Published online Mar 18, 2024. doi: 10.5312/wjo.v15.i3.247
Peer-review started: October 29, 2023
First decision: December 19, 2023
Revised: January 15, 2024
Accepted: March 4, 2024
Article in press: March 4, 2024
Published online: March 18, 2024
Processing time: 137 Days and 15.4 Hours
Computer-assisted systems obtained an increased interest in orthopaedic surgery over the last years, as they enhance precision compared to conventional hardware. The expansion of computer assistance is evolving with the employment of augmented reality. Yet, the accuracy of augmented reality navigation systems has not been determined.
To examine the accuracy of component alignment and restoration of the affected limb’s mechanical axis in primary total knee arthroplasty (TKA), utilizing an augmented reality navigation system and to assess whether such systems are conspicuously fruitful for an accomplished knee surgeon.
From May 2021 to December 2021, 30 patients, 25 women and five men, under
A statistically significant difference was observed regarding mean expected values and radiographic mea
The results indicate satisfactory postoperative coronal alignment without outliers across all three different implants utilized. Augmented reality navigation systems can bolster orthopaedic surgeons’ accuracy in achieving precise axial alignment. However, further research is required to further evaluate their efficacy and potential.
Core Tip: Augmented reality navigation systems can bolster orthopaedic surgeons’ accuracy in achieving precise axial alignment. Our study unveils compelling evidence showcasing how Augmented Reality (AR) aids surgeons in achieving meticulous axial alignment. This innovative approach significantly enhances accuracy, marking a paradigm shift in surgical procedures. Surgeons leveraging AR navigation exhibit heightened precision, promising improved patient outcomes. Delve into the full manuscript to grasp the groundbreaking findings propelling orthopaedic surgery into a new era of technological advancement. Elevate your understanding and practice within the realm of AR-guided orthopaedic surgery.
- Citation: Sakellariou E, Alevrogiannis P, Alevrogianni F, Galanis A, Vavourakis M, Karampinas P, Gavriil P, Vlamis J, Alevrogiannis S. Single-center experience with Knee+™ augmented reality navigation system in primary total knee arthroplasty. World J Orthop 2024; 15(3): 247-256
- URL: https://www.wjgnet.com/2218-5836/full/v15/i3/247.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i3.247
Total knee arthroplasty (TKA) is indubitably one of the most common orthopaedic procedures ordinarily performed for knee joint osteoarthritis. In the United States, over 600000 TKAs/year are carried out, with the numbers soaring annually[1].
The preponderant goals of TKA are pain relief, joint function restoration and prostheses’ longevity. TKA’s success and artificial joint longevity are achieved with the restoration of limb alignment. Malalignment is recurrently associated with copious long-term complications, such as tibiofemoral and patellofemoral instability, joint stiffness, patellar fractures, increased polyethylene wear and implant loosening[2,3]. Diligent comprehension of the fundamentals and the em
Computer-assisted systems acquired escalated interest in orthopaedic surgery over the last two decades, as they have been demonstrated to ameliorate accuracy over conventional instruments. The next generation of computer assistance is being developed using Augmented Reality (AR). AR systems are broadly considered to exhibit some essential advantages over traditional computer navigation platforms, as they diminish the requirement for massive external detection equ
The growingly prompt evolution of AR technologies features the prospect of attaining the exemplary form of the human-machine interface[6]. Each AR system comprises distinct hardware and software, which provides the surgeon with real-time computer-processed imaging data. AR systems project their information to the surgeon in a way that combines real-life objects with superimposed computer-generated images[7-11]. A system control software utilizes the data from a position-tracking system, transforming the input into images, which are conveyed to a display system, where the amalgamation with the real-scene view transpires in front of the surgeons’ eyes[12,13].
