Published online Nov 18, 2025. doi: 10.5312/wjo.v16.i11.111052
Revised: August 15, 2025
Accepted: September 25, 2025
Published online: November 18, 2025
Processing time: 145 Days and 21.1 Hours
Comminuted calcaneal fractures present significant treatment challenges. Open reduction and internal fixation carries risks such as infection and skin necrosis, while minimally invasive techniques may compromise reduction stability. Con
A 60-year-old female presented with left foot pain and limited mobility following a fall. Computed tomography scan revealed a Sanders type IV calcaneal fracture with a Böhler angle of 0°. A standardized, stepwise Traditional Chinese manual bone-setting was initially performed, followed by percutaneous screw fixation through several mini-incisions after satisfactory alignment was confirmed under fluoroscopy. The Visual Analog Scale score decreased from 5 on postoperative day 1 to 3 by day 3. The American Orthopaedic Foot and Ankle Society score improved from 73 at 6 weeks to 90 at 3 months, indicating rapid functional recovery and high patient satisfaction. At 7 months postoperatively, the American Orthopaedic Foot and Ankle Society score reached 95, prompting removal of internal fixation. At the 6-year follow-up, reduction remained well maintained, with the Böhler angle preserved at 22°.
The combination of Traditional Chinese manual bone-setting and percutaneous screw fixation achieved satisfactory functional reduction for comminuted calcaneal fractures.
Core Tip: This case report presents a sequential, stepwise manual reduction technique for comminuted calcaneal fractures, incorporating three standardized maneuvers, leverage, traction, and compression, prior to minimally invasive cannulated screw fixation. The Böhler angle was restored from 0° to 22°, with concurrent correction of calcaneal width. This minimally invasive technique uses small incisions, avoiding costly reduction devices or implants. At the 6-year follow-up, reduction was well maintained without loss of the Böhler angle. Thus, this approach with minimal equipment requirements provides a cost-effective surgical option, having significant potential for widespread adoption in resource-limited healthcare settings.
- Citation: Huang HC, Che YF, Sun H, Xu YS, Gao HY, Tang XS. Traditional Chinese bone-setting combined with percutaneous screw fixation for comminuted calcaneal fractures: A case report and review of literature. World J Orthop 2025; 16(11): 111052
- URL: https://www.wjgnet.com/2218-5836/full/v16/i11/111052.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i11.111052
Calcaneal fractures, typically caused by high-energy trauma, are among the most challenging injuries in orthopedic practice due to the calcaneus’s intricate anatomy and essential role in weight-bearing[1]. The standard surgical treatment, open reduction and internal fixation (ORIF) via an extended lateral “L-shaped” incision, offers excellent exposure and enables direct visualization for fracture reduction. However, this approach is associated with a high rate of postoperative soft tissue complications[2]. As an alternative, the sinus tarsi approach (STA) uses a 4-5 cm oblique incision extending from the fibular tip to the base of the fourth metatarsal. While less invasive, this technique provides limited visualization, complicating the restoration of calcaneal height and width. Additionally, the STA increases technical difficulty and carries a risk of peroneal nerve injury and peroneal tendonitis due to restricted access to the posterolateral aspect of the calcaneus[3].
The various percutaneous fixation methods, such as the Ilizarov frame, external fixator, Kirschner wires, or cannulated screws, each have advantages and disadvantages for the treatment of calcaneal fractures. The Ilizarov external fixator, for example, performs exceptionally well in treating complex fractures, particularly in cases with severe soft tissue damage[4]; however, its bulky structure and exposed pin tracts can inconvenience postoperative care, and long-term wear may lead to complications such as pin tract infections[5]. Additionally, the Ilizarov external fixator remains suboptimal for treatment of calcaneal fractures due to the bone’s complex anatomy and weight-bearing characteristics[6].
In contrast, Kirschner wires and cannulated screws have also demonstrated favorable outcomes in certain scenarios. For Sanders type III calcaneal fractures, the combination of Kirschner wires with absorbable screws has been shown to effectively improve foot function and reduce postoperative complications[7]. Moreover, in calcaneal fracture treatment Kirschner wires have been shown to provide good functional recovery with lower rates of soft tissue complications[8], although their fixation strength may be inferior to that of cannulated screws in some cases[9].
Cannulated screws also offer unique advantages in the management of calcaneal fractures. For example, in practice, accuracy of their placement has been improved by robot-assisted technology, further reducing postoperative complications and improving functional outcome scores[10,11]. With advancements in minimally invasive surgical techniques, their application in the management of calcaneal fractures has steadily increased. Compared to traditional ORIF, minimally invasive approaches offer several advantages, including reduced surgical trauma, faster recovery, and lower medical costs[12]. The traditional Chinese bone-setting technique represents a novel, minimally invasive strategy for treating comminuted calcaneal fractures. By integrating traditional bone-setting principles with cannulated screw fixation, this method minimizes soft tissue injury while achieving satisfactory functional reduction.
A 60-year-old woman presented to the orthopedic clinic with swelling, pain, and restricted movement of the left heel, approximately 4 hours after a fall.
The patient experienced acute left heel pain, swelling, and restricted mobility immediately following an accidental fall at home, which had occurred approximately 4 hours prior to presentation. An initial X-ray at an outside hospital revealed a comminuted fracture of the left calcaneus, prompting referral to the emergency department at our institution for further evaluation.
The patient had undergone a myomectomy for uterine fibroids 8 years prior without any subsequent gynecological complications. She had no history of chronic medical conditions, metabolic bone disorders, nor previous traumatic injuries.
The patient denied any personal or family history of genetic disorders, metabolic bone diseases, or heritable musculoskeletal conditions.
The left heel exhibited localized tenderness, significant swelling and restricted mobility. No palpable bone crepitus was noted. Axial percussion pain of the left lower extremity elicited pain, rendering the patient unable to stand or ambulate. The dorsalis pedis pulse was palpable, with intact distal perfusion, normal skin temperature, and preserved sensation and motor function in the toes. Physiological reflexes were present, and no pathological reflexes were observed.
