data form: The Sociodemographic data form included information on the participants’ sociodemographic characteristics, such as age, gender, history of mental and physical illness, smoking, alcohol and substance use, and grade point average (GPA). This form was used to evaluate the general health status, medical history, and academic performance of the participants.
Morningness-Eveningness Questionnaire: The Morningness-Eveningness Questionnaire (MEQ), developed by Horne and Östberg[25], was used to determine individuals’ circadian rhythm preferences. The Turkish adaptation was carried out by Pündük et al[26]. This self-assessment tool consists of 19 items and classifies participants as morning-type, evening-type, or intermediate-type. Each item is evaluated on a Likert-type scale, with total scores ranging from 16 to 86. High scores indicate a morning preference, while low scores indicate an evening preference. The internal consistency reliability coefficient for the Turkish version was 0.785 in the first application and 0.812 in the second. The test–retest reliability was 0.84 (P < 0.0001).
Pittsburgh Sleep Quality Index: The Pittsburgh Sleep Quality Index (PSQI), developed by Buysse et al[27], was used to assess sleep quality over the past month. The Turkish adaptation was conducted by Ağargün et al[28]. The PSQI consists of 18 items and evaluates seven components: Subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each component is scored between 0 and 3, with a total score ranging from 0 to 21. Higher total scores indicate poorer sleep quality, and a total score of 5 or above indicates poor sleep quality.
Dysfunctional Beliefs and Attitudes about Sleep-16: The Dysfunctional Beliefs and Attitudes about Sleep-16 (DBAS-16) scale, developed by Morin et al[29], was used to evaluate dysfunctional thoughts and beliefs about sleep. The Turkish adaptation was carried out by Boysan et al[30]. Each of the 16 items is scored on a scale from 1 (strongly disagree) to 10 (strongly agree). Higher scores indicate more dysfunctional beliefs. The internal consistency reliability (Cronbach’s alpha) for the Turkish version was reported as 0.82, with a test–retest reliability of 0.83 over two weeks. The DBAS-16 scale includes the following subscales: Consequences, Worry/Helplessness, Expectations, and Medication.
Prior to data collection, the necessary approvals were obtained from the Eskişehir Osmangazi University Ethics Committee (Date: April 11, 2023; No: 2023/52) and the Dean’s Office of the Faculty of Medicine. The study sample consisted of medical students, and data were collected using online forms hosted on a secure digital platform. Data collection was conducted between April and September 2023. During this period, the participants completed standardized measures assessing their sleep quality, circadian rhythm preferences, and dysfunctional beliefs about sleep.
Data analyses were conducted using the JAMOVI 2.2.5 statistical software[31]. A correlation analysis was performed to determine the relationships between the variables. To examine the pattern of relationships among the variables, a mediation analysis was performed using the GLM Mediation Model add-on[31,32]. Within the scope of these analyses, both direct and indirect effects between the independent and dependent variables were evaluated, and the significance of the mediation effect was tested.
