Published online Jan 18, 2026. doi: 10.5312/wjo.v17.i1.112222
Revised: August 21, 2025
Accepted: November 28, 2025
Published online: January 18, 2026
Processing time: 172 Days and 13.5 Hours
Ankle fractures are well-documented in snow sports, but concomitant Achilles tendon and peroneal tendon ruptures are rare. This case report presents a pre
A 50-year-old male snowboarder presented with severe right ankle pain following a high speed tumbling crash. Initial evaluation revealed an Achilles tendon ru
This case underscores the importance of maintaining a high index of suspicion for concomitant injuries in high-energy ankle trauma during snow sports. Timely advanced imaging and a comprehensive surgical approach are crucial for optimal outcomes in such complex cases.
Core Tip: Here, we present the case report of a previously unreported injury pattern: Concomitant Achilles tendon rupture, peroneal tendon ruptures, and Weber A lateral malleolus fracture sustained in a high energy snowboarding fall. Initially, peroneal tendon tears were missed and discovered intraoperatively, changing the course of clinical care. We discuss the mechanism of injury and review the literature around similar cases of high energy tendon rupture and concomitant ankle fracture. This case underscores the importance of maintaining a high index of suspicion for concomitant injuries in high-energy ankle trauma during snow sports.
- Citation: Vlasak A, Orear C, Sakryd G, Metzl J. Achilles, peroneus longus and brevis ruptures with lateral malleolus fracture: A case report and review of literature. World J Orthop 2026; 17(1): 112222
- URL: https://www.wjgnet.com/2218-5836/full/v17/i1/112222.htm
- DOI: https://dx.doi.org/10.5312/wjo.v17.i1.112222
Snowboarding is a popular winter sport associated with distinct injury profiles due to high-energy falls in fixed boot-binding systems. While ankle fractures and Achilles tendon ruptures have been reported independently in snowboarders, simultaneous occurrence of these injuries is rare. Even less frequently documented are cases in which Achilles tendon rupture occurs in conjunction with peroneal tendon injuries or malleolar fractures. These complex trauma cases present diagnostic and management challenges, particularly as initial clinical examination may fail to detect concomitant tendon pathology without a high index of suspicion for these trauma patterns.
Here we describe a previously unreported injury triad—Achilles tendon rupture, complete peroneus longus and brevis tendon ruptures, and a Weber A lateral malleolus fracture—in a recreational snowboarder. This case highlights the biomechanical forces involved in snowboarding injuries, underscores the importance of maintaining a high index of suspicion for multi-structure ankle trauma, and reviews the limited literature on combined Achilles, peroneal, and malleolar injuries.
A 50-year-old male presented to clinic with chief complaints of right ankle pain and inability to bear weight.
A 50-year-old male presented to the clinic 3 days status post snowboarding fall at a local ski area. He reported a tumbling fall down the hill in which he reported feeling a severe “pop” in the posterior aspect of the right ankle. He was unable to bear weight and was transported down the hill via ski patrol to the clinic ski area base. He was evaluated by an on-site physician and diagnosed with an Achilles tendon rupture. Radiographs from the facility demonstrated a non-displaced Weber A lateral malleolus fracture. The patient was placed into a well-padded posterior slab split, given crutches, and instructed to remain non-weight bearing until follow-up with orthopedic surgery.
The patient had no past medical history relevant to his acute condition.
The patient had no relevant personal or family history relevant to his acute condition.
Physical exam of the right lower extremity upon presentation to the orthopedic clinic revealed a positive Thompson and Matles test, moderate global ecchymosis and moderate soft tissue edema about the foot and ankle. There was a palpable defect in the Achilles tendon approximately 6 cm proximal to the calcaneal insertion. The patient reported tenderness over the deltoid ligament and lateral malleolus. There was significant loss of strength with resisted plantar flexion and eversion of the ankle.
No laboratory examinations were obtained.
Subsequently, magnetic resonance imaging (MRI) of the right ankle was obtained.
