Published online Dec 9, 2025. doi: 10.5409/wjcp.v14.i4.109771
Revised: June 20, 2025
Accepted: August 27, 2025
Published online: December 9, 2025
Processing time: 161 Days and 0 Hours
In pediatric patients, gallbladder polyps (GBPs) are lesions that are usually found incidentally on ultrasonography, which is the first-line modality for diagnosis. Though common in adults, GBPs are rare in children, and their prevalence re
Core Tip: Gallbladder polyps (GBPs) in children are rare and are often detected inci
- Citation: Al Atrash E, Ammori B. Approach to gallbladder polyps in pediatric patients. World J Clin Pediatr 2025; 14(4): 109771
- URL: https://www.wjgnet.com/2219-2808/full/v14/i4/109771.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v14.i4.109771
Gallbladder polyps (GBPs) are mucosal lesions that project into the lumen of the gallbladder, arising from the proliferation of the biliary epithelium. These lesions are most commonly identified incidentally, either during ultrasonographic examinations or following cholecystectomies[1]. With the increasing use of high-resolution ultrasonography (US), the detection rate of GBPs has significantly risen among both symptomatic and asymptomatic individuals[1,2]. In adults, GBPs are relatively common, observed in approximately 5% of patients undergoing abdominal US. In contrast, GBPs in the pediatric population are considered rare, and their true prevalence remains undefined. Although these polyps can occur at any age, including infancy, most reported pediatric cases fall within the median age range of 10–13 years, with a slightly higher incidence in females[2].
The majority of GBPs are benign in nature and are typically classified as hyperplastic or cholesterol polyps resulting from lipid accumulation. In adults, certain features are associated with an increased risk of malignancy, such as polyps greater than 10 mm in size[3]. However, similar criteria for assessing the malignant potential in children have not been clearly defined. The natural history of pediatric GBPs is highly variable, and current understanding of their malignancy risk remains limited.
Management strategies for pediatric GBPs are largely extrapolated from adult guidelines as no standardized treatment algorithm currently exists for children. This review aims to provide a comprehensive analysis of the classification, clinical characteristics, diagnostic modalities, and management strategies of gallbladder polyps in the pediatric population.
A comprehensive review of English-language literature on gallbladder polyps in children was conducted using two primary databases: PubMed and Google Scholar. The literature search encompassed publications from 1999 onwards and included meta-analyses, case reports, case series, systematic reviews, randomized controlled trials, and both prospective and retrospective cohort studies.
The search strategy utilized the keywords "gallbladder polyps" and "pediatrics". Abstracts were screened, and full-text articles of relevant studies were retrieved and evaluated. Duplicate publications were excluded. In areas where pediatric data were limited, the search was broadened to incorporate relevant adult literature.
The search yielded 14 case reports, 7 prospective studies, and 9 review articles. After excluding 5 articles deemed irrelevant, a total of 25 publications were included for full review.
In the 1970s, Christensen and Ishak[4] classified GBPs into benign polyps, pseudopolyps, and malignant neoplasms. Benign polyps include cholesterol accumulation, adenomas, hemangiomas, fibromas, lipomas, and leiomyomas. Pseudopolyps include cholesterol polyps, inflammatory polyps, cholesterolosis, adenomyomas, and hyperplastic polyps. Adenocarcinomas are accepted as malignant polyps[1,4].
Cholesterol polyps: Cholesterol polyps are the most common, representing approximately 60% of all GBPs, and are usually asymptomatic. Cholesterol polyps are usually multiple and pedunculated polypoid lesions less than 10 mm in diameter with no malignant potential and are usually diagnosed incidentally on US[1,2,4].
Inflammatory polyps: Inflammatory polyps may be sessile or pedunculated and are made up of granulation and fibrous tissue, along with plasma cells and lymphocytes, often associated with chronic cholecystitis. They account for 5%–10% of GBPs and are usually 5–10 mm in size[1,2,4].
Gallbladder adenomas: Gallbladder adenomas are the most common premalignant neoplastic lesions of the gallbladder and are commonly solitary lesions of 5–20 mm diameter. Their incidence increases with age. Their risk of malignant differentiation is usually correlated with polyp size[1,2,4].
