©The Author(s) 2025.
World J Orthop. Oct 18, 2025; 16(10): 108992
Published online Oct 18, 2025. doi: 10.5312/wjo.v16.i10.108992
Published online Oct 18, 2025. doi: 10.5312/wjo.v16.i10.108992
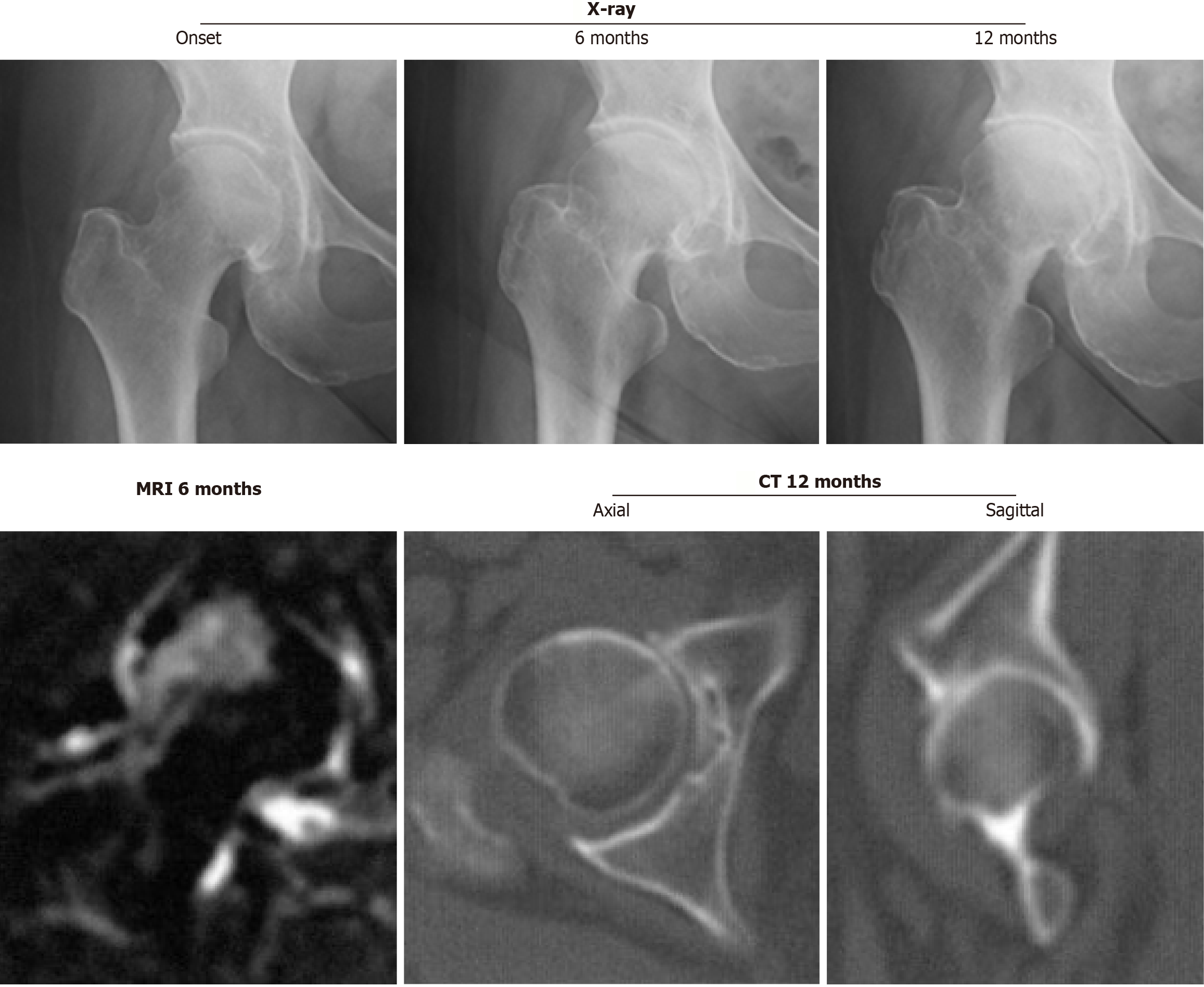
Figure 1 Right hip joint with rapidly progressive osteoarthritis of the hip showing chondrolysis greater than 2 mm/year on a series of radiographs without femoral head destruction on computed tomography at 12 months after the onset.