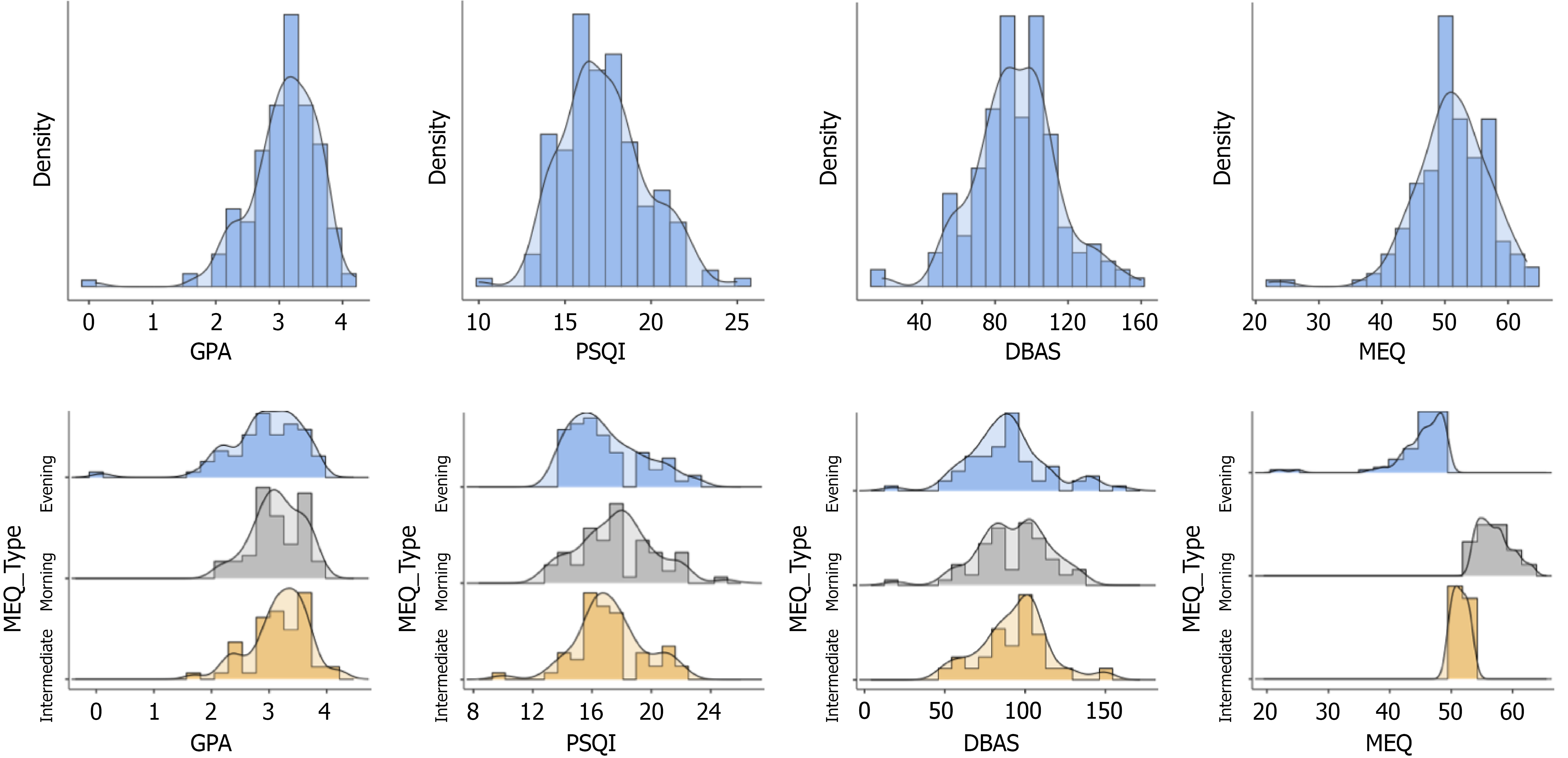
Descriptive statistics for the students’ GPAs and PSQI, Dysfunctional Beliefs and Attitudes about Sleep (DBAS), and MEQ scores were calculated. The data are presented in Table 1. The descriptive statistics are shown separately for morning-type, evening-type, intermediate-type, and all participants.
| MEQ type | Mean | SD | Min | Max | Skewness | Kurtosis | |||
| Skew | SE | Kurt | SE | ||||||
| GPA | Evening-type | 2.93 | 0.64 | 0.10 | 3.80 | -1.49 | 0.30 | 4.75 | 0.59 |
| Morning-type | 3.14 | 0.43 | 2.10 | 3.90 | -0.38 | 0.31 | -0.27 | 0.60 | |
| Intermediate-type | 3.19 | 0.49 | 1.70 | 4.20 | -0.66 | 0.32 | 0.75 | 0.63 | |
| All | 3.08 | 0.54 | 0.10 | 4.20 | -1.26 | 0.18 | 4.33 | 0.36 | |
| PSQI | Evening-type | 16.99 | 2.44 | 14.00 | 23.00 | 0.72 | 0.30 | -0.30 | 0.59 |
| Morning-type | 17.70 | 2.56 | 13.00 | 25.00 | 0.28 | 0.31 | 0.09 | 0.60 | |
| Intermediate-type | 17.21 | 2.32 | 10.00 | 22.00 | -0.11 | 0.32 | 0.88 | 0.63 | |
| All | 17.30 | 2.45 | 10.00 | 25.00 | 0.34 | 0.18 | 0.04 | 0.36 | |
| DBAS | Evening-type | 89.34 | 24.92 | 18.00 | 160.00 | 0.38 | 0.30 | 1.15 | 0.59 |
| Morning-type | 92.64 | 22.45 | 19.00 | 136.00 | -0.49 | 0.31 | 0.79 | 0.60 | |
| Intermediate-type | 93.57 | 21.26 | 49.00 | 150.00 | 0.14 | 0.32 | 0.66 | 0.63 | |
| All | 91.75 | 22.96 | 18.00 | 160.00 | 0.02 | 0.18 | 0.80 | 0.36 | |
| MEQ | Evening-type | 45.12 | 4.80 | 22.00 | 49.00 | -3.02 | 0.30 | 11.73 | 0.59 |
| Morning-type | 57.11 | 2.61 | 54.00 | 63.00 | 0.63 | 0.31 | -0.49 | 0.60 | |
| Intermediate-type | 51.45 | 1.17 | 50.00 | 53.00 | 0.10 | 0.32 | -1.48 | 0.63 | |
| All | 51.09 | 5.99 | 22.00 | 63.00 | -1.03 | 0.18 | 3.81 | 0.36 | |
Table 1 shows that the means and standard deviations and the minimum and maximum values of the studied variables differ across groups. When we examined the GPA, the mean values for evening-type, morning-type, and intermediate-type students were similarl however, evening-type students (1.49) exhibited a higher negative skewness compared to the other groups. The overall GPA for all participants was calculated as 3.08, with a skewness of 1.26, indicating a left-skewed distribution. The mean PSQI scores were similar between morning-type students (17.70), evening-type students (16.99), and intermediate-type students (17.21). The overall PSQI average for all participants was 17.30, showing a slight right-skewed distribution with a skewness of 0.34. When examining the means for the DBAS scale scores, the average for evening-type students was 89.34, 92.64 for morning-type students, and 93.57 for intermediate-type students. The overall average for all participants was 91.75, with a skewness of 0.02, indicating a symmetric distribution. Regarding the MEQ scores, there was a noticeable difference between the mean for evening-type students (45.12) and morning-type students (57.11). The mean for intermediate-type students was 51.45. The overall average for all participants was calculated as 51.09, showing a left-skewed distribution (skewness = 1.03). Overall, when evaluating the data, the skewness and kurtosis values in some variables indicated deviations from symmetry.
