Published online Nov 18, 2025. doi: 10.5312/wjo.v16.i11.110465
Revised: June 25, 2025
Accepted: September 19, 2025
Published online: November 18, 2025
Processing time: 160 Days and 22.4 Hours
The Ilizarov apparatus was designed by its author 75 years ago and addresses a wide range of orthopedic conditions. Its classical assemblies are still self-sufficient and versatile. However, certain clinical scenarios require a more specialized approach, and some groups of patients may benefit from customized Ilizarov constructs. Engineering science has designed various external fixators for ortho
Core Tip: The Ilizarov apparatus was designed 75 years ago and addresses a wide range of orthopedic conditions. Its classical assemblies are still self-sufficient. However, certain clinical scenarios require a more specialized approach, and some groups of patients benefit from customized or modified Ilizarov constructs. They are half-pin hexapod or hybrid fixators for gradual deformity correction, and compression-distraction fixators for definite limb segments. Special devices were developed for moving the split fragment for tibial revascularization. The external frames for the foot and hand were modified to consider their complex anatomy and implement lengthening, correction of multi-plane deformities, and web-space soft-tissue growing.
- Citation: Sutyagin I, Malkova TA. Impact of the Ilizarov apparatus on external fixation: Current modifications of the 75-year-old orthopedic tool. World J Orthop 2025; 16(11): 110465
- URL: https://www.wjgnet.com/2218-5836/full/v16/i11/110465.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i11.110465
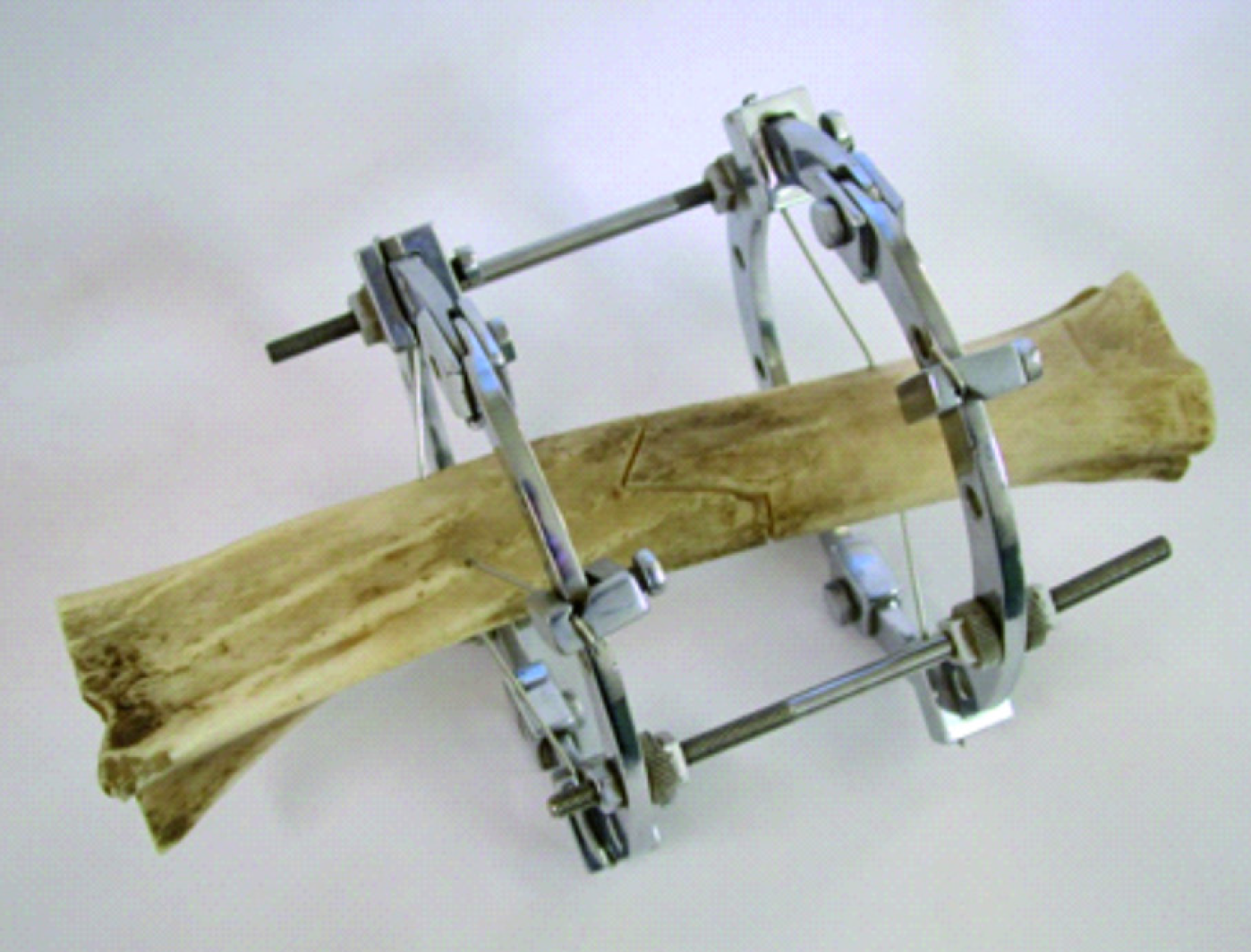
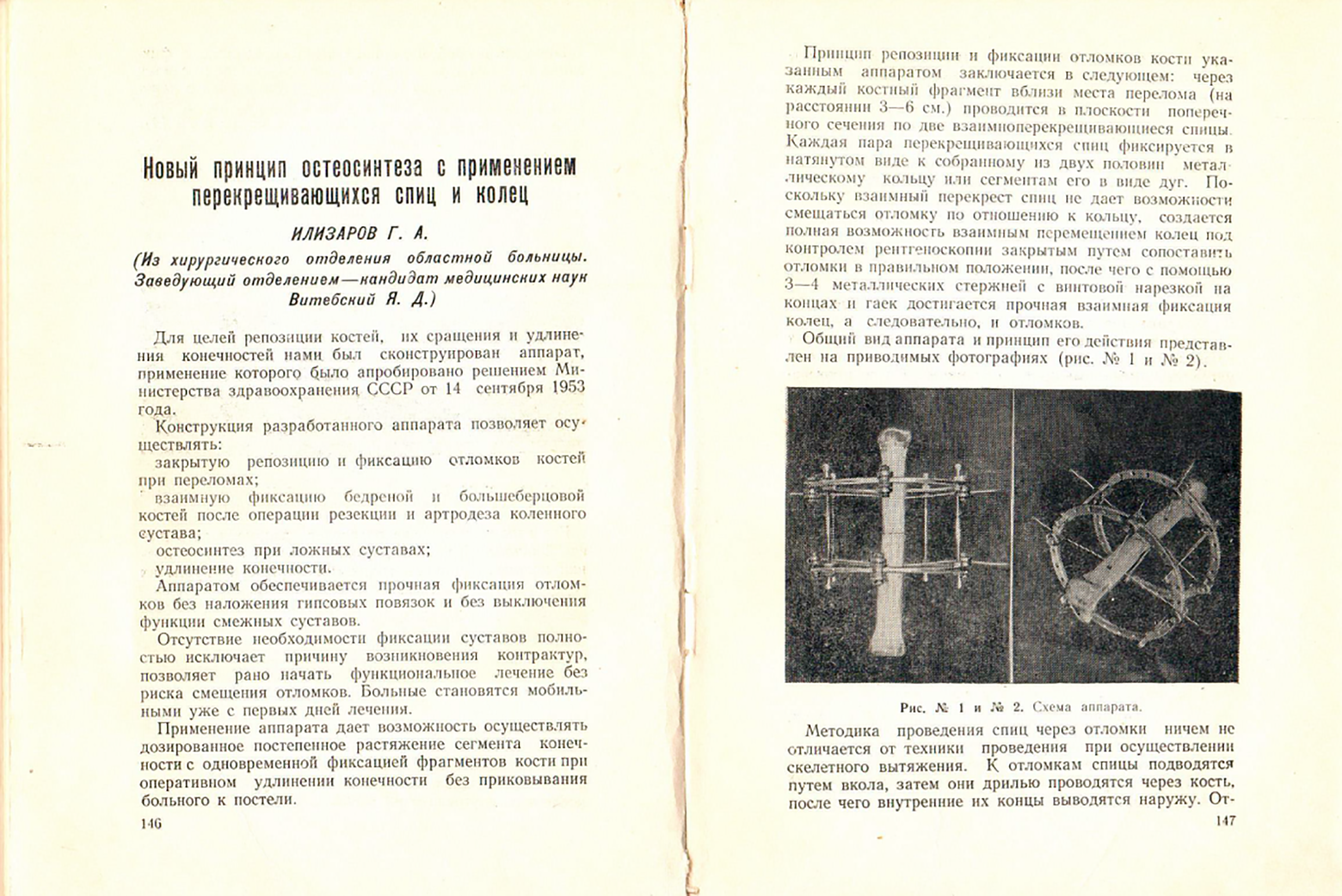
The Ilizarov apparatus or the Ilizarov circular (ring) external fixator is almost 75 years old and is still one of the most popular tools currently employed by orthopedic surgeons for bone reconstruction worldwide[1,2]. It was designed by its author, Gavriil Ilizarov, in 1951 and was claimed for patenting in Russia in June 1952 (Figure 1). The first presentation of the outcomes in 43 patients treated in 1951-1953 with the original version of the apparatus for several orthopedic conditions including bone lengthening, nonunion and delayed consolidation was published in the collected works on medical studies of the Kurgan regional scientific medical society in 1954 (Figure 2).
Since then, the design of the Ilizarov fixator has changed greatly as the solutions of orthopedic problems required introduction of new elements, units, hinges, connection plates and threaded parts. Currently, it is a set of stainless-steel parts (rings, half-rings, wires, posts, threaded rods, connection plates and other elements of different sizes) that can be assembled into personalized constructs to solve specific orthopedic tasks. Its established assemblies and customized frames are able to address a wide range of orthopedic conditions, the main of which are temporary and definite fixation of fractures, bone lengthening and deformity correction, management of bone defect and nonunion, both post-traumatic and infected[3].
