Published online May 24, 2025. doi: 10.5306/wjco.v16.i5.105444
Revised: February 27, 2025
Accepted: March 24, 2025
Published online: May 24, 2025
Processing time: 118 Days and 0.3 Hours
Multiple primary carcinoma (MPC) refers to two or more types of primary malig
In this study, we report a case of a 40-year-old female who was diagnosed with invasive ductal carcinoma of the breast (T3N1M0 stage IIIA LuminalB type) as the first primary cancer and DLBCL (stage IIIA) as the second primary cancer. The patient underwent the modified radical mastectomy for left breast cancer and received Rituximab, cyclophospha-mide, hydroxydaunorubicin, Oncovin (vincri
Accurate diagnosis and management of metachronous MPC requires an interdisciplinary team and selection of an appropriate treatment plan.
Core Tip: We report a case of a 40-year-old female diagnosed with invasive ductal carcinoma of the breast (T3N1M0 stage IIIA LuminalB type) as the first primary cancer and diffuse large B-cell lymphoma (DLBCL) (stage IIIA) as the second primary cancer. A modified radical mastectomy was selected for the treatment of left breast cancer and Rituximab, cyclophospha-mide, hydroxydaunorubicin, Oncovin (vincristine) and prednisolone regimen chemotherapy treatment to control DLBCL. At the last follow-up, the patient is in stable condition. In clinical practice, the simultaneous existence of metachronous primary breast cancer and lymphoma is rare. This case underscores the need for a multidisciplinary management approach and the adoption of advanced imaging techniques to facilitate early identification and treatment of rare multiple primary carcinoma cases.
- Citation: Luo M, Liu RN, He ZM, Liang QF, Huang FL. Diagnosis and treatment of metachronous multiple primary carcinoma: A case report and review of literature. World J Clin Oncol 2025; 16(5): 105444
- URL: https://www.wjgnet.com/2218-4333/full/v16/i5/105444.htm
- DOI: https://dx.doi.org/10.5306/wjco.v16.i5.105444
Breast cancer is one of the most common malignant tumors in women, which can be fatal, deteriorating the physical and mental health of women worldwide. In 2020, an estimated 2.3 million new cases of breast cancer were reported globally, accounting for 11.7% of all malignant tumors, making it the most prevalent malignant tumor among women, surpassing lung cancer[1]. Invasive carcinoma is the most common pathological type of breast cancer[2]. Non-Hodgkin’s lymphoma (NHL) is a malignant tumor of the lymphatic system, accounting for about 90% of lymphoma cases. Diffuse large B-cell lymphoma (DLBCL) is the most common NHL, affecting gastrointestinal tract, the neck and other lymphoid tissues or organs rich in lymphoid tissue. Environmental pollution caused by pollutants, such as food additives and pesticides, has contributed to the progressively rising incidence of lymphoma[3]. Simultaneous or metachronous primary breast cancer and lymphoma are rare in clinical practice. In this case report, we describe the diagnosis and treatment process of a pa
A 40-year-old female presented with a mass in the left breast during a physical examination in November 2017. There was no skin redness, fever, headache, vomiting, or tenderness. In the outpatient clinic, the patient received a breast ultrasound examination, which identified a solid mass in the left breast and bilateral axillary hypoechoic masses. Conse
Physical examination revealed a mass in the left breast, without skin redness, fever, headache, or vomiting.
The patient denied any history of hypertension, coronary heart disease, diabetes, hepatitis, tuberculosis, or other infec
Her occupation and working conditions were free from industrial toxins, dust, radioactive substances and exposure his
Physical examination did not find any systemic abnormalities except for a left breast lump with a Karnofsky performance status score of 1.
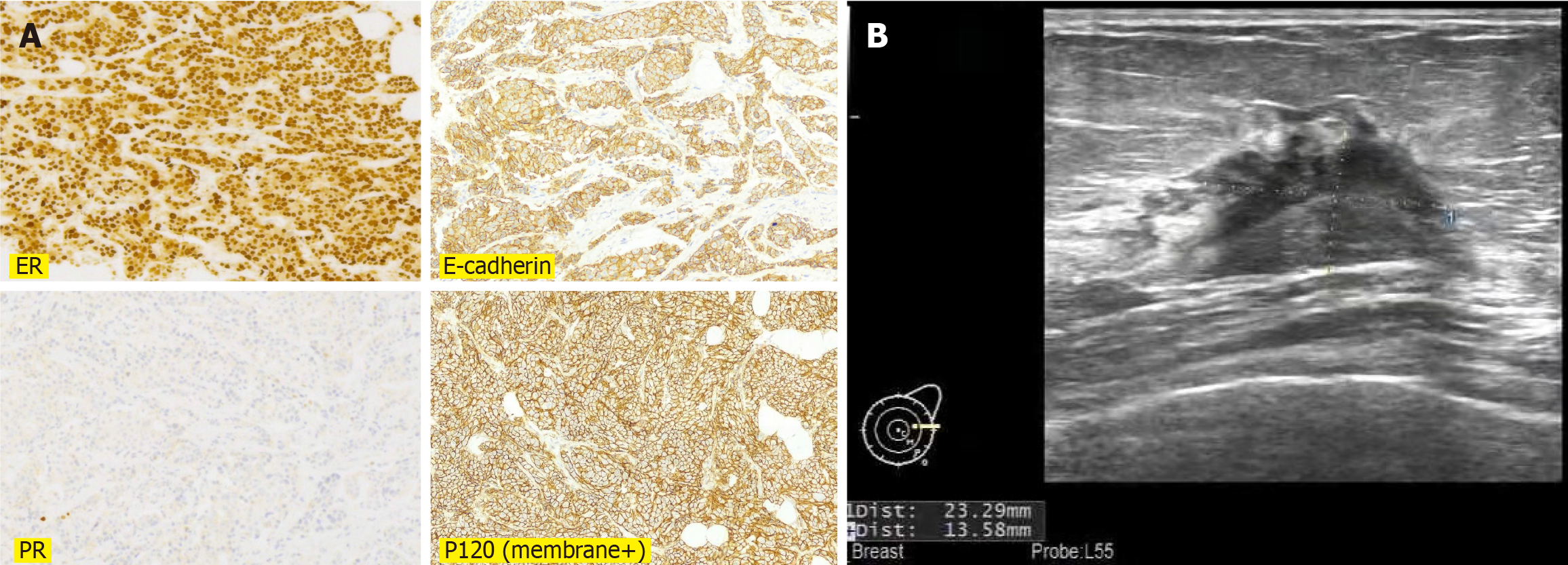
Immunological examination: In November 2017, rotational resection of a breast mass was performed. Immunohistochemistry revealed CK5/6 (-), P63 (-), CD10 (-), E-cadherin (+), P120 (membrane+), ER (90%), PR (5%), HER-2 (0), P53 (+), P16 (-), epidermal growth factor receptor (-), and Ki-67 (60%) (Figure 1A). These tests suggested a diagnosis of invasive ductal carcinoma of the breast. Routine blood test, urinalysis, routine stool and liver and kidney function did not find any significant abnormalities.
