Published online Oct 18, 2025. doi: 10.5312/wjo.v16.i10.109196
Revised: June 12, 2025
Accepted: September 19, 2025
Published online: October 18, 2025
Processing time: 161 Days and 16 Hours
In 2017, our institution implemented a high efficiency (HE) pathway for lower limb orthopedic surgery. The employed strategy included patient selection, surgical instrument standardization, preoperative surgical nerve blocks, avoi
To determine whether the implementation of a HE pathway was correlated with a reduction in postoperative recovery time.
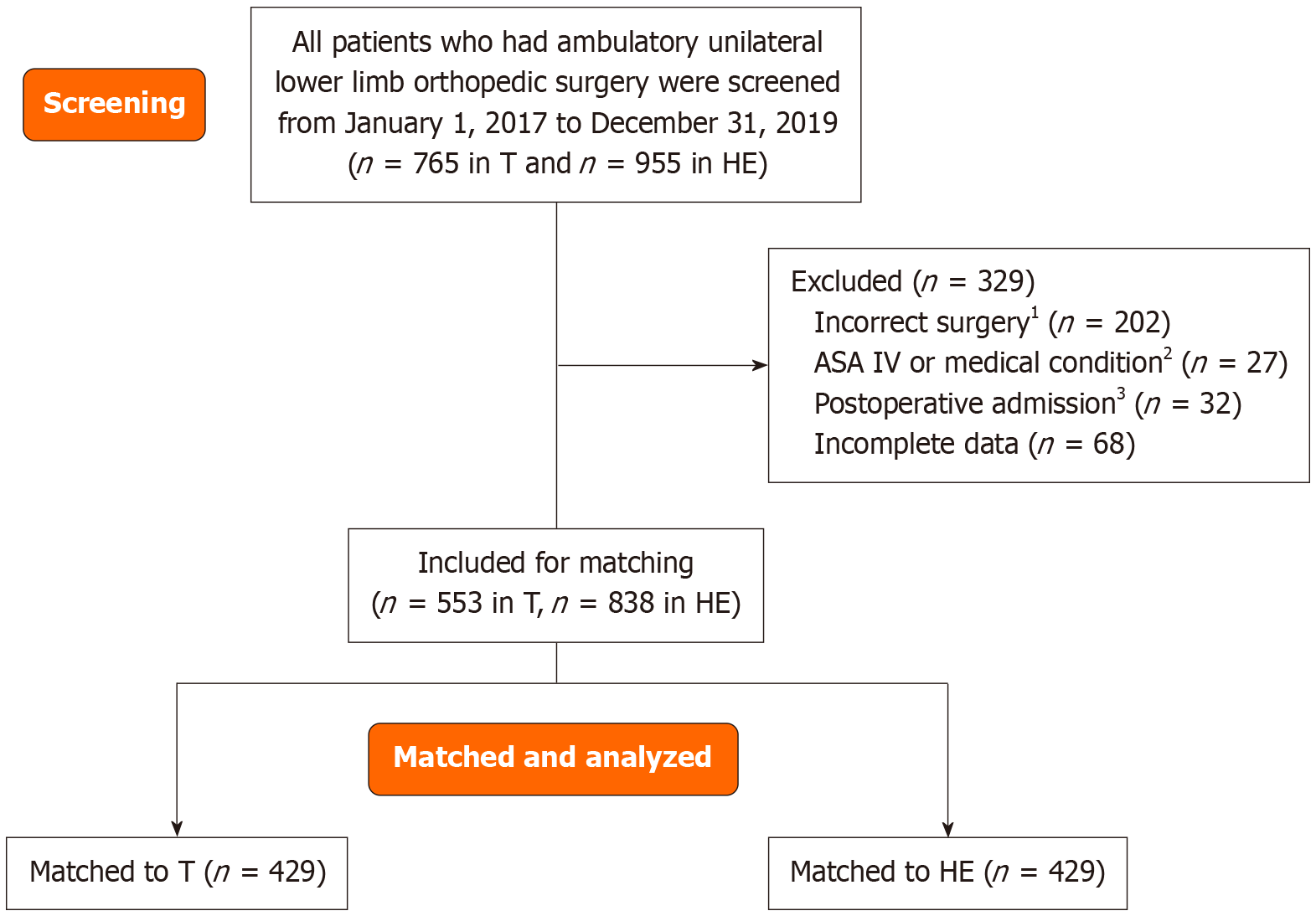
Patients who had unilateral elective lower limb orthopedic procedures through the T and HE pathway were screened between 2017 to 2019. Patients were at least 18 years old, and American Society of Anesthesiologists (ASA) Physical Status I to III without major systemic comorbidities were included. Propensity score was generated using multivariable regression taking age, body mass index, sex, ASA class and surgical type as covariates using nearest neighbour methods between the two pathways. Mann Whitney U test were used to analyzed total postoperative time.