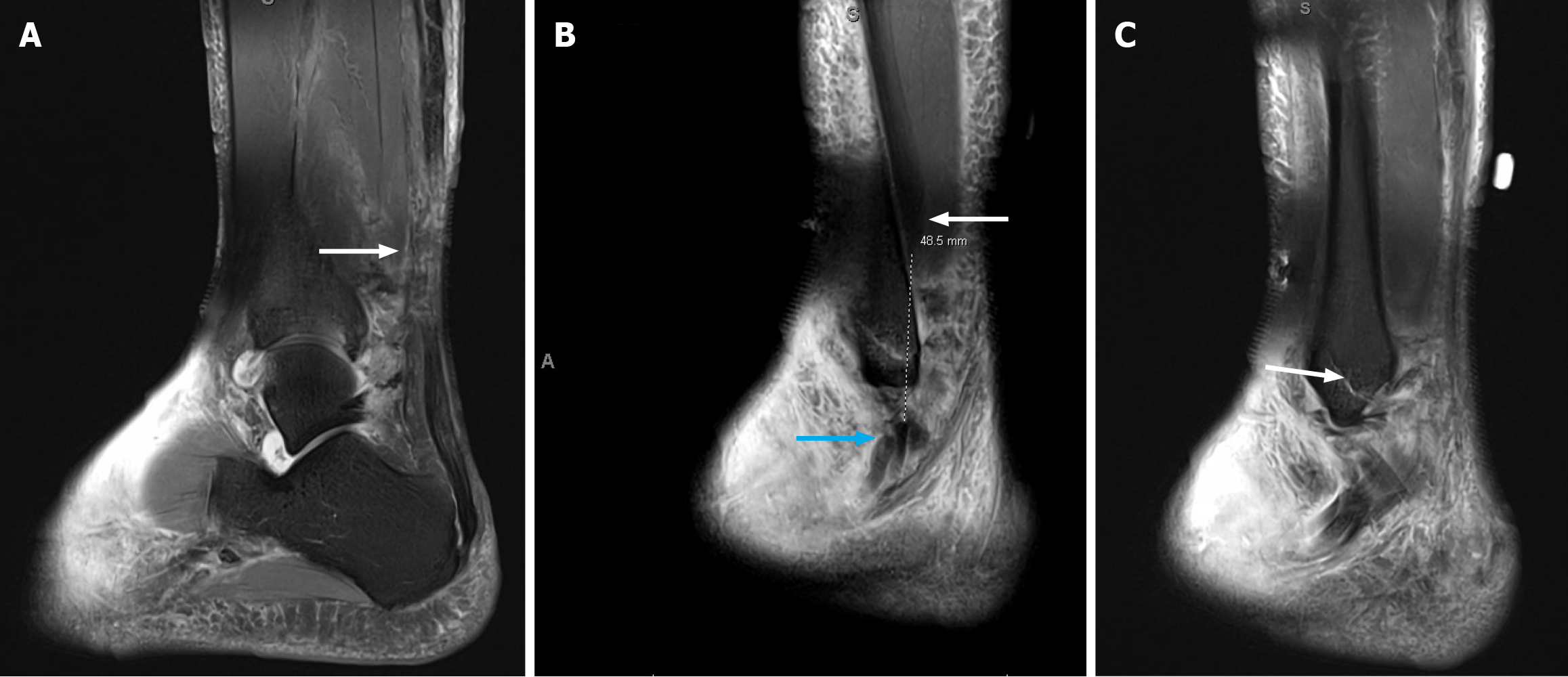
MRI findings included: (1) Complete tear of the Achilles tendon approximately 6 cm proximal to the calcaneal attachment, with approximately 5 cm of diastasis between the torn portions of the tendon (Figure 1A, Video 1); (2) Complete tears of the peroneus longus and brevis tendons, located just proximal to the lateral malleolus with approximately 5 cm of diastases between the torn portions of the two tendons (Figure 1B, Video 1); (3) Strain and partial tearing of the distal myotendinous junction of the flexor hallucis longus muscle. Moderate strain of the distal tibialis posterior tendon without discrete tear (Video 1); (4) Nondisplaced fracture of the distal lateral malleolus, distal to the talar dome (Figure 1C). Additional marrow contusions of the medial cuneiform, dorsal anterior talus, and anterior distal tibia; (5) Sprain with suspected high-grade partial-thickness tearing of the deep deltoid ligament fibers; and (6) Sprain and likely low-grade partial tearing of the anterior talofibular ligament and calcaneofibular ligaments of the fibular attachment. Distal tibiofibular ligaments appeared scarred without evidence of acute tear.
After a lengthy discussion with the patient regarding the severity of his injury, all parties agreed that surgical intervention was the best course of action. The planned surgery included Achilles tendon repair with repair of both peroneal tendons. Given the non-displaced nature of the lateral malleolus fracture, nonoperative treatment was anti
Informed consent was obtained after discussing the risks, benefits, and alternatives to surgery. Specific risks-including bleeding, infection, wound complications, numbness, neuritis, neurovascular injury, deep venous thrombosis, non-union, malunion, and persistent discomfort - were reviewed in detail. The severity of the injury, risk of postoperative stiffness, and potential need for revision or tendon transfer procedures were also discussed.
General endotracheal anesthesia was initiated in the operating room (the patient declined pre-operative popliteal block but did consent to post-operative rescue block if needed). For ease of placement before positioning a thigh tourniquet was placed on the right lower extremity and was used throughout the entirety of the procedure. The patient was placed into the prone position taking care to ensure that all vital structures were well-padded. The operative extremity was then prepped and draped in sterile fashion.