Breast ultrasound revealed a solid mass in the left breast (BI-RADS 4b grade) with a diameter of 2.4 cm and lymph node ultrasound identified oval hypoechoic mass in the bilateral (Figure 1B). Abdominal ultrasound and chest computed tomo
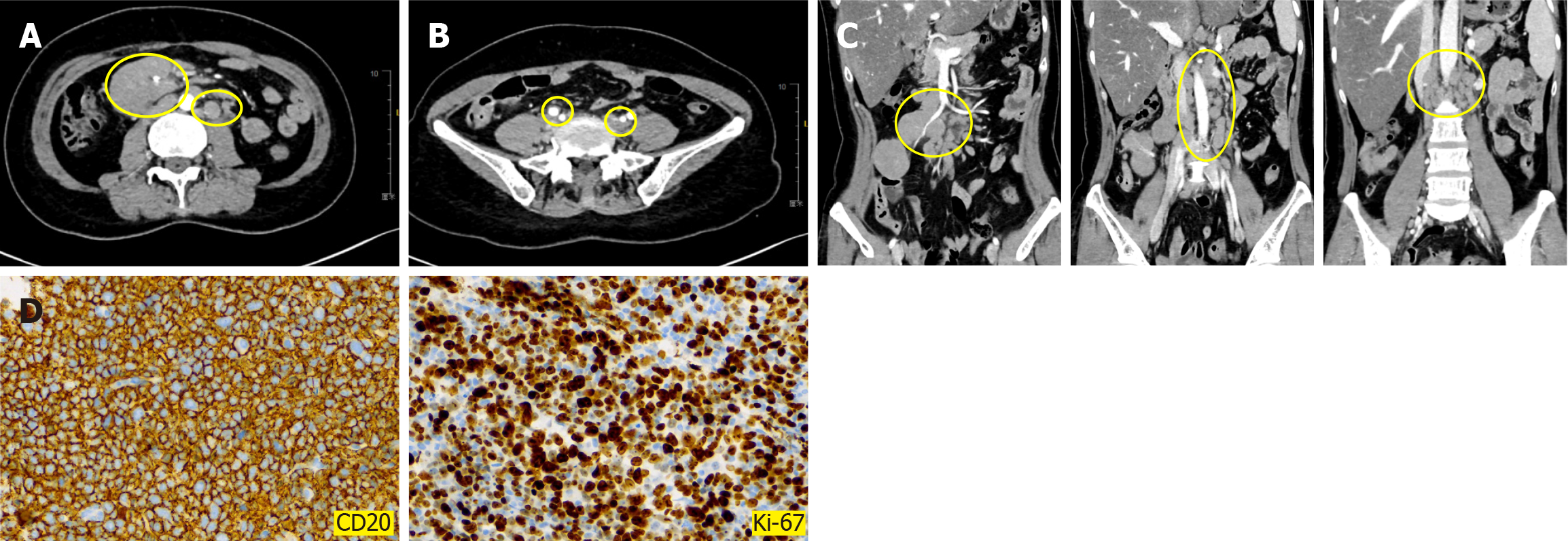
In August 2023, re-examination CT identified multiple enlarged lymph nodes in the abdominal cavity (Figure 2A-C). Subsequently, the pathological biopsy of the right abdominal mass was performed and immunohistochemical examina
A final diagnosis of metachronous MPC was made, with invasive ductal carcinoma of the breast (T3N1M0 stage IIIA LuminalB type) as the first primary cancer and DLBCL (stage IIIA) as the second primary cancer.
In December 2017, a modified radical mastectomy was performed to treat left breast cancer together with four cycles of EC regimen chemotherapy (epirubicin + cyclophosphamide) from December 2017 to March 2018. In April 2018, she was administered with four cycles of chemotherapy using the docetaxel regimen.