There was an associated reduction in total postoperative recovery time of 63 minutes (95%CI: -69 to -57) in the HE group. The operating room time and total length of stay also had an associated decrease of 20 minutes (95%CI: -23 to -17) and 84 minutes (95%CI: -92 to -75) respectively.
Utilizing multifaceted strategies to improve perioperative efficiency was associated with a reduction in the postoperative recovery time in our retrospective study. This model can be a potential strategy to deal with surgical backlog in the face of ongoing human resource challenges.
Core Tip: This study shows that adopting a high-efficiency approach for lower limb orthopedic surgery, by selecting appropriate patients, using standardized instruments, applying regional anesthesia, and bypassing phase one recovery, significantly shortens postoperative recovery time, reduces operating room duration, and decreases total hospital stay. This model provides a practical and scalable way to enhance perioperative care and tackle surgical backlogs in the face of on
- Citation: Lin C, Nagdev T, Zhu DA, Nair GS, Cheng S, Kumar K. High efficiency pathway for lower limb orthopedic surgery: A matched historic cohort study. World J Orthop 2025; 16(10): 109196
- URL: https://www.wjgnet.com/2218-5836/full/v16/i10/109196.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i10.109196
The Ontario Medical Association estimated that the backlog resulting from the coronavirus disease 2019 pandemic would require the hospitals to work at 120% above baseline capacity for more than two years to clear[1]. However, due to the ongoing health human resources challenges, many Canadian hospitals struggle to operate at capacity, resulting in cancellation[2]. Longer wait time can cause patient distress, economic loss due to missed working days and worsening pain[3]. Therefore, fast-track ambulatory surgery that allows higher throughput while utilizing similar resources could be one solution to address the backlog while the authorities work to resolve the human resource shortage.
In 2017, our institution implemented a highly optimized perioperative process for lower limb orthopedic procedures. We adopted strategies well known to reduce hospital length of stay, including patient selection, avoidance of general anesthesia, utilization of peripheral nerve blocks, standardization of surgical instrument and bypassing phase 1 recovery[4,5]. Patients received preoperative education regarding ambulation and pain management. Additionally and uniquely, we created a separate but parallel pathway to the traditional (T) pathway. Preoperative bays were set aside so patients could be prepared for surgery and porters could easily identify these patients to expedite transfer between perioperative areas. A subset of perioperative staff was involved in the pathway, increasing familiarity with their tasks and patient needs and education. To reduce turnover time, surgical instruments were condensed into a single tray with 25 ins
To date, we were not aware of a published protocol utilizing a multidisciplinary pathway and peripheral nerve block as the sole anesthetic technique for ambulatory lower limb procedure. Therefore, we conducted a retrospective propensity score matching between the high efficiency (HE) and T surgical pathway to demonstrate the association between the perioperative processes and the duration of each part of the patients’ perioperative journey. We hy
This historic cohort study aimed to examine the impact of HE pathway on postoperative recovery time. The study was approved by Health Sciences Research Ethics Board (HSREB) at Western University (ID 113648) and the HSREB waived the requirement for informed consent.
All surgery took place in Victoria Hospital, London, Ontario, a tertiary trauma centre for Southwest Ontario with a catchment population of 1.5 million and annual surgical volume of more than 15000 cases. The perioperative area was equipped with 18 ORs and 24 bay phase one recovery, 10 bay phase two recovery and 3 bay block room.