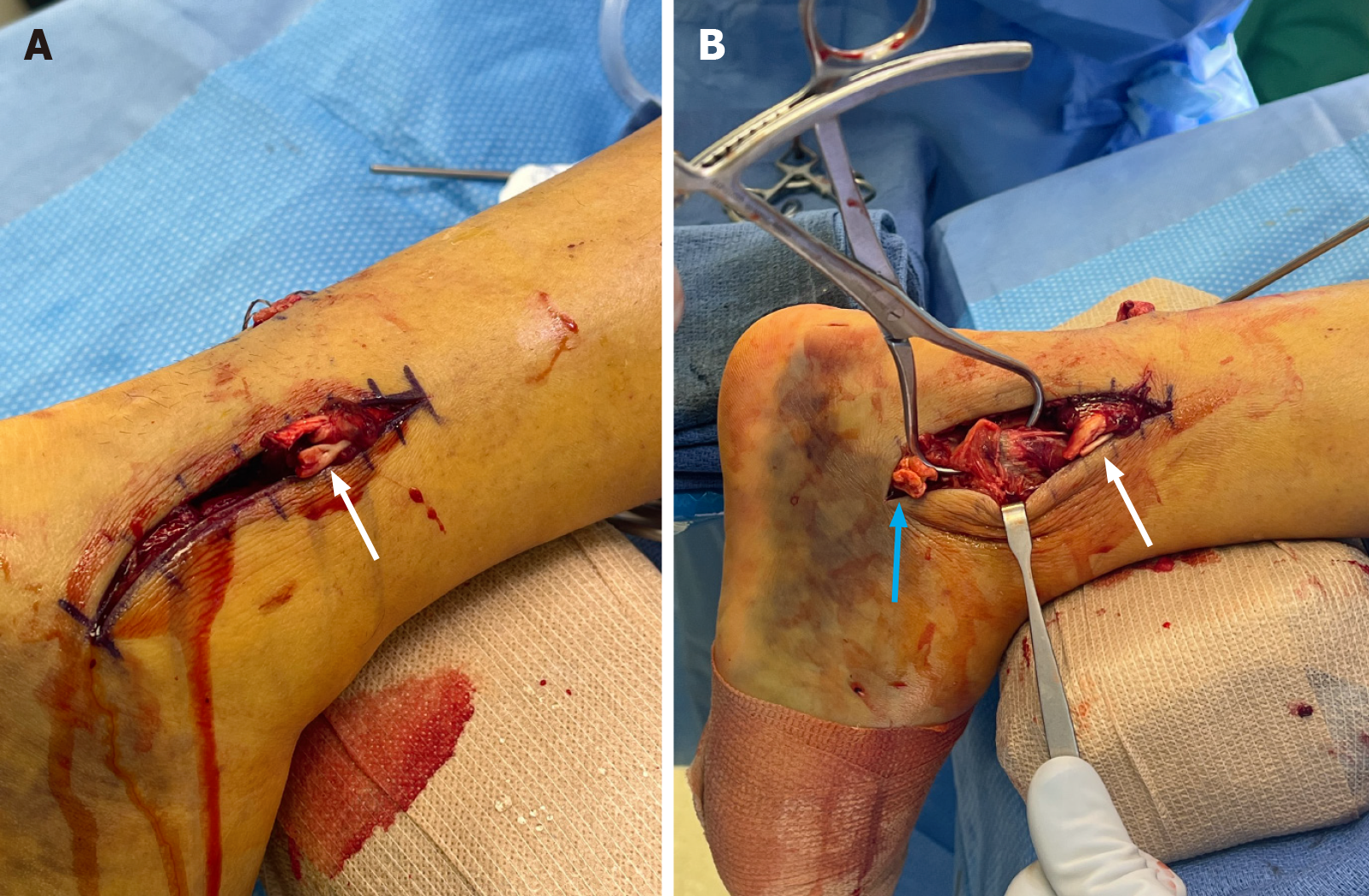
A longitudinal incision measuring 2 cm was made over the more proximal aspect of the Achilles tendon rupture. The incision was created slightly medial to the midline for greater protection of the sural nerve. Care was taken to gently retract skin flaps and dissection was carried to paratenon. Longitudinal deep incision was carried through the isolated paratenon layer (in line with the incision) and paratenon flaps were carefully preserved for later repair. The proximal tendon stump was identified and tendon ends were debrided of hematoma and secured with a 4-suture core Kraków repair (Figure 2). A flat nonabsorbable braided suture tape composed of ultra-high molecular weight polyethylene and polyester approximately 2 mm in width was selected for the repair to add additional surface area to the repair.
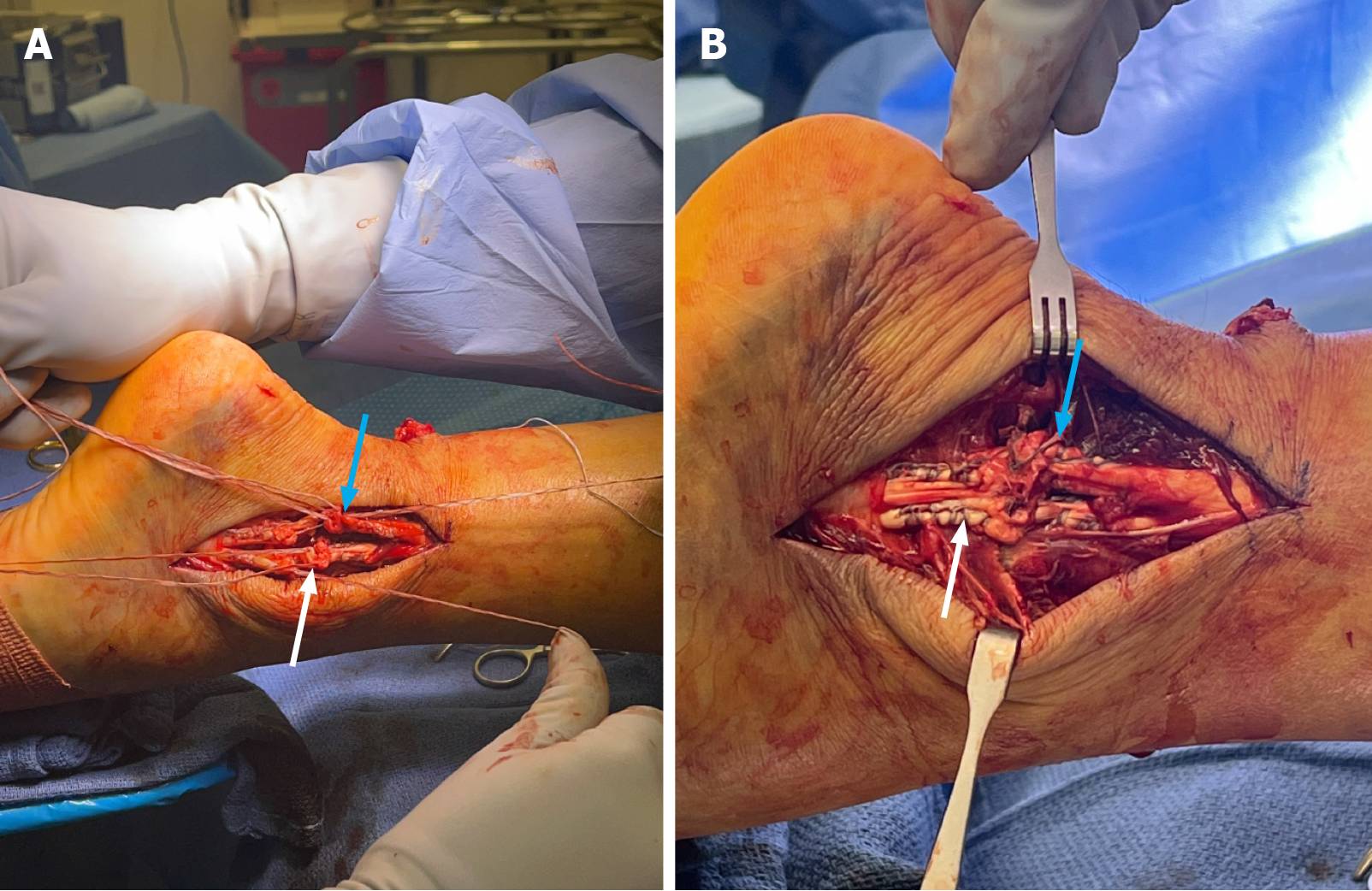
Next, attention was directed to the peroneal pathology prior to completing the distal Achilles repair. A separate incision over the posterior-lateral aspect of the ankle was made to access the peroneal tendons and posterior fibula. Lacerations of both the peroneus longus and brevis tendons were immediately identified (Figure 3); the tendons were sharply transected as opposed to irregularly torn. Inspection more anteriorly revealed that the distal fibula fracture was at the level of the peroneal tendon lacerations, revealing that the fibula had broken and the proximal spike had propagated transection of the adjacent peroneus longus and brevis tendons. At this point, fixation of the fibula fracture was performed to protect the repaired tendons from further damage after their repair. The distal fibular fracture was anatomically reduced and secured with two 3.0 mm lag (by technique) screws (Figure 4). The heads were countersunk to reduce the risk of adjacent soft tissue or tendon irritation. With the distal fibula reduced and fixated, a 2-suture core Kraków repair of the peroneus longus and brevis tendons both