In June 2018, a follow-up CT indicated the presence of proliferative lesions in the lung posterior right upper lobe, which were treated with radiotherapy with a scheduled target volume of 50 Gy/25 fractions in August and tamoxifen endocrine therapy applied afterwards. In November 2019, the patient underwent re-examinations, which confirmed no signs of tumor recurrence or metastasis. Breast ultrasound showed solid nodules in the right breast (BI-RADS class 3, suggestive of proliferative nodules) and tamoxifen was administered as endocrine therapy. In May 2021, magnetic resonance imaging of the abdominal and pelvic revealed no clear signs of tumor recurrence or metastasis. The patient continues to receive tamoxifen treatment combined with leuprorelin.
In August 2023, re-examination positron emission tomography (PET)-CT showed multiple enlarged lymph nodes in the abdominal cavity, which were considered manifestations of DLBCL based on immunological results as determined by a multidisciplinary team. According to the basic treatment principles of multiple primary tumors of the Chinese Society of Clinical Oncology Guidelines in 2024[4] and the National Comprehensive Cancer Network Clinical Guidelines in 2024[5], the patient was put on the standard first-line treatment Rituximab, cyclophospha-mide, hydroxydaunorubicin, Oncovin (vincristine) and prednisolone (R-CHOP) regimen chemotherapy, consisting of rituximab 600 mg/day 1, cyclo
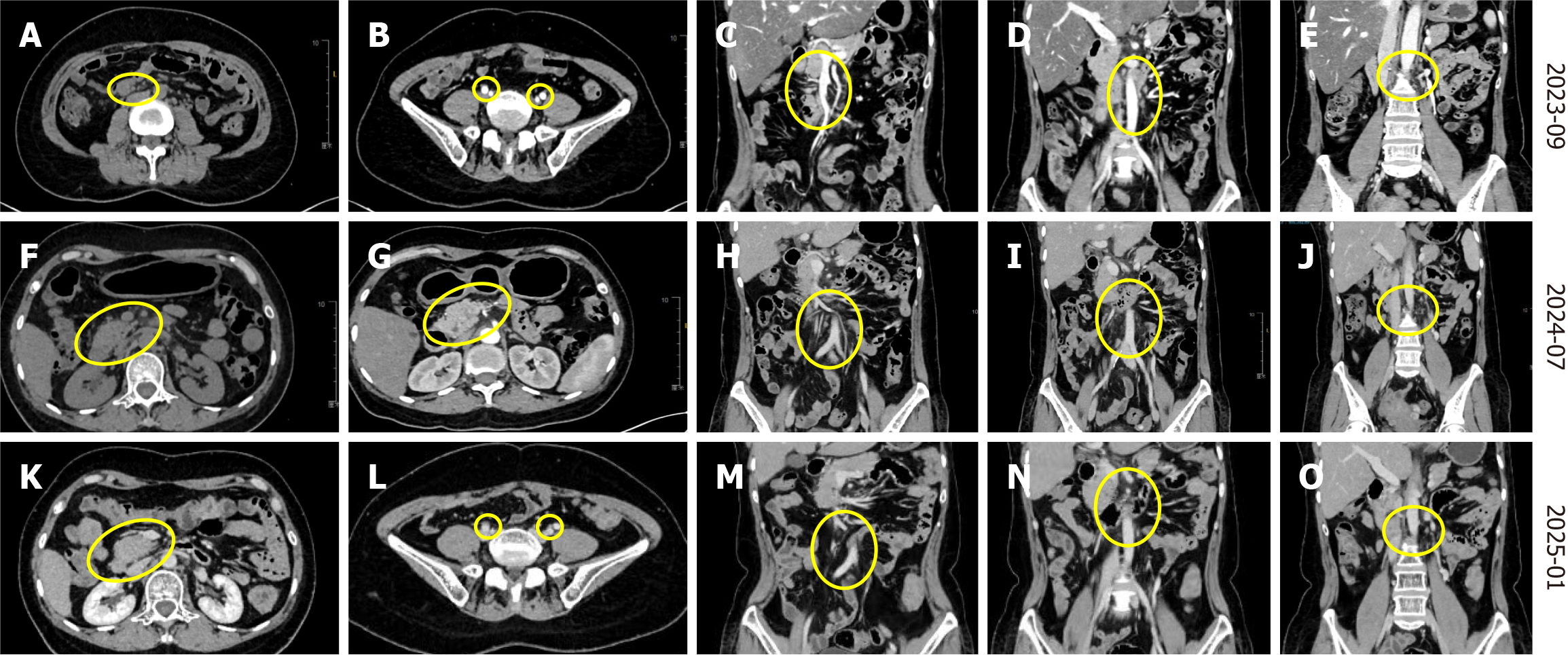
From September to December 2023, the second to sixth cycles of R-CHOP chemotherapy were administered as follows: Rituximab 600 mg/day 1, cyclophosphamide 1000 mg/day 1, pirarubicin 70 mg/day 1, vincristine 2 mg/day 1, and prednisone 100 mg/day 1-5. After the second cycle of R-CHOP chemotherapy, CT revealed a significant reduction of the lymph nodes in the abdominal aorta, bilateral iliac vessels and abdominal compared to earlier tests. The therapeutic effect of the drugs was evaluated as the partial response (PR). However, the complete response (CR) was achieved on the sixth cycle of chemotherapy. In January 2024, the treatment was changed to rituximab 500 mg/day 0, etoposide 0.15 g/day 1-3, ifosfamide 8 g/day 2, carboplatin 0.5 g/day 2. These drugs achieved significant bone marrow suppression. In February 2024, the chemotherapy dosage was adjusted to rituximab 600 mg/day 0, etoposide 0.15 g/day 1-2, 0.1 g/day 3, ifosfa
From April to June 2024, the patient underwent four cycles of chemotherapy comprising 600 mg zuberitamab and gemox regimen (gemcitabine 1.7 g/day 1, oxaliplatin 170 mg/day 1 q2w). After the last chemotherapy cycle, the patient developed grade III bone marrow suppression. In July, a follow-up CT showed a marked reduction in the abdominal tumor and the therapeutic effect evaluation was PR. The patient was administered with a fifth round of chemotherapy including 600 mg of zuberitamab and gemox regimen (gemcitabine 1.0 g/day, oxaliplatin 150 mg/day 1 q2w) and lenali
Rituximab 600 mg/day, gemcitabine 1 g/day, oxaliplatin 120 mg/day 1 q2w in November 2024. Targeted therapy with zebitumumab 600 mg was administered in January 2025.