The inclusion criteria were age of 18 year and above, American Society of Anesthesiologists (ASA) class I to III, receipt of a preoperative peripheral nerve block and an ambulatory, unilateral below knee procedure. The procedures include foot and ankle fracture fixation, arthrodesis, tendon transfer, corrective surgery for deformities, hardware removal and irrigation and debridement. Exclusion criteria were bilateral procedures, neuraxial blocks, planned postoperative admission and with a history of malignant hyperthermia, presence of major cardiac, respiratory, hepatic, renal, neu
Both pathways happened simultaneously during the study period but in different ORs. Patient selection was done at surgeons’ offices using an eligibility criteria (Supplementary material) to minimize the risk of intra- and post-operative complications. Patients, once deemed eligible for the HE pathway, were scheduled to the earliest available spot in either pathway.
Both groups received preoperative surgical blocks in form of popliteal sciatic blocks and adductor canal blocks in the block room 20 to 30 minutes before incision. Tourniquets were applied to the leg instead of the thigh whenever possible to reduce anesthetic requirement. In the HE group, the patients would be prepared as soon as the OR was ready. The intraoperative anesthetic consists of a sedation targeting a Ramsay Sedation Scale of 1 to 4 and general anesthesia was only provided if necessary. In the T group, patients would be prepared in the sequence they registered, among other non-orthopedic patients, scrub nurse would be utilized, and the intraoperative anesthetic choice was at the discretion of the anesthesiologists.
Patients from both groups could bypass phase one recovery after scoring 12 on a modified 12-point White Fast Track Score per our institutional policy (Supplementary Table 1). Phase one recovery consisted of two patients to one nursing ratio with continuous oximetry. Vital signs and the Modified Aldrete’s score were assessed every 15 minutes. Patients who score at least 9 on the Modified Aldrete’s score could be discharged to phase two recovery. Phase two recovery consisted of four to one nursing ratio and intermittent monitoring and vital signs every 30 minutes. Patients received acetaminophen and non-steroidal anti-inflammatory drugs in phase two recovery prior to discharge, after scoring at least 9 out of 10 on the Post Anesthetic Discharge Scoring System.
The primary outcome was the total postoperative recovery time, defined as when patient left the OR to the time that patient was ready for hospital discharge. The secondary outcomes include preoperative time: The time between patient registration to OR entry, OR time: Time between OR entry to OR exit and total hospital length of stay, the proportion of patients who utilize phase one recovery and the proportion receiving opioids in the postoperative period.
G-Power (version 3.1.9.7) was utilized for sensitivity analysis. The sample size was calculated with α = 0.05 and β = 0.8, using a 30-minute difference in recovery time as significant. Our institution audit showed the average and standard deviation of recovery time in the T surgical set up were 140 and 58.6 minutes respectively. With this parameter, a total sample size of 128, 64 in each group was required.
All patients who met the criteria between January 1, 2017 to December 31, 2019 were screened. Data were extracted from our electronic medical records by co-investigator Lin C, Nagdev T and Zhu DA using all available information, including those not related to surgery. Patients with incomplete data were excluded. Anyone with unexpected admission were included in the analysis, with total postoperative recovery time defined from end of operation to ready for hospital discharge.
Statistical analysis was performed using R (version 4.2.2). Patient demographics including age, sex, body mass index (BMI), ASA class and type of surgery were presented in mean and standard deviation or number and percentage. Propensity score matching was used to mitigate confounders. The matching was generated with multivariable regression, using the nearest neighbour method, with 1:1 matching, starting at a caliper of 0.1 of logit, without replacement, taking age, sex, BMI, ASA class and surgery type as covariates. Age and BMI were analyzed as continuous variables. Sex (biological male vs female), ASA class (I and II vs III) and surgery type [below vs at or above ankle (AA)] were analyzed as non-ordinal categorical variables. The demographic variables were analyzed this way as they have been shown to correlated with longer recovery time[6,7]. The anatomic location of the surgery were only matched exactly (i.e. AA to AA only) as it determined whether the tourniquet was applied to the blocked leg or unblocked thigh, thus leading to different sedation requirement. The standardized difference in means (SDM) were examined after propensity score matching. Continuous and categorical outcomes were further adjusted using linear and logistic regression respectively taking any co-variates with SDM above 0.1. Cluster-robust standard errors were calculated from the adjusted outcomes. We calculated E-value for all statistically significant outcome to determine the effect of unmeasured confounders on the outcomes.