The key biological phenomenon of the Ilizarov method technical solutions for bone healing and reconstruction is the generation of viable new bone tissue via distraction osteogenesis triggered by tension stress in the external frame applied to a limb that yields high union rates and the functional weight-bearing during the treatment process[3,4].
Professor Ilizarov GA not only developed his circular fixator for new bone formation, but also was the first to conduct research on distraction osteogenesis with his team and publish the findings both in the domestic and international journals[5-7]. In the 1980s, the phenomenon of distraction osteogenesis was deeply investigated in experimental and radiographic clinical studies and was estimated by the USSR science as a discovery on the law of tension stress[7].
The classical Ilizarov techniques and frame assemblies for different pathological conditions are still self-sufficient and versatile. However, certain clinical scenarios require a more specialized approach[8]. Some groups of patients may benefit from customized Ilizarov constructs, especially in such conditions as bone deformities in the foot, hand, pelvis and lower/upper limbs in several systemic or congenital diseases such as osteogenesis imperfecta, achondroplasia or tibial hemimelia.
It should be clearly distinguished that the Ilizarov apparatus is a tool of the techniques applied to bone and soft tissues based on the Ilizarov principles of distraction and/or compression discovered by this outstanding orthopedic surgeon and his team in the 1970s and 1980s such as the rules of osteotomy (corticotomy) performance, distraction rates for large and small bone generation, weight-bearing and fixation rigidity. These principles are implemented by a variety of other devices and combined modifications that evolved thereafter[1,3,8].
We aimed to study the current state and novel modifications in external fixation for specific clinical situations which are based on the principles of the Ilizarov method.
We performed a comprehensive search in the available Internet platforms (PubMed, Scopus) that index medical studies to identify recent clinical studies and literature reviews on the advances of external fixation techniques and the Ilizarov method modifications using the terms “Ilizarov method”, “external fixation”, “modifications of the Ilizarov method”, “novel external fixation devices”, “bone lengthening”, “deformity correction”, ‘’bone nonunion and defects”, “mini-fixators”, “fracture repair”, “joint arthrodesis” published within the period from 2020 throughout 2024. Literature reviews and clinical full-text studies in English and Russian (including case series or reports) were screened and those that reported on advances and modifications of external fixation techniques for specific clinical scenarios (limb lengthening, deformity correction, nonunion/defects, joint arthrodesis, foot and hand pathology) or customized Ilizarov frame application were chosen. Thirty-four studies that met the criteria were included (Table 1)[8-41]. Experimental studies and literature in other languages were excluded.