Most pediatric GBPs are primary in nature, with an unclear etiology. Although several risk factors are associated with their formation, the underlying mechanisms in children differ significantly from those in adults. In adult populations, GBPs are commonly linked to metabolic factors, such as obesity and glucose intolerance, as well as male gender, cholelithiasis, and hepatitis B infection. In contrast, pediatric cases exhibit a distinct etiological profile with no strong evidence supporting associations with gender, obesity, or exogenous hormone exposure[5,6]. Instead, GBPs in children are more frequently observed in conjunction with specific genetic syndromes, such as Peutz-Jeghers syndrome and Gardner syndrome as well as congenital biliary abnormalities, including choledochal cysts[6].
Hyperlipidemia appears to be a shared risk factor for the development of GBPS in both pediatric and adult po
The likelihood of malignancy in pediatric patients with GBPs is exceedingly low. Nonetheless, recognizing potential risk factors for malignant transformation remains crucial for effective management and follow-up. In adult populations, several risk factors have been identified (Table 1), including polyps 10 mm in size, solitary and sessile polyps with irregular margins, presence of gallstones, localized thickening or irregularity of the gallbladder wall near the polyps, and rapid polyp growth during follow-up[11].
| Risk factor | Description | Evidence and references |
| Polyp size > 10 mm | Larger polyps have a higher risk of malignancy | In adults, polyps ≥ 10 mm have a 5.9% risk of gallbladder cancer; similar trends were observed in pediatric cases[17] |
| Sessile morphology | Sessile polyps are more likely to be malignant compared to pedunculated ones | Adult studies show sessile polyps increase malignancy risk by a factor of 7.32[16] |
| Associated genetic syndromes | Conditions like Peutz–Jeghers syndrome and metachromatic leukodystrophy may increase risk[14,15] | Pediatric cases with these syndromes have been noted to have GBPs with potential for malignancy |
| Presence of gallstones | Coexistence of gallstones may elevate the risk of malignancy[17] | Some studies suggest an increased risk, though evidence is not conclusive |
| Age > 50 years | Older age is a known risk factor for gallbladder cancer in adults; relevance in children is unclear[16] | Adult studies indicate increased malignancy risk with age over 50[16] |
While some studies have explored a possible link between gallstones and malignancy risk in GBPs, the evidence remains weak. Currently, there are no strong recommendations supporting prophylactic cholecystectomy solely based on the coexistence of gallstones and GBPs[12,13]. However, the presence of gallstones can obscure the accurate evaluation of polyps via US, necessitating a more careful imaging interpretation[13].
Additionally, genetic factors, such as primary sclerosing cholangitis or familial syndromes, particularly familial adenomatous polyposis, may elevate the risk of both polyp development and malignant transformation. That said, the natural history of gallbladder polyps in children is highly variable, and our understanding of their potential for malignancy remains limited[14-16].
Gallbladder polypoid lesions are typically asymptomatic and are most often detected incidentally during abdominal imaging[10]. In adults, the coexistence of cholelithiasis with GBPs is more frequent and contributes to symptomatic presentation, typically due to intermittent obstruction of the cystic duct. This can lead to biliary colic, a higher rate of complications, and ultimately increased detection rates, compared with pediatric populations[12].
Although rare, large or rapidly growing polyps may result in nausea, vomiting, obstructive jaundice, or even a palpable mass in the right upper quadrant due to the extrinsic compression of adjacent biliary structures[13].
In pediatric patients, abdominal pain is the most frequent clinical symptom prompting ultrasonographic evaluation. In a retrospective study by Demirbaş et al[8] 79% of pediatric cases were identified through imaging performed for abdominal pain, whereas 21% were discovered incidentally without specific hepatobiliary complaints. This trend was echoed by Ferzeliyev et al[10], who reported incidental detection in 73.3% of cases, with the remaining 26.7% presenting with localized right upper quadrant discomfort. Further supporting these findings, Bayram Kabaçam et al[16] reported that, among 74 patients who underwent cholecystectomy for GBPs, the vast majority (91%) presented with symptoms including right upper quadrant pain, dyspepsia, and jaundice. Ballouhey et al[17], in their analysis of 18 pediatric patients with GBPs, noted that 50% were symptomatic at diagnosis, highlighting the variability in presentation across different age groups and the role of lesion characteristics in symptomatology. These findings underline the importance of maintaining a high index of suspicion in symptomatic children and support the use of abdominal US as a frontline diagnostic tool.