Preoperative evaluation was unremarkable. Complete blood count, metabolic panel, and coagulation profile were all within normal physiological ranges.
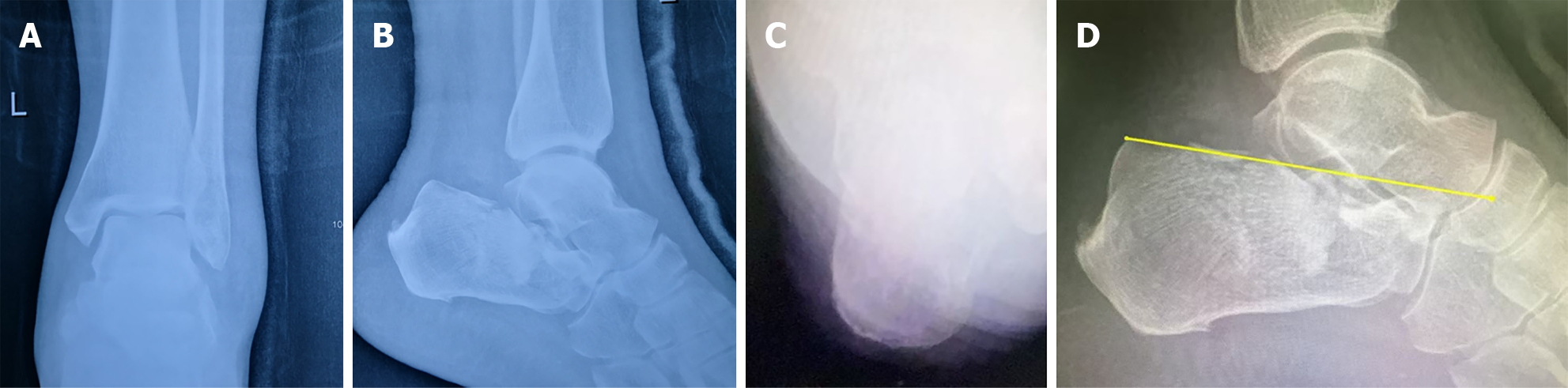
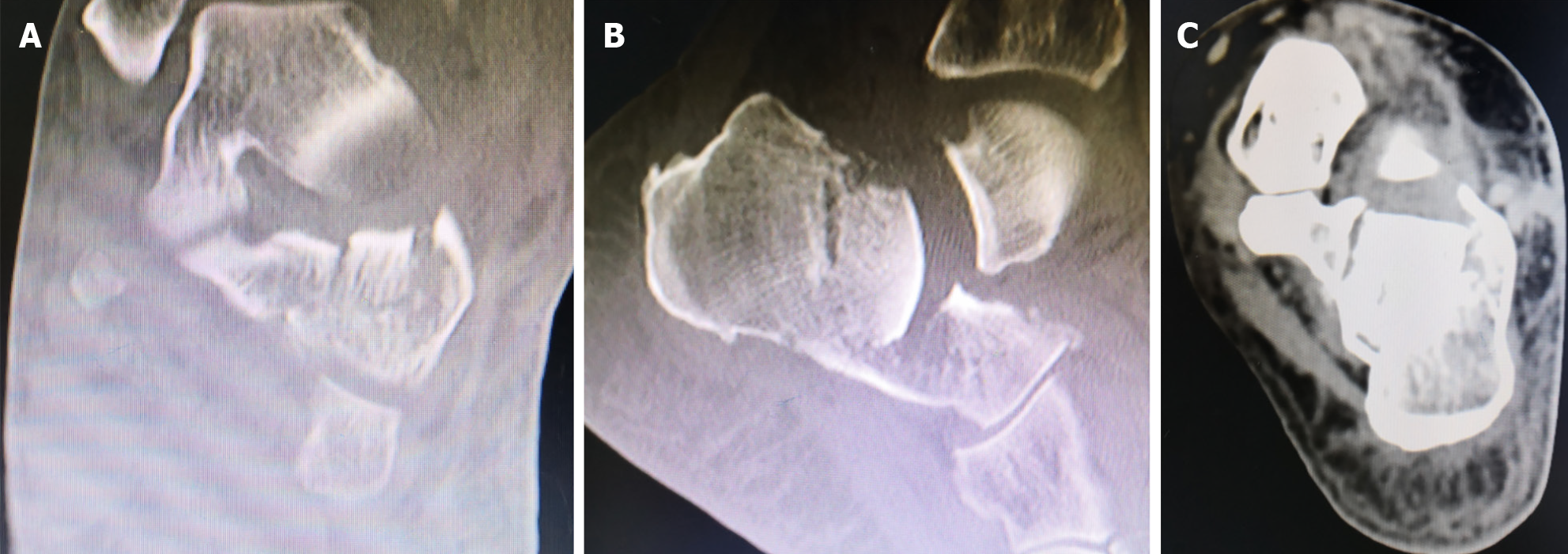
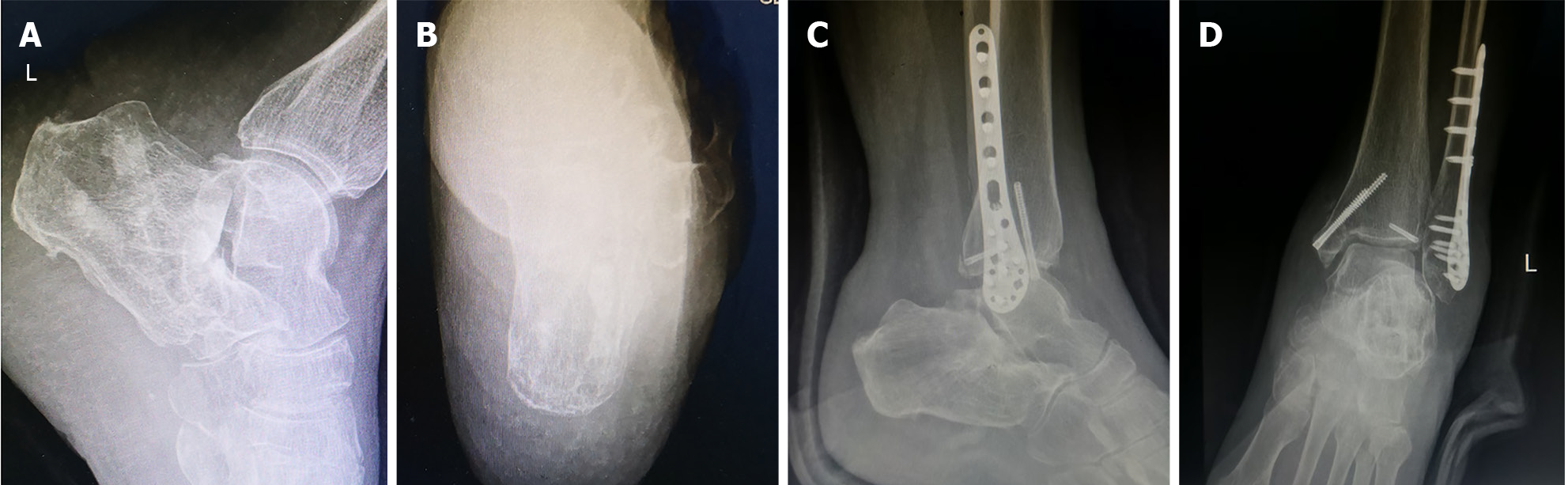
Radiographs and computed tomography (CT) scans confirmed a Sanders type IV comminuted fracture of the left calcaneus, characterized by a Böhler angle of 0° of and mild calcaneal widening (Figures 1 and 2).
Left comminuted calcaneal fracture (Sanders type IV).
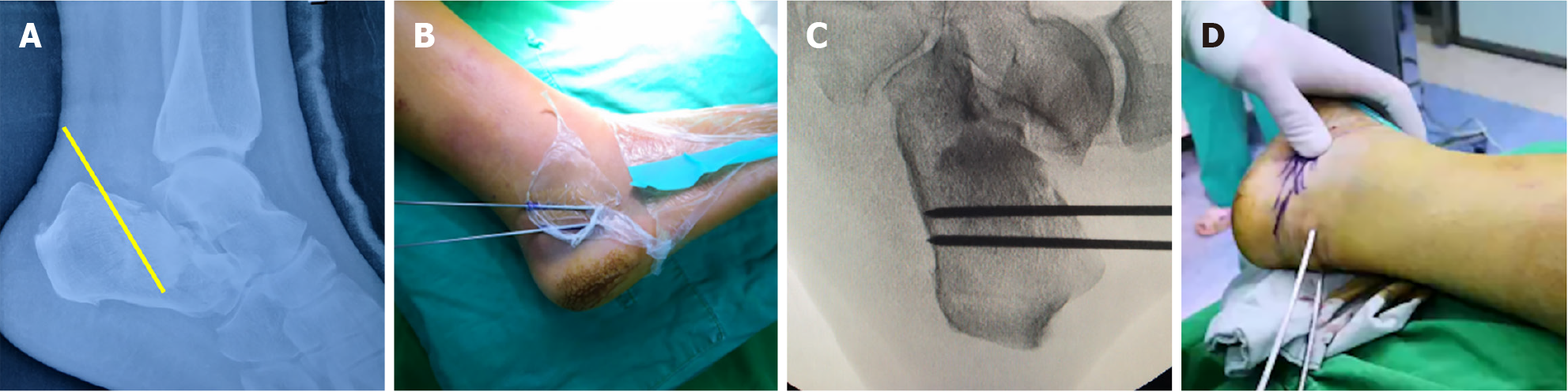
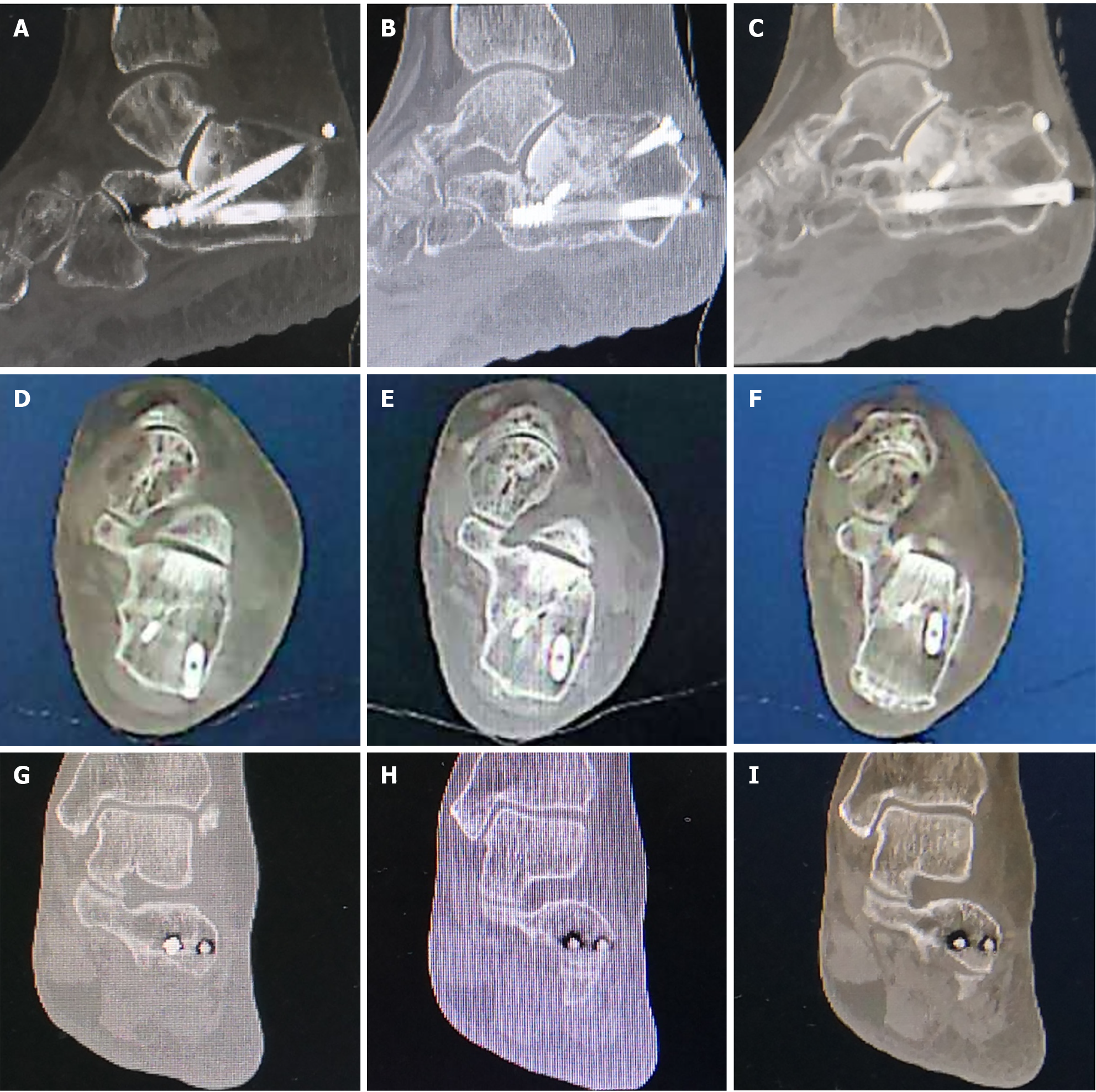
Upon admission, the patient received local ice application. Surgical intervention was performed on the second day after completion of the routine preoperative examinations and without waiting for