Magnetic resonance imaging at 6 months after the onset demonstrates inhomogeneous high intensity on the short τ inversion recovery sequence image, including the superolateral portion of the femoral head. CT: Computed tomography; MRI: Magnetic resonance imaging.
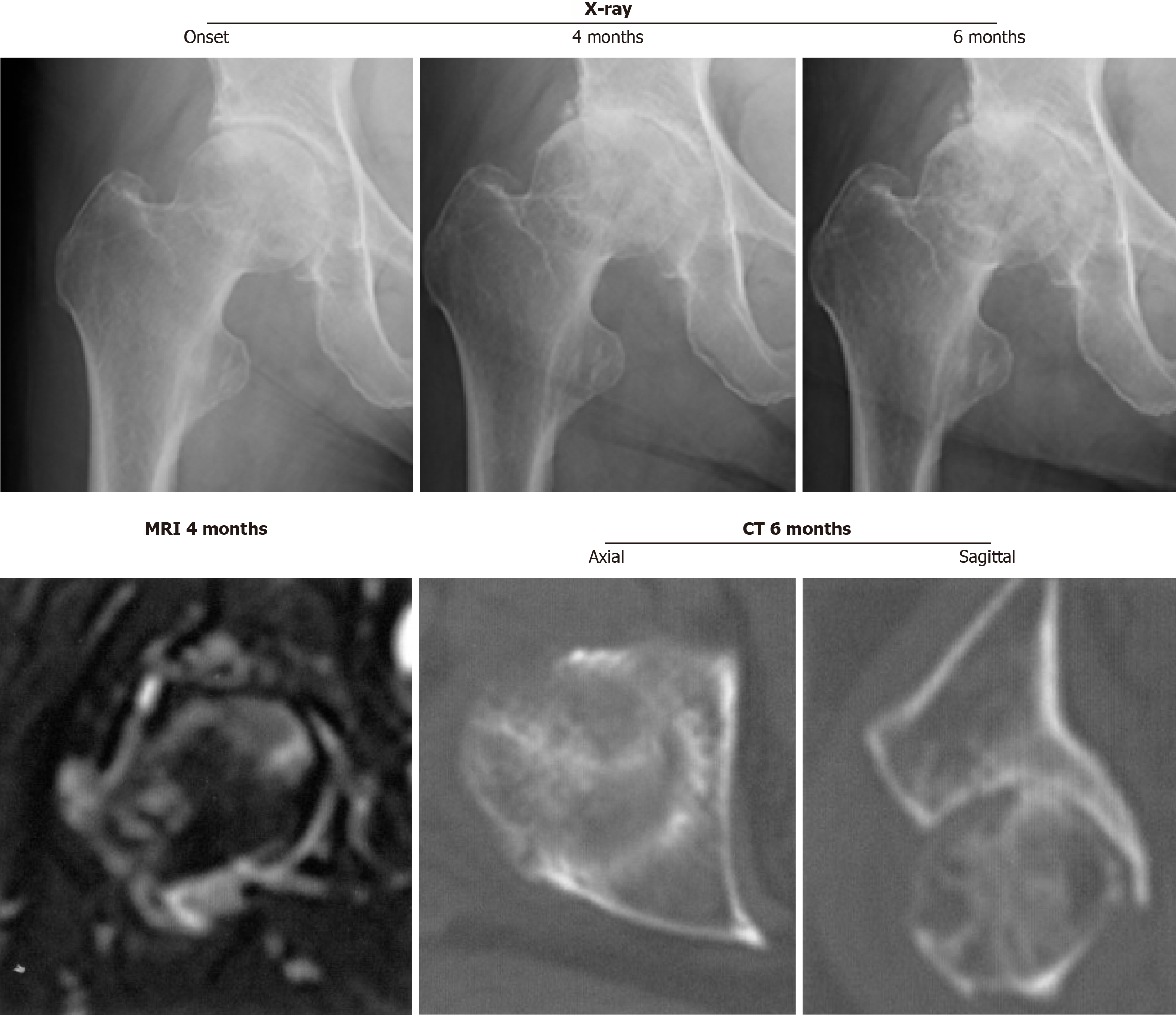
Figure 2 Right hip joint with rapidly progressive osteoarthritis of the hip demonstrating partial destruction of the anterior portion of the femoral head on computed tomography at 6 months after the onset subsequent to rapid chondrolysis.