The treatment regimen is presented in Table 1.
| Date | Treatment management | Efficacy evaluation |
| December 2017 to April 2018 | In December 2017, modified radical mastectomy for left breast cancer and 4 cycles of EC regimen chemotherapy from December 2017 to March 2018. In April 2018, 4 cycles of chemotherapy were administered using the docetaxel regimen | The therapeutic effect was evaluated as CR |
| June 2018 to May 2021 | Radiotherapy for proliferative lesions with a PTV of 50 Gy/25 fractions for proliferative lesions in the lung posterior right upper lobe in August and tamoxifen endocrine therapy was taken after it. The patient continues to receive treatment with tamoxifen combined with leuprorelin in May 2021 | The therapeutic effect was evaluated as CR |
| August 2023 | Diagnosed as DLBCL. R-CHOP regimen chemotherapy was administered, consisting of rituximab 600 mg/day 1, cyclophosphamide 1200 mg/day 1, doxorubicin 80 mg/day 1, vincristine 2 mg/day 1, and prednisone 100 mg/day 1-5 | The patient developed neutropenia and fever after chemotherapy and then the dose was adjusted |
| September 2023 to December 2023 | R-CHOP chemotherapy rituximab 600 mg/day 1, cyclophosphamide 1000 mg/day 1, pirarubicin 70 mg/day 1, vincristine 2 mg/day 1, and prednisone 100 mg/day 1-5. After second cycle of R-CHOP chemotherapy, CT showed a significant reduction of lymph nodes in the abdominal aorta, bilateral iliac vessels and abdominal compared to before | The therapeutic effect was evaluated as PR |
| January 2024 to February 2024 | In January 2024, the treatment was changed to rituximab 500 mg/day 0, etoposide 0.15 g/day 1-3, ifosfamide 8 g/day 2, carboplatin 0.5 g/day 2. Bone marrow suppression significantly occurred after chemotherapy. In February 2024, the chemotherapy dosage was adjusted to rituximab 600 mg/day 0, etoposide 0.15 g/day 1-2, 0.1 g/day 3, ifosfamide 65 g/day 2, and carboplatin 0.4 g/day 2 | The CT in July showed a reduction in the abdominal tumor, and the therapeutic effect was evaluated as PR |
| April 2024 to August 2024 | From April to June 2024, 4 cycles of chemotherapy using a combination of 600 mg zuberitamab and Gemox regimen. The patient developed grade III bone marrow suppression at last chemotherapy. The fifth round of chemotherapy which included 600 mg of zuberitamab and Gemox regimen and lenalidomide starting from July. Targeted combination chemotherapy was administered in August, specifically consisting of rituximab 600 mg/day, gemcitabine 12 g/day, oxaliplatin 120 mg/day q2w, lenalidomide chemotherapy has been used ever since | The therapeutic effect was evaluated as PR |
| November 2024 until now | Rituximab 600 mg/day, gemcitabine 1 g/day, oxaliplatin 120 mg/day 1 q2w in November 2024. Targeted therapy with zebitumumab 600 mg was be administered in January 2025 | The therapeutic effect was evaluated as CR. Currently, the patient's condition remained stable |
In December 2017, the patient underwent a modified radical mastectomy of left breast cancer and the chemotherapy of EC × 4 and T × 4 scheme. There were no signs of tumor recurrence and metastasis and the therapeutic effect was eva
Examination of the proliferative lesions in the lung posterior right upper lobe in August 2018 following radiotherapy and endocrine therapy did not find any signs of tumor recurrence or metastasis and the therapeutic effect was evaluated as CR.