One thousand seven hundred and twenty patients were screened, and 1391 patients met the inclusion criteria. After matching, 858 patients were included in the final analysis (Figure 1).
The pre- and post-matched demographic information are presented in Table 1. There was a higher proportion of female in both groups as commonly seen for foot and toe corrective surgery. The breakdown of the number of different surgical procedures are shown in Table 2.
| Pre-match | Post-match | |||||
| Traditional (n = 553) | High efficiency (n = 838) | SD | Traditional (n = 429) | High efficiency (n = 429) | SD | |
| Female, n (%) | 342 (63.9) | 619 (73.9) | 0.27 | 289 (67.4) | 289 (67.4) | 0 |
| Age (year), mean (SD) | 52.3 (15.4) | 55.9 (14.1) | 0.26 | 54.2 (14.7) | 53.9 (14.9) | 0.02 |
| BMI (kg/m2), mean (SD) | 29.5 (6.5) | 28.0 (5.6) | 0.26 | 29.2 (6.3) | 28.3 (5.7) | 0.16 |
| ASA I and II, n (%) | 380 (68.7) | 622 (74.2) | 0.13 | 294 (69.9) | 300 (68.5) | 0.03 |
| Surgery below ankle, n (%) | 317 (57.3) | 718 (85.7) | 0.81 | 314 (73.2) | 314 (73.2) | 0 |
| Pre-match | Post-match | |||
| Traditional (n = 553) | High efficiency (n = 838) | Traditional (n = 429) | High efficiency (n = 429) | |
| Below ankle | 318 (57.5) | 718 (85.6) | 314 (73.2) | 314 (73.2) |
| Soft tissue excision | 14 (2.5) | 48 (5.7) | 14 | 20 |
| Toe or foot hardware removal | 26 (4.7) | 69 (8.2) | 26 | 30 |
| Toe or foot arthrodesis | 147 (26.6) | 256 (30.5) | 145 | 108 |
| Toe open reduction | 17 (3.1) | 39 (4.7) | 17 | 21 |
| Toe or foot osteotomy | 81 (14.6) | 288 (34.4) | 81 | 127 |
| Foot tendon repair | 33 (6.0) | 18 (2.1) | 31 | 8 |
| At or above ankle | 235 (42.5) | 120 (14.3) | 115 (26.8) | 115 (26.8) |
| Ankle arthroscopy | 20 (3.6) | 6 (0.8) | 8 | 6 |
| Ankle or tibial hardware removal | 46 (8.3) | 100 (11.9) | 23 | 95 |
| Ankle arthrodesis | 25 (4.5) | 0 (0) | 10 | 0 |
| Ankle ligament repair | 8 (1.4) | 1 (0.1) | 4 | 1 |
| Ankle or tibial osteotomy | 25 (4.5) | 2 (0.2) | 11 | 2 |
| Ankle open reduction | 111 (20.0) | 11 (1.3) | 59 | 11 |
There were significantly higher number of ankle fusion and open reduction for the T group as surgeon preferentially chose below ankle (BA) procedures for the HE group. Before matching, all co-variates showed heterogeneity. With caliper at 0.05, SDM’s of all co-variates were below 0.10.
All continuous outcomes were non-parametric and were analyzed using Mann Whitney U tests. The outcomes and E-values of any statistically significant outcomes were summarized in Table 3.
