Published online Jan 18, 2026. doi: 10.5312/wjo.v17.i1.112677
Revised: August 30, 2025
Accepted: November 11, 2025
Published online: January 18, 2026
Processing time: 160 Days and 2.6 Hours
Anterior cruciate ligament (ACL) reconstruction using bone-patellar tendon-bone (BPTB) autografts remains the gold standard for young, active individuals due to its superior biomechanical strength and bone-to-bone healing. However, donor site morbidity, particularly anterior knee pain (AKP), limits its utilization despite its advantages. Various techniques have been proposed to reduce AKP, but they show variable outcomes and several limitations.
To assess the incidence and severity of AKP following BPTB ACL reconstruction using an autologous bone grafting technique.
We conducted a retrospective observational study of 24 patients aged 20-45 years, who had primary ACL reconstruction with BPTB grafts. During surgery, au
With scores ranging from 86 to 100, the average overall Kujala score was 95.67 ± 4.01. No patient scored below 85. There was no complication such as patellar fracture, tibial tuberosity fracture, or infection. Grouped data showed 20.8% of patients scored 100, whereas 54.2% scored between 95 and 99, and 25% scored between 86 and 94. One patient (4.2%) had an 8/10 pain subcomponent, whereas 23 patients (95.8%) had a 10/10.
This procedure is easy to incorporate into routine surgical practice, cost-effective and reproducible without requiring extra incisions or raising the patient’s surgical expenses. Excellent short-term results back up this technique.
Core Tip: This study highlights that by utilizing bone already available from femoral and tibial tunnel drilling during bone-patellar tendon-bone anterior cruciate ligament reconstruction, routine bone grafting of donor tibial and patella harvest site defects is a simple and reproducible technique that results in excellent functional outcomes with minimal donor site morbidity. This method offers a cost-effective approach. The high Kujala scores and absence of clinically significant anterior knee pain in this cohort support the integration of this technique into standard surgical practice.
- Citation: Byravamoni Venugopal A, Chauhan N, Wani S, Maramreddy LVSK, Pathak K, Mittal R. Anterior knee pain in anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft and autologous bone grafting. World J Orthop 2026; 17(1): 112677
- URL: https://www.wjgnet.com/2218-5836/full/v17/i1/112677.htm
- DOI: https://dx.doi.org/10.5312/wjo.v17.i1.112677
Anterior cruciate ligament (ACL) tears are among the most frequently encountered orthopaedic injuries, particularly in young individuals and athletes involved in pivoting sports[1-5]. Surgical reconstruction using autologous grafts is the standard treatment for restoring knee stability and function[6-9]. Among the available graft options, the bone-patellar tendon-bone (BPTB) autograft remains a popular choice due to its superior biomechanical properties, including bone-to-bone healing, high tensile strength, and reliable graft fixation[7,10-12].
However, despite these advantages, BPTB grafts are often associated with donor site morbidity, particularly anterior knee pain (AKP), which can significantly hinder postoperative rehabilitation, delay return to sports, and reduce overall patient satisfaction[6,13-15]. The incidence of AKP following BPTB graft harvest has been reported in multiple studies to be as high as 48%[16-18].
The etiology of AKP after BPTB ACL reconstruction is multifactorial[14,19,20]. Several strategies have been proposed to address this issue. While some studies report reduced morbidity with these techniques, concerns remain regarding graft strength, donor site healing, and increased surgical costs[13,14,21].
This study aims to evaluate the incidence and severity of AKP following BPTB ACL reconstruction using an autologous bone grafting technique. Cancellous bone harvested during femoral and tibial tunnel drilling was used to fill the patellar and tibial bone defects, as described by Krishna et al[22]. We assessed the clinical utility of this approach in reducing donor site morbidity by analyzing functional outcomes and AKP scores in patients who underwent this grafting method.
This retrospective observational study was conducted after obtaining ethical approval from the institutional ethics committee. The study size included all consecutive patients who underwent ACL reconstruction with the novel bone grafting technique between July 2022 and April 2024, as identified from the hospital record database. Patients meeting the inclusion criteria were contacted telephonically from July 15 to July 30, 2025, and included in the study after obtaining verbal informed consent. The inclusion criteria comprised adults aged 20-45 years who underwent primary ACL reconstruction using a BPTB graft with autologous bone grafting. Only patients with a minimum postoperative follow-up of twelve months were included. Exclusion criteria were revision ACL surgeries, multiligamentous knee injuries, and cases with incomplete medical records or inadequate follow-up data.