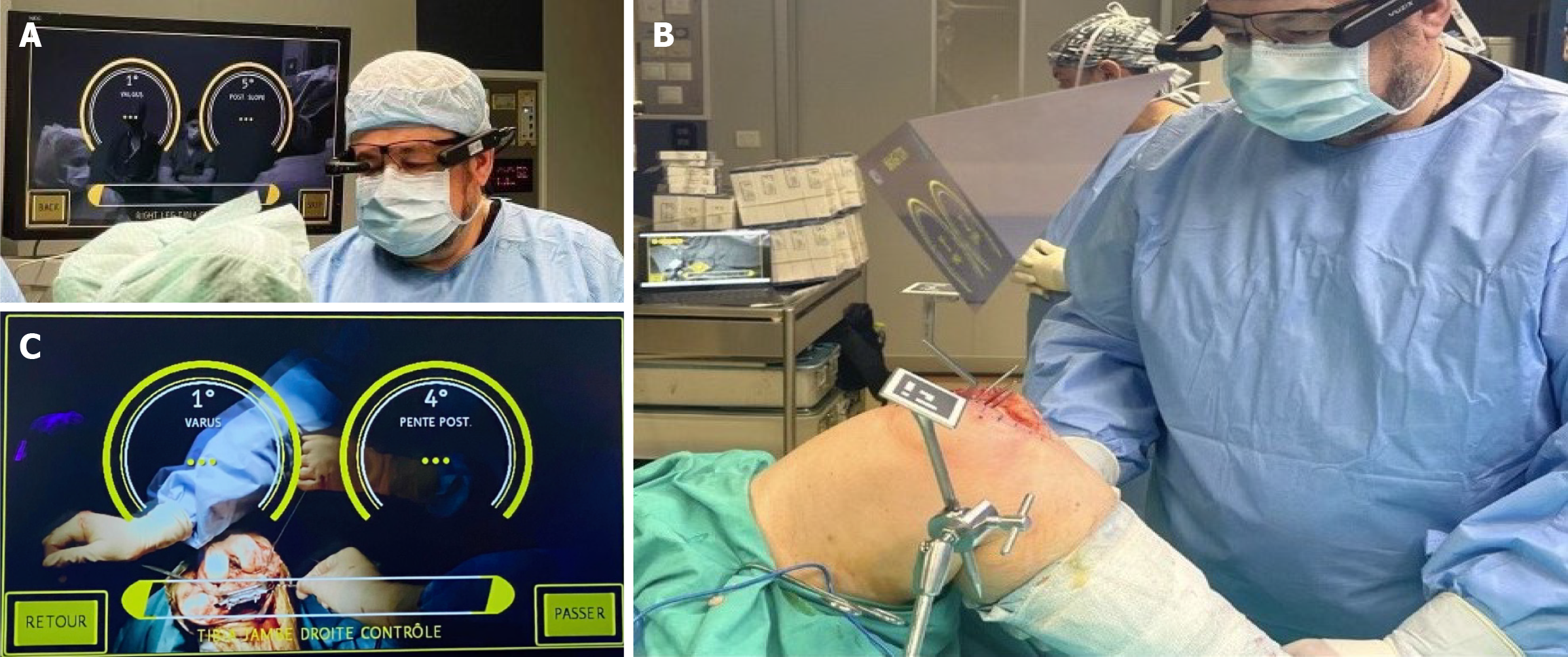
Knee+™ AR navigation system (Pixee medical company, Besancon, France) comprises a pair of smart glasses worn by the surgeon, specific markers (QR-code) connected to the tibial and femoral cutting guides and a central laptop (Figure 1A). The Knee+™ system assists the surgeon in determining reference alignment axes in relation to anatomical landmarks for precise positioning of cutting guides regarding computed mechanical axis (Figure 1B). The smart glasses (Vuzix 2000) enable the surgeon to visualize the tibial and femoral axis superimposed on the patient in real-time during operation, providing meaningful information concerning surgical decisions. With this information, surgeons can accurately specify the distal femoral cut, flexion/extension gaps, the varus/valgus axis, and the tibial cut’s posterior slope. Smart glasses can also offer real-time information to the surgeon regarding the accuracy of osteotomies according to the operative plan, combining the difference in the axis between the anatomical cut and the computerized plan. At this point, the system allows the surgeon to deliberate on the osteotomies and reach a new surgical plan.
This case series endeavors to scrutinize the accurateness of component alignment and restoration of the affected limb’s mechanical axis in primary TKA, employing the Knee+™ system. Additionally, this study aims to evaluate whether such systems are substantively beneficial for a high-experienced knee surgeon.
In our study, 30 patients underwent a primary unilateral TKA for osteoarthritis with AR guidance from May 2021 to December 2021. The average age of patients was 71.6 years, with 5 men and 25 women. Patients were included irrespective of age, diagnosis, deformity and body mass index. Revision surgery cases were excluded.