proximally and distally was completed with a braided long strand suture composed of ultra-high molecular weight polyethylene and polyester (Figure 5A). This resulted in anatomic approximation of the tendon ends (Figure 5B). A 4.0 nonabsorbable monofilament polypropylene suture was utilized for epitendinous reinforcement of the peroneal tendon repairs providing additional fixation. The peroneal tendons were stable through gentle passive ankle range of motion, without subluxation or dislocation within the retromalleolar groove.
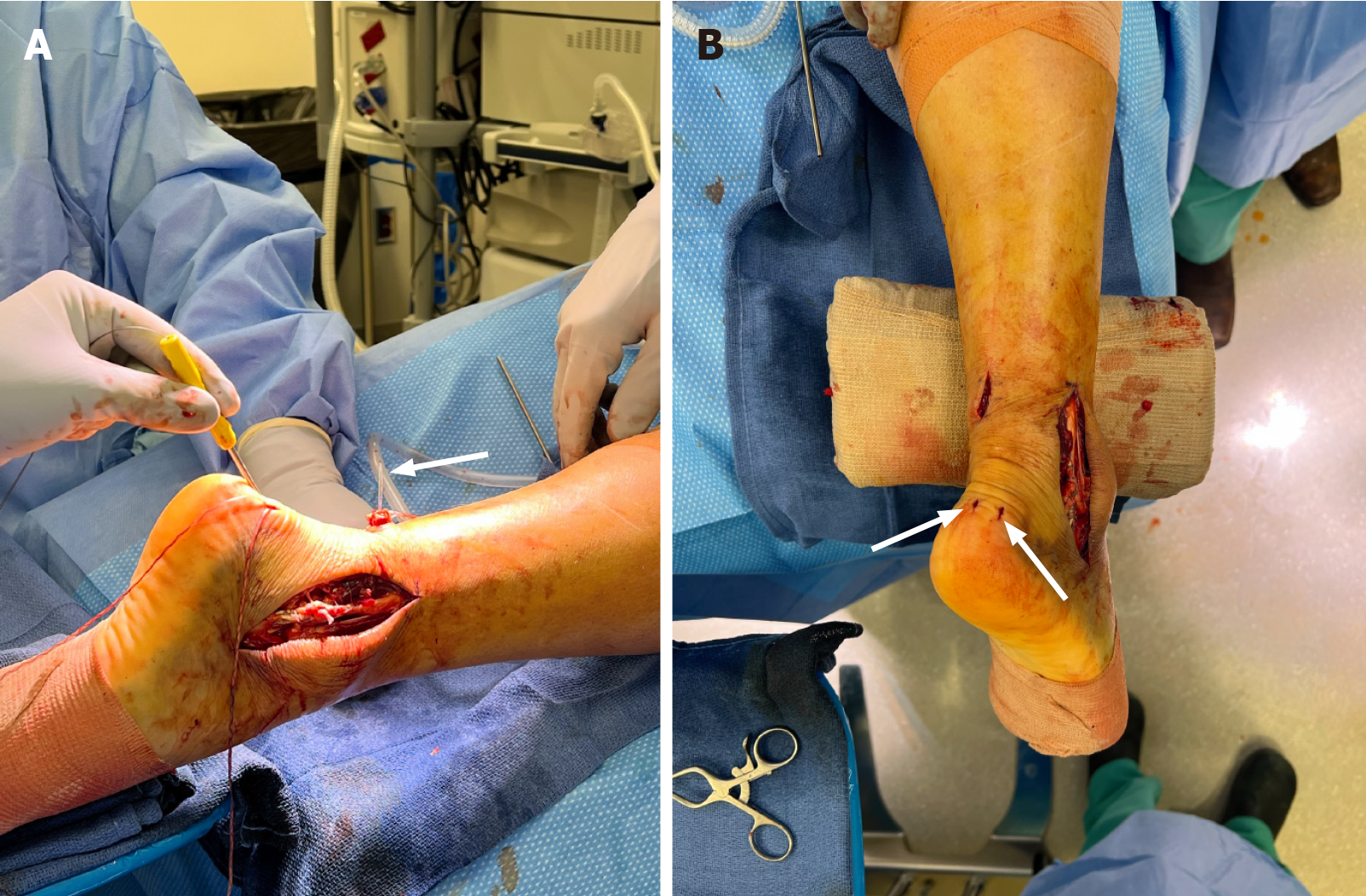
Due to the high-energy injury to the Achilles tendon and need for concomitant peroneal tendon and distal fibular fracture repair, we elected to proceed with docking the proximal Achilles tendon stump into the calcaneus. Two 4.0 mm knotless polyetheretherketone anchors were introduced into the Achilles tendon insertion on the calcaneus via two separate stab incisions. The Kraków repair of the more proximal aspect of the rupture was then shuttled subcutaneously from proximal to distal (Figure 6A) and passed through the anchors with the foot in maximum plantar flexion (to allow ideal tension to be incurred over the repair) completing the distal aspect of the repair (Figure 6B).
The wounds were then irrigated and closed in a layered fashion. Care was taken to carefully close paratenon flaps over the Achilles tendon to restore tendon vascularity and help tendon gliding. Sterile dressings and splint were applied with the foot in maximal plantar flexion. The patient did not require a rescue block and was discharged to home the same day.
Due to the severity of his injury, a modified Achilles’ repair protocol was initiated. The patient returned to clinic 8 days post-surgery. The splint was removed. Incisions were healing well. A short leg cast was applied in maximal plantar flexion. The patient was non-weight bearing for three weeks total. At the 3-week mark post-surgery, the patient returned to clinic for cast and suture