As shown in Figure 2, the GPA histogram was slightly left-skewed for evening-type participants, while it showed a more symmetric distribution for morning-type and intermediate-type participants. The overall GPA distribution for all participants exhibited a slight left skew, indicating that a larger number of participants achieved higher academic success scores. The PSQI histogram showed a relatively normal distribution with a slight right skew for evening-type participants, whereas morning-type and intermediate-type participants displayed more symmetric distributions. The combined distribution for all participants appeared close to normal. In the DBAS histogram, evening-type participants were more dispersedly distributed with some skewness, while morning-type and intermediate-type participants exhibited more clustered distributions. The overall distribution of the total scores on the DBAS scale for all participants appeared slightly right-skewed, indicating a concentration of participants with moderately dysfunctional beliefs about sleep. The MEQ total score histogram revealed a left-skewed distribution for evening-type participants, while morning-type participants showed a distribution concentrated around higher MEQ scores, reflecting their morning chronotype. The distribution of the MEQ scores of intermediate-type participants was concentrated in the middle range. The overall distribution of total MEQ score showed moderate left skewness, consistent with the variability in circadian rhythm preferences.
Correlation analyses were conducted to determine the relationship between students’ GPAs and PSQI, DBAS, and MEQ scores. The analysis was computed in four different ways according to sleep chronotype: Evening-type, morning-type, intermediate-type, and the entire group. The data are presented in Table 2.
Upon analysis, we identified a significant negative correlation between GPA and PSQI in the evening-type group (r = 0.30, P < 0.05) and among all participants (r = 0.18, P < 0.05). This relationship was not significant in the morning-type and intermediate groups. A significant positive correlation between PSQI and DBAS was found in the evening-type group (r = 0.33, P < 0.01), the morning-type group (r = 0.47, P < 0.001), and the intermediate group (r = 0.33, P < 0.05). For all participants, this relationship was stronger (r = 0.38, P < 0.001) than in any of the chronotype subgroups. There was a significant negative correlation between DBAS and MEQ in the evening-type group (r = 0.27, P < 0.05). This relationship was not significant in the other groups. The results indicate meaningful relationships between sleep quality, dysfunctional sleep beliefs, and chronotypes.
To determine the relationship patterns among the students’ GPA, PSQI, and DBAS, we performed a mediation analysis. The analysis was computed in four different ways according to sleep chronotype: Evening-type, morning-type, intermediate-type, and the entire group. The calculated results are presented in Table 3.