local swelling to subside. Preoperative X-ray and CT scans were obtained to evaluate the displacement pattern of the calcaneal fracture to guide planning of the reduction strategy; the entry point, angle, and depth of the prying pin were considered (Figure 3A). A three-person team was organized for the procedure, composed of two assistants who were responsible for traction and the chief surgeon who performed the reduction; in performance of the procedure, all three members coordinated closely. Following successful spinal anesthesia, a tourniquet was applied to the thigh, and the patient was positioned in the right lateral decubitus position. The calcaneus was placed beyond the edge of the operating table to facilitate both manual reduction and intraoperative fluoroscopy.
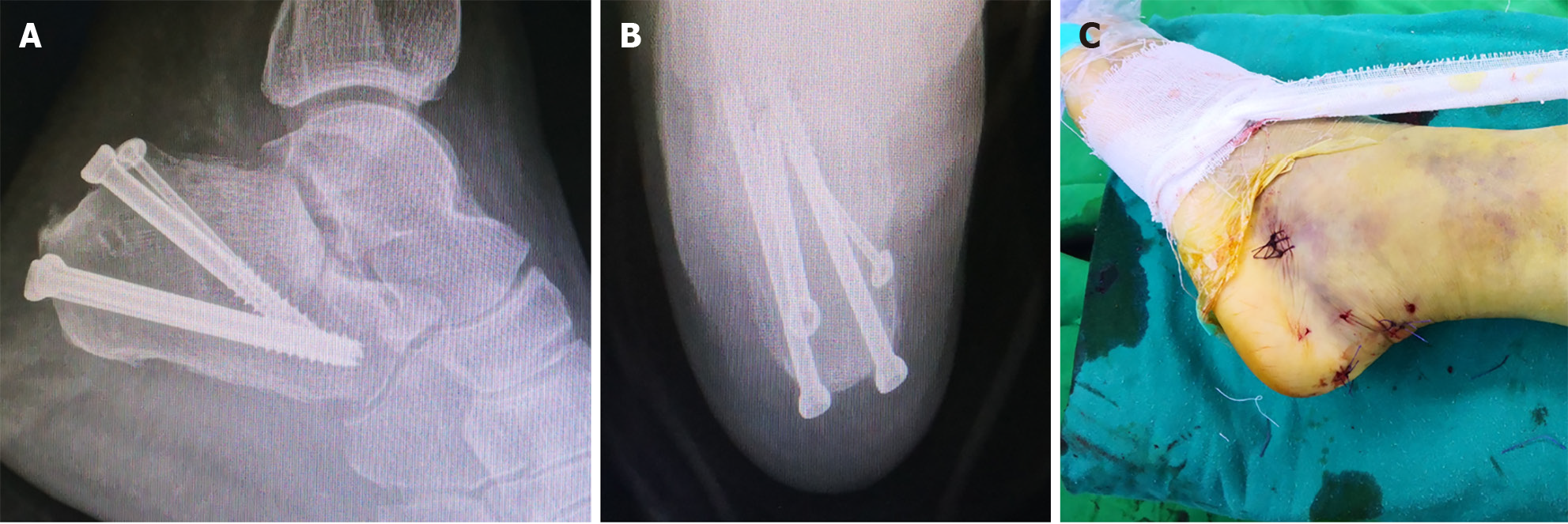
Step 1 (levering): The lateral view on X-ray and CT demonstrated approximately 1 cm of posterior-inferior depression of the posterior talar articular surface at an angle of roughly 40 degrees. Initially, two 2.0 mm Kirschner wires were placed superficially to simulate the intended trajectory and insertion depth. After confirmation of satisfactory positioning under fluoroscopy, two 3.0 mm Steinmann pins were inserted approximately 1.5 cm apart from the anterior margin of the calcaneal tuberosity, guided by the optimized Kirschner wire alignment (Figure 3B and C). The pins were then advanced to the deepest point of the depressed fracture fragment (Figure 3A), corresponding to the area of increased bone density seen on the preoperative X-ray imaging of the compressed calcaneal body (Figure 3D).