Following the diagnosis of DLBCL in August 2023, which was treated with the R-CHOP regimen chemotherapy, a follow-up abdominal CT after the second cycle of chemotherapy confirmed that the lymph nodes in the abdominal aorta, bilateral iliac vessels and abdominal were significantly resolved compared to earlier tests, and the therapeutic effect was evaluated as PR (Figure 3A-E). Notably, the therapeutic effect was only evaluated as CR at the sixth cycle of chemothe
Clinically, MPC refers to the existence of two or more different types of primary malignant tumors occurring simultaneously or sequentially in the same patient. Each tumor originates from different tissues and organs and exhibits distinct pathological features, without metastasis or mutually transformation[6]. MPC can be divided into two types: Synchro
To identify similar cases, we conducted a search on PubMed database using the key words, "breast cancer", "lympho
| Year | Patient description | Primary carcinoma | Second primary malignancy | Follow up management | Ref. |
| 1983 | A 52-year-old premenopausal white woman | Breast carcinoma | Aggressive, large cell lymphoma of the ileum (occur to twelve years after diagnosis and five years after the start of chemotherapy) | Treated for breast carcinoma with postoperative adjuvant chest wall irradiation, followed four and seven years later with therapy to spinal ports for palliation of metastatic disease. For the next three and a half years, she received oral cyclophosphamide on a daily basis to a total of more than 110 g | [12] |
| 1989 | A 51-year-old woman | Malignant lymphoma of the breast | Scirrhous carcinoma (two years after the operation) | For primary carcinoma modified radical mastectomy (Patey's method), in combination with chemotherapy (Cyclophosphamide, Vincristine, Prednisolone). for scirrhous carcinoma performed a modified radical mastectomy (Auchincloss' method), followed by chemotherapy (Tegafur) | [13] |
| 1990 | A 53-year-old female | Breast cancer (1980) | Malignant lymphoma of diffuse, small cell type (lymphoplasmacytic) (1988) | Radical mastectomy, followed by irradiation was performed in 1980 | [14] |
| 2002 | A 70-year-old woman | A history of non-Hodgkin’s lymphoma and melanoma | Moderately differentiated infiltrating ductal carcinoma | Underwent a right breast lumpectomy with right axillary lymph node dissection | [15] |
| 2015 | A 55-year-old Caucasian woman | Simultaneous ductal carcinoma in situ of the right breast, and follicular lymphoma involving an inguinal lymph node and the left breast | Multifocal ductal carcinoma of the left breast and reappearance of the lymphoma in the left axillary lymph nodes (2 years later) | The patient underwent local excision and radiotherapy for the ductal carcinoma in situ, while a watch and wait strategy was adopted for the lymphoma. Two years later, underwent bilateral mastectomy, left sentinel node biopsy, and chemotherapy | [16] |
| 2021 | A 58-year-old woman | Breast cancer | Malignant lymphoma and colon cancer (2 years later) | Maliqnant lymphoma and colon cancer that occurred during breast cancer treatment | [17] |
| Year | Patient description | Primary carcinoma | Primary management | Second primary malignancy | Follow up management | Ref. |
| 1998 | An 87-year-old woman | Invasive lobular carcinoma of the breasts | Underwent breast conserving surgery with ipsilateral axillary lymph node dissection | Stage IV diffuse large B-cell lymphoma (REAL classification) | 3 courses of combination chemotherapy, vincristine, cyclophosphamide, idarubicin and prednisolon (CIOP) | [18] |
| 2004 | A 53-year-old woman | Breast cancer | Complete axillary lymph-node dissection | Low grade lymphoma | Not mentioned | [19] |
| 2006 | A 63-year-old woman | Invasive, grade 1, ductal carcinoma | Radiotherapy to left breast and was started on tamoxifen. Chemotherapy with four courses of adriamycin, carmustine, cyclophosphamide, and melphalan | B cell lymphoma, with peripheral mantle cells | Chemotherapy with fludarabine and cyclophosphamide | [20] |
| A 50-year-old woman | Grade 1 invasive ductal carcinoma | Mastectomy | B cell type non-Hodgkin’s lymphoma, mature, follicular (all follicular, grade 1) | Radiotherapy to the left breast and was started on tamoxifen (20 mg daily). Treated with six courses of chlorambucil and dexamethasone | ||
| A 58-year-old woman | Ductal carcinoma in situ of the comedo type | Left mastectomy | Low grade follicular non-Hodgkin’s lymphoma | No systemic treatment | ||
| 2008 | A 50-year-old female | Infltratingductal carcinoma of mucinous type | Axillary lymph a node dissection. The patient refused further radiotherapy treatment for the breast carcinoma | Non-Hodgkin's lymphoma of axillary lymph nodes | Chemotherapy regimen for CLL (cyclophosphamide 300 mg and prednisolone 30 mg daily) | [21] |
| 2010 | 74-year-old woman | Multicentric invasive ductal breast carcinoma | Modified radical right mastectomy with level 2 axillary lymph node dissection | SLL | Chemotherapy, radiation, traztuzumab and hormonal therapy | [22] |
| 74-year-old woman | Invasive lobular breast carcinoma | Wide local excision and sentinel node biopsy | Low-grade B cell lymphoma | 6 weeks of adjuvant radiotherapy followed by an aromatase inhibitor | ||
| 79-year-old woman | Breast cancer | Modified radical right mastectomy with axillary mass excised in continuity with the whole breast | Classical Hodgkin lymphoma | Local irradiation was chosen as initial treatment | ||
| 54-year-old woman | Grade 2, invasive ductal carcinoma | Wide local excision and axillary node dissection | Small lymphocytic B cell lymphoma | The decision was made to treat the lymphoma as a priority; this patient also required radiation treatment to the breast and axilla as well as further chemotherapy for stage IIA breast carcinoma followed by hormonal treatment | ||
| 2010 | A 52-year-old woman | Invasive ductal carcinoma, grade 2 of 3 (moderately differentiated) | Right total mastectomy and right axillary node dissection | Stage 1A follicular lymphoma | An adjuvant chemotherapy regimen, which entailed four cycles of dose dense doxorubicin (60 mg/m2) and cyclophosphamide (600 mg/m2), followed by dose dense paclitaxel | [23] |
| 2011 | A 47-year-old female | Ductal car cinoma right breast | Modified radical mastectomy of right breast | B-cell non-Hodgkin lymphoma | Not mentioned | [24] |