| Type | Effect | Est | SE | 95%CI | β | Z | P value | ||
| Lower | Upper | ||||||||
| E | Indirect | DBAS ⇒ PSQI ⇒ GPA | -0.00 | 0.00 | -0.01 | 0.00 | -0.10 | -1.88 | 0.06 |
| Component | DBAS ⇒ PSQI | 0.03 | 0.01 | 0.01 | 0.05 | 0.33 | 2.80 | 0.01 | |
| PSQI ⇒ GPA | -0.08 | 0.03 | -0.15 | -0.02 | -0.32 | -2.54 | 0.01 | ||
| Direct | DBAS ⇒ GPA | 0.00 | 0.00 | -0.00 | 0.01 | 0.06 | 0.48 | 0.63 | |
| Total | DBAS ⇒ GPA | -0.00 | 0.00 | -0.01 | 0.01 | -0.04 | -0.35 | 0.72 | |
| M | Indirect | DBAS ⇒ PSQI ⇒ GPA | -0.00 | 0.00 | -0.00 | 0.00 | -0.04 | -0.57 | 0.57 |
| Component | DBAS ⇒ PSQI | 0.05 | 0.01 | 0.03 | 0.08 | 0.47 | 4.19 | < 0.001 | |
| PSQI ⇒ GPA | -0.01 | 0.02 | -0.06 | 0.03 | -0.08 | -0.57 | 0.57 | ||
| Direct | DBAS ⇒ GPA | -0.00 | 0.00 | -0.01 | 0.00 | -0.09 | -0.64 | 0.52 | |
| Total | DBAS ⇒ GPA | -0.00 | 0.00 | -0.01 | 0.00 | -0.13 | -1.03 | 0.31 | |
| I | Indirect | DBAS ⇒ PSQI ⇒ GPA | -0.00 | 0.00 | -0.00 | 0.00 | -0.06 | -1.10 | 0.27 |
| Component | DBAS ⇒ PSQI | 0.04 | 0.01 | 0.01 | 0.06 | 0.33 | 2.59 | 0.01 | |
| PSQI ⇒ GPA | -0.04 | 0.03 | -0.09 | 0.02 | -0.17 | -1.21 | 0.23 | ||
| Direct | DBAS ⇒ GPA | 0.00 | 0.00 | -0.00 | 0.01 | 0.07 | 0.50 | 0.61 | |
| Total | DBAS ⇒ GPA | 0.00 | 0.00 | -0.01 | 0.01 | 0.02 | 0.11 | 0.91 | |
| All | Indirect | DBAS ⇒ PSQI ⇒ GPA | -0.00 | 0.00 | -0.00 | -0.00 | -0.07 | -2.27 | 0.02 |
| Component | DBAS ⇒ PSQI | 0.04 | 0.01 | 0.03 | 0.05 | 0.38 | 5.52 | < 0.001 | |
| PSQI ⇒ GPA | -0.04 | 0.02 | -0.08 | -0.01 | -0.20 | -2.49 | 0.01 | ||
| Direct | DBAS ⇒ GPA | 0.00 | 0.00 | -0.00 | 0.00 | 0.04 | 0.52 | 0.60 | |
| Total | DBAS ⇒ GPA | -0.00 | 0.00 | -0.00 | 0.00 | -0.03 | -0.45 | 0.66 | |
The indirect effect of DBAS on GPA was not significant in the evening-type group (β = 0.001, 95%CI: 0.01-0.00, P = 0.06). However, we identified a significant effect of DBAS on PSQI (β = 0.03, 95%CI: 0.0-0.05, P = 0.01). Additionally, PSQI had a negative and significant effect on GPA (β = 0.08, 95%CI: 0.15-0.02, P = 0.01). The effect of DBAS on PSQI was significant in the morning-type group (β = 0.05, 95%CI: 0.03-0.08, P < 0.001). However, the indirect effect was not significant (β = 0.00, 95%CI: 0.00-0.00, P = 0.57). In the intermediate-type group, the effect of DBAS on PSQI was significant (β = 0.04, 95%CI: 0.01-0.06, P = 0.01), though the indirect effect was not significant (β = 0.00, 95%CI: 0.00-0.00, P = 0.27). In the analysis conducted for all participants, the indirect effect was significant (β = 0.00, 95%CI: 0.00-0.00, P = 0.02). The effect of DBAS on PSQI (β = 0.04, 95%CI: 0.03-0.05, P < 0.001) and the effect of PSQI on GPA was strong and significant (β = 0.04, 95%CI: 0.08-0.01, P = 0.01).
This study demonstrated that the impact of dysfunctional sleep-related beliefs on academic achievement is not direct but mediated through sleep quality. This finding indicates that academic performance should be understood through the lens of sleep quality rather than attributing a direct influence[16,33,34]. While the indirect pathway was significant in the overall sample, the results were statistically significant only for the evening-type student subgroup. This mediation model was not supported in either the morning-type or intermediate-type groups. These results suggest that chronotype alone may not act as an independent risk factor; rather, it appears to interact with cognitive sleep schemas, influencing academic performance via sleep quality.
Dysfunctional sleep-related beliefs can negatively affect sleep quality and mental health among university students[34]. Such beliefs have been reported to be more prevalent among healthcare professionals and are associated with poor sleep quality, as well as symptoms of depression and anxiety[35]. In our sample, 59.3% of participants reported that their academic workload disrupted their sleep schedules. This finding suggests that chronic academic stress among medical students may impair sleep quality and, consequently, lower GPA, particularly in individuals with dysfunctional sleep beliefs[36].