All patients underwent ACL reconstruction using a BPTB autograft. An oblique incision from the centre of the patella to a point 1 cm distal and 1.5 cm medial to the tibial tuberosity was used to approach the patellar tendon. The central third of the patellar tendon was harvested along with bony plugs from the patella and tibial tuberosity. While harvesting bone plugs, a 1 cm wide saw blade was used. The cuts were made adequately so that the bone plugs could be harvested only by levering out with a small osteotome. No hammering of the osteotome was done. Autologous cancellous bone ge
Postoperative functional assessment was conducted using the Kujala Anterior Knee Pain Score. The pain component of the Kujala score was also assessed independently.
Data were analyzed using Statistical Package for the Social Sciences version 30. Continuous variables are expressed as mean ± SD, categorical variables are presented as n (%). Given the retrospective nature of the study without a control group, comparative hypothesis testing was not performed. Instead, our results were benchmarked against well do
Twenty-four patients were included in the study. The mean age was 28.54 ± 5.17 years, with 11 males (45.83%) and 13 females (54.17%). The mean total Kujala score was 95.67 ± 4.01, indicating a high level of knee function and minimal anterior knee discomfort across the cohort. The scores ranged from 86 to 100, and importantly, none of the patients had a score below 85, which is generally considered the threshold for clinically significant AKP (Table 1). Grouped data showed 20.8% patients scored 100, 54.2% scored between 95 and 99, 16.7% scored between 90 and 94 and 8.3% scored between 86 and 89. Focusing specifically on the pain subcomponent within the Kujala scale, 23 out of 24 patients (95.8%) reported a perfect score of 10 out of 10, reflecting an absence of AKP during routine activities. Only one patient (4.2%) scored 8 out of 10, indicating mild anterior knee discomfort (Table 2). No intraoperative or postoperative complications were observed in the study population. There were no cases of patellar fracture, tibial tuberosity fracture, wound infection, or donor site complications such as persistent pain, numbness, or delayed healing.
| Kujala score range | Number of patients | Percentage |
| 100 | 5 | 20.8 |
| 95-99 | 13 | 54.2 |
| 90-94 | 4 | 16.7 |
| 86-89 | 2 | 8.3 |
| Pain score | Number of patients | Percentage |
| 10/10 | 23 | 95.8 |
| 8/10 | 1 | 4.2 |
AKP is a well-documented complication following ACL reconstruction with BPTB autografts[14,23-26]. It has a complex pathophysiology and remains one of the key deterrents for surgeons and patients considering BPTB grafts, despite their superior biomechanical advantages[14,18]. Previous literature has consistently reported AKP in up to 48% of cases following such reconstructions[16,17]. The cause of AKP postoperatively can be traced to direct trauma during tendon harvesting, stripping of periosteum, damage to the infrapatellar nerve, formation of scar tissue[18,20], and most im
Across studies using BPTB autografts without donor-site bone grafting (Table 3)[16,17,23-25], the reported incidence of AKP at approximately 2 years varies considerably, ranging from 16.1% in the series by Aune et al[23] to 48.4% in that of Guglielmetti et al[16], with Shaieb et al[24] reporting 41.9%. With extended follow-up, Sajovic et al[17] documented an incidence of 48.0% at 11 years, indicating that AKP may persist over time. By contrast, studies incorporating donor-site bone grafting have consistently demonstrated lower rates. Brandsson et al[25] reported a 12.5% incidence at 2 years following grafting of the patellar defect, while the present study, employing routine grafting of both patellar and tibial harvest sites, observed an incidence of only 4.2% at 1 year.