Diagnostic imaging of gallbladder polyps: Radiological imaging plays a pivotal role in the diagnosis and management of GBPs by informing both therapeutic decisions and follow-up protocols. Imaging is critical not only for distinguishing polyps from other gallbladder abnormalities but also for differentiating true polyps from pseudopolyps, each requiring distinct clinical approaches due to differing malignant potential. Key modalities include US, computed tomography (CT), and magnetic resonance imaging (MRI), each with specific strengths and limitations[18].
Transabdominal US: Transabdominal US remains the cornerstone imaging technique for the detection and surveillance of gallbladder polyps. It is widely accessible, non-invasive, and free from ionizing radiation, making it particularly suitable for pediatric use[18]. US provides essential information on polyp size, number, and morphology. Polyps typically appear as fixed, non-shadowing, hyperechoic lesions protruding from the gallbladder wall, which helps differentiate them from mobile gallstones that cast acoustic shadows[19]. The limitations of US include difficulty in differentiating small polyps from biliary sludge or tiny calculi due to similar echogenic characteristics, and that the diagnostic accuracy is influenced by the operator’s expertise and the patient’s body habitus[18,19]. Despite these limitations, US remains the first-line diagnostic modality due to its safety, effectiveness and availability. Its diagnostic performance for polyps > 10 mm is well-documented with a sensitivity of 80% and specificity of 99.3%. A systematic review by Martin et al[20] found transabdominal US to have a pooled diagnostic sensitivity for GBPs of 79% and a specificity of 89%[19-21].
Contrast-enhanced US: Contrast-enhanced US is an emerging tool that augments the diagnostic power of traditional US. The utilization of intravenous contrast agents enhances visualization of vascular patterns within polyps and is particularly valuable for differentiating benign from malignant lesions[5,21]. This modality provides a real-time assessment of blood flow and perfusion characteristics, with diffuse and branched vascularity patterns being highly indicative of carcinoma and carries a 100% sensitivity and 76% specificity. However, the standardized application of contrast-enhanced US in children remains under development[21].
MRI and magnetic resonance cholangiopancreatography: MRI and magnetic resonance cholangiopancreatography (MRCP) offer superior soft tissue contrast and detailed imaging of the biliary system, making them particularly useful in evaluating suspected malignancy or complex biliary anatomy, and MRCP excels in visualizing bile duct structures and detecting obstructive abnormalities[22]. MRI also provides high-resolution images of the gallbladder and adjacent tissues, helping to distinguish polyps from other lesions. Importantly, MRI avoids ionizing radiation, which is advantageous in the pediatric population[22]. However, MRI comes with high cost and limited accessibility, and younger children may require sedation or general anesthesia for optimal image acquisition[21,22].
CT: CT delivers detailed cross-sectional imaging of the abdomen, allowing comprehensive assessment of gallbladder pathology and surrounding structures[22,23]. However, it is generally reserved for specific clinical indications due to concerns about radiation exposure in children. It is most often employed when malignancy is suspected or to evaluate suspected metastases when findings from other modalities are inconclusive[24].