Magnetic resonance imaging at 4 months after the onset shows high intensity on the short τ inversion recovery sequence image in the proximal femur, including the femoral neck and head. CT: Computed tomography; MRI: Magnetic resonance imaging.
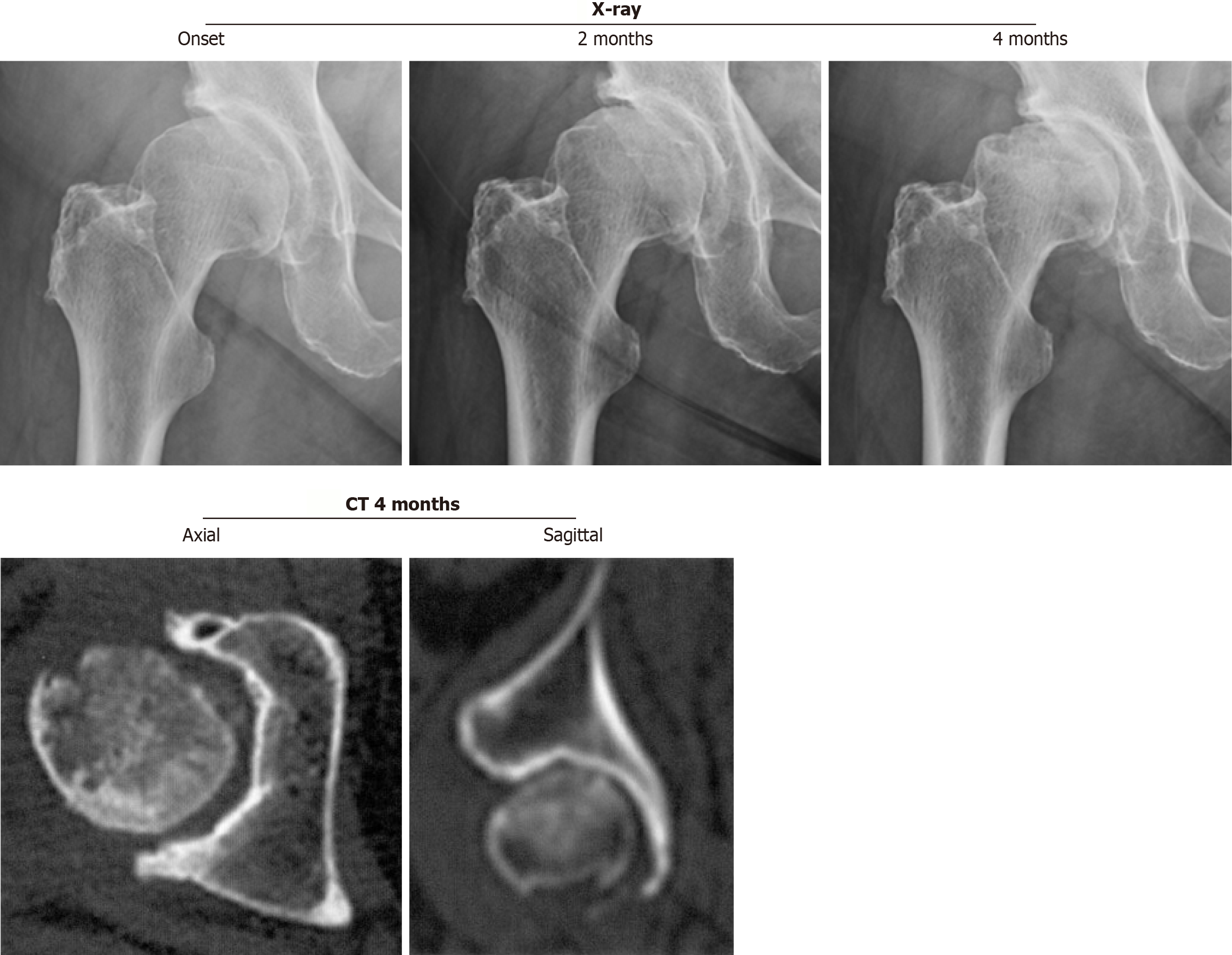
Figure 3
Right hip joint with subchondral insufficiency fracture of the femoral head showing fracture on the subchondral area in the superolateral portion of the femoral head without joint space narrowing.
CT: Computed tomography.