removal. Radiographs demonstrated well maintained fracture fixation with no loss of reduction. The patient was placed in a boot with heel lifts (three foam wedges approximately 2.5 cm of height each) and instructed to be partial weightbearing (approximately 50%) for 3 weeks. The patient was instructed to remove one heel lift per week over the next three weeks as tolerated. At 4 weeks post-op, formal physical therapy began with gentle passive range of motion with ankle dorsi-flexion limited to 0 degrees (neutral) and effusion/edema control. At the 6 weeks post-op visit, skin incisions were well healed over. Radiographs again showed maintained reduction of the distal fibula fracture. Active range of motion of the ankle was somewhat limited, but the patient was able to obtain dorsiflexion to neutral. The patient was instructed to slowly start weight bearing as tolerated and to progress off crutches while wearing the boot. Once the patient was able to ambulate without crutches comfortably in the boot, they were instructed to progress to normal footwear. The patient was able to achieve these goals by approximately 8 weeks post-surgery. Physical therapy progressed along normal protocols with progressive range of motion (ROM), gait training, and then progression to strengthening activities. Radiographs at the 16-week mark (approximately 4 months) demonstrated a well healed distal fibula fracture (Figure 7). Physical exam revealed intact Achilles and peroneal tendon repairs. Range of motion was still mildly limited in dorsiflexion (10 degrees active ROM); however, the patient was back to full daily and work activities with no restrictions. At the 6-month mark post-surgery, the patient was able to perform a single leg heel lift without difficulty and was progressing with recreational activities (including a 40-mile bike ride). Approximately 1.5 years post-surgery the patient is doing well and participating in high level athletic activities without pain or functional limitation (Figure 8, Video 2).