| Limb lengthening and deformity correction | Bone defects and nonunion | Foot and ankle pathology | Small bone foot and hand pathology | Fracture repair | Rare application |
| Flexible intramedullary nailing + external fixation in children with metabolic bone disorders, skeletal dysplasias with compromised bone tissue development, femoral deficiency and fibular hemimelia, polyostotic fibrous dysplasia | Novel technique of three-ring Ilizarov fixator frame in gap non-union of tibia | Universal external configuration for correction of foot and ankle deformities | Enlargement of the great toe by applying transverse distraction with a mini-fixator of the original type for future finger transposition | Definitive circular external fixation for acute tibial fracture-related infection | Lengthening after limb replantation |
| Intramedullary telescopic nailing used in combination with a reduced Ilizarov frame in children with osteogenesis imperfecta | Post-traumatic infected non-union of the humerus managed by hybrid ring fixators | Calcaneal lengthening using a specialized Ilizarov external fixator assembly in posttraumatic shortening | Metacarpal lengthening for thumb reconstruction with special mini-ring fixators | Closed reduction and Ilizarov/hybrid fixator application for complex proximal tibia fractures | Modified hip reconstruction surgery |
| External fixation and extramedullary intamedullary nailing for lengthening and deformity correction in fibular hemimelia | Internal cable as a guide to transport the fragment with a unilateral fixator | Transverse tibia distraction for the treatment of diabetic foot ulcer complicated with chronic osteomyelitis | First web-space plasty with the Ilizarov mini-fixator for functional and esthetic improvement | Treatment of intra-articular calcaneal fractures with Polish modification of the Ilizarov external fixator | |
| Bone lengthening and deformity correction with Smart Taylor spatial frame | Hexapod system with a computer program for combined soft-tissue and osseous defects | Technique of hindfoot reconstruction in chronic calcaneal osteomyelitis | Ilizarov mini-fixator for the purpose of interdigital widening and elongation of the flap | ||
| Bone lengthening with motorized intramedullary nail in posttraumatic length discrepancies | Hybrid techniques (external fixators with internal implants) | Use of tibial bone transport for treatment of massively infected hindfoot defects to salvage it | Treatment of chronic Monteggia fracture-dislocations in children with Ilizarov mini-fixator | ||
| Modifications on Ilizarov fixation for flexed knee deformity and double telescope rods design for limb lengthening | Integrating three-dimensional-printed customized guides with hemicorticotomy bone transport | Closed arthrodesis in infected neuropathic ankles using Ilizarov ring fixation | |||
| Minimally invasive osteotomy and simple circular fixation for adolescent late-onset tibia vara | Transverse tibial transport in thromboangiitis obliterans and mini-transverse tibial transport | Distraction arthroplasty in the treatment of moderate-to-severe ankle arthritis | |||
| Personalized assemblies constructed from the Ilizarov apparatus sets for complex congenital deformities | |||||
| Management of complex knee deformity using Ortho-SUV |
Surgical techniques, external fixator systems, and materials for managing bone pathology have made a continuous advance[3]. The benefits of traditional external fixation have been enhanced in recent years with innovative configurations, ring and pin modifications such as carbon rings, double telescopic rods for lengthening and bioactive pin coating aimed at frame weight and infection rate reduction or bone healing acceleration[9,42]. Chinese and Indian scholars are among the leading Ilizarov philosophy followers[9-11]. They developed some special treatment methods, made many modifications to the Ilizarov external fixator, developed a number of external fixators for special purposes and published a great number of papers in the international journals being the most active researchers and users of the Ilizarov method and its modifications nowadays according to the published studies[9]. It is noteworthy, that external fixation used in China differs from the one in Russia and the Western world, especially in the instruments and techniques that are aimed to use minimum components for maximal efficiency[9].
Currently, the original techniques of bone lengthening and deformity correction have been utilized alongside with several adaptations resulting from the introduction of novel fixation tools and methods of their application, such as hexapod external fixators and motorized intramedullary lengthening nails[1,3]. Engineering science has designed various external fixators for orthopedic purposes, and some of those have become the gold standard for specific clinical tasks. The introduction of the Taylor spatial frame (TSF) in 1997 was the most remarkable change in external fixation[43]. This hexapod fixator based on the use of software is a more complex device but gained the world market of hexapod fixators that many companies develop. Its new version, the Smart TSF, was introduced in Baltimore in 2021[12]. The introduction of intramedullary lengthening nails at the beginning of the 2000s and their wide dissemination that started approximately in 2013 made external fixation more applicable for certain more complex indications[3,13]. External fixators still play an important role in tibial lengthening, especially in young children with open physis and small bone diameter that prevent insertion of a rigid nail. One of the recent advancements of internal lengthening enables to perform internal lengthening both intramedullary and extramedullary. Extramedullary internal lengthening is a new technique and was described for fibular hemimelia that uses an implantable nail attached to the bone like an internal-external fixator[14].
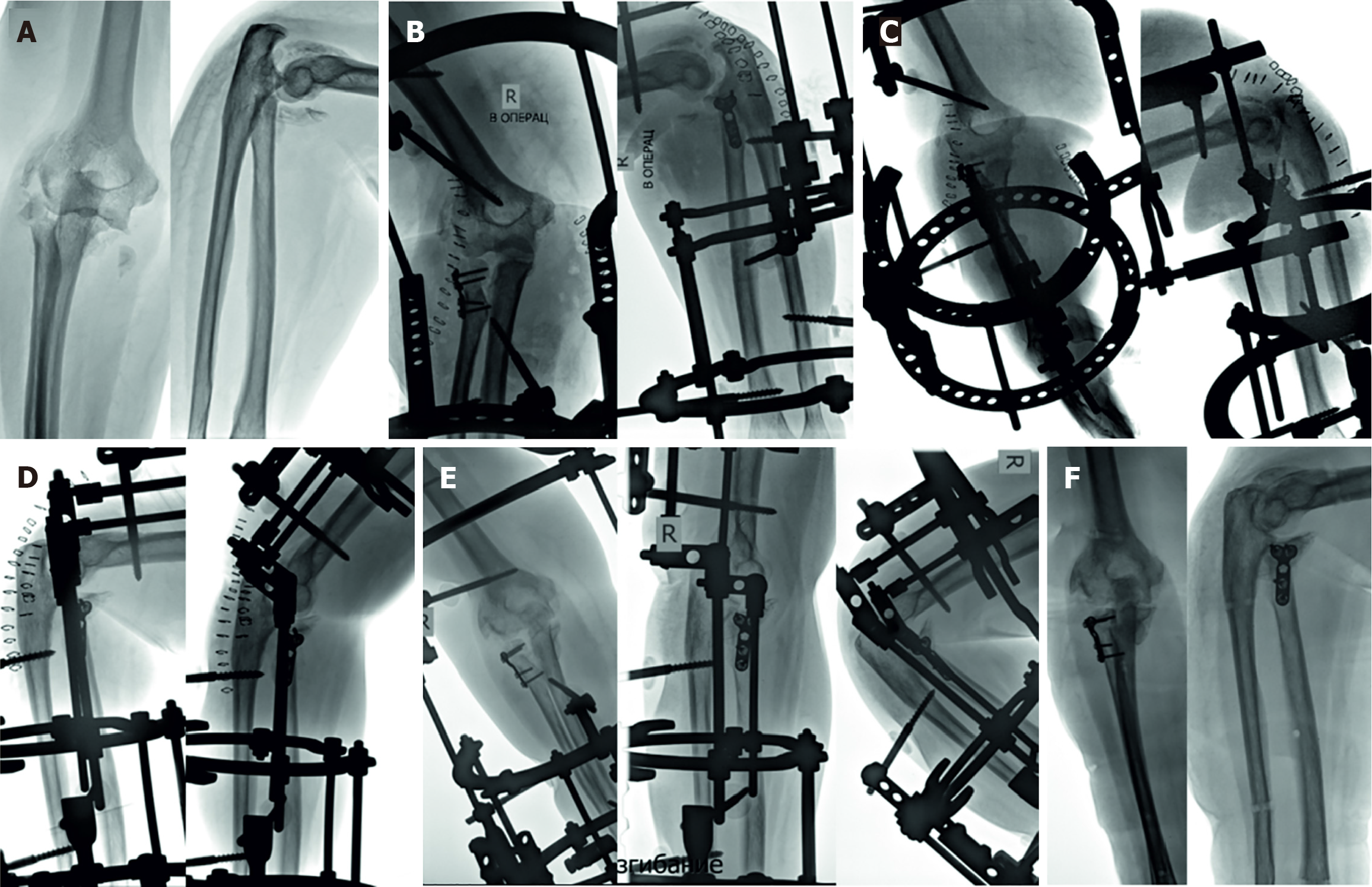