| 2012 | A 72-year-old Japanese woman | Breast tumor | Surgical resection for the breast tumor | IVLBCL | 7 courses of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone) at 3-week intervals | [25] |
| 2014 | A 51-year-old woman | Invasive ductal carcinoma (grade III) | Left modified radical mastectomy with ipsilateral axillary lymph node dissection | Diffuse large B-cell lymphoma | Combination of treatment including surgical excision, chemotherapy, and bone marrow transplantation | [26] |
| 2014 | A 75-year-old Malay woman | PBLs | Modified radical mastectomy with level II axillary clearance | ILBCL | Rituximab, cyclophospha-mide, hydroxydaunorubicin, Oncovin (vincristine) and prednisolone (R-CHOP) chemotherapy regimen | [27] |
| 2014 | A 47-year-old Japanese female | Invasive ductal carcinoma of the right breast | Right mastectomy with sentinel lymph node biopsy and axillary lymph node dissection | Low grade B-cell lymphoma with plasmacytic differentiation | Spontaneous regression of the MALT lymphoma originally | [8] |
| 2014 | A 51-year-old woman | Invasive ductal carcinoma of the breast | Left mastectomy, axillary clearance and right lumpectomy | DLBCL | Epirubicin, vincristine, prednisone and cyclophosphamide (CHOP) chemotherapy with rituximab and planned to follow adjuvant endocrine therapy after chemotherapy | [28] |
| A 47-year-old woman | Invasive ductal carcinoma of the breast | Right mastectomy and axillary clearance | DLBCL | 6-8 cycles of R-CHOP chemotherapy and planned to follow trastuzumab for one year, and adjuvant endocrine therapy after that | ||
| 2017 | A 65-year-old man | Grade II invasive ductal carcinoma (stage IIA) | Modified radical mastectomy | MCL (stage I, group A) | 6 courses of CHOP (A chemotherapy protocol consists of cyclophosphamide 12 g day 1, doxorubicin 80 mg day 1, vindesine 4 mg day 1, and prednisone 90 mg from day 1 to 5) for lymphoma and breast cancer. The patient was also administered endocrine therapy | [29] |
| 2018 | A 73-year-old female | Breast cancer | Not mentioned | DLBCL | Not mentioned | [30] |
| 2020 | An elderly woman | Grade 2 invasive ductal carcinoma with axillary lymphadenopathy | Mastectomy and axillary node dissection | SLL | Not mentioned | [31] |
| 2019 | A woman in her early 60 | Invasive ductal carcinoma | Multidisciplina-breast radiotherapy | Diffuse large B-Cell lymphoma | 3 coures of R-CHOP and 3 courses of R-CEOP | [32] |
| 2021 | A 72-year-old female | Invasive lobular carcinoma of the right breast Stage IIIA (pT2pN3cM0) | Right modified radical mastectomy followed by chemotherapy | Right inguinal lymph node + follicular lymphoma Stage 2 (intermediate risk) | The lymphomas were low grade, which the oncologist closely followed | [33] |
| A 60-year-old female | Stage IIB (pT2pN2acM0) | Right mastectomy and right axillary LN dissection, followed by adjuvant chemotherapy and radiotherapy | Abdominal mesenteric lymph node + follicular lymphoma Stage 2 (intermediate risk) | |||
| A 74-year-old female | Multifocal Stage IB (pT1CpN2acM0) | Left mastectomy and complete left axillary dissection followed by chemotherapy and radiotherapy | Follicular neoplasia in situ in two of her left dissected axillary LNStage 1 (low risk) | |||
| 2021 | A 78-year-old male | Breast mucinous carcinoma | Modified radical left mastectomy with lymph node dissection for mucinous carcinoma | Diffuse large B-cell lymphoma | Hormonal therapy with tamoxifen and chemotherapy with the R-CHOP protocol (cyclophosphamide, doxorubi cin, vincristine, and prednisone; given every 21 days for 6 cycles) in combination | [34] |
| 2021 | A 72-year-old female | T2N1Mx (stage 2) for the breast cancer | The patient underwent courses of CHOP (cyclophosphamide, doxorubicin, vincris-tine, prednisolone) chemotherapy and was planned for surgery | Chronic lympho cytic leukemia/SLL | The patient underwent courses of CHOP (cyclophosphamide, doxorubicin, vincris- tine, prednisolone) chemotherapy and was planned for surgery | [35] |
| 2021 | A 78-year-old woman | Breast invasive ductal carcinoma | Wide local excision of the breast mass with sentinel node biopsy | Abdominal DLBCL | R-CHOP regimen (rituximab 375 mg/m2, vincristine 14 mg/m2, doxorubicin 50 mg/m, cyclophosphamide 750 mg/m2, and prednisolone 100 mg orally). The tumor rapidly relapsed, and the patient received rituximab in combination with gemcitabine and vinorelbine chemotherapy (rituximab 375 mg/m2, gemcitabine 880 mg/m2, vinorelbine 25 mg/m2). Radiotherapy was then administered | [2] |
| 2022 | A 35-year-old woman | Invasive ductal carcinoma with no special type grade III (i.e., poorly differentiated) in the breast | Modified radical mastectomy for stage IIIA IDC | NHL | Received R-CHOP chemotherapy for stage I NHL | [1] |
| 2022 | A 72-year-old female | Infiltrating ductal carcinoma grade III of the right breast | Resection. | NHL, B cell type, high grade | RHCOP for 6 cycles to overcome lymphoma then received hormonal therapy afterwards | [11] |
| 2024 | A 54-year-old post-menopausal female | Breast cancer was staged as Stage IIA | Right breast-conserving surgery with axillary lymph node dissection | DLBCL as Stage IE | 3 cycles of R-CHOP protocol. Recommended weekly paclitaxel for 12 cycles and trastuzumab and pertuzumab for 1 year. Endocrine treatment will be started once chemotherapy is completed | [3] |
Currently, the diagnosis of MPC is challenging, especially for patients with solid tumors as the first primary cancer and hematological or lymphatic system tumors as the second primary cancer. This is because patients present with symptoms such as high fever and lymph node enlargement, requiring that clinicians distinguish them from the recurrence of the first primary cancer or other febrile diseases. In this report, the patient was diagnosed with invasive breast cancer during physical examination and she underwent a modified radical mastectomy to treat the left breast cancer. Notably, the patient did not manifest any symptoms before the identification of NHL. A follow-up PET-CT examination performed five years and nine months after surgery revealed multiple soft tissue nodules in the abdominal aorta and right lower abdominal cavity, with mildly increased glucose metabolism and a PET-CT standard uptake value of 2.0, suggesting a high possibility of hematological disease. Lymph node pathological examination confirmed a diagnosis of DLBCL.