This case report delineates a novel injury complex in a snowboarder, comprising concurrent Achilles tendon rupture, lateral malleolus fracture, and complete peroneal tendon tears - an injury triad previously unreported in the literature. Concomitant Achilles ruptures with medial malleolus fractures have been well-reported recently in the literature[1-10]. Additionally, several cases were reported before the early 2000s, bringing the total number of isolated case reports of concomitant Achilles rupture and medial malleolus fracture to 14[11-14]. Additionally, 2 case reports of Achilles tendon rupture with lateral malleolus fracture[15,16] and 2 case reports of Achilles tendon rupture with trimalleolar ankle fracture have been described[17,18]. There have been 3 case reports documenting concomitant superior peroneal re
| Ref. | Patient | Mechanism | Key injuries | Management | Outcome |
| Present case | 50-year-old male, snowboarder | High-energy tumbling fall; immediate “pop”, unable to bear weight | Achilles rupture; complete peroneus longus and brevis ruptures; nondisplaced Weber A distal lateral malleolus fracture; additional bone marrow contusions on MRI | Achilles Kraków repair with calcaneal docking using two 4.0 mm knotless PEEK anchors; primary repair of both peroneal tendons; ORIF distal fibula; cast/boot with staged heel lifts; early PT with DF limited to neutral initially | 16 weeks: Fracture healed, repairs intact; 6 months: Single-leg heel rise, full activities; approximately 1.5 years: High-level athletics without pain/Limits |
| Bowers et al[26], 2021 | 35-year-old male, snowboarder | Jump landing on rock causing hyperdorsiflexion and eversion | Midsubstance Achilles rupture; medial malleolus fracture (posterior colliculus avulsion) with deep deltoid injury; SPR avulsion with peroneal dislocation; CFL avulsion; distal fibular cortical avulsion | Percutaneous Achilles tendon-to-bone fixation with two 4.75 mm × 15 mm anchors; indirect fibular groove deepening; CFL repair; SPR repair with knotless anchors; deep deltoid anchor repair; staged heel lifts; PT progression with DF past neutral only after 8 weeks | 4 months: Wounds healed, normal gait; 9 months: Returned to all activities, no limitations |
| Jadib et al[18], 2024 | 44-year-old male, snowboarder | High-energy ankle trauma; initially casted, surgery at 2 weeks | Subcutaneous Achilles rupture 4 cm from insertion with approximately 5 cm gap; trimalleolar fracture without syndesmotic opening; traumatic peroneal dislocation with SPR bony avulsion; distal fibular avulsion | Open end-to-end Achilles Krakow repair with absorbable sutures; excision small avulsed fibular fragment; SPR reinsertion via bone tunnels; medial/posterior malleoli left unfixed after satisfactory reduction; splint/cast in approximately 10 PF; staged rehab and PT | 12 months: MRI confirmed healed Achilles/SPR and fractures; 18 months: Full ROM, returned to all activities; fractures healed radiographically |
The injury pattern is most coherently explained as a sequential torsional cascade produced by snowboarding’s fixed-foot kinematics, wherein a rotational fall transmits multiplanar loads through the hindfoot-ankle axis without the protective dissipation afforded by independent foot motion. In this setting, forced dorsiflexion appears to be the initiating vector, abruptly tensioning the gastrocsoleus complex and preloading the Achilles to eccentric failure risk under sudden axial constraint. Superimposed eversion and external rotation then increase lateral hindfoot stress, elevating traction on the peroneal tendons within the retromalleolar groove and on the superior peroneal retinaculum, a failure pattern mechanistically consistent with snowboard-related torsional insults described by Lee and Schuberth in concomitant overload scenarios of the posterior and lateral structures[22]. Reflexive or protective co-contraction of the triceps surae and peroneal musculature at the moment of peak torsion likely amplifies tensile forces across both tendon complexes, further predisposing to rupture or subluxation under constrained rotation.
In addition to these soft-tissue-directed forces, the osseous response of the distal fibula can contribute to tendon injury propagation. A subtle initial displacement at the moment of the fibular fracture may orient the fracture line such that a sharp cortical edge becomes exposed toward the peroneal corridor; in this configuration, the fragment’s bevel can act as a focal cutting interface during continued eversion-external rotation and tendon excursion, initiating a linear rent in the peroneal tendons that propagates into a partial- or full-thickness tear under ongoing load. This tendon-bone interaction is biomechanically plausible within the same torsional cascade: Rotational energy can present the fracture edge to the moving tendon, converting frictional shear into a laceration-like failure rather than a purely eccentric traction-based rupture. The net result is a triad: (1) Achilles rupture from forced dorsiflexion under active contraction; (2) Peroneal retinacular disruption with tendon subluxation and a fracture-edge-initiated rent that progresses to tearing; and (3) Distal fibular fracture as the osseous result of transmitted rotation in the fixed-binding context. While Lee and Schuberth[22] emphasize the coupled overload of the Achilles-peroneal retinacular complex under snowboard torsion, the present case reflects greater lateral soft-tissue compromise consistent with an interposed sharp fracture margin exacerbating tendon injury propagation within the peroneal sheath.
A final anatomic factor likely contributing to the severity of this combined injury in this case is its occurrence on the right foot in a snowboarder. Research indicates that the majority of snowboarders use the “regular” stance (right foot rearward) rather than the “goofy” stance (left foot rearward). In a large epidemiological study of 1918 snowboarders with upper extremity injuries, 90.8% were riding in the “regular” stance, while only 9.2% used the “goofy” stance[27]. Research also indicates that the rear foot in snowboarding often experiences greater forces. On study showed that during carving turns, especially toe-side turns, riders may exert greater forces on the rear foot[28]. Another study found that the largest moments (rotational forces) at the ankle joint occur in the rear leg during snowboarding, suggesting higher mechanical demands on the rear foot compared to the front[29]. Plantar pressure analyses also reveal that during both front-side and back-side turns, significant vertical force and pressure are applied to the rear foot, supporting the idea of increased loading on the rear leg in various turn scenarios[30]. All of these findings serve to highlight that the patient’s right lower extremity was likely the rear leg in this scenario, the result of which is a much greater injuring force than had it involved the left lower extremity.
