Published online May 24, 2025. doi: 10.5306/wjco.v16.i5.104398
Revised: March 11, 2025
Accepted: March 18, 2025
Published online: May 24, 2025
Processing time: 152 Days and 10.9 Hours
Simultaneous oncological and reconstructive plastic surgery on the mammary gland in the treatment of cancer is currently one of the important stages in the psychological rehabilitation of patients. In order to achieve a good cosmetic result, reconstruction must be performed simultaneously with radical surgical treatment. Currently, there are a large number of methods for performing breast recon
Core Tip: Simultaneous oncological and reconstructive plastic surgery on the mammary gland in the treatment of cancer is currently one of the important stages in the psychological rehabilitation of patients. Flap necrosis during oncoplastic surgery can compromise the procedure. Unfortunately, this is a frequent complication in oncoplastic surgery. Doppler ultrasonography imaging, indocyanine green imaging and cover of the breast implant with inferior mammary ligament can provide better outcomes in patients who undergo subcutaneous mastectomy for breast cancer.
- Citation: Sukhotko AS, Bumbu A, Covantsev S. Preservation of the nipple-areolar complex during subcutaneous mastectomy: A surgical and diagnostic method. World J Clin Oncol 2025; 16(5): 104398
- URL: https://www.wjgnet.com/2218-4333/full/v16/i5/104398.htm
- DOI: https://dx.doi.org/10.5306/wjco.v16.i5.104398
Breast cancer is the leading cause of cancer death and account for 6.9% of cancer-related deaths worldwide[1]. The treatment includes surgery, chemotherapy, radiotherapy, endocrine therapy, targeted therapy, and immunotherapy, which often requires an oncological consilium and multidisciplinary team of healthcare providers. Surgery is often the main treatment option for patients with breast cancer and it has changed dramatically over the past four decades due to cultural and social aspects of the disease[2]. These changes lead to the emergence of a special branch of breast surgery called oncoplastic surgery.
Oncoplastic surgery is a type of procedure that involves plastic surgery techniques for reconstruction or correction of the breast[3]. The term has evolved over the years and now represents any surgery maintain quality of life and allows acceptable breast appearance and does not affect in a negative way the oncological effectiveness[4].
There are many types of oncoplastic procedures. They can be classified into prosthetic reconstruction (tissue expander or implant) and flaps (personal tissue)[5]. Recently there have been several attempts to combine these methods with the use of 3D printing[6]. However, every procedure is associated with possible complications especially in case of subcutaneous mastectomy in patients with ptosis when there is possible vascular compromise. Therefore, we have adapted a special method for reconstruction that lowers the risk of skin and areola necrosis as well as implant-related complications.
Position of the nipple-areolar complex (NAC) is one of the important factors for oncoplastic surgery. Preoperative degree of ptosis can be categorized by the Regnault classification, that aims to assesses the breast according to the relative position of the nipple to the inframammary fold[7]. As a result, there are several grades of ptosis. Grade 1 (mild ptosis)-the nipple is at the level of the inframammary fold. Grade 2 (moderate ptosis)-the nipple is below the level of the inframammary fold but is not the most dependent part of the breast. Grade 3 (severe ptosis)-the nipple is below the inframammary fold and is the most dependent part of the breast[7].
Subcutaneous mastectomy can be associated with early (16.8%) and late (34.2%) complications[8]. Early complications related to vascular insufficiency include nipple-areola necrosis in 6.4% of cases, nipple necrosis in 2.8% and skin flap necrosis in 0.6%[8]. While late complications usually are associated with the implant and include capsular contracture in 22.2% of cases, prosthesis dislocation in 8.2% and prosthesis extrusion in 3.8%[8].
The NAC has complex overlapping vascularity from different arterial sources. The blood supply to the nipple is provided by the internal mammary artery perforators, lateral thoracic and thoracoacromial arteries, intercostal arteries[9]. However, the sum of the two lower quadrants represents the greatest vascularization of the breast[10]. Therefore, the NAC an important anatomical point where the vascular supply can be compromised[11].
Currently, there are a large number of methods for performing breast reconstruction. One of the most commonly used is radical subcutaneous/skin-sparing mastectomy with simultaneous reconstruction with a silicone endoprosthesis. Grand W Carlson type technique is used, with skin incisions in the form of an inverted T is usually performed in patients with large mammary gland with severe grade III ptosis, as the patients usually require reduction of excess skin. However, the most vulnerable aspects of this type of reconstruction is the impossibility of preserving the NAC, which is associated with a high risk of developing such complications as partial/complete necrosis of the NAC.