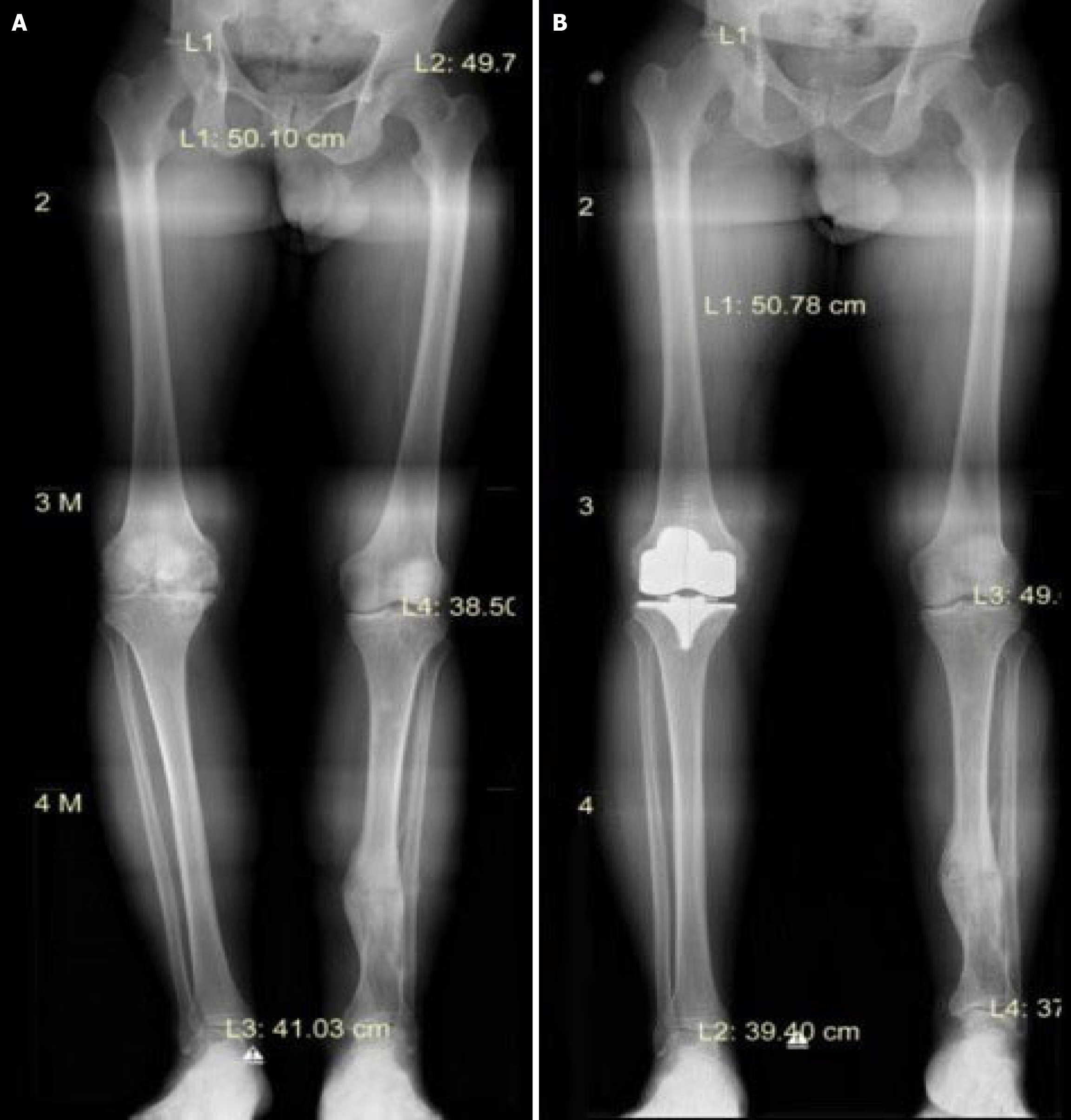
Preoperatively, radiographic exams (simple A/P and lateral knee X-rays) and full leg-length A/P X-rays were performed to all patients to assess the axial limb alignment (Figure 2A). The radiographic examinations were performed in the same center, utilizing the same software protocol. All radiological views were obtained with the patients on standing position. With regard to full leg-length A/P X-rays particulars, the images included in each set of radiographs were hip, knee and ankle views, with each image dimension being 3408 × 3320 pixels and with a resolution of 150 × 150, as well as a full-length lower limb x-ray performed by the same versed radiologist. The digital radiography system employed was the “NOVA FA” (Sedecal, Madrid, Spain), which featured a flat panel detector. The distance between the x-ray source and the patient was 160 cm. This specific system was a linear system in which the x-ray source moved from top to bottom to capture the images. It is pivotal to underline that this special preoperative imaging examination is routinely not necessary for the utilization of Knee+™ system intraoperatively, and we carried out this protocol for the purposes of our study.