| Pre-match1 | Post-match2 | Mean difference or odds ratio3 (95%CI) | P value | E value (5%CL) | |||
| Traditional (n = 553) | High efficiency (n = 838) | Traditional (n = 429) | High efficiency (n = 429) | ||||
| Total recovery time (minute), median [IQR] | 133 [102-169] | 68 [51-90] | 133 [100-171] | 67 [49-88] | -63 (-69 to -57) | < 0.001a | 6.2 |
| Preoperative time (minute), median [IQR] | 40 [32-54] | 42 [31-58] | 39 [32-52] | 41 [31-59] | -2 (-4 to 1) | 0.17 | |
| Operating time (minute), median [IQR] | 59 [43-76] | 40 [27-52] | 59 [43-77] | 39 [27-51] | -20 (-23 to -17) | < 0.001a | 4.2 |
| Total length of stay (minute), median [IQR] | 324 [279-380] | 238 [203-275] | 320 [275-378] | 236 [205-273] | -84 (-92 to -75) | < 0.001a | 5.7 |
| Phase 1 recovery utilization, n/total, n (%) | 458/553 (82.8) | 45/838 (5.4) | 403 (93.4) | 26 (6.1) | 0.016 (0.010-0.026) | < 0.001a | 15.3 |
| Opioid utilization, n/total, n (%) | 175/553 (31.6) | 87/745 (11.7) | 139 (32.4) | 45 (10.5) | 0.24 (0.17-0.36) | < 0.001a | 3.5 |
In the primary outcome, total postoperative recovery time, there was an associated reduction of 63 minutes (95%CI: -69 to -57) when patients go through the HE pathway. There was also an associated reduction in OR time of 20 minutes (95%CI: -23 to -17) and total hospital length of stay of 84 minutes (95%CI: -92 to -75). There was no difference detected in the preoperative time between the two setups. The odds ratio for phase one recovery utilization in HE group was 0.016 (95%CI: 0.010-0.026) and for opioid utilization 0.24 (95%CI: 0.17-0.36).
There was a higher proportion of ankle fusion and ankle open reduction in the T group, which could be associated with longer perioperative duration whereas the HE group saw more hardware removal. Therefore, we performed a subgroup analysis based on BA or at and AA surgery. We followed the same matching algorithm on the pre-matched population.
Both subgroups had SDM’s in all covariates below 0.1 at a caliper of 0.1. The pre- and post-match demographics and distribution of surgical procedures were listed in Tables 4 and 5.
| Pre-match | Post-match | |||||
| Traditional | High efficiency | SD | Traditional | High efficiency | SD | |
| Below ankle | n = 317 | n = 718 | n = 312 | n = 312 | ||
| Female, n (%) | 224 (70.1) | 545 (75.9) | 0.12 | 220 (70.5) | 230 (73.7) | 0.07 |
| Age (year), mean (SD) | 56.9 (13.4) | 57.5 (13.1) | 0.04 | 56.8 (13.5) | 57.3 (12.9) | 0.05 |
| BMI (kg/m2), mean (SD) | 29.7 (6.5) | 28.0 (5.6) | 0.30 | 29.3 (6.0) | 28.9 (6.1) | 0.07 |
| ASA I and II, n (%) | 198 (62.4) | 522 (72.7) | 0.23 | 198 (63.5) | 200 (64.1) | 0.04 |
| Above ankle | n = 236 | n = 120 | n = 114 | n = 114 | ||
| Female, n (%) | 118 (50.0) | 74 (61.7) | 0.24 | 68 (59.6) | 70 (61.4) | 0.04 |
| Age (year), mean (SD) | 46.1 (15.8) | 46.5 (16.6) | 0.03 | 45.6 (16.2) | 45.8 (16.2) | 0.01 |
| BMI (kg/m2), mean (SD) | 29.2 (6.4) | 28.4 (5.7) | 0.15 | 28.8 (6.1) | 28.6 (5.6) | 0.03 |
| ASA I and II, n (%) | 182 (77.1) | 100 (83.3) | 0.17 | 98 (86.0) | 96 (84.2) | 0.05 |
| Traditional | High efficiency | |
| Below ankle | n = 312 | n = 312 |
| Soft tissue excision | 14 (4.5) | 15 (4.8) |
| Toe or foot hardware removal | 26 (8.3) | 27 (8.7) |
| Toe or foot arthrodesis | 141 (45.2) | 130 (41.2) |
| Toe or foot open reduction | 17 (5.4) | 24 (7.7) |
| Toe or foot osteotomy | 81 (26.0) | 111 (35.6) |
| Foot tendon repair | 33 (10.6) | 5 (1.6) |
| At or above ankle | n = 116 | n = 116 |
| Ankle arthroscopy | 10 (8.6) | 6 (5.2) |
| Ankle or tibial hardware removal | 19 (16.4) | 96 (82.8) |
| Ankle arthrodesis | 14 (12.1) | 0 (0) |
| Ankle ligament repair | 3 (2.6) | 1 (0.9) |
| Ankle or tibial osteotomy | 14 (12.1) | 2 (1.7) |
| Ankle open reduction | 56 (48.3) | 11 (9.5) |
The AA subgroups were younger compared to their BA counterparts, reflecting trauma as a cause of their presentation. Other between and within group characteristics appeared similar. The outcomes from the matched subgroups were listed in Tables 6, 7 and 8. Associated reductions were observed in both subgroups in the postoperative recovery time, OR time, total length of stay, phase one recovery utilization and postoperative opioid consumption when the HE pathway was employed.
| Pre-match1 | Post-match2 | Mean difference (95%CI) | P value3 | E value (5%CL) | |||
| Traditional (n = 317) | High efficiency | Traditional (n = 312) | High efficiency | ||||
| Total recovery time (minute), median [IQR] | 137 [101-173] | 69 [51-92] | 137 [101-173] | 68 [51-92] | -63 [-70 to -56] | < 0.001a | 5.8 |
| Preoperative time (minute), median [IQR] | 39 [32-51] | 42 [31-58] | 40 [32-51] | 42 [33-56] | -2 [-5 to 1] | 0.12 | 3.5 |
| Operating time (minute), median [IQR] | 59 [41-77] | 41 [28-52] | 59 [41-77] | 41 [28-54] | -17 [-20 to -13] | < 0.001a | |
| Total length of stay (minute), median [IQR] | 321 [278-378] | 240 [204-275] | 321 [278-378] | 242 [203-271] | -84 [-94 to -74] | < 0.001a | 5.8 |
| Phase 1 recovery utilization, n (%) | 249 (78.5) | 32 (4.5) | 245 (78.5) | 15 (4.8) | 0.014 (0.007-0.025) | < 0.001a | 16.4 |
| Opioid utilization, n (%) | 96 (30.2) | 71 (9.9) | 96 (30.8) | 30 (9.6) | 0.24 (0.15-0.38) | < 0.001a | 3.5 |
| Pre-match1 | Post-match2 | Mean difference (95%CI) | P value | E value (5%CL) | |||
| Traditional (n = 235) | High efficiency | Traditional (n = 116) | High efficiency | ||||
| Total recovery time (minute), median [IQR] | 130 [103-166] | 60 [48-82] | 131 [103-166] | 60 [48-81] | -67 (-77 to -56) | < 0.001 | 7.9 (5.9) |
| Preoperative time (minute), median [IQR] | 42 [32-59] | 42 [31-59] | 41 [33-59] | 41 [31-60] | 0 (-5 to 5) | 0.97 | 4.6 (3.4) |
| Operating time (minute), median [IQR] | 59 [46-73] | 34 [26-45] | 58 [44-78] | 35 [27-46] | -22 (-27 to -17) | < 0.001 | |
| Total length of stay (minute), median [IQR] | 330 [281-383] | 225 [200-274] | 327 [286-378] | 226 [200-274] | -101 (-117 to -82) | < 0.001 | 7.6 (5.6) |
| Recovery events | Traditional | High efficiency | Traditional | High efficiency | Odds ratio (95%CI) | P value1 | E value (5%CL) |
| Phase 1 recovery utilization, n/total | 209 (88.9) | 13 (10.8) | 98 (84.5) | 12 (10.3) | 0.022 (0.009-0.049) | < 0.001a | 13.0 (8.5) |
| Opioid utilization, n/total | 79 (33.6) | 16 (13.3) | 44 (37.9) | 16 (13.8) | 0.26 (0.13-0.52) | < 0.001a | 3.3 (2.1) |
Our study demonstrated an associated decrease in length of stay in each part of the perioperative journey except preoperative time. There was no currently published fast track pathway for minor orthopedic lower limb surgery to our knowledge. Studies on lower limb orthopedic surgery focused on peripheral nerve block in addition to general anesthesia instead of using nerve blocks as the sole anesthetic technique. Womble et al[8] in their retrospective study, analyzed 9459 patients undergoing ankle reduction surgery found regional anesthesia found a modest reduction in operative time when regional anesthesia was added to general anesthesia (66 minutes vs 72 minutes, P < 0.001) for outpatient surgery. Polshin et al[5] included 57040 patients undergoing orthopedic and non-orthopedic surgery in their retrospective study and found the use of peripheral nerve block in addition to general anesthesia reduced phase 1 recovery stay by 7.3 minutes (95%CI: 6.1 minutes to 8.6 minutes, P < 0.001). We believe we were able to achieve a significant reduction in hospital length of stay and each stage of the perioperative journey by adopting a multidisciplinary strategy.