In addition, 68% of the participants were female. This female-dominant sample may have increased the prominence of cognitive distortions related to sleep and poor sleep quality. Previous studies have shown that women tend to report more dysfunctional sleep beliefs and poorer sleep quality[20]. Furthermore, increased caffeine consumption has been linked to poorer sleep quality[37]. A total of 72.5% of the students reported consuming 1-3 cups of coffee per day. Although coffee may enhance alertness in the short term, it delays sleep onset in the evening, thereby reinforcing the influence of maladaptive sleep-related beliefs. A psychiatric diagnosis rate of 19.7% in the sample may have further amplified the prevalence of cognitive distortions, contributing to reduced sleep quality and increasing the indirect association[34]. The literature also reports that dysfunctional sleep-related beliefs interact bidirectionally with stress and psychological symptoms, thereby further compromising sleep quality[19,38].
Evening-type students: Evening-type students reported the highest levels of dysfunctional sleep-related beliefs, which were associated with lower sleep quality and a marginal decline in GPA[8,34]. These students often face greater conflict with early academic schedules that misalign with their circadian rhythms, potentially fostering distorted cognitions about sleep[39]. Even when total sleep duration is sufficient, the belief that “sleep can be delayed” may degrade sleep quality[40]. Limited flexibility in scheduling during exam periods may further amplify this indirect effect[41].
This repeated misalignment between evening-types’ biological clocks and institutional routines may play a central role in the development of maladaptive sleep beliefs and their consequences[39].
Morning-type students: Although dysfunctional sleep beliefs were associated with poorer sleep quality in morning-type individuals, this deterioration did not translate into reduced academic performance. The strong alignment between chronotype and class schedules appears to buffer the indirect pathway[13,41,42]. In addition, frequent daytime napping and effective time management strategies, commonly employed by the morning-type group, may compensate for declines in sleep quality, thereby preserving GPA.
Intermediate-type students: Individuals with an intermediate chronotype exhibited a similar pattern to the morning-type group in the relationship between dysfunctional sleep beliefs and sleep quality; however, this did not have a significant effect on GPA. This finding suggests that a more flexible circadian structure may buffer the academic consequences of mild disruptions in sleep quality[43]. Additionally, the presence of more balanced social support networks and enhanced emotional regulation skills observed in this group may further attenuate the direct link between sleep quality and academic performance. Moreover, the relatively high rate of room sharing (30.8%) may promote collective sleep hygiene behaviors, positively influencing sleep-related environmental factors[44,45].
While the findings of this study make significant contributions to understanding the relationships between sleep beliefs, sleep quality, and academic achievement, they are subject to several limitations. First, the composition of the sample, which consisted solely of medical students, limits the generalizability of the results. Due to their intense academic schedules and stress levels, medical students may experience unique effects on their sleep habits and academic performance. This could lead to different outcomes for students in other disciplines or in the broader university population.
Second, the sample size may have constrained the power of the analyses conducted, particularly for subgroups (morning-type, evening-type, and intermediate-type). Larger and more diverse samples would allow for a more precise evaluation of the effects that were marginally significant in this study. For instance, the marginal significance of the indirect effect observed in the evening-type group might be attributed to an insufficient sample size, potentially resulting from random errors.
Third, all participants in this study reported perceiving their sleep quality as poor. This could introduce selection bias into the results and complicate the broader evaluation of the relationship between sleep quality and academic success. The exclusion of participants who perceived their sleep quality as good likely led to findings that are specific only to students with low sleep quality. Future studies should aim to include a wider range of sleep quality perceptions to address this limitation.
Fourth, the cross-sectional design of this study precludes the determination of causal relationships between variables. Longitudinal studies examining how the relationships between sleep beliefs, sleep quality, and academic achievement evolve over time would provide more definitive insights into causality. Such research designs would help clarify whether changes in sleep beliefs precede changes in sleep quality and academic outcomes, or vice versa.
Fifth, an important limitation arises from the method used to classify the participants’ chronotypes. The original MEQ cut-off scores proposed by Horne and Östberg[7] did not yield meaningful group distinctions within our sample, as most participants clustered into a single chronotype category (intermediate-type). Therefore, to enable group comparisons, we applied an alternative classification scheme based on the distribution ranges suggested by our statistical analysis software. Although similar approaches have been used in prior research, this deviation from the original scale may introduce a methodological bias in chronotype categorization. As a result, the sensitivity of comparisons across chronotypes may be limited, and caution is advised when interpreting these findings.
Sixth, another methodological concern relates to the self-reported nature of the chronotype assessment. While convenient, this method is inherently subjective and prone to bias. Future studies could incorporate biological markers or technological tools that track sleep patterns to more accurately determine chronotypes. Objective assessments of this kind would enable a more reliable classification of individuals’ true chronotype characteristics.