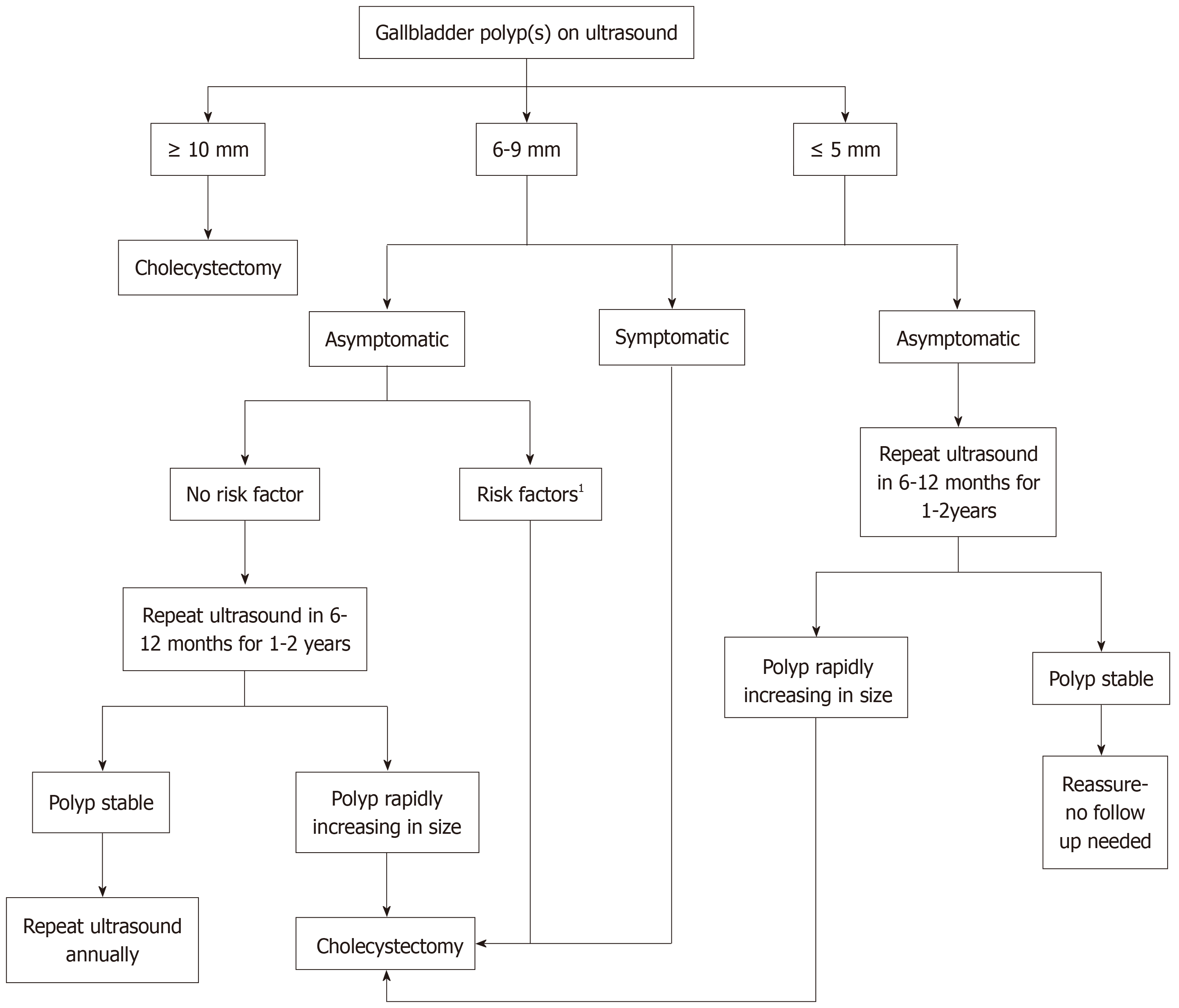
Currently, there are no universally established guidelines for the management of GBPs in children. Therapeutic decisions are primarily influenced by symptomatology, polyp size, morphology, and the presence of risk factors associated with malignant transformation. Figure 1 describes a flowchart for the management of GBPs in the pediatric population.
Symptomatic patients: Cholecystectomy remains the treatment of choice in pediatric patients presenting with sym
Asymptomatic patients: The management of asymptomatic GBPs is primarily guided by lesion size and the presence of risk factors suggestive of malignant potential. For polyps ≥ 10 mm, cholecystectomy is recommended due to the significantly increased risk of malignancy (Figure 1). MRI or CT may be employed to assess malignant features and assist in surgical planning[1,10,23]. The management of polyps 6–9 mm depends on associated risk factors, including sessile morphology, rapid interval growth, or a family history of gallbladder carcinoma, with surgical intervention being warranted if one or more risk factors are present; otherwise, follow-up with 6-12 monthly US for 1-2 years and annually thereafter is advisable to monitor polyp evolution[1,10]. Polyps ≤ 5 mm are typically benign, often cholesterol polyps, and rarely necessitate intervention. Surveillance with US at 6–12-month intervals for 1-2 years can be conducted to confirm lesion stability and can be discontinued if no changes are observed over time[1,10,22].