Though the Ilizarov apparatus is the most commonly used fixator to address deformities and limb lengthening, gradual correction of deformities can be achieved with number of modified techniques and modified fixators[9,15-17,44]. Thus, the strategy of intramedullary flexible nailing combined with external fixation ensured a reduction in external fixation time and high accuracy of alignment. Intramedullary nails are left in situ and prevent deformity recurrence in dysplastic or abnormal bone zones[17,44]. External hexapods incorporate universal reduction units to perform correction and lengthening[43]. The newer six-axis devices such as the Ortho-SUV can greatly aid in deformity correction[18]. External hexapods are universal reduction devices that can provide any type of movement but independent movements are impossible because of hexapod construction. All reductional maneuvers are made by simultaneous compression/distraction forces in all struts of the hexapod. Alternatively, external fixators with special connection mechanisms are able to provide independent movements of the rings in six degrees of freedom[45-47]. Devices of this type have advantage in gradual reduction and treatment of nonunion by compression-distraction method due to their ability to produce separate movements of bone fragments in any direction (Figure 3)[46,47]. Another advantage of such devices is unnecessary software in the treatment process.
It is noteworthy to stress that complex deformities involving congenital conditions and several joints are better addressed with specific personalized assemblies constructed from the Ilizarov apparatus sets like in the study that presented eight pediatric cases of previously non-ambulatory children in which deformities were corrected gradually with construction of individual Ilizarov frames and additional soft- tissue releases in three knees[16]. Despite that minor recurrence of deformity is expected in such cases, all patients became ambulatory aided with braces and supports.
Intramedullary telescopic nailing used in combination with a reduced Ilizarov frame in children with osteogenesis imperfecta was another modification for such specific cases of deformity correction in the femur and tibia in 12 children in the age up to 13 years[19]. Reduced external fixation enabled to overcome the limitations of telescopic systems to provide longitudinal and rotational stability. Children were able to walk weight-bearing in the postoperative period because of external fixation that lasted 35.8 ± 13.2 days in average. Telescopic gain related to spontaneous growth assessed at one-year follow-up control was 13.7 mm in the tibia and 15.9 mm in the femur. There were no deep infection or neurologic complications. Gait and joint problems resolved after one year.
Thus, hybrid techniques (external fixation + intramedullary nailing) have become suitable in difficult scenarios (big lengthening magnitude or deficient bone) and may have sequential or simultaneous protocols[3,17].
The Ilizarov bone transport is the most used technique for bone defect management, especially in the tibia[48]. Today, newer methods of bone transport have been described using a hexapod system with a computer program to move the ring fixator[20], or unilateral fixation and an internal cable as a guide to transport the fragment[48]. Multiple osteotomy techniques, such as tandem, trifocal, tetra-focal and penta-focal transport techniques, were reported in the literature with successful reduction of the transport time[49]. However, monorail systems for infected and non-infected nonunion of the tibia had similar functional results as the Ilizarov fixator but lower external fixation time[50].
Hybrid techniques may combine the advantages of external fixators with internal implants. They allow early removal of the external fixator after the transport phase is over, thus shortening the external fixation time by several folds[21,22]. Also, internal implants can maintain bony alignment and stability, protect the distraction callus and the docking site from fracture and deformity. Hybrid techniques may be sequential internal fixation after bone transport or simultaneous internal fixation along with bone transport.
The Ilizarov bone transport, based on the principle of distraction osteogenesis, has demonstrated remarkable success in treating chronic osteomyelitis with associated bone loss, achieving infection control rates of up to 95% in some series[23]. Modified techniques such as hemicorticotomy for bone transport have been proposed in recent years. This approach involves partial osteotomy and transport of a vascularized bone flap rather than complete segmental resection. Three-dimensional (3D)-printed customized guides offer the potential for a more precise osteotomy site, optimized frame configuration, and improved overall surgical accuracy[23]. Another modified technique for treatment of bone defects is cable-assisted bone transport that was compared with the established Ilizarov bone transport[48]. It allows bone transport for defects greater than 10 cm in the presence of compromised soft tissues, while the patient continues to weight-bear as tolerated. The transport strut is designed to provide a stable and efficient motor for the cable performing the bone transport. However, the technique is complex technically. If required, customized Ilizarov external frames can be designed for special conditions, as in a case report after a failed treatment of infected nonunion in an obese patient[51].
Transverse tibia transport, once used by the Ilizarov team, was further developed by Chinese orthopedic surgeons to use it for thromboangiitis obliterans and diabetic foot with remarkable treatment outcomes[24,25]. Various fixators and instruments for transverse tibia transport were invented and applied in recent years[9]. Their main features are com
The units of external frames on the foot were modified to consider its complex anatomy and the clinical needs ranging from correction of multi-plane deformities, lengthening, joint arthrodesis or distraction arthroplasty[9,26,52]. Ilizarov or hexapod circular fixators are also utilized for recurrent clubfoot according to surgeon’s preference. Fixator configurations, acute and gradual correction techniques, and case examples have been well described[52,53]. The construction of classical Ilizarov fixator for foot and ankle surgery has been improved for better patient’s comfort by designing pads for floor contact or a modular U-shaped foot frame and forefoot frame modifications[9]. The transverse tibia distraction was found effective for the treatment of diabetic foot ulcer complicated by chronic osteomyelitis[27]. Calcaneal lengthening using a specialized Ilizarov external fixator assembly was a technique to restore the length and height of the calcaneus in three cases of posttraumatic shortening[26]. Individual osteotomies and personalized Ilizarov frames were constructed to fix the tibia, calcaneus, talus, and forefoot and start distraction after a latency period of 7 days that achieved satisfactory foot function[26]. A modified technique of hindfoot reconstruction in chronic calcaneal osteomyelitis was very effective to recover the shape of the segment[28]. The new surgical procedure was reported with the use of the Ilizarov apparatus for partial or total calcaneal osteomyelitis that was aimed to preserve the hindfoot[29].