The chief surgeon firmly grasped the proximal ends of both Steinmann pins with the right hand and applied posterior-inferior pressure while simultaneously palpating the depressed area of the lateral calcaneal wall with the left thumb. Following the strategy determined in preoperative planning, approximately 40° of inferior-directed pressure was then applied to the proximal pin ends, utilizing the lever principle to elevate the compressed posterior talar articular fragment. During this maneuver, the chief surgeon’s left thumb was able to determine both the gritty sensation of disimpaction and the separation of impacted fracture fragments, indicative of successful reduction. Fluoroscopic confirmation of Böhler angle restoration was then obtained. Of note, during the prying reduction technique the Steinmann pins must reach slightly below the base of the depressed bone fragment. The pin length should not extend beyond the fracture line into the collapsed articular surface, as this would compromise the levering effect and prevent successful reduction.
Step 2 (traction): The chief surgeon and two assistants coordinated simultaneous traction for reduction. Two 3.0 mm Steinmann pins were transversed through the distal fracture fragment, initiating laterally at the posteroinferior aspect of the calcaneal body (Figure 4A). One assistant applied inferoposterior traction through the Steinmann pins while simultaneously performing eversion reduction according to the predetermined displacement pattern. The other assistant maintained counter-traction by firmly grasping the lower leg with both hands. The chief surgeon, while maintaining continuous traction by flexing and pulling the mid-forefoot with both hands, used the thumbs to apply downward pressure on the proximal calcaneus, restoring the calcaneocuboid joint alignment. Throughout this step, the chief surgeon’s thumb remained in close contact with the fracture site to monitor the separation of fracture fragments tactilely during reduction.
Step 3 (compression): The chief surgeon placed both thumbs on the lateral aspect of the calcaneus while positioning the remaining fingers medially. Using the sustentaculum tali as a fixed fulcrum, the surgeon applied opposing forces - pressing the markedly expanded lateral wall medially with the thumbs while countering with medial support. This step can restore the calcaneal width through controlled medial compression of the displaced lateral fragment.
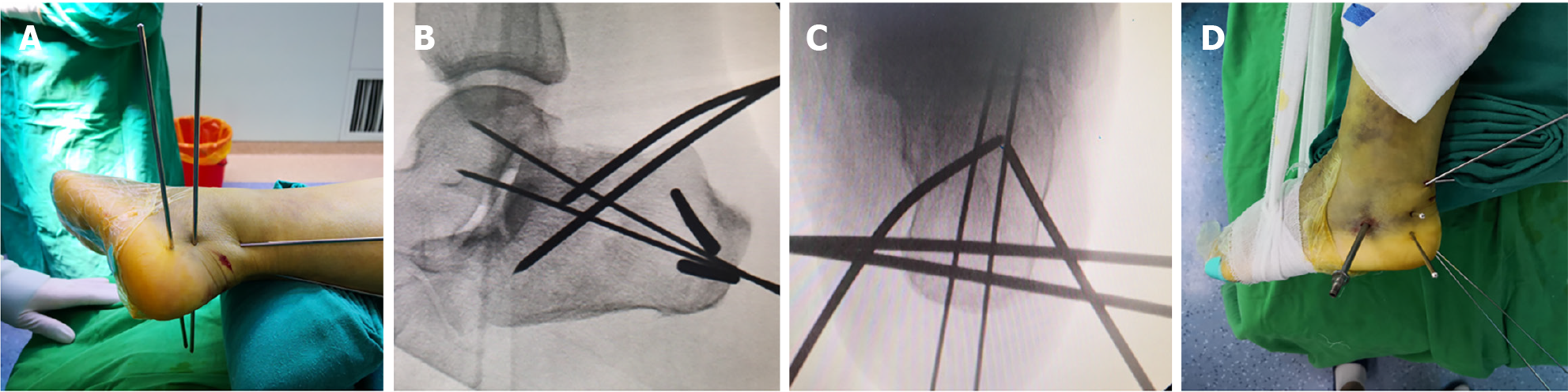
Satisfactory fluoroscopic confirmation includes the following: (1) Böhler’s angle restoration (25°-40°); (2) Intact lateral wall of calcaneus; (3) Proper talocalcaneal joint alignment (100°-145° between articular surfaces); and (4) Acceptable calcaneal dimensional restoration (within 2-3 mm in width/height/Length), achieved upon two 2.5 mm guide wires being drilled from the posterior aspect of the calcaneus first, carefully avoiding the Achilles tendon insertion (Figure 4B-D). For the full fixation, three 6.5 mm and one 4.5 mm cannulated and partially threaded compression screws were inserted, under fluoroscopic guidance, over the appropriately positioned guide wires to achieve compression fixation of the lateral fracture fragments. Meticulous attention was paid to prevent articular penetration. Prior to guide wire removal, final fluoroscopic verification of satisfactory screw positioning was obtained (Figure 5A and B, Video).
Following the screw placement, fluoroscopic examination revealed a significant residual gap (approximately 1.5 cm × 1.5 cm) in the posteroinferior aspect of the calcaneal tuber angle after reduction. An 0.5 cm incision was made subsequently at the corresponding anatomical location, through which an allogeneic bone graft was implanted.
The wound was sutured routinely, disinfected, and dressed (Figure 5C), with the ankle immobilized in 110° plantar flexion using an anterior plaster splint. Routine prophylactic antibiotics were administered for 24 hours postoperatively. On postoperative day 2, the patient was allowed to walk with crutches, maintaining non-weight-bearing status, and lower limb muscle exercises were initiated to prevent muscle atrophy. At 1 month postoperatively, the splint was removed and ankle flexion-extension exercises were initiated. At 2 months postoperatively, toe-standing exercises were introduced to prevent osteoporosis, and the patient was permitted to begin partial weight-bearing walking. Full weight-bearing walking was allowed at 6 weeks postoperatively.
The total surgical duration, from skin incision to wound closure, was approximately 2 hours and required several mini-incisions only, resulting in minimal blood loss (5 mL). The wounds healed well and without incidence. The Visual Analog Scale score showed a decreasing trend, from 5 on postoperative day 1 to 3 by postoperative day 3. The American Orthopaedic Foot and Ankle Society score showed improvement, from 73 at 6 weeks postoperatively to 90 at 3 months postoperatively. During the postoperative period, the patient reported only mild pain, experienced during time without support, and a slight gait disturbance. Radiographic evaluation via X-ray and CT demonstrated maintenance of good alignment, indicating the appropriateness of full-return to normal daily activities, including walking, stair climbing, and squatting. A follow-up CT scan at 7 months postoperatively demonstrated excellent fracture healing; consequently, the screws were removed (Figure 6).
A comparison of preoperative (Figure 2) and 7-month postoperative CT scans (Figure 7) indicated that the patient’s Sanders type IV calcaneal fracture met functional reduction criteria. The height, width, and length of the calcaneus were restored to near-normal parameters, with the Böhler’s angle corrected to 22°. The subtalar joint surface exhibited a step-off of less than 2 mm, and the integrity of the lateral wall was maintained.
Longitudinal evaluation at the 6-year follow-up demonstrated maintenance of the clinical outcomes. The patient exhibiting no symptoms and enjoyed full functional capacity (American Orthopaedic Foot and Ankle Society score of 95) until an incidental traumatic event precipitated a lateral malleolar fracture requiring surgical intervention. Notably, postoperative imaging surveillance revealed preservation of the calcaneal reduction (Böhler angle of 22°), confirming the durability of the initial fracture reduction despite subsequent unrelated trauma (Figure 6).
Comminuted calcaneal fractures are common yet complex injuries that pose significant challenges in management. Treatment options include both conservative and surgical approaches, each with its own indications and limitations. However, regardless of the chosen method, complications may still occur. Conservative treatment is generally ap
Surgical treatment includes a range of approaches, such as ORIF, minimally invasive surgery (MIS), and percutaneous fixation. The main advantage of surgical intervention is its ability to achieve more precise anatomical restoration of the calcaneus, which is often associated with improved functional outcomes[14]. However, surgical management carries inherent risks, including infection, impaired wound healing, and postoperative pain[15,16]. These risks are particularly pronounced in ORIF procedures, where extensive surgical exposure significantly increases the likelihood of postoperative complications, especially infection[16]. MIS offers several advantages, including reduced soft tissue damage, preservation of blood supply, shorter operative time, and relatively lower rates of postoperative complications[17]. However, in cases of severely comminuted fractures, MIS may provide inadequate stability and less precise fracture reduction, which can increase the risk of postoperative complications and compromise long-term outcomes[18].
Locking nail fixation performed through MIS represents an effective treatment strategy for calcaneal fractures. Studies have shown that this method can successfully restore subtalar joint alignment and calcaneal angles while preserving the benefits of minimal soft tissue disruption[19]. Additionally, Calcanail®-assisted MIS fixation or subtalar arthrodesis has demonstrated particular efficacy in patients at high risk of postoperative soft tissue complications[20].
Another minimally invasive technique involves the use of a limited STA with Kirschner wire fixation and bone grafting, which has shown excellent outcomes in pediatric patients. This approach enables satisfactory reduction of the articular surface while providing stable fixation. Notably, studies have reported no occurrences of infection nor tissue necrosis[21].
Limited ORIF has also demonstrated favorable outcomes in the management of calcaneal fractures. Studies suggest that this approach provides good functional recovery with a low incidence of complications, particularly in patients with Sanders type III fractures[22]. It enables effective restoration of calcaneal geometry while significantly reducing the risk of wound infections compared to more extensive surgical exposures[23].
External fixators provide favorable clinical and radiographic outcomes in the treatment of complex intra-articular calcaneal fractures. Studies have demonstrated that external fixation achieves results comparable to internal fixation techniques while reducing soft tissue complications significantly[24]. Furthermore, research has highlighted that minimally invasive external fixation assisted by a Limb Reconstruction System excels in restoring calcaneal morphology and articular surface alignment, with fewer complications. This technique is particularly suitable for most type II and III calcaneal fractures, though not recommended for comminuted fractures of the calcaneal tuberosity[25]. For high-energy open fractures or cases with severe soft tissue damage, staged external fixation combined with delayed ORIF and subtalar arthrodesis addresses both skeletal and soft tissue challenges effectively, yielding satisfactory pain relief and functional recovery postoperatively[26]. However, while external fixation offers certain advantages in managing comminuted calcaneal fractures, its postoperative complication rates remain a clinical concern. Pin tract infections are particularly common and troublesome; moreover, the use of external fixators may also restrict patient mobility, which could impact quality of life and hinder rehabilitation progress[27,28].
In recent years, advancements in medical technology and greater focus on patient-centered care have led to increased recognition of manual reduction techniques for displaced fractures. This approach offers key advantages, including minimized surgical trauma and a lower risk of postoperative complications[29]. The most substantive essence of manual reduction is its capacity to achieve functional reduction of fractures through non-invasive methods, thereby minimizing surgery-related risks and complications[30,31].
Traditional Chinese medicine is gaining global recognition for its holistic approach to health and its integration with modern medical practices. Traditional Chinese bone-setting techniques have a long history and demonstrated efficacy in conservative fracture management. However, their broader adoption has been limited by a lack of standardized protocols and few reported cases. In recent years, research interest has grown in exploring the clinical applications of traditional Chinese medicine bone-setting reduction in fracture treatment[32-34].
This bone-setting reduction technique has been applied successfully in numerous cases of comminuted calcaneal fractures. Unfortunately, incomplete case data documentation has limited reporting to case series format. Subsequent rigorous randomized controlled trials should be conducted to systematically validate the reliability and reproducibility of traditional Chinese bone-setting reduction techniques. The “three-step standardized protocol” based on traditional Chinese bone-setting theory emphasizes personalized treatment, recognizing that each patient’s fracture requires unique reduction forces and directional adjustments.
Whether bone grafting is necessary during calcaneal fracture surgery remains a topic of debate. The most current studies have shown that while bone defects commonly occur after calcaneal fractures, whether these defects require grafting remains controversial. Research has indicated, however, that most postoperative bone defects improve spontaneously without grafting[35], suggesting that bone grafting may not be essential for all cases. In the treatment of calcaneal fractures, the volume of bone defects decreases significantly within 1 year postoperatively, with an average reduction of 77%[35]. This indicates a natural healing tendency, and residual defects show no significant correlation with clinical or radiographic outcomes. Therefore, bone grafting may not be a mandatory step, especially when defects can heal independently. It is important to note however that while grafting may not be universally required, it may still offer benefits in certain scenarios; for instance, in cases of severe bone loss or poor healing potential, grafting may accelerate recovery and improve functional outcomes[36]. In our case fluoroscopy revealed a substantial gap between fracture fragments after reduction. Considering that filling the defect might promote faster healing and enable earlier weight-bearing, allogeneic bone grafting was performed.
This approach offers significant minimally invasive advantages, requiring only a few 5-mm incisions, making it especially suitable for high-risk patients, such as the elderly, pediatric populations, or those with compromised skin integrity, who benefit particularly from reduced surgical trauma. Compared to ORIF, it eliminates the need for extensive surgical exposure, thereby lowering the risk of wound complications and allowing for earlier rehabilitation. Economically, the procedure relies solely on K-wires and a minimal number of screws, significantly reducing implant costs. The success of this technique, however, is highly dependent on achieving satisfactory reduction. To master this manual reduction technique, the surgeon must carefully analyze the fracture pattern first and then develop a reduction plan pre-surgery. Based on intraoperative fluoroscopy, they will need to construct a three-dimensional mental image to guide their assistant’s coordination. Simultaneously, the surgeon must accumulate experience through treatment of multiple cases, developing an intuitive sense of reduction. Only through such practice can they achieve successful reduction in fewer attempts, ideally accomplishing it in one step. Otherwise, excessive attempts may increase radiation exposure, and repeated prying maneuvers could cause further comminution of fracture fragments.
This article introduces an innovative reduction technique for comminuted calcaneal fractures and systematically standardizes its operation steps and reduction criteria. Once satisfactory reduction is confirmed under fluoroscopic guidance, fracture fixation can be completed using only percutaneous screw placement. Clinical practice has demonstrated that this technique offers clear minimally invasive advantages, including reduced intraoperative blood loss.
The combination of traditional Chinese bone-setting and percutaneous screw fixation for comminuted calcaneal fractures achieves satisfactory functional reduction. Emphasizing reduced surgical trauma, this technique holds considerable promise for broader adoption, especially in resource-limited settings or among high-risk patient populations.
| 1. | Xiao J, Xin Z, Fu X, Huang J, Zhang B, Yu H. Treatment of Fracture of the Calcaneus via Bone Axial X-Ray Image-Based Minimally Invasive Approach. Comput Math Methods Med. 2022;2022:3012589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Bin Y, Xingguo Z, Hua L, Decheng W. Clinical comparison of modified sinus tarsi approach and L-shaped approach in open reduction and internal fixation for Sanders typeIII-IV intra-articular calcaneal fractures: Complications, security, effectiveness analysis. J Orthop Sci. 2025;S0949-2658(25)00042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Nosewicz TL, Dingemans SA, Backes M, Luitse JSK, Goslings JC, Schepers T. A systematic review and meta-analysis of the sinus tarsi and extended lateral approach in the operative treatment of displaced intra-articular calcaneal fractures. Foot Ankle Surg. 2019;25:580-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Zhang Q, Rehemutula A, Maitudi M, Yang Q, Yalikun A, Zhou H, Si Y, Chen Z, Liu D, Li Q, Liu T, Li L, Yusufu A. Surgical treatment of infectious severe calcaneal bone defects in children by the Ilizarov technique. Injury. 2025;56:112224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Khan MS, Rashid H, Umer M, Qadir I, Hafeez K, Iqbal A. Salvage of infected non-union of the tibia with an Ilizarov ring fixator. J Orthop Surg (Hong Kong). 2015;23:52-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Morasiewicz P, Pelc M, Tomczyk Ł, Kochanska-Bieri J, Bobiński A, Pili D, Reichert P. Clinical and radiological assessment of the Polish modification of the Ilizarov external fixator for the treatment of intra-articular calcaneal fractures. Adv Clin Exp Med. 2025;34:1321-1329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Zeng G, Xie Q, Cai L, Mai H, Zhang L, Liang X, Huang Z, Su B. Arthroscopy-assisted absorbable screw combined with Kirschner wire internal fixation for Sanders type III displaced intra-articular calcaneal fractures: a retrospective study. BMC Musculoskelet Disord. 2025;26:181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Mesregah MK, Shams A, Gamal O, Zaki EM. Clinical and Radiological Outcomes of Minimally Invasive Reduction and Percutaneous K-wire Fixation for Intra-articular Calcaneal Fractures. Orthopedics. 2020;43:97-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | El-Azab H, Ahmed KFE, Khalefa AH, Marzouk AR. A prospective comparative study between percutaneous cannulated screws and Kirschner wires in treatment of displaced intra-articular calcaneal fractures. Int Orthop. 2022;46:2667-2683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Cao ZY, Cui BH, Wang F, Zhou XG, Zhao FF. Robot-assisted internal fixation of calcaneal fractures versus conventional open reduction internal fixation: a systematic review and meta-analysis. J Robot Surg. 2024;18:329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Wang J, Han W, Su Y, Wang J, Jiang X. Comparison of Robot-Assisted Percutaneous Cannulated Screws Versus Open Reduction and Internal Fixation in Calcaneal Fractures. Orthop Surg. 2023;15:724-730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 12. | Miao K, Wang J, Yu K, Hong J, Lu X. Percutaneous reduction and cannulated screw fixation assisted by 3D printing technology of calcaneal fractures in children. J Orthop Sci. 2024;29:236-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Han X, Zhang Y, Zhang X, Tan J. Comprehensive comparison between conservative therapy and surgical management for completely displaced and comminuted mid-shaft clavicle fractures. Int Orthop. 2024;48:1871-1877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Nia A, Hajdu S, Sarahrudi K, Widhalm HK, Popp D, Schmoelz L, Doering K, Tiefenboeck T. Surgical Treatment of Calcaneal Fractures by Minimally Invasive Technique Using a 2-Point Distractor Versus ORIF and Conservative Therapy-A Retrospective Multicenter Study. J Clin Med. 2025;14:2015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Hu JS, Huang CB, Mao SM, Fang KH, Wu ZY, Zhao YM. Development of a nomogram to predict surgical site infection after closed comminuted calcaneal fracture. BMC Surg. 2022;22:313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 16. | Yu X, Pang QJ, Chen L, Yang CC, Chen XJ. Postoperative complications after closed calcaneus fracture treated by open reduction and internal fixation: a review. J Int Med Res. 2014;42:17-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Wilkinson BG, Marsh JL. Minimally Invasive Treatment of Displaced Intra-Articular Calcaneal Fractures. Orthop Clin North Am. 2020;51:325-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Malik C, Najefi AA, Patel A, Vris A, Malagelada F, Parker L, Heidari N, Jeyaseelan L. Percutaneous subtalar joint screw fixation of comminuted calcaneal fractures: a salvage procedure. Eur J Trauma Emerg Surg. 2022;48:4043-4051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 19. | Fascione F, Di Mauro M, Guelfi M, Malagelada F, Pantalone A, Salini V. Surgical treatment of displaced intraarticular calcaneal fractures by a minimally invasive technique using a locking nail: A preliminary study. Foot Ankle Surg. 2019;25:679-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Saß M, Rotter R, Mittlmeier T. Minimally invasive internal fixation of calcaneal fractures or subtalar joint arthrodesis using the Calcanail®. Oper Orthop Traumatol. 2019;31:149-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Wan J, Feng J, Li F, Xu J, Li MJ, Hu T. Therapeutic Advantages of Internal Fixation with Kirschner Wire and Bone Grafting via Limited Tarsal Sinus Incision Approach for Displaced Intra-Articular Calcaneal Fractures of Children. Med Sci Monit. 2018;24:7862-7868. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Bremer AK, Kraler L, Frauchiger L, Krause FG, Weber M. Limited Open Reduction and Internal Fixation of Calcaneal Fractures. Foot Ankle Int. 2020;41:57-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Chen J, Yang Z, Kong C, Wei S. Minimally invasive dual incision with mini plate internal fixation improves outcomes over 30 months in 20 patients with Sanders type III calcaneal fractures. J Orthop Surg Res. 2020;15:167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Checa-Betegón P, Valle-Cruz J, Llanos-Sanz S, Miguel-Miguel C, Sánchez-Del-Saz J, García-Coiradas J. External fixation in intra-articular fractures of the calcaneus: Is it a valid option as definitive treatment? Eur J Orthop Surg Traumatol. 2024;34:201-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 25. | Jiang G, Li J, Zhang X, Shu S, Ma Y, Zhang P, Wang G, Liao H, Hu J. Limb Reconstruction System Assisted Reduction and Internal Fixation for Intra-Articular Calcaneal Fractures: A New Application. Orthop Surg. 2023;15:2540-2548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 26. | Neumaier M, Kohring J, Ciufo D, Ketz JP. Technique and Early Outcomes for High-Energy Calcaneus Fractures Treated With Staged External Fixation to Combined Open Reduction Internal Fixation and Subtalar Arthrodesis. J Orthop Trauma. 2022;36:e412-e417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 27. | Li Y, Bao RH, Jiang ZQ, Wu HY. Complications in operative fixation of calcaneal fractures. Pak J Med Sci. 2016;32:857-862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 28. | Fu TH, Liu HC, Su YS, Wang CJ. Treatment of displaced intra-articular calcaneal fractures with combined transarticular external fixation and minimal internal fixation. Foot Ankle Int. 2013;34:91-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Shah MM, Gupta G, Rabbi Q, Bohra V, Wang KK. Close Reduction Technique for Severely Displaced Radial Neck Fractures in Children. Indian J Orthop. 2021;55:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Karantana A, Handoll HH, Sabouni A. Percutaneous pinning for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2020;2:CD006080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 31. | Krul M, van der Wouden JC, Kruithof EJ, van Suijlekom-Smit LW, Koes BW. Manipulative interventions for reducing pulled elbow in young children. Cochrane Database Syst Rev. 2017;7:CD007759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Liu T, Xia Y, Zhang Y, Kuang G, Zhou L. Acupuncture combined with TCM bonesetting in the treatment of distal radius fractures: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e28279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 33. | Wang B, Yin X, Zhang P, Yang K, Sun W, Jin Z, Li J, Gao C, Gao J. Effect of traditional Chinese manipulation on ankle sprains: A systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e24065. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Ziebarth K, Slongo T. [Pediatric traumatology: closed or minimally invasive reduction technique for upper and lower limb fractures]. Oper Orthop Traumatol. 2025;37:184-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 35. | Park YH, Cho HW, Choi JW, Choi GW, Kim HJ. Bone Defects After Surgery for Displaced Intraarticular Calcaneal Fractures Spontaneously Improve Without Bone Grafting. Clin Orthop Relat Res. 2021;479:1265-1272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Li Z, Chen W, Su Y, Zhang Q, Hou Z, Pan J, Zhang Y. The application of closed reduction internal fixation and iliac bone block grafting in the treatment of acute displaced femoral neck fractures. PLoS One. 2013;8:e75479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/