Seventh, this study did not account for several key circadian rhythm-related variables that may influence the relationships between sleep beliefs, sleep quality, and academic performance. One important factor, habitual light exposure, whether beneficial daytime light or potentially disruptive nocturnal light, was not assessed despite its known impact on circadian regulation and sleep-wake cycles. Similarly, the timing of caffeine intake, which can significantly affect sleep latency and quality independent of total consumption, was not measured. Napping behavior, which may compensate for poor nocturnal sleep and influence overall perceptions of sleep quality, was also not evaluated. Furthermore, although the presence of psychiatric diagnoses was assessed, it was not analyzed in detail. Conditions such as anxiety and depression are frequently associated with sleep disturbances and may significantly influence both sleep beliefs and academic performance. Consequently, future research should incorporate these biological, environmental, and psychological variables more comprehensively to provide a holistic understanding of sleep-related outcomes in student populations.
The findings of this study highlight the indirect effects of sleep beliefs and sleep quality on academic achievement, pointing to significant implications at both the individual and institutional levels. Particularly among medical students, the observed relationships across different chronotypes (morning-type, evening-type, and intermediate-type) demonstrate how these groups are differently affected, offering guidance for future interventions.
Understanding the impact of sleep quality on academic performance can help students develop healthier sleep habits. Given that dysfunctional sleep beliefs disrupt sleep quality and consequently lower academic success, especially among evening-type students, personalized sleep interventions are crucial for this group. Therapeutic approaches targeting sleep cognitions, such as cognitive behavioral therapy, could enhance sleep quality and indirectly improve academic outcomes. Furthermore, such interventions may contribute to preventing burnout and sleep disorders in medical students, who face intense academic schedules.
Educational institutions and academic advisors can consider students’ chronotypes and sleep habits when designing more flexible educational programs. For instance, adjusting class schedules to accommodate evening-type students or reducing early-morning course loads could support their academic performance. Additionally, incorporating sleep awareness seminars and sleep hygiene programs into the curriculum would represent a proactive approach to improving sleep quality. By raising awareness and developing supportive strategies, educators have the potential to significantly enhance students’ academic success.
In conclusion, this study demonstrates that sleep beliefs influence academic performance through their impact on sleep quality and highlights that different chronotypes have varying needs in this process. Adapting educational systems, healthcare services, and policies considering these findings could provide innovative solutions to improve student outcomes. Developing personalized interventions and flexible schedules for evening-type students may pave the way for raising healthier and more successful individuals in the future.
This study demonstrated that the impact of dysfunctional sleep-related beliefs on academic achievement among medical students occurs indirectly, mediated by sleep quality. These results empirically validated the triadic interaction between chronotype, sleep beliefs, and academic performance, supporting the cognitive-circadian models described in the literature. While the indirect pathway was disrupted in morning and intermediate chronotypes, its marginal significance in the evening-type group suggests that misalignment between biological rhythms and academic schedules may amplify the influence of maladaptive cognitive schemas.
With a large sample (n = 482), the study offers novel evidence on how demographic factors, such as a predominantly female sample (68%), high caffeine consumption, and a 19.7% prevalence of psychiatric diagnoses, may shape the sleep-academic performance relationship. The use of a cross-sectional design and a percentile-based chronotype classification provided a pragmatic approach to overcoming the challenge of comparison within methodologically homogeneous subgroups.
The primary contribution of this research lies in identifying dysfunctional sleep cognitions, particularly among evening-type students, as a critical mechanism that compromises sleep quality and lowers GPA. This finding suggests that interventions should move beyond generic recommendations, such as “get more sleep,” and instead prioritize chronotype-sensitive cognitive-behavioral strategies. Educational policy can enhance academic outcomes by integrating psychoeducational modules that target sleep beliefs alongside offering flexibility in class scheduling.
What students believe about how sleep shapes how they sleep and how they sleep determines how well they perform. Future research should employ longitudinal designs to further examine this cognitive-circadian mechanism and place sleep-related beliefs at the center of both clinical and academic interventions.