Ankle fusion with the Ilizarov fixator has become an established practice as the rates of success are very high[54,55]. It is seen as a salvage procedure in septic cases and previous failures with internal techniques[55]. Ankle arthrodesis was done in a closed manner using the Ilizarov ring fixator, without surgical preparation of the joint surfaces by cartilaginous debridement, in Charcot joint, Charcot-Maire-Tooth disease, and post-traumatic arthritis and showed comparable results to open methods[30,56]. An interesting practice was shown by a study that demonstrated a special fixator assembly that achieved high clinical efficacy in distraction arthroplasty for treating moderate-to-severe ankle arthritis in a young and elderly people groups at a rather long follow-up proven with visual analysis scale and American Orthopaedic Foot and Ankle Society ankle–hindfoot scores[31].
The use of external fixators in the upper limb remains more limited than their application in the lower limbs due to the spread of new systems of plates and screws and intramedullary lengthening nails that are more comfortable for patients[57]. The indications about when to use external fixation remain open. However, monolateral or circular frames for humeral lengthening and correction of forearm deformities in multiple hereditary exostoses disease or radial longitudinal deficiency sequelae is a common practice[58]. Monoaxial fixators retain a prominent role for skeletal lengthening in the upper limb, including an Orthofix© monolateral fixator[58,59]. However, multiaxial external fixators are used efficiently for humeral lengthening and angular and rotational deformity correction. Circular fixators may be preferred in cases of severe deformity. Thus, hexapod systems are likely to represent the future for the correction of multiplanar forearm deformities[59]. Lengthening of the humeri improves the overall proportion in achondroplasia[59,60]. It is supposed that the role of external fixators could be outclassed by motorized intramedullary nails, especially for humeral lengthening[57].
Mini-fixators are compact external fixators for small bones of the hand and foot. The one that was designed in the 1980s by the Ilizarov team[61] has been still used for finger, toe, metacarpal and metatarsal bone and soft-tissue problems[32,62-65]. Enlargement of the great toe by applying transverse distraction with a mini-fixator of the original type for future finger transposition was presented as a modified technology of transverse distraction implemented with the Ilizarov technique[33]. Multiple tissues of the great toe regenerated, including bone, nail, and plantar skin, and more tissues were preserved after toe-to-hand transfer. This is a novel method to enlarge the donor site for finger reconstruction. Mini-ring external fixators were designed in several sizes for specific tasks such as metacarpal lengthening for thumb reconstruction[34]. Such device was used with a groin flap for single-stage lengthening of the injured thumb with bone exposure. The first web-space plasty was achievable with the Ilizarov mini-fixator to improve esthetics and function in complex injuries of the hand[35]. The Ilizarov mini-fixator was found less invasive than plate fixation for the treatment of chronic Monteggia fracture-dislocations in children[36].
Nowadays, the dominant external fixation technique used for bone injuries is application of monolateral fixators for temporary stabilization in polytrauma and soft tissue management in open fractures or compromised skin conditions followed by definite fixation. Among most common external fixators are a unilateral spanning external fixator for tibial plateau fractures[66] and a delta-frame for comminuted pilon fractures[67]. However, external fixation as a definitive treatment for fractures also remains popular, especially for tibial plateau and pilon fractures[37-39,67,68]. A hybrid type of half-pin and wire external fixator is used for these fractures. The common construct of the external fixator for pilon fractures is generally the same as the Ilizarov-type external fixator[66].
The main merit of fracture treatment using external fixators is their technical capabilities. Unilateral external fixators can only temporarily stabilize fragments, maintaining the axis, length, and rotation of the segment. They do not allow for reduction. On the other hand, ring fixation devices such as the Ilizarov fixator are capable of performing reduction maneuvers by moving the olive wires or rings using hinges[38,39]. The most modern and promising type of a ring fixator for shaft fractures would be the one that allows for six degrees of freedom (Figure 3), as it is time-saving and causes less trauma during reduction[45,47]. Reduction of spiral fractures with this type of fixator was more accurate and the fixation term with the frame on was much shorter than the one performed with the Ilizarov fixator[45].
Fixation of intra-articular fractures remains a weak point of the Ilizarov fixator and its modifications, due to the difficulty in achieving closed anatomical reduction[39]. On the other hand, hinged external fixators are essential for injuries to the elbow, such as the terrible triad[69]. They may be combined with open reduction and internal fixation (Figure 4).
Definitive circular external fixation for acute tibial fracture-related infection with either the Ilizarov or hexapod fixators was efficient in a comparative study that showed their high union rate and infection control. Nevertheless, the hexapod fixation resulted in less residual coronal translation deformity and better callus quality[37]. On the other hand, a comparative study of the time to frame removal for tibia fractures treated with hexapod and Ilizarov circular frames found that there was a significant difference between Ilizarov and hexapod frames in favor of the Ilizarov fixator, especially in metaphyseal fractures the proportion of which was larger in that study[70]. Another study investigated the utility and outcomes of the Ilizarov circular external fixation in the management of failed internal fixation of tibial fractures. It yielded limb salvage in complex infected and non-infected cases with a high union rate (100%) and minimal major complications[71].
A remarkable experience was presented in the use of microsurgery combined with the Ilizarov technique in limb amputation[40]. Limb salvage and reconstruction was performed after replantation with the use of internal and external step-by-step combined fixation, one-stage shortening and two-stage limb lengthening in 44 patients with mostly good functional results.
The minimally invasive modified Ilizarov hip reconstruction surgery was proposed as an alternative for hip re
Thus, the evolution of external fixation for bone pathology has made a long way and has not stopped yet[72,73]. However, a number of biomechanically proven and clinically approved external fixators, modifications of their configurations and techniques have established their role in the contemporary orthopedics in the past decades. Advancement of newer robotic technologies that could motorize and control the process of distraction osteogenesis and 3D accuracy of reduction would be a great step forward in future, if they are commercially available[72].
Until now, the Ilizarov fixator remains a versatile and affordable orthopedic instrument. It can be fabricated at the national level and most of its components are reusable what is important for the developing countries[74,75]. The collection of recent reports of its application to be considered for reviewing is enormous according to the PubMed database diagram that indicates that within the period of 2020 throughout 2024 more than 130 articles related to the Ilizarov method have been published each year in the prominent orthopedic journals worldwide.
Data relevant to Ilizarov technologies from 1994 to 2023 were collected, studied and presented early in 2025[76]. The methodology used identified that the peak of publications occurred in 2020, with 141 articles published. There are a number of previous reviews on the topic of the Ilizarov method and external fixation advances[1-3,76]. They discuss some history of the method and its basic principles[1], advances in bone lengthening[3], international spread of the method on the basis of publications[2,76], and innovations of in the field made by Chinese researchers[9]. Advancements in the external fixation focus on several key areas that include optimization of Ilizarov external fixator essemblies or innovative designs that could increase precision of manipulations with the fixator, reduce the risk of complications, and improve its use by both patients and surgeons. Personalized treatment plans and patient comfort in every case remain the main concerns in the customized approach and external fixator choice. Our mini-review is aimed to focus on recent specific applications and modifications in the Ilizarov method for certain clinical scenarios that require a more specialized approach that are summarized in Table 1[8-41].
The classical Ilizarov ring fixator is still the tool and the Ilizarov principles are the method of choice for complex reconstruction of the injured or deformed bone in adults and in pediatric population. It is crucial to possess a precise comprehension of the Ilizarov principles in order to effectively utilize and modify this method and fixation system. A great variety of external, hybrid and internal fixators based on the Ilizarov principles have been designed lately to generate new bone tissue or repair it and fulfill an ultimate goal of improving treatment outcomes in orthopedic injuries and diseases. This fact reflects the impact of the Ilizarov philosophy of bone regeneration and repair on the contemporary orthopedic clinical science and practice. In 2026, the Ilizarov apparatus will be 75 years old. Millions of patients in the world are thankful to this old orthopedic tool that has improved their quality of life or salvage their lives while orthopedic surgeons worldwide praise this invention for its great utility.
| 1. | Guan S, Du H, Wu Y, Qin S. The Ilizarov Technique: A Dynamic Solution for Orthopaedic Challenges. Orthop Surg. 2024;16:2111-2114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Malkova TA, Borzunov DY. International recognition of the Ilizarov bone reconstruction techniques: Current practice and research (dedicated to 100(th) birthday of G. A. Ilizarov). World J Orthop. 2021;12:515-533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (3)] |
| 3. | Hosny GA. Limb lengthening history, evolution, complications and current concepts. J Orthop Traumatol. 2020;21:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 106] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 4. | Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;249-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1510] [Cited by in RCA: 1354] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 5. | Ilizarov GA, Soĭbel'man LM, Chirkova AM. [Some roentgenologic and morphologic data on regeneration of bone tissue in experimental distraction epiphysiolysis]. Ortop Travmatol Protez. 1970;31:26-30. [PubMed] |
| 6. | Ilizarov GA, Deviatov AA. [Surgical lengthening of the shin with simultaneous correction of deformities]. Ortop Travmatol Protez. 1969;30:32-37. [PubMed] |
| 7. | Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990;8-26. [PubMed] [DOI] [Full Text] |
| 8. | Popkov A, Dučić S, Lazović M, Lascombes P, Popkov D. Limb lengthening and deformity correction in children with abnormal bone. Injury. 2019;50 Suppl 1:S79-S86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Zhu YL, Guo BF, Zang JC, Pan Q, Zhang DW, Peng Y, Qin SH. Ilizarov technology in China: a historic review of thirty-one years. Int Orthop. 2022;46:661-668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 10. | Chalak A, Singh S, Shetty S, Kale S, Singh P, Ghodke A. A Novel technique of three-ring Ilizarov fixator frame in gap non-union of tibia. J Clin Orthop Trauma. 2021;23:101639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Rohilla R, Das J, Sharma PK, Lalchandani T, Dhankhar S, Singh A, Sharma J. Outcomes of Post-traumatic Infected Non-union of the Humerus Managed by Hybrid Ring Fixators. Indian J Orthop. 2025;59:602-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Ferreira N, Arkell C, Fortuin F, Saini AK. Evaluating the Accuracy of the SMART Taylor Spatial Frame Software-Comparison with Manual Radiographic Analysis Methods. J Limb Lengthening Reconstr. 2021;7:31-36. [DOI] [Full Text] |
| 13. | Teulières M, Langlais T, de Gauzy JS, Rölfing JD, Accadbled F. Bone Lengthening with a Motorized Intramedullary Nail in 34 Patients with Posttraumatic Limb Length Discrepancies. J Clin Med. 2021;10:2393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Fuller CB, Shannon CE, Paley D. Lengthening Reconstruction Surgery for Fibular Hemimelia: A Review. Children (Basel). 2021;8:467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Zein AB, Elhalawany AS, Ali M, Cousins GR. Acute correction of severe complex adolescent late-onset tibia vara by minimally invasive osteotomy and simple circular fixation: a case series with 2-year minimum follow-up. BMC Musculoskelet Disord. 2021;22:681. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Leonchuk SS, Novikov KI, Subramanyam KN, Shikhaleva NG, Pliev MK, Mundargi AV. Management of severe congenital flexion deformity of the knee using Ilizarov method. J Pediatr Orthop B. 2020;29:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Popkov A, Pietrzak S, Antonov A, Parol T, Lazović M, Podeszwa D, Popkov D. Limb Lengthening for Congenital Deficiencies Using External Fixation Combined With Flexible Intramedullary Nailing: A Multicenter Study. J Pediatr Orthop. 2021;41:e439-e447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Zodey K, Mankar S, Agrawal PP. The Management of Complex Knee Deformity Using Ortho-SUV: A Case Study. Cureus. 2024;16:e68065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Popkov D, Dolganova T, Mingazov E, Dolganov D, Kobyzev A. Combined technique of titanium telescopic rods and external fixation in osteogenesis imperfecta patients: First 12 consecutive cases. J Orthop. 2020;22:316-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 20. | Schnack LL, Oexeman S, Rodriguez-Collazo ER. Management of Osseous Defects of the Tibia Utilizing Orthofix Hexapod Circular External Fixator: A Technique Guide-An Orthoplastic Approach for Combined Soft Tissue and Osseous Defects. Clin Podiatr Med Surg. 2021;38:e44-e58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Xie L, Huang Y, Zhang L, Si S, Yu Y. Ilizarov method and its combined methods in the treatment of long bone defects of the lower extremity: systematic review and meta-analysis. BMC Musculoskelet Disord. 2023;24:891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 22. | Borzunov DY, Kolchin SN. Nonunion of the femoral shaft associated with limb shortening treated with a combined technique of external fixation over an intramedullary nail versus the Ilizarov method. Arch Orthop Trauma Surg. 2022;142:2185-2192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 23. | Hamiti Y, Abudureyimu P, Lyu G, Zhang J, Xu X, Yusufu A, Yushan M. Integrating 3D-printed customized guides with hemicorticotomy bone transport: clinical outcomes in chronic osteomyelitis management. BMC Musculoskelet Disord. 2024;25:907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Zuo Q, Gao F, Song H, Zhou J. Application of Ilizarov transverse tibial bone transport and microcirculation reconstruction in the treatment of chronic ischemic diseases in lower limbs. Exp Ther Med. 2018;16:1355-1359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 25. | Zhang X, Dong T, Yao S, Lu S, Li W. Application of transverse tibial bone transport and microcirculation reconstruction in the treatment of diabetic foot ulcer: a case report. Ann Palliat Med. 2021;10:8358-8364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 26. | Cui Y, Xu Q, Zang J, Wang G, Liu B, Chen B, Lin J, Zhu L. Preliminary Outcomes of Calcaneal Body Lengthening for the Calcaneus Shortening. Orthop Surg. 2024;16:2283-2288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Chen Y, Kuang X, Zhou J, Zhen P, Zeng Z, Lin Z, Gao W, He L, Ding Y, Liu G, Qiu S, Qin A, Lu W, Lao S, Zhao J, Hua Q. Proximal Tibial Cortex Transverse Distraction Facilitating Healing and Limb Salvage in Severe and Recalcitrant Diabetic Foot Ulcers. Clin Orthop Relat Res. 2020;478:836-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 28. | Harahsheh BH, Almajali A, Al-Zaben R, Rahaymeh J, Sudnitsyn AS. A new technique of hindfoot reconstruction in chronic calcaneal osteomyelitis using the Ilizarov apparatus - a case series. J Pak Med Assoc. 2022;72:342-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 29. | Mekki WA, Kliushin NM, Sudnitsyn AS. Calcaneogenesis: the use of tibial bone transport for treatment of massively infected hindfoot defects. Acta Orthop Belg. 2022;88:127-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 30. | Alammar Y, Sudnitsyn A, Neretin A, Leonchuk S, Kliushin NM. Closed arthrodesis in infected neuropathic ankles using Ilizarov ring fixation. Bone Joint J. 2020;102-B:470-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 31. | Wang J, Wang C, Ding X, Dong Q. Effect of Distraction Arthroplasty in the Treatment of Moderate-to-Severe Ankle Arthritis. Orthop Surg. 2024;16:2167-2172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Hayashi K, Hattori Y, Sakamoto S, Gour V, Sasaki J, Doi K. Reconstruction of Total Hand Degloving Injury with Combined Free and Pedicled Flaps and Ilizarov Minifixator. Plast Reconstr Surg Glob Open. 2024;12:e5976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 33. | Hao L, Rong K, Chen C, Hou Z, Wang Y, Tian X, Wang Z. Transverse Distraction of Great Toe to Enlarge the Donor Site before Finger Reconstruction. Orthop Surg. 2024;16:2289-2294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 34. | Zhu Y, Xu Y, Pu S, Lv Q, Cai X, Zhao Y. Metacarpal Lengthening Using a Mini-Ring Ilizarov Device for Thumb Reconstruction. J Hand Surg Am. 2024;49:708.e1-708.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | Salimi H, Gotani H, Tanaka Y, Sasaki K, Yagi H, Okamoto K, Miyashima Y, Murakami Y, Tsuchiya T. First web space plasty using Ilizarov mini fixator in patients with complex hand injuries. Orthoplast Surg. 2022;9:72-79. [DOI] [Full Text] |
| 36. | Take M, Tomori Y, Sawaizumi T, Majima T, Nanno M, Takai S. Ulnar osteotomy and the ilizarov mini-fixator for pediatric chronic monteggia fracture-dislocations. Medicine (Baltimore). 2019;98:e13978. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 37. | Corona PS, Pujol O, Vicente M, Ricou E, de Albert M, Maestre Cano D, Salcedo Cánovas C, Martínez Ros J. Outcomes of two circular external fixation systems in the definitive treatment of acute tibial fracture related infections. Injury. 2022;53:3438-3445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 38. | Hegde AS, Madegowda A, Khanna V, Rao S. Clinical and Radiological Outcome of Complex Proximal Tibia Fractures Managed with Hybrid/Ilizarov Fixator with or without Minimal Internal Fixation. Ortop Traumatol Rehabil. 2021;23:279-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 39. | Morasiewicz P, Pelc M, Tomczyk Ł, Kochanska-Bieri J, Bobiński A, Pili D, Reichert P. Clinical and radiological assessment of the Polish modification of the Ilizarov external fixator for the treatment of intra-articular calcaneal fractures. Adv Clin Exp Med. 2025;34:1321-1329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 40. | Xie S, Hou J, Wang H, Liu W, Dong Q, Zhang S, Yang C, Qin S. Methods and Strategies of Microsurgery Combined with Ilizarov Technique in the Treatment of Amputation of Limbs in Renji Hospital: A Report of 51 Cases. Orthop Surg. 2024;16:2273-2282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 41. | Luo S, Kong L, Wang J, Nie H, Luan B, Li G. Development of modified Ilizarov hip reconstruction surgery for hip dysfunction treatment in adolescent and young adults. J Orthop Translat. 2021;27:90-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Stoffel C, Eltz B, Salles MJ. Role of coatings and materials of external fixation pins on the rates of pin tract infection: A systematic review and meta-analysis. World J Orthop. 2021;12:920-930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Keshet D, Eidelman M. Clinical utility of the Taylor spatial frame for limb deformities. Orthop Res Rev. 2017;9:51-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 44. | Popkov A, Aranovich A, Antonov A, Journeau P, Lascombes P, Popkov D. Lower limb lengthening and deformity correction in polyostotic fibrous dysplasia using external fixation and flexible intramedullary nailing. J Orthop. 2020;21:192-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Matsukatov FA, Boichuk SP, Khubaev ND. Analysis of functional-and-ergonomic characteristics of external fixators, and prediction of the effectiveness of their use in clinical practice. Gen Ortop. 2013;2. |
| 46. | Matsukatov FA, Gerasimov DV. Factors Affecting the Terms of Fracture Consolidation. N.N. Priorov J Traumatol Orthop. 2016;23:50-56. [DOI] [Full Text] |
| 47. | Matsukatov FA. Compression-distraction apparatus for external fixation and method of closed reduction of bone and bone fragments. Euroasian patent register. https://old.eapo.org/en/patents/reestr/patent.php?id=45163. |