Patients with MPC show poor response to treatments and their prognosis is suboptimal. The pathogenesis of breast cancer complicated with lymphoma is proposed to be a result of antigen stimulation of cancer, low immune function of lymphoma patients, virus infection, chromosome abnormalities, living environment and bad personal lifestyle[11]. Recent studies have proposed a shared immunological predisposition which may underlie the co-occurrence of breast cancer and lymphoma, potentially mediated by therapy-induced antigenicity or genetic mutations common to both malignancies. Previously, Albain and Ultmann[12] reported a rare occurrence of ileocecal diffuse histiocytic lymphoma in a patient administered with large doses of an alkylating agent with radiation therapy for breast carcinoma. In the present case, the patient denied a similar family history and genetic history, and there was no industrial poisons, dust, radioactive sub
This case demonstrates that a correct diagnosis and staging, as well as the involvement of interdisciplinary team to deter
| 1. | Syamsu SA, Setiady R, Smaradania N, Prihantono, Irsandy F, Faruk M. Synchronous breast cancer and non-Hodgkin lymphoma: A case report. Int J Surg Case Rep. 2022;97:107398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 2. | Salemis NS. Synchronous occurrence of breast cancer and refractory diffuse large B-cell abdominal lymphoma: Management and review of the literature. Intractable Rare Dis Res. 2021;10:131-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Yasmeen T, Umar S, Razi MM. Synchronous Invasive Ductal Carcinoma of Breast and Diffuse Large B-cell Lymphoma: A Case Report. J Cancer Allied Spec. 2024;10:655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Li J, Hao C, Wang K, Zhang J, Chen J, Liu Y, Nie J, Yan M, Liu Q, Geng C, Wang X, Wang H, Wang S, Wu J, Yin Y, Song E, Jiang Z. Chinese Society of Clinical Oncology (CSCO) Breast Cancer guidelines 2024. Transl Breast Cancer Res. 2024;5:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 43] [Reference Citation Analysis (0)] |
| 5. | Gradishar WJ, Moran MS, Abraham J, Abramson V, Aft R, Agnese D, Allison KH, Anderson B, Bailey J, Burstein HJ, Chen N, Chew H, Dang C, Elias AD, Giordano SH, Goetz MP, Jankowitz RC, Javid SH, Krishnamurthy J, Leitch AM, Lyons J, McCloskey S, McShane M, Mortimer J, Patel SA, Rosenberger LH, Rugo HS, Santa-Maria C, Schneider BP, Smith ML, Soliman H, Stringer-Reasor EM, Telli ML, Wei M, Wisinski KB, Yeung KT, Young JS, Schonfeld R, Kumar R. Breast Cancer, Version 3.2024, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2024;22:331-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 295] [Article Influence: 147.5] [Reference Citation Analysis (0)] |
| 6. | Ueda Y, Makino Y, Tochigi T, Ota Y, Hidaka H, Nakamura T, Beppu K, Ohuchida J, Odate S, Terasaka S, Nishida T, Yoshida M, Kimura R, Marutsuka K, Otomo N. A rare case of synchronous multiple primary malignancies of breast cancer and diffuse large B-cell lymphoma that responded to multidisciplinary treatment: a case report. Surg Case Rep. 2022;8:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | De Luca A, Frusone F, Vergine M, Cocchiara R, La Torre G, Ballesio L, Monti M, Amabile MI. Breast Cancer and Multiple Primary Malignant Tumors: Case Report and Review of the Literature. In Vivo. 2019;33:1313-1324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Matsuda I, Watanabe T, Enomoto Y, Takatsuka Y, Miyoshi Y, Hirota S. Spontaneous regression of primary extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) colliding with invasive ductal carcinoma of the breast: a case report. Int J Clin Exp Pathol. 2014;7:7020-7027. [PubMed] |
| 9. | Pisani F, Romano A, Anticoli Borza P, Marino M, Micheli A, Botti C, Petti MC. Diffuse large B-cell lymphoma involving the breast. A report of four cases. J Exp Clin Cancer Res. 2006;25:277-281. [PubMed] |
| 10. | Demirci U, Ozdemir N, Benekli M, Babacan NA, Cetin B, Baykara M, Coskun U, Zengin N, Buyukberber S. Lymphoproliferative disorders in multiple primary cancers. Asian Pac J Cancer Prev. 2012;13:383-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Chomariyati A, Diansyah MN, Amrita PNA, Romadhon PZ, Yudho Bintoro SU, Ashariati A, Savitri M. How to prioritize treatment in dual malignancy: A case report of patient with non-Hodgkin lymphoma and breast cancer. Ann Med Surg (Lond). 2022;81:104300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 12. | Albain KS, Ultmann JE. Aggressive large cell lymphoma of the ileum after long-term cyclophosphamide therapy for breast carcinoma. Am J Med. 1983;75:882-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Kobayashi R, Osada T, Hamaguchi M, Ohi T, Inden Y, Hara K, Tomiyama J, Kitayama J, Tsukui G, Kobori O. [A carcinoma of the right breast arising after a mastectomy in primary malignant lymphoma of the left breast]. Gan No Rinsho. 1989;35:1077-1080. [PubMed] |