| 1. | Adan A, Archer SN, Hidalgo MP, Di Milia L, Natale V, Randler C. Circadian typology: a comprehensive review. Chronobiol Int. 2012;29:1153-1175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 714] [Cited by in RCA: 932] [Article Influence: 66.6] [Reference Citation Analysis (0)] |
| 2. | Roenneberg T. What is chronotype? Sleep Biol Rhythms. 2012;10:75-76. [RCA] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Montaruli A, Castelli L, Mulè A, Scurati R, Esposito F, Galasso L, Roveda E. Biological Rhythm and Chronotype: New Perspectives in Health. Biomolecules. 2021;11:487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 203] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 4. | Fabbian F, Zucchi B, De Giorgi A, Tiseo R, Boari B, Salmi R, Cappadona R, Gianesini G, Bassi E, Signani F, Raparelli V, Basili S, Manfredini R. Chronotype, gender and general health. Chronobiol Int. 2016;33:863-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 195] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 5. | Monk TH, Buysse DJ, Potts JM, DeGrazia JM, Kupfer DJ. Morningness-eveningness and lifestyle regularity. Chronobiol Int. 2004;21:435-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 108] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Partonen T. Chronotype and Health Outcomes. Curr Sleep Medicine Rep. 2015;1:205-211. [RCA] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 7. | Horne JA, Ostberg O. Individual differences in human circadian rhythms. Biol Psychol. 1977;5:179-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 189] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Preckel F, Lipnevich AA, Boehme K, Brandner L, Georgi K, Könen T, Mursin K, Roberts RD. Morningness-eveningness and educational outcomes: the lark has an advantage over the owl at high school. Br J Educ Psychol. 2013;83:114-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Vitale JA, Bonato M, Galasso L, La Torre A, Merati G, Montaruli A, Roveda E, Carandente F. Sleep quality and high intensity interval training at two different times of day: A crossover study on the influence of the chronotype in male collegiate soccer players. Chronobiol Int. 2017;34:260-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 10. | Foster RG, Peirson SN, Wulff K, Winnebeck E, Vetter C, Roenneberg T. Sleep and circadian rhythm disruption in social jetlag and mental illness. Prog Mol Biol Transl Sci. 2013;119:325-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 152] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 11. | Haraszti RÁ, Ella K, Gyöngyösi N, Roenneberg T, Káldi K. Social jetlag negatively correlates with academic performance in undergraduates. Chronobiol Int. 2014;31:603-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 146] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 12. | Sato T, Kawakatsu Y, Takahata M, Muraoka S, Kudo D, Satake S, Eakman A. 0093 Chronotypic characteristics of sleep, mental health, and daily life of Japanese university of health sciences students. Sleep. 2023;46:A42-A42. [DOI] [Full Text] |
| 13. | Preckel F, Lipnevich AA, Schneider S, Roberts RD. Chronotype, cognitive abilities, and academic achievement: A meta-analytic investigation. Learn Individ Dif. 2011;21:483-492. [RCA] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 141] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 14. | Shimura A, Sakai H, Inoue T. Paradoxical association between chronotype and academic achievement: eveningness reduces academic achievement through sleep disturbance and daytime sleepiness. Sleep Biol Rhythms. 2022;20:353-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Jongte L, Trivedi AK. Chronotype, sleep quality and academic performances among Mizo students. Chronobiol Int. 2022;39:398-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 16. | Morin CM, Espie CA. Insomnia: A Clinical Guide to Assessment and Treatment. 1st ed. New York: Springer Science & Business Media, 2007. Available from: https://link.springer.com/book/10.1007/b105845. |
| 17. | Sella E, Cellini N, Miola L, Sarlo M, Borella E. The Influence of Metacognitive Beliefs on Sleeping Difficulties in Older Adults. Appl Psychol Health Well Being. 2019;11:20-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Yang CM, Chou CP, Hsiao FC. The association of dysfunctional beliefs about sleep with vulnerability to stress-related sleep disturbance in young adults. Behav Sleep Med. 2011;9:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Peng J, Zhang T, Li Y, Wu L, Peng X, Li C, Lin X, Yu J, Mao L, Sun J, Fang P. Effects of dysfunctional beliefs about sleep on sleep quality and mental health among patients with COVID-19 treated in Fangcang shelter hospitals. Front Public Health. 2023;11:1129322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Jin L, Zhou J, Peng H, Ding S, Yuan H. Investigation on dysfunctional beliefs and attitudes about sleep in Chinese college students. Neuropsychiatr Dis Treat. 2018;14:1425-1432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Palagini L, Ong JC, Riemann D. The mediating role of sleep-related metacognitive processes in trait and pre-sleep state hyperarousal in insomnia disorder. J Psychosom Res. 2017;99:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 22. | Eidelman P, Talbot L, Ivers H, Bélanger L, Morin CM, Harvey AG. Change in Dysfunctional Beliefs About Sleep in Behavior Therapy, Cognitive Therapy, and Cognitive-Behavioral Therapy for Insomnia. Behav Ther. 2016;47:102-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 23. | Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46:124-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 914] [Cited by in RCA: 1058] [Article Influence: 66.1] [Reference Citation Analysis (0)] |