| 48. | Alibakan G, Kanar M, Armağan R, Sülek Y, Altuntaş Y, Eren OT. Cable-asisted bone transport versus circular external fixators-asisted bone transport in the management of bone defects of the Tibia: clinical and imaging results. J Orthop Surg Res. 2025;20:264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 49. | Yushan M, Abulaiti A, Maimaiti X, Hamiti Y, Yusufu A. Tetrafocal (three osteotomies) and pentafocal (four osteotomies) bone transport using Ilizarov technique in the treatment of distal tibial defect-preliminary outcomes of 12 cases and a description of the surgical technique. Injury. 2022;53:2880-2887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 50. | Maheshwari V, Raja BS, Bahadur B, Regmi A, Dhingra M, Gowda AKS. Outcome analysis of ilizarov and monorail fixators in the treatment of nonunion of long bones: A systematic review and proportion meta-analysis. J Clin Orthop Trauma. 2023;40:102170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 51. | Ilyas MS, Sattar A, Zehra U, Aziz A. Management of femoral shaft infected nonunion through customised Ilizarov external fixator assembly in a morbidly obese patient. BMJ Case Rep. 2022;15:e245824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 52. | Kirienko A, Malagoli E. Ilizarov Technique in Severe Pediatric Foot Disorders. Foot Ankle Clin. 2021;26:829-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 53. | Meyer Z, Zide JR, Cherkashin A, Samchukov M, Bohl DD, Riccio AI. Narrative review of ring fixator management of recurrent club foot deformity. Ann Transl Med. 2021;9:1104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 54. | Morasiewicz P, Dejnek M, Orzechowski W, Szelerski Ł. Subjective and Objective Outcomes of Ankle Joint Arthrodesis with Either Ilizarov or Internal Fixation. J Foot Ankle Surg. 2023;62:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 55. | Wang S, Li B, Yu X, Wu H, Liu L. Is Ankle Arthrodesis With an Ilizarov External Fixator an Effective Treatment for Septic Ankle Arthritis? A Study With a Minimum of 6 Years of Follow-up. Clin Orthop Relat Res. 2023;481:717-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 56. | Brinkemper A, Lülsdorff RH, Lotzien S, Kruppa C, Schildhauer TA, Cibura C. Ilizarov fixator as salvage procedure after frustrating arthrodesis using intramedullary nailing - is there a chance of consolidation? Arch Orthop Trauma Surg. 2024;144:5031-5038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 57. | Catena N, Arrigoni C, Carvalho M, Matic I, Farr S. External fixators and lengthening systems in pediatric upper limb. J Child Orthop. 2025;19:139-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 58. | Wang S, Herman B, Wu Y, Lei M, Mutasa B, Hong P, Li J. Ulnar lengthening for children with forearm deformity from hereditary multiple exostoses: a retrospective study from a tertiary medical center. BMC Pediatr. 2024;24:585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 59. | Mindler GT, Stauffer A, Chiari C, Mladenov K, Horn J. Achondroplasia current concept of orthopaedic management. J Child Orthop. 2024;18:461-476. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 60. | García López JM, García de la Blanca JC, Martí Ciruelos R, Núñez Ligero G. Bilateral humeral lengthening and deformity correction with hexapod external fixator in an achondroplastic patient: A case report. Int J Surg Case Rep. 2024;123:110285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 61. | Shevtsov V, Kirienko A, Shikhaleva N, Novikov K. History of the Ilizarovs wire-fixator, stages of hand surgery development at the Ilizarov Center. Gen Ortop. 2021;27:299-306. [DOI] [Full Text] |
| 62. | Usami S, Hamada Y, Toyama T, Kinosita R, Sawada M, Saito T. New strategy for shortening the consolidation period in distraction lengthening of phalanges or metacarpal bone. J Plast Reconstr Aesthet Surg. 2024;99:369-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 63. | Gotani H. "Callus Bending Technique" Following Gradual Bone Lengthening for Functional Reconstruction in Cases of Phalangeal Loss Due to Digital Amputation: Two Case Reports. J Hand Surg Glob Online. 2025;7:292-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 64. | Kanchanathepsak T, Gotani H, Hamada Y, Tanaka Y, Sasaki K, Yagi H, Kubota Y, Tawonsawatruk T. The effectiveness of distraction lengthening in traumatic hand amputation with Ilizarov mini fixator. Injury. 2020;51:2966-2969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 65. | Barik S, Farr S. Brachymetacarpia and brachymetatarsia: do we need to operate? EFORT Open Rev. 2021;6:15-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 66. | Liskutin T, Bernstein M, Lack W, Perry M, Summers H. Surgical Technique: Achieving Reduction With Temporizing, Knee-Spanning External Fixation. J Orthop Trauma. 2018;32 Suppl 1:S32-S33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 67. | Harrison WD, Fortuin F, Durand-Hill M, Joubert E, Ferreira N. Temporary circular external fixation for spanning the traumatised ankle joint: A cohort comparison study. Injury. 2022;53:3525-3529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 68. | Bashir A, Satalich JR, Hampton H, Cinats DJ. Circular External Fixation of Ankle and Pilon Fractures Using Novel Polyaxial Locking Struts. J Long Term Eff Med Implants. 2024;34:65-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 69. | Leschinger T, Ott N, Hackl M, Wegmann K, Müller LP. [External fixator of the elbow]. Oper Orthop Traumatol. 2020;32:387-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 70. | Watts A, Sadekar V, Moulder E, Souroullas P, Hadland Y, Barron E, Muir R, Sharma H. A comparative evaluation of the time to frame removal for tibia fractures treated with hexapod and Ilizarov circular frames. Injury. 2023;54:996-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 71. | Marwan Y, Turner J, Senan R, Muir R, Barron E, Hadland Y, Moulder E, Sharma H. Circular external fixation for revision of failed tibia internal fixation. Eur J Orthop Surg Traumatol. 2024;34:353-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 72. | Bliven EK, Greinwald M, Hackl S, Augat P. External fixation of the lower extremities: Biomechanical perspective and recent innovations. Injury. 2019;50 Suppl 1:S10-S17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (1)] |
| 73. | Ferreira N, Sabharwal S, Hosny GA, Sharma H, Johari A, Nandalan VP, Vivas M, Parihar M, Nayagam S, Ferguson D, Rölfing JD. Limb reconstruction in a resource-limited environment. SICOT J. 2021;7:66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 74. | Pulate A, Olivier LC, Agashe S, Rallan R, Kamal V, Nast-Kolb D. Adaptation of Ilizarov ring fixator to the economic situation of developing countries. Arch Orthop Trauma Surg. 2001;121:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 75. | Chironga K, Swanepoel S, Dey R, Graham SM, Held M, Laubscher M. The reuse of circular external fixator components: an assessment of safety and potential savings. Eur J Orthop Surg Traumatol. 2023;33:119-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 76. | Wang X, Lu F, Wang W, Zhi X. Global Research Hotspots and Trends in Advances of the Ilizarov Technique: A Bibliometric Mapping. Orthop Surg. 2025;17:663-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/