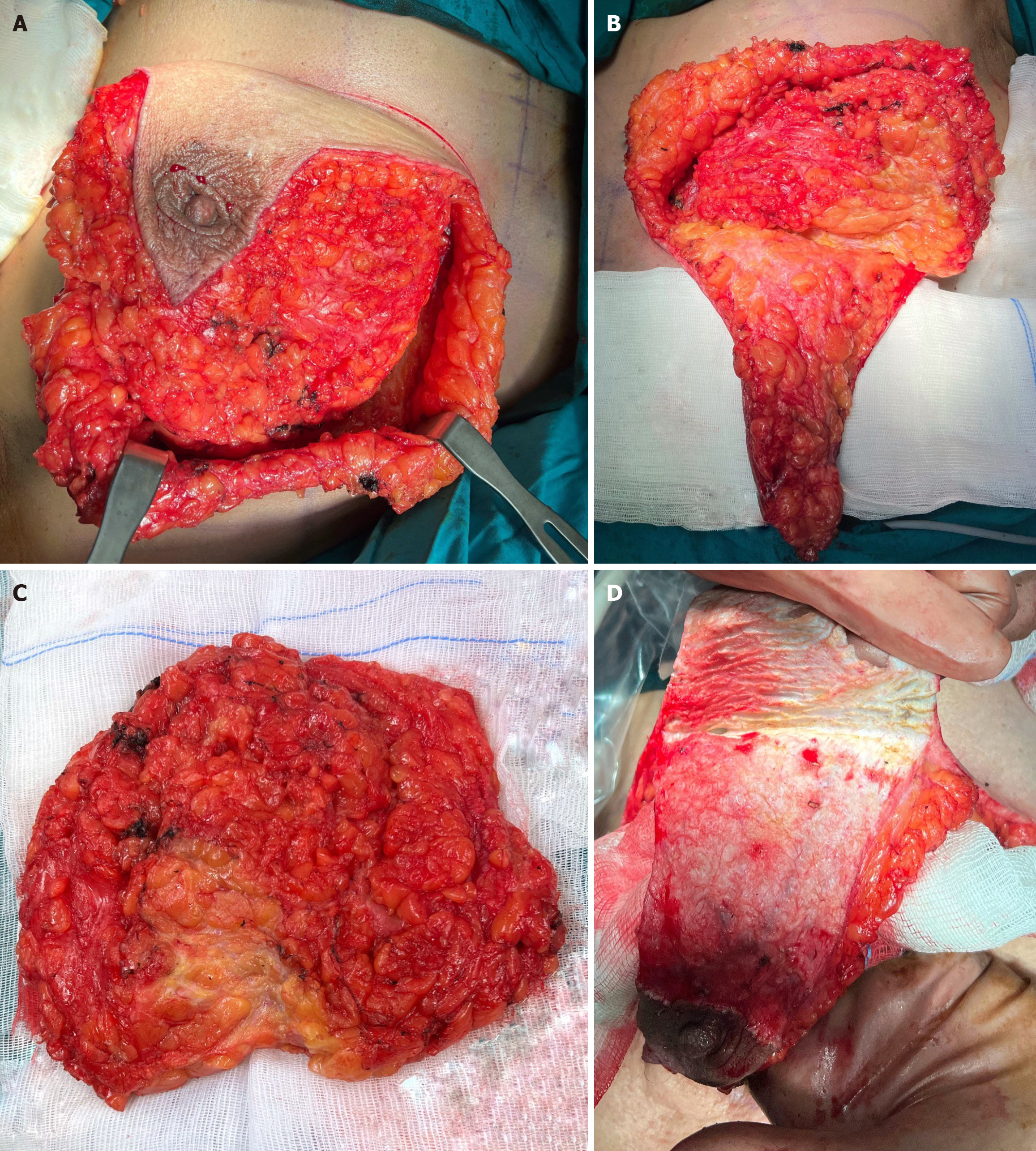
The main feature of subcutaneous mastectomy with de-epithelialized lower dermal fat flap with preserving of the NAC is the dissection of breast tissue along the Scarpa fascia. This technique ultimately reduces the risk of the lateral and medial cutaneous fat flaps vessels damage, thereby, minimizing the risk of ischemic necrosis in the inframammary crease region and NAC impaired blood supply (Figure 1A).