| Ref. | Technique | Number of patients | Follow-up (years) | Anterior knee pain incidence |
| Brandsson et al[25], 1998 | BPTB, bone grafting (only patella defect) | 29 | 2 | 12.5 |
| Aune et al[23], 2001 | BPTB, no bone grafting | 29 | 2 | 16.1 |
| Shaieb et al[24], 2002 | BPTB, no bone grafting | 31 | 2 | 41.9 |
| Sajovic et al[17], 2011 | BPTB, no bone grafting | 32 | 11 | 48.0 |
| Guglielmetti et al[16], 2021 | BPTB, no bone grafting | 31 | 2 | 48.4 |
| Present study | BPTB + donor-site bone grafting | 24 | 1 | 4.2 |
Several approaches have been explored to manage this complication[32-35]. Some have utilized bone grafts from separate donor sites to fill the void left after the graft harvest. The use of synthetic bone substitutes has also been studied, but results have been inconsistent due to limited biological integration and slower incorporation into native bone. The technique used in this study addresses these limitations by employing autologous bone obtained from tunnel drilling during the same surgical procedure. This method offers immediate availability, eliminates the need for additional incisions, and promotes superior biological incorporation.
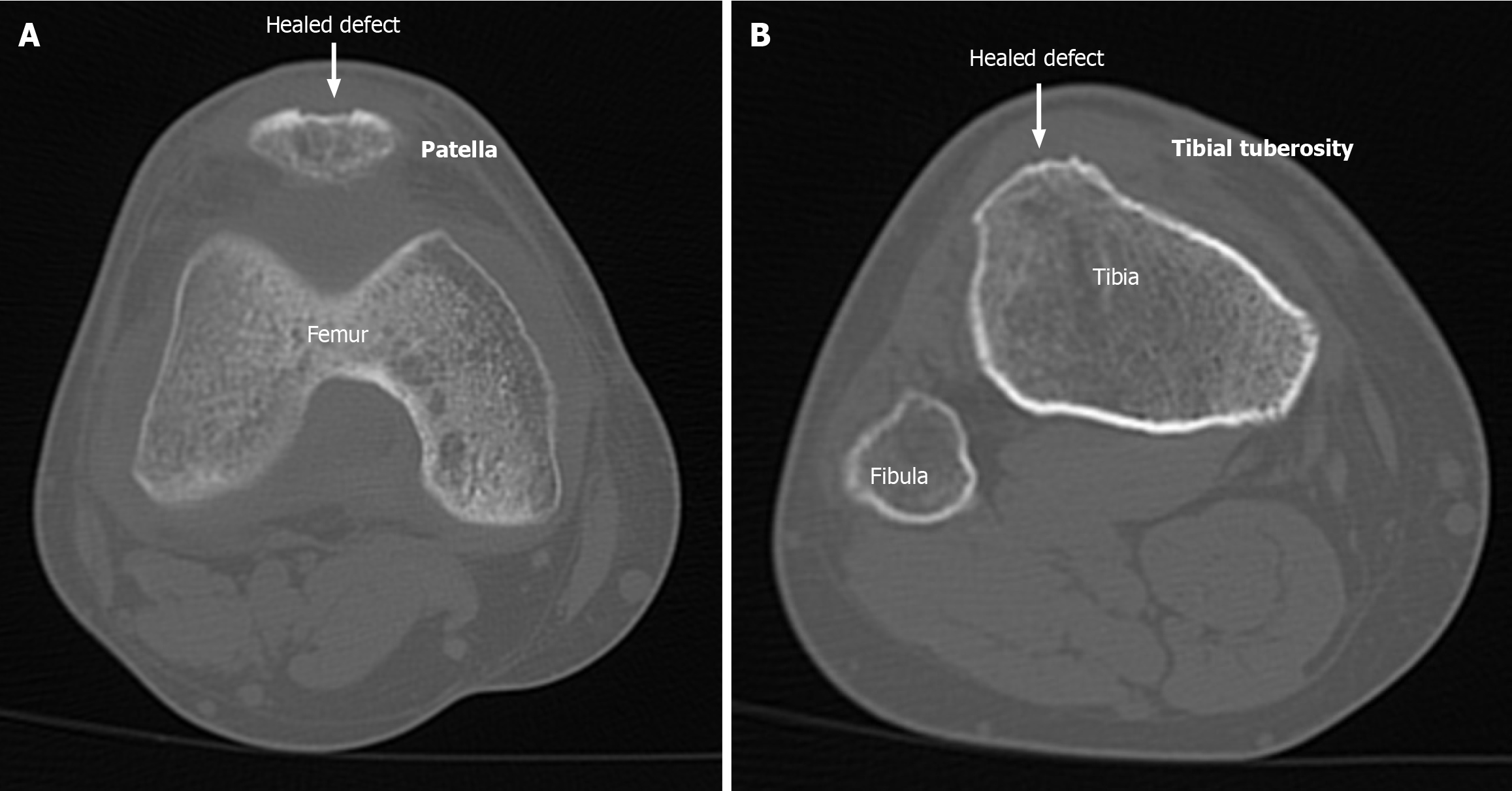
The technique was originally described by Krishna et al[22]. Our study presents the first clinical outcome data, using the same technique. We observed a mean Kujala score of 95.67 ± 4.01, with all patients scoring above 85% and 95.8% achieving a perfect pain score of 10/10. These findings indicate an extremely low incidence of clinically significant AKP and suggest that the autologous bone grafting of tibial and patellar bone defects is both effective and safe. Figure 1 showing the healing of both tibial and patellar defects in one of the patients.