The high rate of missed diagnoses in combined injuries reinforces the necessity for mechanism-based suspicion[16]. Swelling and pain often mask subtle findings, as evidenced by the initial oversight of concomitant peroneal tears in this case. A 2020 literature review of 17 documented cases of combined ankle fractures and Achilles tendon ruptures revealed Achilles tendon ruptures were initially missed in 47% of cases (8/17) while ankle fractures went undetected in 12% (2/17). A delay in diagnosing these injuries can result in considerable long-term morbidity for patients, including persistent pain, weakness, and loss of ankle motion[18].
Advanced imaging's value emerges when contrasting diagnostic modalities: While radiographs identified the fracture, MRI’s soft tissue resolution proved important for detecting the tendon pathologies, corroborating Bowers et al’s advocacy for MRI in high-energy ankle trauma[26]. This imaging imperative gains further urgency considering that a percentage of Achilles ruptures present with intact Thompson tests[31] due to interfragmentary hematoma stabilization and plantarflexion produced by extrinsic foot flexors, potentially delaying diagnosis. At a minimum, all patients in cases such this (with a clear high energy Achilles rupture) must undergo anterior posterior and lateral ankle radiographs[5].
The surgical strategy utilized addressed the injury’s complexity through a combination of bone anchors and limited dissection to optimize the balance between mechanical integrity and tissue preservation[32], facilitating early mobi
In this case, although non-operative management of select distal fibula fractures can be appropriate (and was initially considered), operative fixation was selected to address the unique interplay between osseous instability and concomitant tendon pathology observed intraoperatively. Specifically, the distal fibular fracture lay at the level of the sharply transected peroneus longus and brevis, and reduction stabilized a cortical spike that had likely functioned as a focal cutting interface; fixation removed this exposed edge from the peroneal corridor, restored the retromalleolar buttress, and provided a stable platform to protect primary tendon repairs from recurrent mechanical compromise during early rehabilitation. This choice aligns with established principles in peroneal instability and fracture-associated lateral ankle injuries, wherein bony avulsion or marginal fractures at the posterolateral fibula reflect superior peroneal retinaculum compromise and tendon maltracking, often necessitating osseous stabilization to reconstitute the groove-retinaculum complex and prevent reluxation or attritional tendon failure. Moreover, in high-energy snowboard mechanisms com
Rehabilitation protocols in cases such as this must reconcile conflicting priorities: early motion to prevent stiffness vs protected healing of repaired tendon and bone. The 12-week graduated weight-bearing regimen, incorporating elements from both fracture and tendon protocols, represents a pragmatic synthesis of existing frameworks[34] and aligns with recent evidence that controlled early mobilization may lead to the best outcomes with functional rehabilitation in operatively treated Achilles ruptures[35,36].
This case underscores several practical imperatives for clinicians managing high-energy snowboarding ankle injuries. First, maintain a high index of suspicion for combined injuries when an acute Achilles rupture is identified, as con
Future research should prioritize standardized evaluation protocols and biomechanical studies analyzing forces generated during modern snowboarding maneuvers, particularly aerial tricks and backcountry and terrain park impacts that drive complex injury phenotypes. As snowboarding mechanics evolve, understanding these multidimensional tra
| 1. | Nicolás Fontecilla C, Hube Laurent M, Bastías Bedoya G, Fuentes Carvajal P, Arancibia Mettais M. Acute Achilles Tendon Rupture Associated with Medial Malleolar Fracture: Is it Still a Rare Injury? Case Report and Review of the Literature. Int J Foot Ankle. 2018;2. [DOI] [Full Text] |
| 2. | Nakajima K, Taketomi S, Inui H, Nakamura K, Sanada T, Tanaka S. Missed Medial Malleolar Fracture Associated With Achilles Tendon Rupture: A Case Report and Literature Review. J Foot Ankle Surg. 2016;55:169-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Elmajee M, Rafee A, Williams T. Ankle Fracture Associated With Rupture of the Achilles Tendon: Case Report and Review of the Literature. J Foot Ankle Surg. 2017;56:1320-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Wai LK, Hing LT. Unrecognised Acute Rupture of the Achilles Tendon in Severe Ankle Sprain. J Orthop Trauma Reha. 2015;19:97-99. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Lu J, Maruo Holledge M. Medial malleolus fracture of the ankle combined with rupture of the Achilles tendon. J Surg Case Rep. 2016;2016:rjw062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Türkmensoy F, Türkmen I, Turhan Y, Özkan K, Akçal MA. Achilles Tendon Rupture with Isolated Medial Malleolar Fracture in Ipsilateral Ankle: A Case Report. Open J Orthop. 2013;03:224-226. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Maffulli N, Richards PJ. Subcutaneous rupture of the Achilles tendon and ipsilateral fracture of the medial malleolus. BMC Musculoskelet Disord. 2006;7:59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Tanaka M, Shimizu H. Concurrent occurrence of Achilles tendon rupture and medial malleolar fracture of the ankle joint: a case report. Internet J Orthop Surg. 2009;15. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Assal M, Stern R, Peter R. Fracture of the ankle associated with rupture of the Achilles tendon: case report and review of the literature. J Orthop Trauma. 2002;16:358-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Garneti N, Muralikuttan K, Shenolikar A. Ankle fracture associated with an Achilles tendon rupture: a rare injury. Foot Ankle Surg. 2005;11:219-222. [DOI] [Full Text] |