| 24. | Eller T, Aluoja A, Vasar V, Veldi M. Symptoms of anxiety and depression in Estonian medical students with sleep problems. Depress Anxiety. 2006;23:250-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 97] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 25. | Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97-110. [PubMed] |
| 26. | Pündük Z, Gür H, Ercan I. [A reliability study of the Turkish version of the mornings-evenings questionnaire]. Turk Psikiyatri Derg. 2005;16:40-45. [PubMed] |
| 27. | Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17520] [Cited by in RCA: 23416] [Article Influence: 632.9] [Reference Citation Analysis (0)] |
| 28. | Ağargün MY, Kara H, Anlar Ö. Pittsburgh Uyku Kalitesi İndeksi’nin geçerliği ve güvenirliği. Turk Psikiyatri Derg. 1996;7:107-115. Available from: https://psikiyatridizini.net/viewarticle.aspx?articleid=2668. |
| 29. | Morin CM, Vallières A, Ivers H. Dysfunctional beliefs and attitudes about sleep (DBAS): validation of a brief version (DBAS-16). Sleep. 2007;30:1547-1554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 578] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 30. | Boysan M, Merey Z, Kalafat T, Kağan M. Validation of a brief version of the dysfunctional beliefs and attitudes about sleep scale in Turkish sample. Procedia Soc Behav Sci. 2010;5:314-317. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | The Jamovi Project. Jamovi (Version 2.5). 2024. Available from: https://www.jamovi.org. |
| 32. | Gallucci M. jAMM: jamovi Advanced Mediation Models. 2020. Available from: https://jamovi-amm.github.io. |
| 33. | Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10:323-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 874] [Cited by in RCA: 695] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 34. | Karsan S, Kuhn T, Ogrodnik M, Middleton LE, Heisz JJ. Exploring the interactive effect of dysfunctional sleep beliefs and mental health on sleep in university students. Front Sleep. 2024;3. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 35. | Wang B, Wang Z, Zhang X, Ji Y, Shuai Y, Shen Y, Shen Z, Chen W. Relationship between dysfunctional beliefs and attitudes about sleep and mental health in medical staff: the mediating role of sleep quality. Sleep Breath. 2025;29:141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 36. | Firdous J, Haque E, Lyanna A, Nawwarah A, Najihah F, Norzahidah N, Zakiah NI, Syahirah N. Sleep Disruption and Its Impact on Academic Performance in Medical Students: A Systematic Review. Univers J Public Health. 2023;11:1-7. [DOI] [Full Text] |
| 37. | Concerto C, Conti C, Muscatello MR, Signorelli MS, Zoccali R, Coira D, Aguglia E, Battaglia F. Sleep Quality, Perceived Stress, and Caffeinated Drinks Intake in Psychiatry Residents: A Cross-Sectional Study. J Caffeine Res. 2017;7:18-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 38. | Wang Y, Guang Z, Zhang J, Han L, Zhang R, Chen Y, Chen Q, Liu Z, Gao Y, Wu R, Wang S. Effect of Sleep Quality on Anxiety and Depression Symptoms among College Students in China's Xizang Region: The Mediating Effect of Cognitive Emotion Regulation. Behav Sci (Basel). 2023;13:861. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 39. | Arora T, Vaquerizo-Villar F, Hornero R, Gozal D. Sleep irregularity is associated with night-time technology, dysfunctional sleep beliefs and subjective sleep parameters amongst female university students. Sci Rep. 2025;15:6374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 40. | Herzog-Krzywoszanska R, Krzywoszanski L. Bedtime Procrastination, Sleep-Related Behaviors, and Demographic Factors in an Online Survey on a Polish Sample. Front Neurosci. 2019;13:963. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 41. | van der Vinne V, Zerbini G, Siersema A, Pieper A, Merrow M, Hut RA, Roenneberg T, Kantermann T. Timing of examinations affects school performance differently in early and late chronotypes. J Biol Rhythms. 2015;30:53-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 42. | Varalakshmi D, Rathod D, Kumar DN, Sachdeva D. Investigating the relationship between sleep patterns and academic performance in college students. Asian J Manage Commerce. 2024;5:274-278. [DOI] [Full Text] |
| 43. | Valladares M, Ramírez-Tagle R, Muñoz MA, Obregón AM. Individual differences in chronotypes associated with academic performance among Chilean University students. Chronobiol Int. 2018;35:578-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 44. | Li M, Han Q, Pan Z, Wang K, Xie J, Zheng B, Lv J. Effectiveness of Multidomain Dormitory Environment and Roommate Intervention for Improving Sleep Quality of Medical College Students: A Cluster Randomised Controlled Trial in China. Int J Environ Res Public Health. 2022;19:15337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 45. | Poon K, Ho MSH, Tai APL, Leung MK, Chan MCM, Lau WKW. Mediating roles of sleep quality and resilience in the relationships between chronotypes and mental health symptoms. Sci Rep. 2024;14:5874. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |