Published online Mar 18, 2024. doi: 10.5312/wjo.v15.i3.257
Peer-review started: November 1, 2023
First decision: November 29, 2023
Revised: December 13, 2023
Accepted: January 16, 2024
Article in press: January 16, 2024
Published online: March 18, 2024
Processing time: 134 Days and 12 Hours
In recent years, there has been an increase in the number of total hip arthroplasty procedures in the younger patient population. This active group has higher expectations of their prosthesis in comparison to the older population, and there is a greater physical demand for the prosthesis. Short femoral stems were in
To determine the 5-year survival of the Optimys hip stem.
This was a prospective multicenter cohort study of 500 patients conducted in two hospitals in the Netherlands. All patients received the Optimys short stem (Mathys Ltd, Bettlach, Switzerland). The primary outcome measure was survival of the hip stem, with revision as the endpoint. The secondary outcome measurements included patient-reported outcome measures (PROMs). Kaplan-Meier analysis was used to calculate the 5-year survival rate. Log-minus-log transformation was performed to calculate the 95% confidence interval (95%CI). Mixed model analyses were performed to assess the course of the PROMs during the 1st 2 years after surgery. Analyses were modeled separately for the 1st and 2nd years to calculate the yearly change in PROMs during both follow-up periods with accompanying 95%CIs.
The mean age of the total 500 patients was 62.3 years (standard deviation: 10.6) and 202 were male (40%). At a median follow-up of 5.5 years (interquartile range: 4.5-6.7), 7 patients were deceased and 6 revisions were registered, for infection (n = 3), subsidence (n = 2) and malposition (n = 1). This resulted in an overall 5-year survival of 98.8% (95%CI: 97.3-99.5). If infection was left out as reason for revision, a stem survival of 99.4% (95%CI: 98.1-99.8) was seen. Baseline questionnaires were completed by 471 patients (94%), 317 patients (63%) completed the 1-year follow-up questionnaires and 233 patients (47%) completed the 2-year follow-up. Both outcome measures significantly improved across all domains in the 1st year after the operation (P < 0.03 for all domains). In the 2nd year after surgery, no significant changes were observed in any domain in comparison to the 1-year follow-up.
The Optimys stem has a 5-year survival of 98.8%. Patient-reported outcome measures increased significantly in the 1st postoperative year with stabilization at the 2-year follow-up.
Core Tip: The Optimys hip stem showed an excellent 5-year survival of 98.9%, and when excluding infections this was 99.4%. This is in line with the earlier results of the Roentgen Stereophotogrammetric analysis study completed by our group, and we expect it to be in line with the National Institute for Health and Care Excellence criteria on total hip arthroplasty for the 10-year follow-up. This study showed that in a large, varied patient population there is similar survival as other cohorts with short femoral stems.
- Citation: Hamans B, de Waard S, Kaarsemaker S, Janssen ERC, Sierevelt IN, Kerkhoffs GMMJ, Haverkamp D. Mid-term survival of the Optimys short stem: A prospective case series of 500 patients. World J Orthop 2024; 15(3): 257-265
- URL: https://www.wjgnet.com/2218-5836/full/v15/i3/257.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i3.257
Osteoarthritis has become more prevalent in recent years due to a growing and aging population[1]. According to the Dutch Arthroplasty Registry (LROI), the yearly number of total hip arthroplasties (THA) has increased from approximately 23.000 to 31.500 between 2010 and 2021[2]. As the total number of THAs has increased over the years, the number of younger patients (< 65 years) receiving THA has also increased to 20% of the total[2]. This younger group has a more active lifestyle, which results in a greater demand for hip prostheses. This makes them more susceptible to revision of their total hip, as there is an increase in wear and/or loosening of the components due to increased forces[3-7].
In recent decades, a short, curved stem as a femoral component in THA has been introduced to the market and has become more popular for implantation in this younger patient population. The philosophy behind short stems is bone-stock preservation in the proximal femur due to more proximal loading and restoration of the patient’s specific anatomy[7-10]. With the introduction of new implants, it is important to monitor survival. The Optimys stem, manufactured by Mathys Ltd. Bettlach, is a meta-diaphyseal anchoring short stem and has been on the market since 2010. An earlier radiostereometric analysis study of the Optimys hip stem showed excellent results in the stabilization of the Optimys short stem at 2 years of follow-up[11]. At this time, to the best of the authors’ knowledge, mid-term survival and functional outcomes have been described in only two studies, and the Optimys has an Orthopaedic Data Evaluation Panel (ODEP) rating of 7A[12].
Therefore, the aim of this study was to determine the mid-term survival of the Optimys hip stem in a large, varied patient population and to assess functional outcomes and quality of life in this patient population.
This study was a prospective multicenter cohort study conducted in two centers in the Netherlands, the Xpert Clinics Orthopedie Amsterdam and VieCuri Medisch Centrum Venlo. This study was submitted and approved by the medical ethics research committee of Amsterdam UMC, location AMC Amsterdam (NL47055.048.13). Patients scheduled for THA between January 2014 and December 2021 were asked to participate. All patients suffered from primary or secondary osteoarthritis, which included coxarthrosis, dysplastic coxarthrosis, rheumatoid arthritis, necrosis of the head of the femur, or post-traumatic coxarthrosis. Patients were excluded in cases of revision surgery, an American Society of Anesthesiologists score > 3, sepsis, or malignant tumors. After confirmation of participation, all patients gave informed consent before they were included in this study.
Patients returned for a clinical follow-up at 6 wk, 3 months, and 1 year post surgery. Hereafter, revision status was verified using patient files and the LROI. Prior to the operation, at 6 wk, 3 months, 6 months, 1 year, and 2 years post-surgery, patients were asked to fill out a questionnaire.
All patients received the Optimys short stem (Mathys Ltd, Bettlach, Switzerland). The Optimys stem is a calcar-guided short stem with a curved design. It is made of Ti6Al4V (titanium-aluminum-vanadium), according to ISO 5832-3, with a titan plasma spray and calcium phosphate coating for better ingrowth of the stem into the bone. The approach during THA was left to the surgeon’s preference (anterior, anterolateral, or straight lateral). The day of the surgery or 1 d postoperative, patients were mobilized using two crutches and were allowed full weight bearing (Figure 1).
The primary outcome measure was survival of the hip stem, with revision as the endpoint. Revision was defined as a surgical procedure in which all or part of the previous implanted prosthesis was replaced. Reasons for revision were described. The secondary outcome measurements included patient-reported outcome measures (PROMs), which consisted of the Hip Disability and Osteoarthritis Outcomes Score (HOOS), the 36-item Short Form (SF-36), and a 5-point Likert scale for satisfaction (at 2 years post-surgery)[13-16].
IBM SPSS Statistics 26 (IBM Corp., Armonk, NY, United States) was used for the statistical analysis. In the case of a normal distribution, all continuous outcomes were reported as the means and standard deviation (SD). In the case of a skewed distribution, the outcomes were presented as the median and interquartile range. Categorial outcomes are presented as frequencies with accompanying percentages. Kaplan-Meier analysis was used to calculate the 5-year survival rate by censoring patients at death or at the end of the observation period before 5 years. Log-minus-log transformation was performed to calculate the 95% confidence interval (95%CI).
Second, mixed model analyses were performed to assess the course of the PROMs during the 1st 2 years after surgery. Analyses were modeled separately for the 1st and 2nd years to calculate the yearly change in PROMs during both follow-up periods with accompanying 95%CIs. A P value of < 0.05 was considered statistically significant for all analyses. As PROM analyses were secondary, no correction for multiple testing was performed. Due to considerable loss of patients filling out PROMs during follow-up, a sensitivity analysis was performed according to a last observation carried forward protocol to avoid overestimation of the effect.
A total of 500 consecutive patients were included in this study, of whom 202 (40%) were male. The mean age was 62.3 years (SD: 10.6), and the mean body mass index was 26.5 kg/m2 (SD: 4.1) (Table 1).
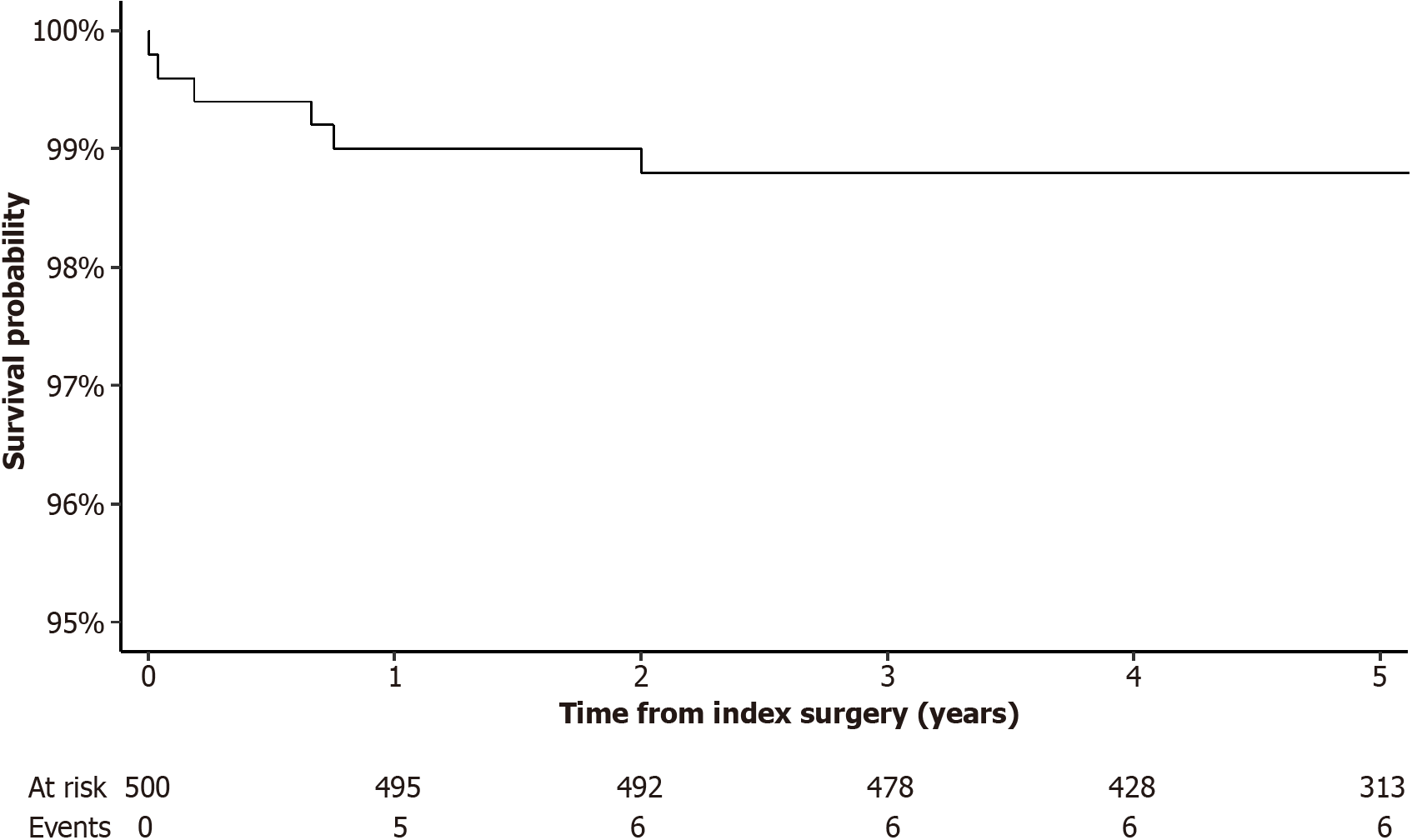
At a median follow-up of 5.5 years (interquartile range: 4.5-6.7), 7 patients were deceased with their prosthesis in situ, and 6 revisions were registered. Infection was the reason for revision in 3 patients, and they were initially treated with debridement, antibiotics, and implant retention. In 1 patient, the debridement, antibiotics, and implant retention failed, and a two-stage revision was needed. Furthermore, 2 patients were revised due to subsidence of the stem (due to an undersized stem but with good fixation), and 1 patient was revised because of malposition of the stem. This resulted in an overall 5-year survival of 98.8% (95%CI: 97.3, 99.5) in the study population (Figure 2). If infection was left out as the reason for revision, a stem survival of 99.4% (95%CI: 98.1, 99.8) was seen, with no cases of aseptic loosening.