| 14. | Kohno A, Kohriyama K, Arimori S. [Breast cancer and B cell malignant lymphoma associated with Sjögren'ssyndrome--a case report and review of literature in Japan]. Ryumachi. 1990;30:388-393, 395; discussion 393. [PubMed] |
| 15. | Pohland ML, Joyce JM, Myers DT, Petursson SR. Incidental detection of primary breast carcinoma with a modified coincident camera in a patient with non-Hodgkin's lymphoma and melanoma. Clin Nucl Med. 2002;27:825-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Michalinos A, Vassilakopoulos T, Levidou G, Korkolopoulou P, Kontos M. Multifocal Bilateral Breast Cancer and Breast Follicular Lymphoma: A Simple Coincidence? J Breast Cancer. 2015;18:296-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Machinaga M, Kitahara M, Takeuchi N, Watanabe Y, Saito H, Ijima T, Hozumi Y. [A Case of Triple Cancer-A Patient Developed Malignant Lymphoma and Colon Cancer, during Breast Cancer Treatment]. Gan To Kagaku Ryoho. 2021;48:1397-1399. [PubMed] |
| 18. | Niedermayr A, Gharehbaghi K, Pacher B, Wirth M, Grünberger W. Coincidence of primary non-Hodgkin's lymphoma and invasive lobular carcinoma of the breasts--clinical diagnosis and management. Acta Oncol. 1998;37:305-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Benoit L, Arnould L, Collin F, Fraisse J, Cuisenier J, Chauffert B. Concurrent lymphoma and metastatic breast carcinoma in the axillary, confounding sentinel lymph-node biopsy. Eur J Surg Oncol. 2004;30:462-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Cox J, Lunt L, Webb L. Synchronous presentation of breast carcinoma and lymphoma in the axillary nodes. Breast. 2006;15:246-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Al-Hussaini MA, Al-Masad JK, Awidi AA. Carcinoma of breast co-existing with non-Hodgkin's lymphoma of axillary lymph nodes. Saudi Med J. 2008;29:138-141. [PubMed] |
| 22. | Cuff KE, Dettrick AJ, Chern B. Synchronous breast cancer and lymphoma: a case series and a review of the literature. J Clin Pathol. 2010;63:555-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Laudenschlager MD, Tyler KL, Geis MC, Koch MR, Graham DB. A rare case of synchronous invasive ductal carcinoma of the breast and follicular lymphoma. S D Med. 2010;63:123-125. [PubMed] |
| 24. | Siddiqui FA, Maheshwari V, Alam K, Jain A. Coexistent non-Hodgkins lymphoma and ductal carcinoma breast: diagnosis on fine needle aspiration cytology. Diagn Cytopathol. 2011;39:767-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Niiyama S, Amoh Y, Katsuoka K. Generalized telangiectasia as the manifestation of intravascular large B-cell lymphoma complicated with breast cancer. Eur J Dermatol. 2012;22:566-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 26. | Liu W, Zhu H, Zhou X. Synchronous bilateral non-Hodgkin's diffuse large B-cell lymphoma of the breast and left breast invasive ductal carcinoma: a case report and review of literature. Int J Clin Exp Pathol. 2014;7:7042-7048. [PubMed] |
| 27. | Ho CW, Mantoo S, Lim CH, Wong CY. Synchronous invasive ductal carcinoma and intravascular large B-cell lymphoma of the breast: a case report and review of the literature. World J Surg Oncol. 2014;12:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Zhong J, Di L, Zheng W. Synchronous breast cancer and breast lymphoma: two case reports and literature review. Chin J Cancer Res. 2014;26:355-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 29. | Liu J, Wei H, Zhu K, Lai L, Han X, Yang Y. Male breast cancer and mantle cell lymphoma in a single patient: A case report and literature review. Medicine (Baltimore). 2017;96:e8911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Hołody Ł, Kunikowska J, Braziewicz J. Simultaneous breast cancer and DLBCL lymphoma - role of PET/CT examination with 18F-FDG and 18F-FES. Nucl Med Rev Cent East Eur. 2018;21:113-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Haynes HR, Rose DSC. Synchronous small lymphocytic lymphoma and metastatic breast carcinoma in axillary lymph nodes: Preservation of follicular architecture only in the portions of affected lymph nodes involved by metastatic carcinoma. Breast J. 2020;26:245-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Fujii T, Ohno N, Matsui T, Sahara N, Yoneyama S, Inoue H, Matsunaga T. [A Case of Synchronous Diffuse Large B-Cell Lymphoma of the Right Breast and Invasive Ductal Carcinoma of the Left Breast]. Gan To Kagaku Ryoho. 2019;46:1775-1778. [PubMed] |
| 33. | Saleem T, Mi K, Pathak R, Yari K, Lu K. Concurrent Breast Carcinoma and Follicular Lymphoma: A Case Series. Am J Case Rep. 2021;22:e931772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 34. | Kim SY, Lee JY. Multiple Primary Malignant Neoplasms: A Case Report of Breast Mucinous Carcinoma and Extramammary Diffuse Large B-Cell Lymphoma in a Male Patient. Taehan Yongsang Uihakhoe Chi. 2021;82:729-736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 35. | Zakhartseva L, Yanovytska M. Collision breast cancer and chronic lymphocytic leukemia/small lymphocytic lymphoma in a single lymph node (clinical case). Exp Oncol. 2021;43:274-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/