Many enhanced recovery after surgery (ERAS) protocols focused on major orthopedic surgery such as joint replacement. The major concepts of orthopedic ERAS protocols included preoperative education, optimization, intraoperative maintenance of homeostasis, minimizing surgical trauma, postoperative early ambulation and minimizing nausea and vomiting and multimodal opioid-sparing analgesia[9]. Although our pathway focused on minor lower limb orthopedic surgery, it shares many concepts with the ERAS protocols. Patients were carefully selected to ensure they were optimized, so the risk of medical complications was minimized. Using a standardized surgical and anesthetic protocol ensured familiarity and predictability with postoperative outcomes. Adopting surgical peripheral nerve blocks and applying opioid-sparing multimodal analgesia further reduced risk of pain and opioid related adverse effects[7]. A number of studies focused on the effect of regional anesthesia in ambulatory surgery. Carli et al[10] noted peripheral nerve blocks enabled fast track surgical pathways in non-orthopedic surgery. Avoidance of general anesthesia and opioids and therefore the adverse effect of nausea, vomiting, drowsiness were attributed factors. However, our study was unique in that it was the first in applying a comprehensive surgical pathway to minor orthopedic procedures.
As a retrospective study, a causal relationship between the HE pathway and reduced postoperative recovery time could not be established and some confounders may remain unbalanced. The care team could be motivated to perform more efficiently when patients were assigned to the HE pathway. Patient selection for the HE pathway was at the surgeons’ discretion. It was likely that more complex and intensive procedures such as ankle open reduction and fusions were left out of the pathway. In the BA subgroup, where surgery were more congruent, similar magnitudes of time reduction were still observed. Some factors that may increase postoperative stay included a history of diabetes, prolonged OR time and social support, were not included in our matching model. The E-values for statistically significant results were high. Taken together, the association between reduced perioperative stay and the HE pathway was robust. A prospective study utilizing our pathway, by multiple facilities, may further consolidate the validity in an external setting.
Cost benefit of this pathway had been published by Chohan et al[11]. The HE pathway cost 60% less when compared to T care. No difference in patient satisfaction or compromised health outcomes were detected. While our study focused on lower limb orthopedic surgery, similar models employing general anesthesia have been applied to hernia and thyroid surgery in our institution[12,13]. The pathway utilized a preoperative block room that may not be available in all hospitals. This was likely crucial for the success for this pathway as the precious OR time could be saved for the actual surgery[14]. There were also other important safety and recovery metrics such as emergency room visit, rebound pain and patient experience that were not recorded in this study.
In response to the surgical backlog, the Ontario Medical Association proposed establishing standalone Integrated Ambulatory Centres (IAC) to perform lower complexity cases outside of hospitals, but the specific detail of the care model was not discussed[1]. We feel our HE care pathway would fit well into the vision of the IAC. Patient selection will help reduce the risk of postoperative complication, prolonged recovery and unexpected admission, leaving more complicated patients in acute care hospitals[15]. Standardization of surgical instrument can facilitate setting up and sterilization where the on-site processing capability may be limited[11]. Utilization of peripheral nerve blocks and avoidance of general anesthesia may permit the use of anesthesia assistants for intraoperative care, relieving anesthesiologists to perform more complicated cases in other OR[16]. Likewise, eliminating the need for scrub nurse and bypassing phase one recovery, therefore enabling higher patient to nurse ratio, can help reduce the stress on regional health care human resource.