From a cost-effectiveness perspective, this technique offers immense benefits, especially in resource-limited settings. Unlike synthetic grafts or secondary autograft harvests, this method requires no additional surgical steps or expenses.
However, the study is not without limitations. Its retrospective design carries an inherent potential for selection and recall bias. Furthermore, being a single-centre study with a relatively small sample size, the generalizability of the findings may be limited. The grafting technique itself requires additional operative time for harvesting cancellous bone graft and filling the donor-site voids. Additionally, this study lacks a control group, which limits direct comparative statistical analysis of this technique’s benefits. However, we have presented our outcome results against the well-documented historical rates of AKP from the literature (Table 3)[16,17,23-25]. Finally, the one year follow up is shorter than that of many comparative studies. While this timeframe is sufficient to show early morbidities and pain that is important for patient rehabilitation, larger prospective trials with longer follow-up are needed to validate these findings and perhaps standardize this technique.
This study demonstrates that bone grafting of donor tibial and patella harvest site defects during BPTB is a simple, biologically effective, and reproducible technique that results in excellent functional outcomes with minimal donor site morbidity. By utilizing bone already available from femoral and tibial tunnel drilling, this method offers a cost-effective approach without added surgical complexity. The high Kujala scores and absence of clinically significant AKP in this cohort support the integration of this technique into standard surgical practice. Future prospective studies with larger sample sizes and longer follow-up durations are warranted to confirm these findings and further establish this technique as a standard of care in ACL reconstruction using BPTB grafts.
| 1. | Montalvo AM, Schneider DK, Webster KE, Yut L, Galloway MT, Heidt RS Jr, Kaeding CC, Kremcheck TE, Magnussen RA, Parikh SN, Stanfield DT, Wall EJ, Myer GD. Anterior Cruciate Ligament Injury Risk in Sport: A Systematic Review and Meta-Analysis of Injury Incidence by Sex and Sport Classification. J Athl Train. 2019;54:472-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 197] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 2. | Chia L, De Oliveira Silva D, Whalan M, McKay MJ, Sullivan J, Fuller CW, Pappas E. Non-contact Anterior Cruciate Ligament Injury Epidemiology in Team-Ball Sports: A Systematic Review with Meta-analysis by Sex, Age, Sport, Participation Level, and Exposure Type. Sports Med. 2022;52:2447-2467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 108] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 3. | Larwa J, Stoy C, Chafetz RS, Boniello M, Franklin C. Stiff Landings, Core Stability, and Dynamic Knee Valgus: A Systematic Review on Documented Anterior Cruciate Ligament Ruptures in Male and Female Athletes. Int J Environ Res Public Health. 2021;18:3826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 4. | Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, Stuart MJ, Krych AJ. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am J Sports Med. 2016;44:1502-1507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 508] [Cited by in RCA: 865] [Article Influence: 86.5] [Reference Citation Analysis (0)] |
| 5. | Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and Diagnosis of Anterior Cruciate Ligament Injuries. Clin Sports Med. 2017;36:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 368] [Article Influence: 40.9] [Reference Citation Analysis (0)] |
| 6. | Herbawi F, Lozano-Lozano M, Lopez-Garzon M, Postigo-Martin P, Ortiz-Comino L, Martin-Alguacil JL, Arroyo-Morales M, Fernandez-Lao C. A Systematic Review and Meta-Analysis of Strength Recovery Measured by Isokinetic Dynamometer Technology after Anterior Cruciate Ligament Reconstruction Using Quadriceps Tendon Autografts vs. Hamstring Tendon Autografts or Patellar Tendon Autografts. Int J Environ Res Public Health. 2022;19:6764. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Dai W, Leng X, Wang J, Cheng J, Hu X, Ao Y. Quadriceps Tendon Autograft Versus Bone-Patellar Tendon-Bone and Hamstring Tendon Autografts for Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med. 2022;50:3425-3439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 105] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 8. | Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E. Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis of Outcomes for Quadriceps Tendon Autograft Versus Bone-Patellar Tendon-Bone and Hamstring-Tendon Autografts. Am J Sports Med. 2019;47:3531-3540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 321] [Article Influence: 45.9] [Reference Citation Analysis (0)] |
| 9. | Murray MM. Optimizing outcomes of ACL surgery-Is autograft reconstruction the only reasonable option? J Orthop Res. 2021;39:1843-1850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Bergeron JJ, Sercia QP, Drager J, Pelet S, Belzile EL. Return to Baseline Physical Activity After Bone-Patellar Tendon-Bone Versus Hamstring Tendon Autografts for Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Am J Sports Med. 2022;50:2292-2303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Zhao D, Pan JK, Lin FZ, Luo MH, Liang GH, Zeng LF, Huang HT, Han YH, Xu NJ, Yang WY, Liu J. Risk Factors for Revision or Rerupture After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med. 2023;51:3053-3075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 78] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 12. | Sporsheim AN, Gifstad T, Lundemo TO, Engebretsen L, Strand T, Mølster A, Drogset JO. Autologous BPTB ACL Reconstruction Results in Lower Failure Rates Than ACL Repair with and without Synthetic Augmentation at 30 Years of Follow-up: A Prospective Randomized Study. J Bone Joint Surg Am. 2019;101:2074-2081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Georgoulis JD, Savvidou OD, Patras K, Melissaridou D, Hadjimichael AC, Papagelopoulos PJ, Georgoulis AD. Association of Anterior Knee Pain With Extension Deficit After Anterior Cruciate Ligament Reconstruction: A Systematic Review. Orthop J Sports Med. 2024;12:23259671241265840. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Janani G, Suresh P, Prakash A, Parthiban J, Anand K, Arumugam S. Anterior knee pain in ACL reconstruction with BPTB graft - Is it a myth? Comparative outcome analysis with hamstring graft in 1,250 patients. J Orthop. 2020;22:408-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Kovindha K, Ganokroj P, Lertwanich P, Vanadurongwan B. Quantifying anterior knee pain during specific activities after using the bone-patellar tendon-bone graft for arthroscopic anterior cruciate ligament reconstruction. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2019;15:6-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Guglielmetti LGB, Salas VER, Jorge PB, Severino FR, Duarte A, de Oliveira VM, Cury RPL. Prospective and Randomized Clinical Evaluation of Hamstring Versus Patellar Tendon Autograft for Anterior Cruciate Ligament Reconstruction in Soccer Players. Orthop J Sports Med. 2021;9:23259671211028168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39:2161-2169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 150] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 18. | Mukhopadhyay R, Shah N, Vakta R, Bhatt J. Anterior knee pain following BPTB graft harvest. Reality or overhyped. J Clin Orthop Trauma. 2018;9:307-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Martorell-de Fortuny L, Torres-Claramunt R, Sánchez-Soler JF, Perelli S, Hinarejos P, Monllau JC. Patellar bone defect grafting does not reduce anterior knee pain after bone-patellar tendon-bone anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2025;33:1299-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 20. | Peebles LA, Akamefula RA, Aman ZS, Verma A, Scillia AJ, Mulcahey MK, Kraeutler MJ. Following Anterior Cruciate Ligament Reconstruction With Bone-Patellar Tendon-Bone Autograft, the Incidence of Anterior Knee Pain Ranges From 5.4% to 48.4% and the Incidence of Kneeling Pain Ranges From 4.0% to 75.6%: A Systematic Review of Level I Studies. Arthrosc Sports Med Rehabil. 2024;6:100902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 21. | Tsuda E, Okamura Y, Ishibashi Y, Otsuka H, Toh S. Techniques for reducing anterior knee symptoms after anterior cruciate ligament reconstruction using a bone-patellar tendon-bone autograft. Am J Sports Med. 2001;29:450-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 75] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Krishna MLVS, Mittal R, Chauhan N. Bone Grafting of the Bone Defects after Harvesting the Bone Patellar Tendon Bone Graft - A Novel Surgical Technique. J Orthop Case Rep. 2023;13:72-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Aune AK, Holm I, Risberg MA, Jensen HK, Steen H. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction. A randomized study with two-year follow-up. Am J Sports Med. 2001;29:722-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 297] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 24. | Shaieb MD, Kan DM, Chang SK, Marumoto JM, Richardson AB. A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:214-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 210] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 25. | Brandsson S, Faxén E, Eriksson BI, Kälebo P, Swärd L, Lundin O, Karlsson J. Closing patellar tendon defects after anterior cruciate ligament reconstruction: absence of any benefit. Knee Surg Sports Traumatol Arthrosc. 1998;6:82-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | He X, Yang XG, Feng JT, Wang F, Huang HC, He JQ, Hu YC. Clinical Outcomes of the Central Third Patellar Tendon Versus Four-strand Hamstring Tendon Autograft Used for Anterior Cruciate Ligament Reconstruction: A Systematic Review and Subgroup Meta-analysis of Randomized Controlled Trials. Injury. 2020;51:1714-1725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Fares A, Hardy A, Bohu Y, Meyer A, Karam K, Lefevre N. The impact of bone graft type used to fill bone defects in patients undergoing ACL reconstruction with bone-patellar tendon-bone (BPTB) autograft on kneeling, anterior knee pain and knee functional outcomes. Eur J Orthop Surg Traumatol. 2024;34:181-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 28. | Suri M, Verma A, Khalid MA, Nammour M, Godshaw B. Functional Anterior Knee Pain and Return to Sport Following Bone-Patellar Tendon-Bone Anterior Cruciate Ligament Reconstruction. Ochsner J. 2023;23:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 29. | Marques FDS, Barbosa PHB, Alves PR, Zelada S, Nunes RPDS, de Souza MR, Pedro MDAC, Nunes JF, Alves WM Jr, de Campos GC. Anterior Knee Pain After Anterior Cruciate Ligament Reconstruction. Orthop J Sports Med. 2020;8:2325967120961082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 30. | Ochiai S, Hagino T, Senga S, Yamashita T, Oda K, Haro H. Injury to infrapatellar branch of saphenous nerve in anterior cruciate ligament reconstruction using vertical skin incision for hamstring harvesting: risk factors and the influence of treatment outcome. J Orthop Surg Res. 2017;12:101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 31. | Widner M, Dunleavy M, Lynch S. Outcomes Following ACL Reconstruction Based on Graft Type: Are all Grafts Equivalent? Curr Rev Musculoskelet Med. 2019;12:460-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 104] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 32. | Ferrari JD, Bach BR Jr. Bone graft procurement for patellar defect grafting in anterior cruciate ligament reconstruction. Arthroscopy. 1998;14:543-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | Shichman I, Baruchi D, Rachevsky G, Amzallag N, Brandstetter AS, Vidra M, Morag G. Bone filling decreases donor site morbidity after anterior cruciate ligament reconstruction with bone-patellar tendon-bone autografts. Arch Orthop Trauma Surg. 2023;143:2565-2572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Schandl K, Horváthy DB, Doros A, Majzik E, Schwarz CM, Csönge L, Abkarovits G, Bucsi L, Lacza Z. Bone-Albumin filling decreases donor site morbidity and enhances bone formation after anterior cruciate ligament reconstruction with bone-patellar tendon-bone autografts. Int Orthop. 2016;40:2097-2104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 35. | Higuchi H, Kobayashi A, Ikeda K, Hatayama K, Yanagisawa S, Kato K. Efficacy of β-Tricalcium Phosphate Graft into the Bone Defects after Bone-Patellar Tendon-Bone Anterior Cruciate Ligament Reconstruction. J Knee Surg. 2017;30:467-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/