When dissecting breast tissue, it is necessary to preserve inframammary crease ligament in order to achieve physiological ptosis (Figure 1B). The breast tissue is completely removed along with the underlying fascia of the pectoralis major (Figure 1C). The next step is delicate de-epithelization of the skin, so blood vessels are left intact as much as possible (Figure 1D).
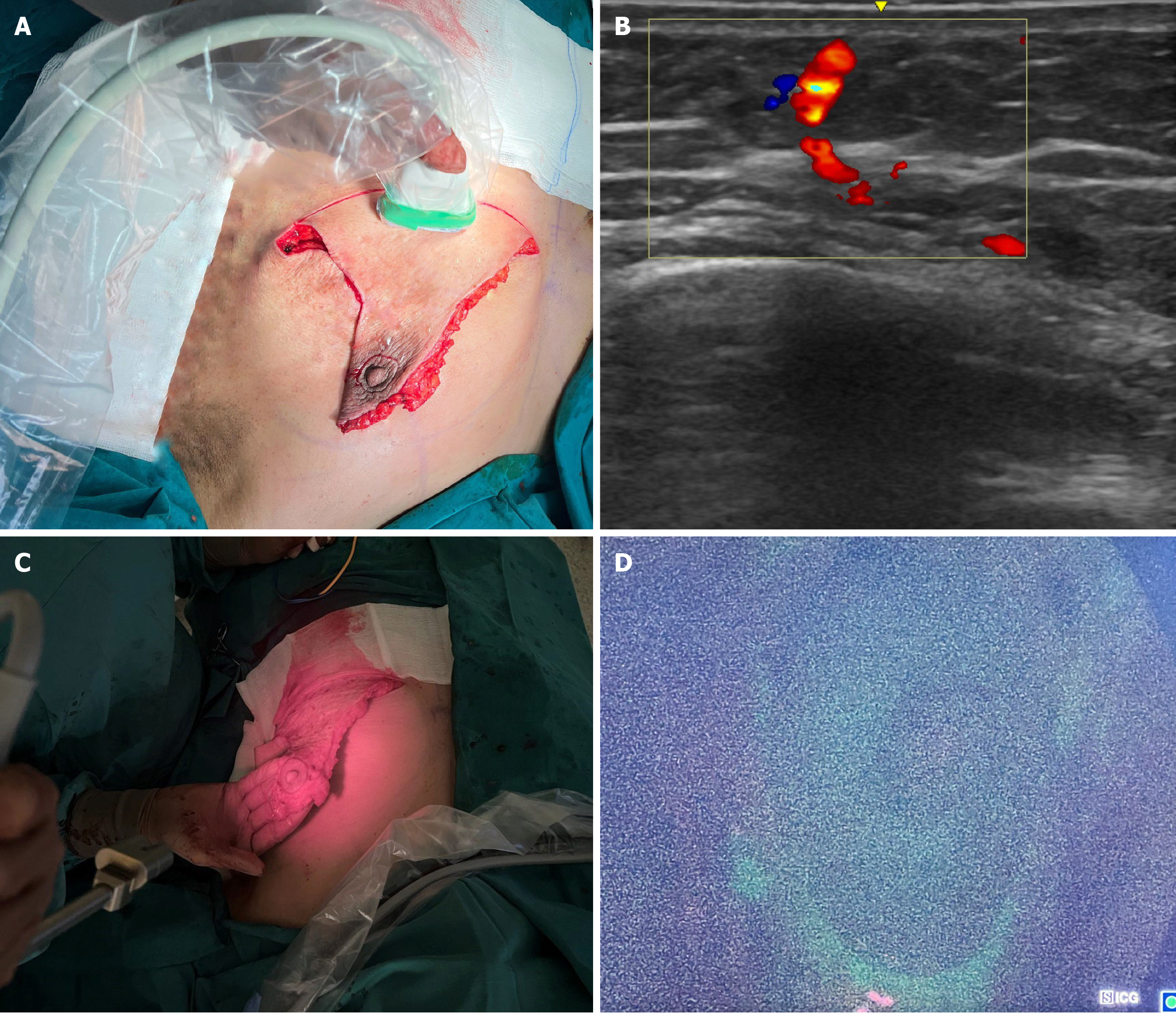
In this case, the NAC remains on the lower pedicle. Intraoperatively, Doppler ultrasound is additionally performed to assess the blood flow velocity in the pedicle (Figure 2A and B).