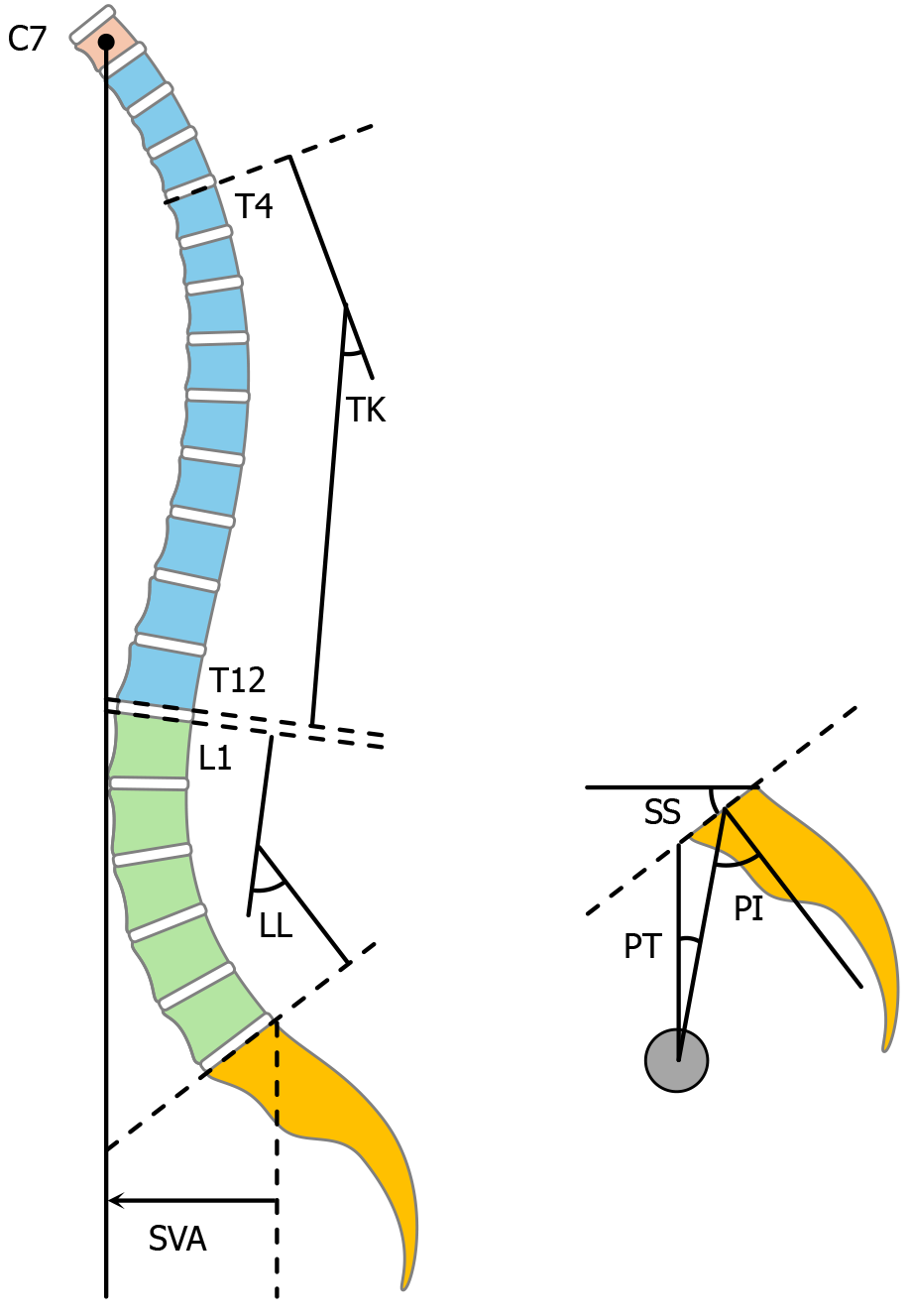
Figure 4 Illustration of the radiological parameters of the sagittal spinopelvic alignment.
Pelvic tilt is the angle between the vertical and the line from the center of the femoral heads to the midpoint of the sacral endplate. Sacral slope is the angle between the horizontal and the first sacral endplate. Pelvic incidence is calculated using the following equation: Pelvic incidence = pelvic tilt + sacral slope. Sagittal vertical axis is defined as the sagittal offset of the seventh cervical vertebra plumb line from the posterosuperior corner of the first sacral endplate. Thoracic kyphosis angle is the angle between the upper endplate of the fourth thoracic vertebra and the lower endplate of the twelfth thoracic vertebra. Lumbar lordosis angle is the angle between the upper endplate of the first lumbar vertebra and the first sacral endplate. PT: Pelvic tilt; SS: Sacral slope; PI: Pelvic incidence; SVA: Sagittal vertical axis; C7: Seventh cervical vertebra; TK: Thoracic kyphosis angle; T4: Fourth thoracic vertebra; T12: Twelfth thoracic vertebra; LL: Lordosis angle.
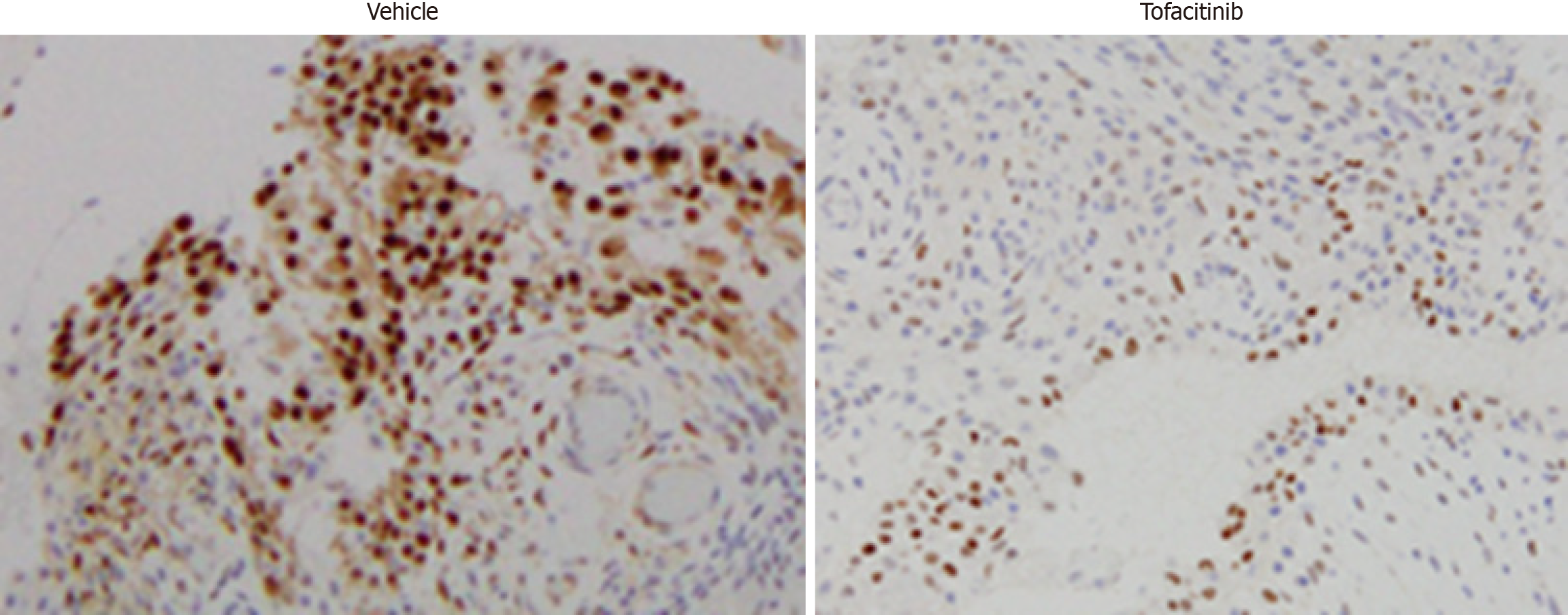
Figure 5 Immunohistochemistry of the synovial tissues from the hip joint with rapidly progressive osteoarthritis of the hip at 6 months from the disease onset.
Tissue sections of the synovial tissues were subjected to immunohistochemical staining using anti-phospho-signal transducer and activator of transcription 3 with or without treatment with tofacitinib. Original magnification × 200.