| 11. | Lubin JW, Miller RA, Robinson BJ, Blevins FT. Achilles tendon rupture associated with ankle fracture. Am J Orthop (Belle Mead NJ). 2000;29:707-708. [PubMed] |
| 12. | Pieper HG, Radas CB, Quack G, Krahl H. Mediomalleolar fracture combined with Achilles tendon rupture--a rare simultaneous injury of the ankle. Int J Sports Med. 1998;19:68-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Martin JW, Thompson GH. Achilles Tendon Rupture. Clin Orthop Relat R. 1986;210:216-218. [DOI] [Full Text] |
| 14. | Barron JL, Yocum LA. Unrecognized Achilles tendon rupture associated with ipsilateral medial malleolar fracture. Am J Sports Med. 1993;21:629-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Mattos e Dinato MC, de Farias Freitas M, D'Elia CO, Bitar AC, Rodrigues Gonçalves FM. Acute calcaneus tendon rupture associated with ipsilateral malleolar fracture: case report and literature review. J Foot Ankle Surg. 2010;49:565.e1-565.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Pyle LH, Al-Gharib RW, Kissel EC. Lateral Malleolar Fracture with Concurrent Achilles Tendon Rupture: A Case Report and Literature Review. Case Rep Emerg Med. 2020;2020:6479140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Brueton RN, Javid KS. Trimalleolar fracture and associated Achilles tendon rupture: Ten year follow up of an unusual water-skiing injury. Trauma Case Rep. 2018;17:33-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Jadib I, Veyrat G, Ionescu S, Belvisi B, Chirpaz-Cerbat JM. Trimalleolar Fracture Associated with Subcutaneous Rupture of the Achilles Tendon and Traumatic Peroneal Dislocation: A Case Report and Review of the Literature. JBJS Case Connect. 2024;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Kopp F. Traumatic peroneal dislocation with medial malleolus fracture: a case report. Foot Ankle Int. 2008;29:756-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Vosoughi AR, Erfani MA. Concomitant Traumatic Peroneal Tendon Dislocation and Medial Malleolus Fracture: A Case Report. Malays Orthop J. 2018;12:57-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Malik AK, Mehta S, Solan M. Significance of flake fracture with medial malleolar fracture. Foot Ankle Int. 2013;34:749-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Lee J, Schuberth JM. Concomitant rupture of achilles tendon and superior peroneal retinaculum: a case report. J Foot Ankle Surg. 2010;49:176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Marti R. Dislocation of the peroneal tendons. Am J Sports Med. 1977;5:19-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 66] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Pelet S, Saglini M, Garofalo R, Wettstein M, Mouhsine E. Traumatic rupture of both peroneal longus and brevis tendons. Foot Ankle Int. 2003;24:721-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Vosoughi AR, Trnka HJ. Peroneal Tendons Rupture in a Closed Talar Body Fracture: A Rare Injury. J Foot Ankle Surg. 2020;59:625-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Bowers M, Hunt KJ, Metzl J. High-Energy Achilles Tendon Rupture With Associated Medial Malleolus Fracture and Traumatic Peroneal Dislocation: A Case Report. Foot Ankle Spec. 2021;14:438-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 27. | Yamauchi K, Wakahara K, Fukuta M, Matsumoto K, Sumi H, Shimizu K, Miyamoto K. Characteristics of upper extremity injuries sustained by falling during snowboarding: a study of 1918 cases. Am J Sports Med. 2010;38:1468-1474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Feeney D, Vladika B, Harrison K. Turn kinetics during snowboard carving. Footwear Sci. 2021;13:S43-S45. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Klous M, Müller E, Schwameder H. Three-dimensional lower extremity joint loading in a carved ski and snowboard turn: a pilot study. Comput Math Methods Med. 2014;2014:340272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Lee C, Nam K, Back J. Biomechanical Analysis of Snowboard Riding Motions. Int J Bio-Sci Bio-Tech. 2017;8:243-252. [DOI] [Full Text] |
| 31. | Inglis AE, Sculco TP. Surgical Repair of Ruptures of the Tendo Achillis. Clin Orthop Relat R. 1981;156:160-169. [DOI] [Full Text] |
| 32. | Clanton TO, Haytmanek CT, Williams BT, Civitarese DM, Turnbull TL, Massey MB, Wijdicks CA, LaPrade RF. A Biomechanical Comparison of an Open Repair and 3 Minimally Invasive Percutaneous Achilles Tendon Repair Techniques During a Simulated, Progressive Rehabilitation Protocol. Am J Sports Med. 2015;43:1957-1964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 89] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 33. | Boin MA, Dorweiler MA, McMellen CJ, Gould GC, Laughlin RT. Suture-Only Repair Versus Suture Anchor-Augmented Repair for Achilles Tendon Ruptures With a Short Distal Stump: A Biomechanical Comparison. Orthop J Sports Med. 2017;5:2325967116678722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2012;94:2136-2143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 325] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 35. | McCormack R, Bovard J. Early functional rehabilitation or cast immobilisation for the postoperative management of acute Achilles tendon rupture? A systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2015;49:1329-1335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 36. | Barfod KW, Bencke J, Lauridsen HB, Dippmann C, Ebskov L, Troelsen A. Nonoperative, dynamic treatment of acute achilles tendon rupture: influence of early weightbearing on biomechanical properties of the plantar flexor muscle-tendon complex-a blinded, randomized, controlled trial. J Foot Ankle Surg. 2015;54:220-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/