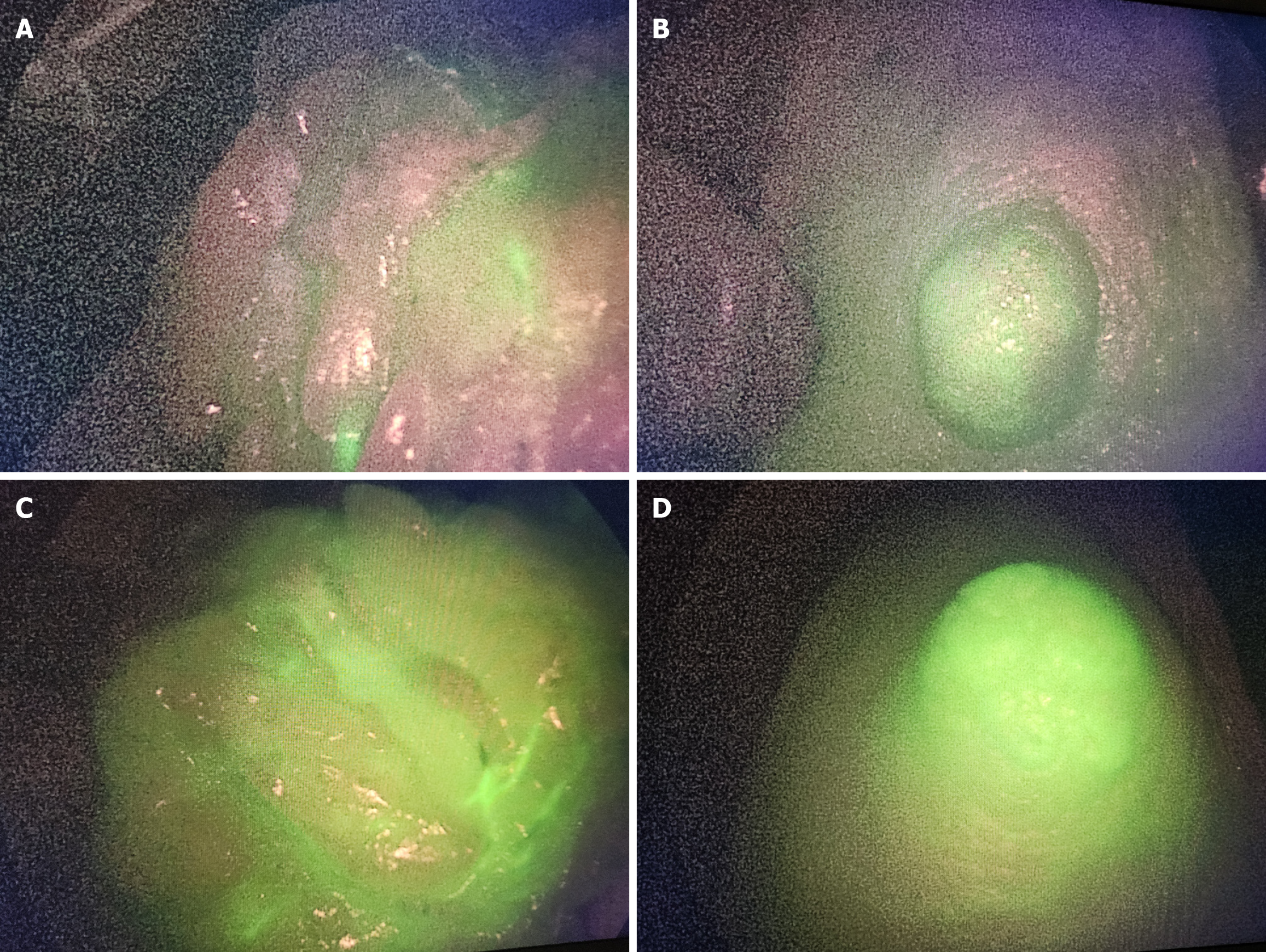
To assess the adequacy of blood supply to cutaneous fat flap, intraoperative fluorescence angiography with indocyanine green (ICG) may be used. ICG (1.5 mL) is injected intravenously and the NAC blood supply is assessed (Figure 2C and D). The usual dosage for assessment of perfusion is 0.1-0.3 mg per kg. This dye is widely used in the angiographic evaluation of large vessels and has the lowest rate of allergic reactions. Using fluorescence imaging system, the blood supply of the lower de-epithelized flap along with NAC is assessed in 2-3 minutes after ICG administration (Figure 2D, Figure 3).
The lower pedicle is supplied directly by perforators of the internal thoracic artery extending from the V-VI intercostal space. The combination of lower dermal flap and ICG blood supply imaging makes it possible to more accurately assess patient's anatomical features and determine the indications for the NAC preservation (Figure 3).