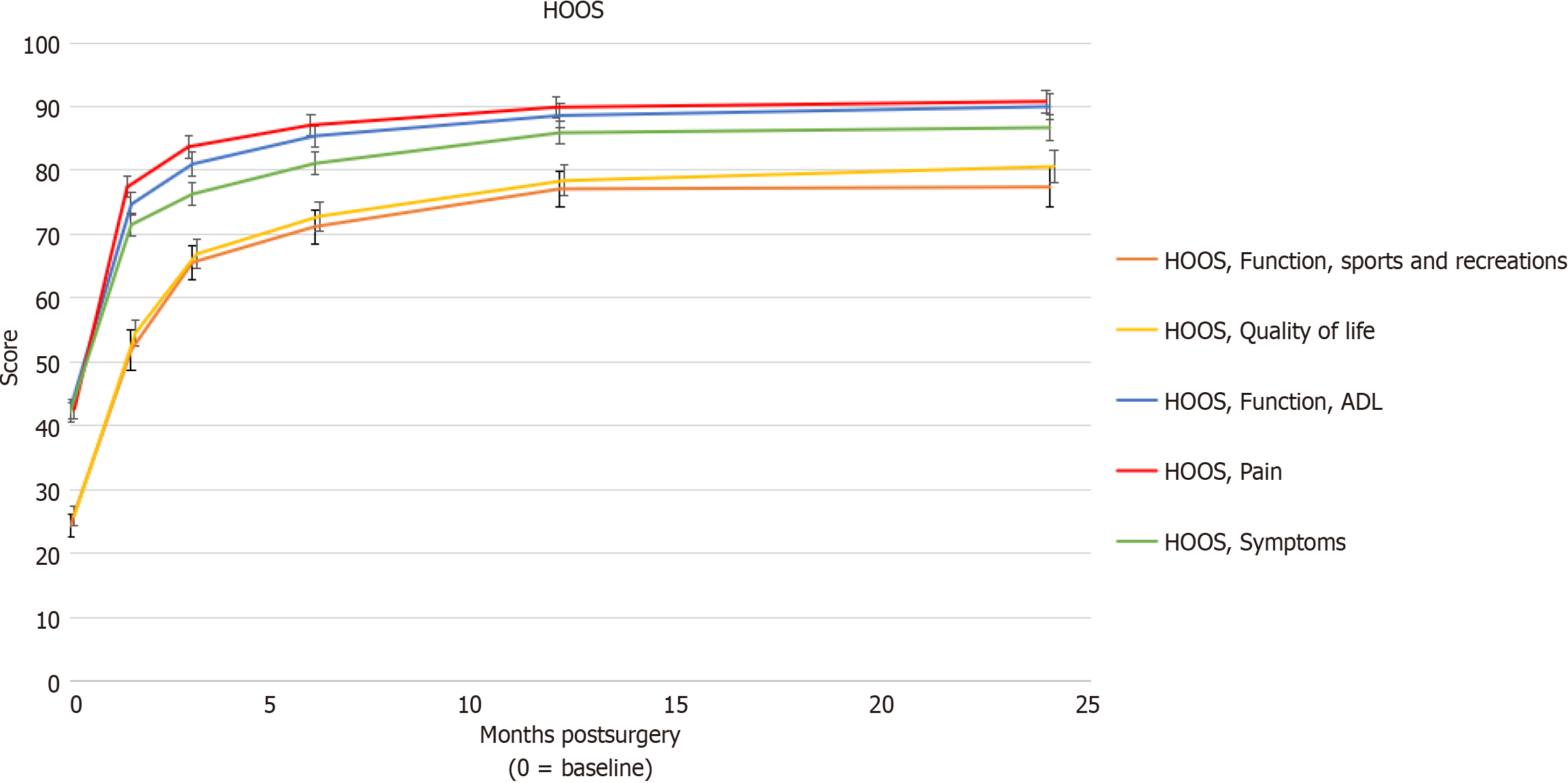
Of the 500 included patients, 471 patients (94%) completed the baseline questionnaires, and 317 patients (63%) completed the 1-year follow-up questionnaires. At the 2-year follow-up, this number had decreased to 233 patients (47%) (Table 2). The HOOS and SF-36 scores at all follow-up time points are presented in Table 2. Both outcome measures significantly improved across all domains in the 1st year after the operation (P < 0.03 for all domains). In the 2nd year after surgery, no significant changes were observed in any domain in comparison to the 1-year follow-up (Table 3 and Figure 3). Although sensitivity analysis showed smaller effects during the 1st year, the same comparable effect was observed during the 2-year follow-up (Supplementary Tables 1 and 2).
| Outcome | Baseline, n = 471 | 6 wk, n = 388 | 3 months, n = 371 | 6 months, n = 355 | 1 yr, n = 317 | 2 yr, n = 233 | |
| HOOS | |||||||
| Symptoms | 42.1 (18.1) | 71.6 (18.2) | 76.3 (17.9) | 81.1 (17.7) | 85.9 (16.2) | 85.9 (16.7) | |
| Pain | 42.5 (16.5) | 77.4 (16.7) | 83.7 (16.6) | 87.1 (15.8) | 89.6 (15.0) | 90.2 (14.7) | |
| ADL | 42.6 (17.5) | 74.7 (17.8) | 81.0 (17.8) | 85.4 (16.1) | 88.6 (16.4) | 89.5 (15.4) | |
| Sports and recreation | 24.3 (19.6) | 51.9 (26.8) | 65.6 (25.1) | 71.2 (24.9) | 77.1 (24.2) | 77.0 (24.9) | |
| Quality of life | 25.9 (15.7) | 54.6 (20.4) | 66.9 (22.3) | 72.8 (21.8) | 78.4 (21.6) | 80.0 (21.0) | |
| SF 36 | |||||||
| Physical functioning | 35.6 (18.6) | 57.8 (22.8) | 69.6 (22.4) | 74.5 (22.4) | 78.7 (22.4) | 81.8 (19.8) | |
| Role physical | 23.3 (35.7) | 29.5 (36.0) | 57.5 (42.5) | 71.0 (40.4) | 81.0 (34.9) | 80.8 (34.4) | |
| Bodily pain | 35.7 (17.2) | 55.9 (22.1) | 70.7 (22.1) | 75.9 (21.2) | 80.6 (22.4) | 80.8 (22.8) | |
| Social functioning | 61.0 (26.0) | 68.1 (26.0) | 79.9 (23.8) | 85.0 (21.0) | 88.5 (19.3) | 87.7 (20.4) | |
| Mental health | 73.4 (17.8) | 80.2 (16.2) | 82.0 (16.3) | 81.8 (15.7) | 83.1 (15.0) | 83.0 (14.3) | |
| Role emotional | 63.3 (43.7) | 67.5 (41.5) | 77.2 (38.2) | 84.1 (33.6) | 89.6 (27.0) | 90.0 (27.2) | |
| Vitality | 57.3 (19.9) | 66.0 (18.4) | 69.5 (18.4) | 70.8 (18.2) | 72.9 (17.4) | 73.9 (16.7) | |
| General health perceptions | 66.6 (18.5) | 73.5 (17.9) | 72.4 (19.0) | 70.4 (19.7) | 72.0 (19.9) | 73.4 (18.5) | |
| Outcome measure | 1st yr | 2nd yr | |||
| β (95%CI)1 | P value | β (95%CI)1 | P value | ||
| HOOS | |||||
| Symptoms | 34.8 (31.9, 37.6) | < 0.001 | 0.7 (-0.9, 2.3) | 0.38 | |
| Pain | 36.8 (34.0, 39.7) | < 0.001 | 0.3 (-1.0, 1.6) | 0.63 | |
| ADL | 36.2 (33.3, 39.1) | < 0.001 | 0.9 (-0.6, 2.5) | 0.24 | |
| Sports and recreation | 43.3 (39.7, 46.9) | < 0.001 | -0.1 (-2.6, 2.4) | 0.93 | |
| Quality of life | 41.8 (38.7, 45.0) | < 0.001 | 1.5 (-0.7, 3.8) | 0.18 | |
| SF-36 | |||||
| Physical functioning | 34.5 (31.4, 37.7) | < 0.001 | 0.8 (-1.7, 3.4) | 0.56 | |
| Role physical | 54.4 (49.0, 59.7) | < 0.001 | -1.2 (-6.2, 3.8) | 0.64 | |
| Bodily pain | 36.5 (33.4, 39.6) | < 0.001 | -0.4 (-3.3, 2.6) | 0.80 | |
| Social functioning | 22.8 (19.5, 26.0) | < 0.001 | -0.9 (-3.5, 1.7) | 0.49 | |
| Mental health | 6.1 (4.1, 8.1) | < 0.001 | -0.7 (-2.4, 1.1) | 0.45 | |
| Role emotional | 23.3 (18.1, 28.5) | < 0.001 | 0.0 (-4.4, 4.5) | 1.00 | |
| Vitality | 10.8 (8.5, 13.1) | < 0.001 | -0.6 (-2.6, 1.4) | 0.56 | |
| General health perceptions | 2.4 (0.3, 4.6) | 0.03 | 0.1 (-1.7, 1.8) | 0.95 | |
At the 2-year follow-up, 210 (42%) had completed the satisfaction score with results as follows: 132 patients (63%) were very satisfied; 60 patients (29%) were satisfied; 9 patients (4%) were neutral; 7 patients (3%) were unsatisfied; and 2 patients (1%) were very unsatisfied with their hip prosthesis.
This study, which included 500 patients, showed a high survival rate of 98.8% at the 5-year follow-up mark with 6 revisions. The reasons for overall revision were an infection (0.6%) in three cases, subsidence of the stem (0.4%) in two cases, and malposition of the stem (0.2%) in one case. During the revision surgery in the two cases with subsidence, it was noted that the femoral stem had good fixation in the femur, confirming that the stem was undersized during the primary placement and was now settled with bone growth around the stem for fixation. If infection as a reason for revision was left out, a survival of 99.4% of the Optimys stem was seen. No aseptic loosening was observed in this cohort.
Furthermore, a significant increase in the PROMs at the 1st year of follow-up was observed. The HOOS scores increased by 34.8 to 43.3 points, and the SF-36 scores increased by 2.4 to 54.5 points across all subscales. After the 1st year, no significant changes in either score were observed. Almost all patients (91.4%) were very satisfied or satisfied with their THA.
The National Institute for Health and Care Excellence (NICE) criteria state that total hip replacements for patients with arthritis have revision rates or projected revision rates of 5% or less after 10 years of follow-up[17]. With a revision rate of almost 99% at the 5-year follow-up, our study results are expected to be in line with these NICE criteria.
In 2022, Kutzner et al[18] published a study on the mid-term results of the Optimys hip stem for 782 patients at 6 years of follow-up. It showed a survival rate of 98.4%, with 26 revisions in total (including infection and acetabular cup malposition), of which 14 were stem revisions. This is comparable to our study with a survival rate of 98.8% and 6 overall revisions, of which 4 were stem revisions in a population of 500 patients.
Furthermore, both studies had comparable baseline characteristics of the patients. Kutzner et al[18] used the Harris Hip Score (HHS) as a functional outcome measure. The HHS is used to evaluate the function of the hip before and after surgery for a range of different disabilities[19]. The outcome showed a large increase in the first 6 months before flattening out. At the 2-year follow-up, the HHS reached a mean of 98.2, meaning that most patients showed an excellent functional outcome after 2 years. This is similar to our study, which indicated consistent excellent survival and functional results among the two different clinics.
Studies on comparable short stems, such as the Nanos and Fitmore stems, are in line with our results. The NANOS stem, produced by Smith and Nephew, is also a calcar-guided short stem and has an ODEP rating of 7A. A study by Ettinger et al[20] presented mid-term results in 65 patients receiving a NANOS short stem at 5 years of follow-up. In this study, the patient population had similar demographics compared to our study population. At the 5-year follow-up, only two infections were registered. As there were no revisions of the stem itself, a survival of 100% was observed. For functional outcomes, this study also used the HHS. The HHS increased from 47.3 before surgery to 97.6 at the final 5-year follow-up.
Another widely used short stem is the Fitmore Hip stem, produced by Zimmer Biomet. It has an ODEP rating of 10A. A study by Thalmann et al[21] presented clinical results in 96 patients at 5 years of follow-up. At the 5-year follow-up, only one revision was seen, resulting in a survival of 99%. The mean HHS increased from 59.3 before the surgery to 93.8 at 5 years of follow-up.
A systematic review by van Oldenrijk et al[22] compared the revision rate of 19 different short stems across 49 studies. These short stems were divided into three groups: Collum; partial collum; and trochanter sparing. In this study, the Optimys stem was classified as a partial collum stem. This group contained eight stem types across 24 studies in 2357 patients. Follow-up ranged from 0.5 years to 11.2 years, with a mean follow-up of 4.0 years and a mean survival rate of 99.3%. Our results for the Optimys stem were in line with these results. The results can also be compared with the trochanter-sparing group, which contained eight stem types across 20 studies in 3628 patients. Follow-up ranged from 0.3-12.0 years, with a mean of 3.4 years and a mean survival of 99.2%. Our results were also in range compared to this group of short stems. The study, however, still used the old NICE benchmark of revision rates of 10% or less at 10 years of follow-up, while the current benchmark as mentioned earlier is 5% or less at 10 years of follow-up.
This study had a few limitations. First, the use of the LROI registry has limited information about the reason for revision. As such, the reason for revision for malposition was not clear, and further information could not be obtained, as the data were anonymous. Second, the number of patients who completed the PROM questionnaire was small. This can especially be seen at the 2-year follow-up. This could lead to a bias of the presented results, as the response rate of patients can depend on the results of their prosthesis. However, as the functional outcome scores in our study did not differ between the 1-year and 2-year follow-ups and a sensitivity analysis showed similar results, it is assumed that not only the patients with lasting complaints of their hip filled out the 2-year follow-up questionnaires. A strong point in this study was the large prospective cohort. A total of 500 patients were followed for a median follow-up of 5.5 years.
Although this study shows a good survival rate at the 5-year follow-up, further research on the Optimys short hip stem is still necessary to include the long-term survival of this hip stem. This cohort will be followed for the long-term survival data.
This study showed a 5-year survival rate of 98.8% for the Optimys hip stem in a population of 500 patients. Functional outcome and quality of life increased significantly in the 1st year after implantation with subsequent stabilization at the 2-year follow-up.
Short stems in total hip arthroplasty are becoming more popular in the younger patient population. The philosophy behind short stems is bone-stock preservation in the proximal femur due to more proximal loading and restoration of the patient’s specific anatomy. As with all new implants on the market, stepwise introduction is needed to avoid a high failure rate in patients. This study contributes to the knowledge of midterm survival data of the Optimys hip stem.
Short hip stems have advantages compared to the widely used conventional stems, especially in the younger and more active patient population. However, long-term survival of the conventional stems is high, so newly introduced implants must have at least a survival rate of 95% at the 10-year follow-up, according to the National Institute for Health and Care Excellence guidelines.
The aim of this study was to determine the mid-term survival of the Optimys hip stem in a large, varied patient population and to assess functional outcomes and quality of life in this patient population. This can show us if the hip stem is an implant that can be commonly used in the daily practice of an orthopedic surgeon. The study can contribute to the fact that this hip stem is safe to implant in a large and varied patient population with an excellent survival rate.
This was a prospective multicenter cohort study conducted in two hospitals in the Netherlands (Amsterdam and Venlo). This gave a large and varied patient population. The primary outcome measure was survival of the hip stem, with revision as the endpoint. Revision was defined as a surgical procedure in which all or part of the previous implanted prosthesis was replaced. Reasons for revision were described. Kaplan-Meier was used for survival rate, by censoring patients at death or at the end of the observation period before 5 years. Log-minus-log transformation was performed to calculate the 95% confidence interval. The secondary outcome measurements included patient-reported outcome measures (PROMs), which consisted of the Hip Disability and Osteoarthritis Outcomes Score, the 36-item Short Form, and a 5-point Likert scale for satisfaction (at 2 years post-surgery). Mixed model analyses were performed to assess the course of the PROMs during the 1st 2 years after surgery. Analyses were modeled separately for the 1st and 2nd years to calculate the yearly change in PROMs during both follow-up periods with accompanying 95% confidence intervals. A P value of < 0.05 was considered statistically significant for all analyses.
The survival rate of the Optimys hip stem at the 5-year follow-up was 98.8% in a group of 500 patients if all revisions were included (n = 6). If infection was left out (n = 3), a survival of 99.4% was seen. The functional outcome and quality of life was significantly improved at the 1-year follow-up and subsequently stabilized at the 2-year follow-up.
Short curved hip stems had a high survival rate at the 5-year follow-up, showing that it is a safe and viable stem for common use in total hip arthroplasty.
Future research includes the long-term follow-up of the Optimys hip stem to determine the survival rate at the 10-year follow-up.
We would like to thank Marjolein Schager for her help in editing the manuscript.
| 1. | Murphy NJ, Eyles JP, Hunter DJ. Hip Osteoarthritis: Etiopathogenesis and Implications for Management. Adv Ther. 2016;33:1921-1946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 174] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 2. | LROI. Annual report 2022, (2022, accessed 06-03 2023). Available from: https://www.lroi-report.nl/. |
| 3. | Swarup I, Marshall AC, Lee YY, Figgie MP. Implant survival and patient-reported outcomes after total hip arthroplasty in young patients with developmental dysplasia of the hip. Hip Int. 2016;26:367-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Swarup I, Shields M, Mayer EN, Hendow CJ, Burket JC, Figgie MP. Outcomes after total hip arthroplasty in young patients with osteonecrosis of the hip. Hip Int. 2017;27:286-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Swarup I, Sutherland R, Burket JC, Figgie MP. Total hip arthroplasty in young patients with post-traumatic arthritis of the hip. Hip Int. 2017;27:546-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, Coyte PC, Wright JG. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51:428-436. [PubMed] |
| 7. | Evans JT, Evans JP, Walker RW, Blom AW, Whitehouse MR, Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393:647-654. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 254] [Cited by in RCA: 399] [Article Influence: 57.0] [Reference Citation Analysis (1)] |
| 8. | de Waard S, van der Vis J, Venema PAHT, Sierevelt IN, Kerkhoffs GMMJ, Haverkamp D. Short-term success of proximal bone stock preservation in short hip stems: a systematic review of the literature. EFORT Open Rev. 2021;6:1040-1051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 9. | Kutzner KP, Kovacevic MP, Roeder C, Rehbein P, Pfeil J. Reconstruction of femoro-acetabular offsets using a short-stem. Int Orthop. 2015;39:1269-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Kutzner KP. Calcar-guided short-stem total hip arthroplasty: Will it be the future standard? Review and perspectives. World J Orthop. 2021;12:534-547. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | de Waard S, Sierevelt IN, Jonker R, Hoornenborg D, van der Vis HM, Kerkhoffs GMMJ, Haverkamp D. The migration pattern and initial stability of the Optimys short stem in total hip arthroplasty: a prospective 2-year follow-up study of 33 patients with RSA. Hip Int. 2021;31:507-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | ODEP. Optimys, (2021, accessed 24-03 2023).Available from: https://www.odep.org.uk/product/optimys/. |
| 13. | de Groot IB, Reijman M, Terwee CB, Bierma-Zeinstra SM, Favejee M, Roos EM, Verhaar JA. Validation of the Dutch version of the Hip disability and Osteoarthritis Outcome Score. Osteoarthritis Cartilage. 2007;15:104-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 146] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 14. | Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, Sprangers MA, te Velde A, Verrips E. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51:1055-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1547] [Cited by in RCA: 1716] [Article Influence: 61.3] [Reference Citation Analysis (0)] |
| 15. | Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23352] [Cited by in RCA: 24541] [Article Influence: 721.8] [Reference Citation Analysis (3)] |
| 16. | Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 620] [Cited by in RCA: 816] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 17. | Kandala NB, Connock M, Pulikottil-Jacob R, Sutcliffe P, Crowther MJ, Grove A, Mistry H, Clarke A. Setting benchmark revision rates for total hip replacement: analysis of registry evidence. BMJ. 2015;350:h756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 18. | Kutzner KP, Maurer SM, Meinecke I, Heers G, Bosson D. Survivorship, complications and patient-reported outcomes in calcar-guided short-stem THA: prospective mid-term multicenter data of the first 879 hips. Arch Orthop Trauma Surg. 2023;143:1049-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 19. | Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737-755. [PubMed] |
| 20. | Ettinger M, Ettinger P, Lerch M, Radtke K, Budde S, Ezechieli M, Becher C, Thorey F. The NANOS short stem in total hip arthroplasty: a mid term follow-up. Hip Int. 2011;21:583-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Thalmann C, Kempter P, Stoffel K, Ziswiler T, Frigg A. Prospective 5-year study with 96 short curved Fitmore™ hip stems shows a high incidence of cortical hypertrophy with no clinical relevance. J Orthop Surg Res. 2019;14:156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | van Oldenrijk J, Molleman J, Klaver M, Poolman RW, Haverkamp D. Revision rate after short-stem total hip arthroplasty: a systematic review of 49 studies. Acta Orthop. 2014;85:250-258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 115] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Netherlands
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kutzner KP, Germany S-Editor: Liu JH L-Editor: Filipodia P-Editor: Zhao YQ