Our HE care model offers a compelling solution to address the current surgical backlog and the human resources shortage. By carefully selecting and educating patients, utilizing preoperative nerve blocks and standardizing surgical instruments we achieved a reduction in postoperative recovery time, OR time and total hospital length of stay all without increasing preoperative time. A key benefit in our model was the reduced nursing requirement. Such care model can serve as the basis of the OMA’s vision of IAC.
| 1. | Ontario Medical Association. A Three-Stage Approach to Addressing Ontario's Critical Surgical and Procedural Wait Times. Available from: https://www.oma.org/uploadedfiles/oma/media/public/addressing-wait-times-proposal.pdf. |
| 2. | Beattie S. Ontario health-care workers warn of "brutal" nurse shortage as hospitals brace for 4th wave Social Sharing. Available from: https://www.cbc.ca/news/canada/toronto/ontario-health-care-workers-warn-of-brutal-nurse-shortage-as-hospitals-brace-for-4th-wave-1.6150255. |
| 3. | Denis A, Montreuil J, Harvey EJ, Berry GK, Reindl R, Bernstein M. Cancellations and delays of emergent orthopedic operations at a Canadian level 1 trauma centre. Can J Surg. 2022;65:E382-E387. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 4. | Koyle MA, AlQarni N, Odeh R, Butt H, Alkahtani MM, Konstant L, Pendergast L, Koyle LCC, Baker GR. Reduction and standardization of surgical instruments in pediatric inguinal hernia repair. J Pediatr Urol. 2018;14:20-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Polshin V, Petro J, Wachtendorf LJ, Hammer M, Simopoulos T, Eikermann M, Santer P. Effect of peripheral nerve blocks on postanesthesia care unit length of stay in patients undergoing ambulatory surgery: a retrospective cohort study. Reg Anesth Pain Med. 2021;46:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Bodrogi A, Dervin GF, Beaulé PE. Management of patients undergoing same-day discharge primary total hip and knee arthroplasty. CMAJ. 2020;192:E34-E39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 7. | Awad IT, Chung F. Factors affecting recovery and discharge following ambulatory surgery. Can J Anaesth. 2006;53:858-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 94] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Womble TN, Comadoll SM, Dugan AJ, Davenport DL, Ali SZ, Srinath A, Matuszewski PE, Aneja A. Is supplemental regional anesthesia associated with more complications and readmissions after ankle fracture surgery in the inpatient and outpatient setting? Foot Ankle Surg. 2021;27:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Riga M, Altsitzioglou P, Saranteas T, Mavrogenis AF. Enhanced recovery after surgery (ERAS) protocols for total joint replacement surgery. SICOT J. 2023;9:E1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 10. | Carli F, Kehlet H, Baldini G, Steel A, McRae K, Slinger P, Hemmerling T, Salinas F, Neal JM. Evidence basis for regional anesthesia in multidisciplinary fast-track surgical care pathways. Reg Anesth Pain Med. 2011;36:63-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 124] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 11. | Chohan M, Bihari A, Tieszer C, MacNevin M, Churcher C, Vandersluis C, Cassar F, Lin C, Schemitsch E, Sanders D, Lawendy AR. Evaluation of a tiered operating room strategy at an academic centre: comparing high-efficiency and conventional operating rooms. Can J Surg. 2022;65:E739-E748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Ernst H, Sowerby L, Sahovaler A, Macneil D, Nichols A, Yoo J, Hilsden R, Strychowsky J, Fung K. Rapid standardized operating rooms (RAPSTOR) in thyroid and parathyroid surgery. J Otolaryngol Head Neck Surg. 2021;50:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | 2017 Canadian Surgery Forum Abstracts. Can J Surg. 2017;60:S109-S181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | McHardy P, Wong P. How to Build a Block Room: A Canadian Perspective. American Society of Regoinal Anesthesia. Available from: https://www.asra.com/news-publications/asra-newsletter/newsletter-item/asra-news/2019/08/19/how-to-build-a-block-room-a-canadian-perspective. |
| 15. | Rajan N, Rosero EB, Joshi GP. Patient Selection for Adult Ambulatory Surgery: A Narrative Review. Anesth Analg. 2021;133:1415-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 16. | Canadian Society of Respiratory Therapists. National Competency Framework In Anesthesia Assistance. Available from: https://www.cas.ca/CASAssets/Documents/Practice-Resources/Reports-Position-Papers/FR/125_National-Educational-Framework.pdf. |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/