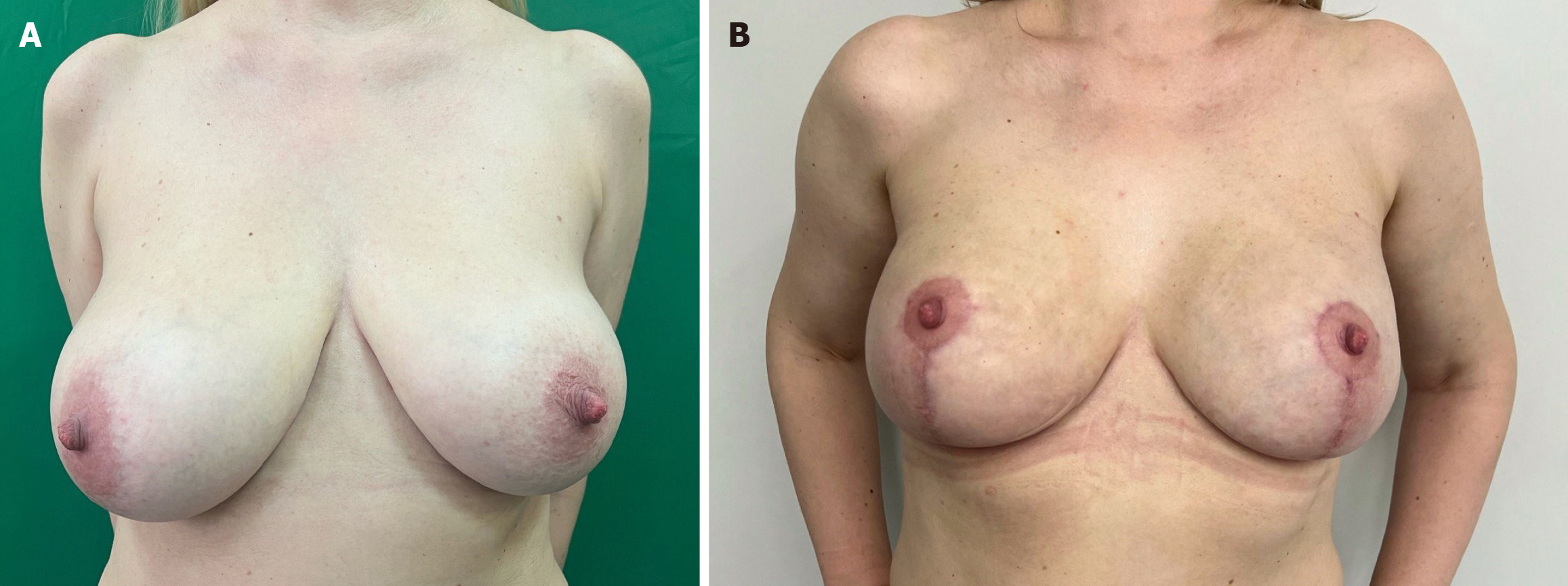
When choosing a breast endoprosthesis, in order to obtain a good aesthetic result, it is necessary to choose models with a high and extra-high projection (Figure 4).
A silicone implant is installed on the pectoralis major muscle and a de-epithelized flap is applied on the implant in the inferior region. Then the lateral and medial skin flaps are fixed to the central part of the de-epithelized flap and brought together at the bottom of the submammary fold. In the superior region the silicone endoprosthesis remains covered only with lateral and medial skin flaps. The NAC is placed to a new position and the wound is sutured cosmetically. Thus, this method allows to maintain NAC blood supply using lower de-epithelialized flap.
The preoperative and postoperative results of this procedure are demonstrated in Figure 4.
Breast surgery will always be a mix of oncological, plastic, and microsurgery. Therefore, these type of procedure should be provided by a team of specialists[4]. Of course, it is possible to have one surgeon who will incorporate all of these features, however, this is not always possible as it requires rigorous and long training in different surgical aspects[12].
Technological advancement made it possible to rely on both simple and more complex methods to assess vascular supply of tissue segment. Ultrasonography (USG) with Doppler imaging proved to be simple method to examine a flaps[13]. It allows to evaluate basic blood flow, vascular distribution and diameter, flow velocity, flow volume, vascular resistance, and arterial waveform that altogether are essential to examine the hemodynamics of the flap[14]. ICG is a newer technique to facilitates the detection of perforators in tissue flaps and can help to evaluate flap microcirculation and perfusion[15,16]. The combination of these methods together can guide surgeons intraoperatively to decrease the risk of postoperative flap necrosis.