Special considerations in pediatric patients: The management of GBPs in children must consider several unique clinical and developmental factors that distinguish the pediatric population from adults. Due to the rarity of this condition in children, data remain limited, and evidence-based pediatric guidelines are lacking. Extrapolation from adult studies poses limitations as pediatric patients may differ in their clinical course, risk profiles, and response to treatment. The absence of large-scale pediatric-specific data necessitates the cautious interpretation of adult-based recommendations and highlights the need for further prospective studies focused on children. Additionally, whilst cholecystectomy is generally well-tolerated in children and is not associated with significant long-term adverse effects on growth or digestive function, concerns may arise regarding bile flow alterations and nutrient absorption, particularly in young children. Although the available literature suggests that, in most cases, growth trajectories and nutritional status remain unaffected post-cholecystectomy[18,24], individualized treatment planning is essential, particularly in children with coexisting metabolic or gastrointestinal disorders. A lower threshold for surgical intervention and closer radiologic follow-up may be warranted in children with a family history of gallbladder cancer or hereditary polyposis syndromes, such as Peutz-Jeghers syndrome or familial adenomatous polyposis, and such families should be offered genetic consultation[1,2,4,10].
The management of GBPs in pediatric patients requires a tailored approach based on symptom status, polyp size, morphology, and the presence of risk factors for malignancy. Cholecystectomy is recommended for symptomatic patients, larger polyps (≥ 10 mm), and smaller polyps with concerning features. For asymptomatic patients with small polyps (< 10 mm), surveillance imaging is the preferred approach to monitor for changes over time. While malignancy is rare in children, careful management and follow-up are essential to ensure optimal outcomes. Further research and pediatric-specific guidelines are needed to refine the treatment strategies for this rare condition.
| 1. | Stringer MD, Ceylan H, Ward K, Wyatt JI. Gallbladder polyps in children--classification and management. J Pediatr Surg. 2003;38:1680-1684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Jørgensen T, Jensen KH. Polyps in the gallbladder. A prevalence study. Scand J Gastroenterol. 1990;25:281-286. [PubMed] |
| 3. | Cha BH, Hwang JH, Lee SH, Kim JE, Cho JY, Kim H, Kim SY. Pre-operative factors that can predict neoplastic polypoid lesions of the gallbladder. World J Gastroenterol. 2011;17:2216-2222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 57] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 4. | Christensen AH, Ishak KG. Benign tumors and pseudotumors of the gallbladder. Report of 180 cases. Arch Pathol. 1970;90:423-432. [PubMed] |
| 5. | Yankov I, Boyanov N, Aleksova L, Ivanov B, Moshekov E, Chatalbashev D, Stefanova P. Gallbladder polyp in children - a rare finding during ultrasound examination. J Ultrason. 2022;22:e64-e66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Ali TA, Abougazia AS, Alnuaimi AS, Mohammed MAM. Prevalence and risk factors of gallbladder polyps in primary health care centers among patients examined by abdominal ultrasonography in Qatar: a case-control study. Qatar Med J. 2021;2021:48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Liu H, Lu Y, Shen K, Zhou M, Mao X, Li R. Advances in the management of gallbladder polyps: establishment of predictive models and the rise of gallbladder-preserving polypectomy procedures. BMC Gastroenterol. 2024;24:7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 8. | Demirbaş F, Çaltepe G, Comba A, Bilgin MC, Eren E, Abbasguliyev H, Kalayci AG. Gallbladder Polyps: Rare Lesions in Childhood. J Pediatr Gastroenterol Nutr. 2019;68:e89-e93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Yang HL, Kong L, Hou LL, Shen HF, Wang Y, Gu XG, Qin JM, Yin PH, Li Q. Analysis of risk factors for polypoid lesions of gallbladder among health examinees. World J Gastroenterol. 