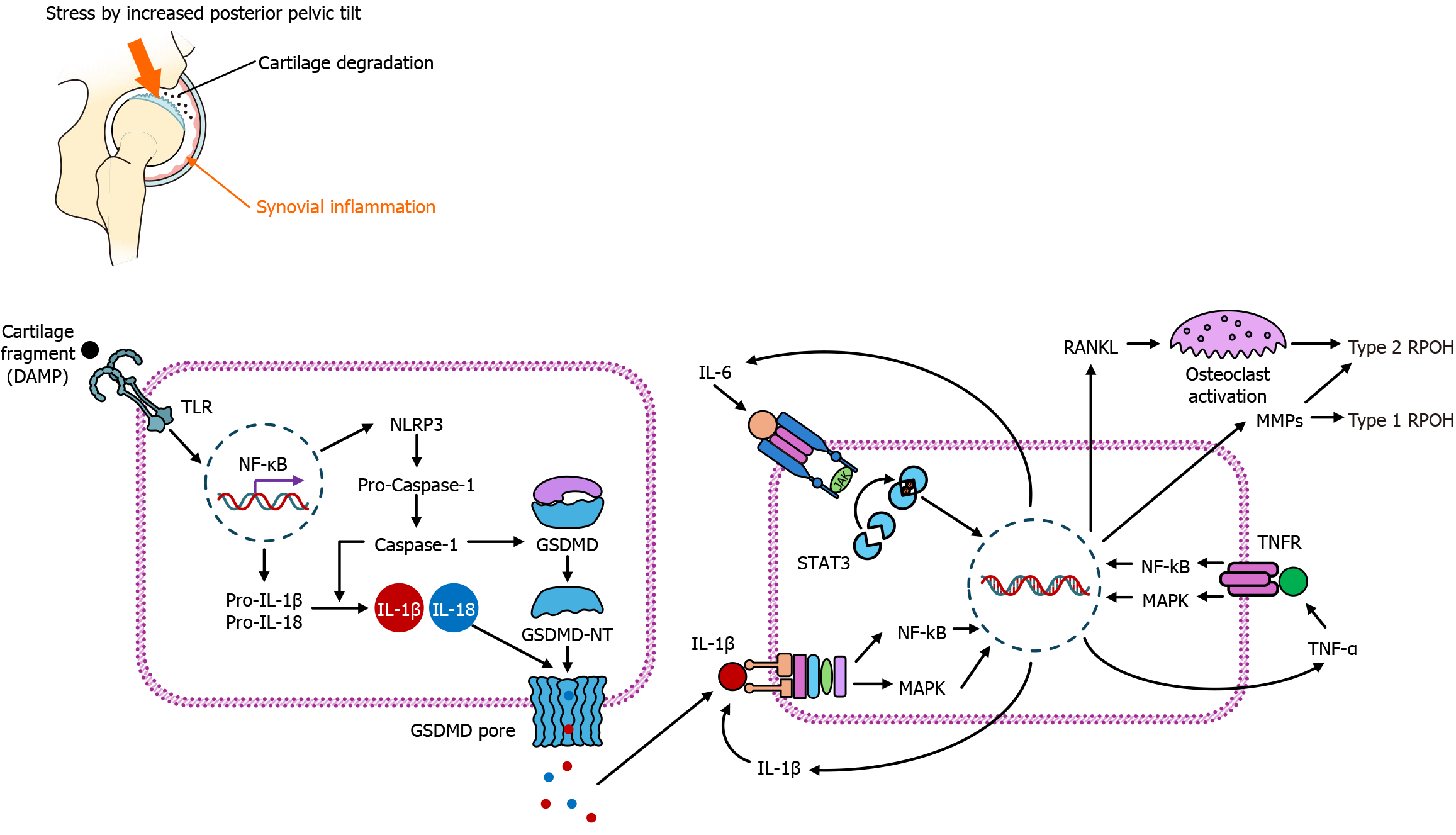
Figure 6 Putative pathophysiology at the initial stage of rapidly progressive osteoarthritis of the hip.
DAMP: Danger-associated molecular pattern; TLR: Toll-like receptor; NF-κB: Nuclear factor κB; NLRP3: Nucleotide-binding and oligomerization domain-like receptor family pyrin domain containing 3; GSDMD: Gasdermin D; GSDMD-NT: N-terminal pore-forming gasdermin D fragment; IL: Interleukin; TNF-α: Tumor necrosis factor α; JAK: Janus kinase; STAT3: Signal transducer and activator of transcription 3; MAPK: Mitogen-activated protein kinase; MMPs: Matrix metalloproteinases; RANKL: Receptor activator of nuclear factor-κB ligand; RPOH: Rapidly progressive osteoarthritis of the hip.
- Citation: Yasuda T. Early diagnosis and targeted intervention based on the pathogenesis of rapidly progressive osteoarthritis of the hip. World J Orthop 2025; 16(10): 108992
- URL: https://www.wjgnet.com/2218-5836/full/v16/i10/108992.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i10.108992