All patients were operated on by the same adept orthopaedic surgeon, under combined regional anesthesia and without a tourniquet. The following prostheses were employed: Evolution® Medial-Pivot Knee System/MicroPort Orthopedics (7 cases), BalanSys BICONDYLAR® Knee System/Mathys European Orthopaedics (12 cases) and Vanguard® Complete Knee System/Zimmer Biomet (13 cases).
All operations were conducted with the assistance of the Knee+™ AR navigation system (Pixee medical company, Besancon, France), using a standardized protocol of cutting first the tibial and then the femoral component. Concerning intraoperative soft tissue balance assessment, depending on the type of implant utilized, pertinent spacer blocks were employed for diligent evaluation of flexion and extension gaps in valgus and varus stress.
Acute postoperatively, plain knee X-rays (A/P and lateral) were carried out. Subsequently, all patients were mobilized 2-3 h after the surgery with the aid of physiotherapists specialized in rapid recovery rehabilitation techniques. On the second postoperative day, following intensive physiotherapy sessions, a new full leg-length x-ray was performed in each patient, employing the same radiographic exam protocol as pre-surgery, for confirming the implants’ position, orientation and alignment in the coronal plane (Figure 2B).
We recorded measurements in three steps during the entire procedure for the femoral varus and flexion, for the tibial varus and posterior slope (Figure 1C). At first, we documented the expected values preoperatively after the evaluation of joint deformity and the mechanical axis from the AR system. Afterwards, we recorded the same measurements after each cut intraoperatively, and ultimately, we also measured these values radiologically after the operation.
Lin’s concordance correlation coefficient (CCC) was estimated in terms of statistical analysis. Also, results for Bland and Altman’s limits-of-agreement procedure are provided as the mean of the two values, minus and plus 1.96 standard deviations. CCCs between 0.60 and 0.80 are considered substantial, while coefficients greater than 0.80 are considered excellent. As the discrepancies between the measurements could not be assumed to be normal, the Wilcoxon Signed Rank Test was also performed to examine whether there was a significant difference between the mean values of the expected values and the radiographic measures, as well as between the mean values of the expected and controlled values. If a statistically significant difference was detected, a Wilcoxon Signed Rank Test was carried out to test if the differences were significantly different from the 1 degree. The level of statistical significance was set to 0.05.
A total of 30 patients were included in the study. For patients’ femur calculations, the difference between the controlled and the expected varus/valgus values ranged from -1 to 1 degree, whilst there was no discrepancy in terms of radio
| The 25th percentile | Median | The 75th percentile | Mean | SD | |
| Femur | |||||
| Varus | |||||
| Expected values | 0 | 0 | 0 | 0.2 | 0.4 |
| Controlled values | 0 | 0 | 1 | 0.4 | 0.6 |
| Radiographic measures | 0 | 0 | 0 | 0.2 | 0.4 |
| Flexion | |||||
| Expected values | 6 | 6 | 7 | 6.2 | 0.9 |
| Controlled values | 5 | 6 | 7 | 6.1 | 1 |
| Radiographic measures | 5 | 6 | 6 | 5.8 | 0.7 |
| Tibia | |||||
| Varus | |||||
| Expected values | 0 | 0 | 0 | 0.1 | 0.3 |
| Controlled values | 0 | 0 | 1 | 0.3 | 0.5 |
| Radiographic measures | 0 | 0 | 0 | 0 | 0 |
| Posterior slope | |||||
| Expected values | 5 | 5 | 6 | 5.4 | 1 |
| Controlled values | 5 | 5.5 | 6 | 5.7 | 0.9 |
| Radiographic measures | 5 | 5 | 6 | 5.4 | 0.8 |
| Minimum | 25th percentile | Median | 75th percentile | Maximum | |
| Femur | |||||
| Varus (degrees) | |||||
| Controlled values | -1.00 | -1.00 | 0.00 | 0.00 | 1.00 |
| Radiographic measures | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Flexion (degrees) | |||||
| Controlled values | -1.00 | 0.00 | 0.00 | 0.00 | 1.00 |
| Radiographic measures | -1.00 | 0.00 | 0.00 | 1.00 | 1.00 |
| Tibia | |||||
| Varus (degrees) | |||||
| Controlled values | -1.00 | -1.00 | 0.00 | 0.00 | 1.00 |
| Radiographic measures | 0.00 | 0.00 | 0.00 | 0.00 | 1.00 |
| Posterior slope (degrees) | |||||
| Controlled values | -2.00 | 0.00 | 0.00 | 0.00 | 1.00 |
| Radiographic measures | -1.00 | 0.00 | 0.00 | 0.00 | 1.00 |
Concerning tibia calculations, the discrepancy between controlled and expected values for varus ranged from -1 to 1 degree with a medium value of zero degrees, while the difference between radiographic measurements and expected values for varus ranged from 0 to 1 degree with a medium value of zero degrees. Finally, the difference between controlled and expected values for the posterior slope ranged from -2 to 1 degree and between radiographic measure
| Mean (SD) | CCC (95%CI) | 95% LOA | Number of differences out of the LOA | |
| Femur | ||||
| Varus (degrees) | ||||
| Controlled values | -0.20 (0.61) | 0.25 (-0.06, 0.56) | (-1.40, 1.00) | 3 |
| Radiographic measures | 0.00 (0.00) | 1.00 (1.00, 1.00) | - | - |
| Flexion (degrees) | ||||
| Controlled values | 0.03 (0.56) | 0.83 (0.71, 0.94) | (-1.06, 1.10) | 0 |
| Radiographic measures | 0.33 (0.61) | 0.66 (0.48, 0.84) | (-0.86, 1.52) | 2 |
| Tibia | ||||
| Varus (degrees) | ||||
| Controlled values | -0.23 (0.50) | 0.31 (0.06, 0.56) | (-1.22, 0.76) | 1 |
| Radiographic measures | 0.10 (0.31) | - | (-0.50, 0.70) | 3 |
| Posterior slope (degrees) | ||||
| Controlled values | -0.22 (0.63) | 0.75 (0.59, 0.91) | (-1.46, 0.99) | 3 |
| Radiographic measures | 0.03 (0.41) | 0.89 (0.82, 0.95) | (-0.78, 0.84) | 5 |
Near-perfect CCCs were reckoned for comparisons only between estimated flexion values and controlled and radiographic measurements in the femur and between estimated posterior slope values and controlled and radiographic measurements in the tibia, varying from 0.66 to 0.89. Also, as mentioned before, no deviation was observed between expected varus values and radiographic measurements in the femur. The 95% limits of agreement were within -1.46 to 1.52 degrees, and most estimates lie within the indicating (Table 3). Low CCC was estimated for expected and controlled values of varus in the femur and tibia.
A Wilcoxon Signed Rank Test was performed to determine whether there was a statistically significant difference re
Our study aimed to denote the reproducible accuracy of an AR system (Knee+™, Pixee Medical) in 30 TKA patients compared to their intraoperative measurements. At this time, to the best of our knowledge, this is one of the largest clinical studies of this size to examine the accuracy and efficacy of this system, but the first to include implants with different characteristics. The results indicate that good varus/valgus alignment was accomplished without outliers, whilst sagittal alignment was generally featured satisfactory. The procedure was performed comfortably and repeatedly by the same team. With regard to the rigorous limits and standards employed for the goals of our study, it is vitally important to emphasize that a difference of 1˚ in final implants’ position is unlikely to be clinically significant, as numerous studies have demonstrated that differences in coronal alignment after TKA of up to 3˚ (or even up to roughly 6˚) result in good clinical outcomes[14]. This exact point is crucial when considering the position of AR systems in the overall context of TKA.
There is an expanding interest in surgical variables intraoperatively controlled by orthopaedic surgeons, involving lower leg alignment, component positioning and soft-tissue balancing. Punctilious control over these factors is associated with improved outcomes, which is the main reason why several computer navigation and robotic-assisted systems have emerged[11-13].
In our study, three different types of implants were used with similar characteristics as surface arthroplasties. Their main difference lies in femoral flexion and posterior tibial slope. According to the aforementioned results, the Knee+™ AR system is a repeatable open platform method, eligible to use with the same accuracy regardless of the characteristics of the implants employed.
AR solutions can potentially decrease the outcome dependence on the surgeon’s parameters by providing preoperative planning in the surgeon’s field of view or even indicating impeccable trajectories for placing implants with overlays[11,12]. Diminishing cutting errors is the challenge of every AR system assisting TKA. According to literature data and the system’s design, the system’s accuracy lies principally in the varus/valgus tibial cut regarding the restoration of the mechanical axis.
More specifically, a recent study by Bennett et al[13] suggested that coronal mean error for femoral and tibial cuts is 1.3˚ and 1.1˚, respectively. That present-day paper examined total knee arthroplasties carried out with the assistance of Knee+™ AR system, as in our study. Comparing the two contemporary studies, results are featured comparatively similar, indicating that the robustness of this AR system regarding restoration of mechanical axis after primary TKA is perceptibly rigorous[13]. In a 2021 systematic review scrutinizing the accuracy of Knee+™ AR system by Iacono et al[15], it was deduced that this system is capable of executing cutting errors of less than 1˚ of discrepancy regarding coronal alignment and less than 2˚ in terms of posterior tibial slope and femoral extension/flexion, however, the copious limitations of this study need to be taken into consideration[15]. Perusing literature, it is patently evident that there are limited data concerning the effectiveness and accuracy of other AR systems used in TKA. Tsukada et al[16] examined the efficacy of another AR system regarding the exactness of bone resection in TKA, concluding that AR technology can bolster surgeons’ distal femoral resection accuracy compared to traditional intramedullary-guided techniques[16]. Additionally, another study by Fucentese and Koch[17] examined the impact of “NextAR” AR TKA system (Medacta International SA, Castel San Pietro, Switzerland) in prosthesis alignment and positioning. It was inferred that, despite being employed in a low number of cases, the initial results seemed promising, requiring further research to corroborate the potency of this system[17].
The Knee+™ AR system equips the surgeon with a thorough preoperative plan projected in real-time concerning the alignment of bone components and mechanical axis restoration[18]. Notwithstanding, after initial cuts are executed, and the system describes a significant difference, it enables the surgeon to alter their surgical plans and correct the previously made osteotomies by contrasting the expected and controlled values. The design of this AR system does not require the utilization of intramedullary rods for femoral and tibial osteotomies, which are correlated with low-incidence intraoperative thromboembolic episodes[18].
All measurements are calculated intraoperatively, thus, there is no demand for time and cost-consuming preoperative radiographic scans that expose the patients to radiation[19,20]. During surgery, not using extra pins as markers for restoration of the mechanical axis is linked with reduced risk of periprosthetic fractures during implantation, chiefly of the femoral component, and eliminated infection risk. Marker stabilization on the cutting guides is considered safe because it decreases the risk of systemic malalignment calculations due to intraoperative pin stretching, triggering imprecise cuts[21].
Although it has been demonstrated that AR might positively impact surgeons by diminishing surgical errors, verifying the learning curve would be an engrossing aim. Nonetheless, it is a user-friendly system with an effortless intraoperative setup that guides the surgeon throughout the surgery and is versatile in amending operative plans if necessary[22,23]. In our study, operative time and blood loss were not investigated, thus further research is incontrovertibly required to evaluate the potential impact of Knee+™ and other AR systems on this area.
Concerns have been raised regarding the extent of potentially spurious and disturbing AR information displayed intraoperatively. This AR system does not require substantial space or instrumentation in the operating room. Compared with other navigation systems, this digital tool allows the surgeon to concentrate on the surgical field through smart glasses and not get distracted by other display screens, allowing precious coordination between the surgical team. Apposite contrast and clarity of the AR technology and avoidance of masking structures in real patient view are of paramount significance[23].
Present-day literature data propound that AR systems, such as Knee+™, are becoming comparable to conventional navigation techniques in terms of precision and safety for routine clinical practice. AR appears to be a robust contemporary digital tool capable of revolutionizing the field of orthopaedic surgery, providing substantive information regarding intraoperative guidance and decision-making. In the future, it will distinctly possibly serve as a transcendent human-computer interface, enabling dexterous surgeons to attain superior results. Nonetheless, further technological and medical research is requisite to achieve AR technologies' maximum potential and cost-effectiveness. Until then, it is vitally important for the orthopaedic surgeon to rely on their training and adroitness for decision-making and opting wisely to employ an AR system.
Computer-assisted systems obtained an increased interest in orthopaedic surgery over the last years, as they enhance precision compared to conventional hardware. The expansion of computer assistance is evolving with the employment of augmented reality (AR). With the implementation of navigation systems, orthopaedic surgeons can precisely track and visualize surgical instruments in real-time, conforming to the anatomical structures. Yet, the accuracy of AR navigation systems has not been determined. This case series endeavors to scrutinize the accurateness of component alignment and restoration of the affected limb’s mechanical axis in primary total knee arthroplasty (TKA), employing the Knee+™ system. Additionally, this study aims to evaluate whether such systems are substantively beneficial for a high-experienced knee surgeon.
This study aims to examine the accuracy of component alignment and restoration of the affected limb’s mechanical axis in primary TKA, utilizing an AR navigation system and to assess whether such systems are conspicuously fruitful for an accomplished knee surgeon. Our study denotes the reproducible accuracy of an AR system (Knee+™, Pixee Medical) in 30 TKA patients compared to their intraoperative measurements, which is one of the largest clinical studies of this size to examine the accuracy and efficacy of this system. AR solutions can potentially decrease the outcome dependence on the surgeon’s parameters by providing preoperative planning in the surgeon’s field of view or even indicating impeccable trajectories for placing implants with overlays. In particular, the Knee+™ AR system equips the surgeon with a thorough preoperative plan projected in real-time concerning the alignment of bone components and mechanical axis restoration.
The results indicate satisfactory postoperative coronal alignment without outliers across all three implants. The procedure was performed comfortably and repeatedly by the same team. AR navigation systems can bolster orthopaedic surgeons’ accuracy in achieving precise axial alignment. With regard to the rigorous limits and standards employed for the goals of our study, it is vitally important to emphasize that a difference of 1˚ in final implants’ position is unlikely to be clinically significant, as numerous studies have demonstrated that differences in coronal alignment after TKA of up to 3˚ (or even up to roughly 6˚) result in good clinical outcomes
From May 2021 to December 2021, 30 patients, 25 women and 5 men, underwent a primary unilateral TKA. Revision cases were excluded. A preoperative radiographic procedure was performed to evaluate the limb’s axial alignment. All patients were operated on by the same team, without a tourniquet, utilizing three distinct prostheses with the assistance of the Knee+™ AR navigation system in every operation. Postoperatively, the same radiographic exam protocol was executed to evaluate the implants’ position, orientation and coronal plane alignment. We recorded measurements in 3 stages regarding femoral varus and flexion, tibial varus and posterior slope. Firstly, the expected values from the AR system were documented. Then we calculated the same values after each cut and finally, the same measurements were recorded radiologically after the operations. Concerning statistical analysis, Lin’s concordance correlation coefficient was estimated, while Wilcoxon Signed Rank Test was performed when needed.
A Wilcoxon Signed Rank Test was performed to determine whether there was a statistically significant difference re
Our study aimed to denote the reproducible accuracy of an AR system (Knee+™, Pixee Medical) in 30 TKA patients compared to their intraoperative measurements. At this time, to the best of our knowledge, this is one of the largest clinical studies of this size to examine the accuracy and efficacy of this system, but the first to include implants with different characteristics. The results indicate that good varus/valgus alignment was accomplished without outliers, whilst sagittal alignment was generally featured satisfactory, while the procedure was performed comfortably and repeatedly by the same team. AR solutions can potentially decrease the outcome dependence on the surgeon’s parameters by providing preoperative planning in the surgeon’s field of view or even indicating impeccable trajectories for placing implants with overlays. Diminishing cutting errors is the challenge of every AR system assisting TKA. The Knee+™ AR system equips the surgeon with a thorough preoperative plan projected in real-time concerning the alignment of bone components and mechanical axis restoration. It is a user-friendly system with an effortless intraoperative setup that guides the surgeon throughout the surgery and is versatile in amending operative plans if necessary. Further research is required to evaluate their efficacy and potential.
In the future, it will distinctly possibly serve as a transcendent human-computer interface, enabling dexterous surgeons to attain superior results. Nonetheless, further technological and medical research is requisite to achieve AR technologies' maximum potential and cost-effectiveness. Until then, it is vitally important for the orthopaedic surgeon to rely on their training and adroitness for decision-making and opting wisely to employ an AR system.
| 1. | HCPUnet, Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality. Dec 20, 2012. [cited 23 February 2024]. Available from: http://hcupnet.ahrq.gov. |
| 2. | Lavernia CJ, Guzman JF, Gachupin-Garcia A. Cost effectiveness and quality of life in knee arthroplasty. Clin Orthop Relat Res. 1997;134-139. [PubMed] |
| 3. | Ewurum CH, Guo Y, Pagnha S, Feng Z, Luo X. Surgical Navigation in Orthopedics: Workflow and System Review. Adv Exp Med Biol. 2018;1093:47-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Mandal P, Ambade R. Surgery Training and Simulation Using Virtual and Augmented Reality for Knee Arthroplasty. Cureus. 2022;14:e28823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 5. | Hernandez D, Garimella R, Eltorai AEM, Daniels AH. Computer-assisted Orthopaedic Surgery. Orthop Surg. 2017;9:152-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Wang G, Li L, Xing S, Ding H. Intelligent HMI in Orthopedic Navigation. Adv Exp Med Biol. 2018;1093:207-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Azuma RT. A survey of augmented reality. Presence (Camb). 1997;6:355-385. [DOI] [Full Text] |
| 8. | Vávra P, Roman J, Zonča P, Ihnát P, Němec M, Kumar J, Habib N, El-Gendi A. Recent Development of Augmented Reality in Surgery: A Review. J Healthc Eng. 2017;2017:4574172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 267] [Cited by in RCA: 181] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 9. | Gavaghan KA, Peterhans M, Oliveira-Santos T, Weber S. A portable image overlay projection device for computer-aided open liver surgery. IEEE Trans Biomed Eng. 2011;58:1855-1864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (1)] |
| 10. | Gavaghan K, Oliveira-Santos T, Peterhans M, Reyes M, Kim H, Anderegg S, Weber S. Evaluation of a portable image overlay projector for the visualisation of surgical navigation data: phantom studies. Int J Comput Assist Radiol Surg. 2012;7:547-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Kocev B, Ritter F, Linsen L. Projector-based surgeon-computer interaction on deformable surfaces. Int J Comput Assist Radiol Surg. 2014;9:301-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Nikou C, Digioiai A, Blackwell M, Jaramaz B, Kanade T, Digioia A. Augmented reality imaging technology for orthopaedic surgery. Oper Tech Orthop. 2000;10:82-86. [RCA] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Bennett KM, Griffith A, Sasanelli F, Park I, Talbot S. Augmented Reality Navigation Can Achieve Accurate Coronal Component Alignment During Total Knee Arthroplasty. Cureus. 2023;15:e34607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 14. | Bilgin E, Bombacı H, Turgut A, Kalenderer Ö, Kılınç BE, Adıyeke L, Görgeç M. How are clinical outcomes related to the deviation severity of the tibiofemoral mechanical axis on coronal plane following knee arthroplasty? J Clin Orthop Trauma. 2019;10:91-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Iacono V, Farinelli L, Natali S, Piovan G, Screpis D, Gigante A, Zorzi C. The use of augmented reality for limb and component alignment in total knee arthroplasty: systematic review of the literature and clinical pilot study. J Exp Orthop. 2021;8:52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Tsukada S, Ogawa H, Nishino M, Kurosaka K, Hirasawa N. Augmented Reality-Assisted Femoral Bone Resection in Total Knee Arthroplasty. JB JS Open Access. 2021;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | Fucentese SF, Koch PP. A novel augmented reality-based surgical guidance system for total knee arthroplasty. Arch Orthop Trauma Surg. 2021;141:2227-2233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 18. | Pokhrel S, Alsadoon A, Prasad PWC, Paul M. A novel augmented reality (AR) scheme for knee replacement surgery by considering cutting error accuracy. Int J Med Robot. 2019;15:e1958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 19. | Maharjan N, Alsadoon A, Prasad PWC, Abdullah S, Rashid TA. A novel visualization system of using augmented reality in knee replacement surgery: Enhanced bidirectional maximum correntropy algorithm. Int J Med Robot. 2021;17:e2223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Andrews CM, Henry AB, Soriano IM, Southworth MK, Silva JR. Registration Techniques for Clinical Applications of Three-Dimensional Augmented Reality Devices. IEEE J Transl Eng Health Med. 2021;9:4900214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 21. | Ma L, Fan Z, Ning G, Zhang X, Liao H. 3D Visualization and Augmented Reality for Orthopedics. Adv Exp Med Biol. 2018;1093:193-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Jud L, Fotouhi J, Andronic O, Aichmair A, Osgood G, Navab N, Farshad M. Applicability of augmented reality in orthopedic surgery - A systematic review. BMC Musculoskelet Disord. 2020;21:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 101] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 23. | Chytas D, Malahias MA, Nikolaou VS. Augmented Reality in Orthopedics: Current State and Future Directions. Front Surg. 2019;6:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Xiao JL, China; Yang FC, China S-Editor: Li L L-Editor: A P-Editor: Zhao YQ