2012;18:3015-3019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 10. | Ferzeliyev O, Oğuz B, Soyer T, Boybey Türer Ö, Haliloglu M, Tanyel FC. Clinical Features and Outcomes of Gallbladder Polyps in Children. Turk J Gastroenterol. 2022;33:803-807. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Konstantinidis IT, Bajpai S, Kambadakone AR, Tanabe KK, Berger DL, Zheng H, Sahani DV, Lauwers GY, Fernandez-del Castillo C, Warshaw AL, Ferrone CR. Gallbladder lesions identified on ultrasound. Lessons from the last 10 years. J Gastrointest Surg. 2012;16:549-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 12. | Said K, Glaumann H, Bergquist A. Gallbladder disease in patients with primary sclerosing cholangitis. J Hepatol. 2008;48:598-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 119] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 13. | Zhu Y, Wang S, Zhao S, Qi L, Li Z, Bai Y. Obstructive jaundice due to a blood clot after ERCP: a case report and review of the literature. BMC Gastroenterol. 2018;18:163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Elmasry M, Lindop D, Dunne DF, Malik H, Poston GJ, Fenwick SW. The risk of malignancy in ultrasound detected gallbladder polyps: A systematic review. Int J Surg. 2016;33 Pt A:28-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 88] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 15. | Wiles R, Thoeni RF, Barbu ST, Vashist YK, Rafaelsen SR, Dewhurst C, Arvanitakis M, Lahaye M, Soltes M, Perinel J, Roberts SA. Management and follow-up of gallbladder polyps : Joint guidelines between the European Society of Gastrointestinal and Abdominal Radiology (ESGAR), European Association for Endoscopic Surgery and other Interventional Techniques (EAES), International Society of Digestive Surgery - European Federation (EFISDS) and European Society of Gastrointestinal Endoscopy (ESGE). Eur Radiol. 2017;27:3856-3866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 133] [Cited by in RCA: 167] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 16. | Bayram Kabaçam G, Akbıyık F, Livanelioğlu Z, Tiryaki HT, Karakuş E, Kabaçam G. Decision for surgery in the management of a rare condition, childhood gallbladder polyps, and the role of ultrasonography. Turk J Gastroenterol. 2013;24:556-560. [PubMed] |
| 17. | Ballouhey Q, Binet A, Varlet F, Baudry M, Dubois R, Héry G, Podevin G, Abbo O, Arnaud A, Barras M, Guerin F, Reinberg O, Piolat C, Fourcade L. Management of Polypoid Gallbladder Lesions in Children: A Multicenter Study. Eur J Pediatr Surg. 2018;28:6-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Beck PL, Shaffer EA, Gall DG, Sherman PM. The natural history and significance of ultrasonographically defined polypoid lesions of the gallbladder in children. J Pediatr Surg. 2007;42:1907-1912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | McCain RS, Diamond A, Jones C, Coleman HG. Current practices and future prospects for the management of gallbladder polyps: A topical review. World J Gastroenterol. 2018;24:2844-2852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 83] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (5)] |
| 20. | Martin E, Gill R, Debru E. Diagnostic accuracy of transabdominal ultrasonography for gallbladder polyps: systematic review. Can J Surg. 2018;61:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 21. | Akyürek N, Salman B, Irkörücü O, Sare M, Tatlicioğlu E. Ultrasonography in the diagnosis of true gallbladder polyps: the contradiction in the literature. HPB (Oxford). 2005;7:155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Liang X, Jing X. Meta-analysis of contrast-enhanced ultrasound and contrast-enhanced harmonic endoscopic ultrasound for the diagnosis of gallbladder malignancy. BMC Med Inform Decis Mak. 2020;20:235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Atherton JC. MRCP and the diagnosis of suspected bile duct obstruction. Gut. 1999;44:765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Chodick G, Kim KP, Shwarz M, Horev G, Shalev V, Ron E. Radiation risks from pediatric computed tomography scanning. Pediatr Endocrinol Rev. 2009;7:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/