The future of breast implants is now aimed at the use of new tissues that are more compatible with the human body. Although, breast implants have improved over the years and the medium lifespan is 10.8-16.4 years depending on the material, type and manufacturer there are still possibilities for improvement and necessity to decrees postoperative complications[17-19]. It seems that 3D printing will be more frequently used for tissue transplant and reconstruction creating more opportunities for those patients who can benefit from these procedures[20-22].
The sensitivity and specificity of these methods (ICG and Doppler imaging) deserves separate attention. The sensitivity of intraoperative ICG is 90.9%, and the accuracy is 98.6%, while Doppler USG has 100% sensitivity and 82% specificity[15,23,24]. The use of both methods intraoperatively can help surgeons to assess perfusion during subcutaneous mastectomies at the level of NAC.
Flap necrosis during oncoplastic surgery can compromise the procedure. Unfortunately, this is a frequent complication in oncoplastic surgery. Doppler USG imaging, ICG imaging and cover of the breast implant with inferior mammary ligament can provide better outcomes in patients who undergo subcutaneous mastectomy for breast cancer.
| 1. | Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5690] [Cited by in RCA: 12416] [Article Influence: 6208.0] [Reference Citation Analysis (6)] |
| 2. | Sakorafas GH. Breast cancer surgery--historical evolution, current status and future perspectives. Acta Oncol. 2001;40:5-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Hoffmann J, Wallwiener D. Classifying breast cancer surgery: a novel, complexity-based system for oncological, oncoplastic and reconstructive procedures, and proof of principle by analysis of 1225 operations in 1166 patients. BMC Cancer. 2009;9:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Macmillan RD, McCulley SJ. Oncoplastic Breast Surgery: What, When and for Whom? Curr Breast Cancer Rep. 2016;8:112-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 5. | Shaitelman SF, Jeruss JS, Pusic AL. Oncoplastic Surgery in the Management of Breast Cancer. J Clin Oncol. 2020;38:2246-2253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Sukhotko AS, Covantsev S, Kovaleva MV. Tissue engineering in breast reconstruction: a look into the future. Iberoam J Med. 2023;5:141-142. [DOI] [Full Text] |
| 7. | Lee S, Lee J, Lee S, Bae Y. Oncoplastic breast surgery with latissimus dorsi myocutaneous flap for large defect in patients with ptotic breasts: is it feasible when combined with local flaps? World J Surg Oncol. 2014;12:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Metere A, Fabiani E, Lonardo MT, Giannotti D, Pace D, Giacomelli L. Nipple-Sparing Mastectomy Long-Term Outcomes: Early and Late Complications. Medicina (Kaunas). 2020;56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Spring MA, Macias LH, Nadeau M, Stevens WG. Secondary augmentation-mastopexy: indications, preferred practices, and the treatment of complications. Aesthet Surg J. 2014;34:1018-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Salas-López A, Morgado-Águila C, López-de-Celis C, Rodríguez-Sanz J, Ortiz-Miguel S, Pérez-Bellmunt A. Breast Vascularization and Its Implication in Breast Reduction and Mastopexy Surgery: Anatomical Study. J Pers Med. 2024;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Teng E, Broer PN, Heidekrueger PI, Forte AJ, Lentz R, Durand M, Raghu M, Kwei SL. In Vivo Changes of Breast Perfusion After Augmentation. Aesthet Surg J. 2016;36:1133-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Chatterjee A, Dayicioglu D, Khakpour N, Czerniecki BJ. Oncoplastic Surgery: Keeping It Simple With 5 Essential Volume Displacement Techniques for Breast Conservation in a Patient With Moderate- to Large-Sized Breasts. Cancer Control. 2017;24:1073274817729043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Taylor GI, Doyle M, McCarten G. The Doppler probe for planning flaps: anatomical study and clinical applications. Br J Plast Surg. 1990;43:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 170] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Ogino A, Onishi K. Vascular waveform analysis of flap-feeding vessels using color Doppler ultrasonography. Plast Surg Int. 2014;2014:249670. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Li K, Zhang Z, Nicoli F, D'Ambrosia C, Xi W, Lazzeri D, Feng S, Su W, Li H, Ciudad P, Tremp M, Zhang YX. Application of Indocyanine Green in Flap Surgery: A Systematic Review. J Reconstr Microsurg. 2018;34:77-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 16. | Choudhary S, Khanna S, Mantri R, Arora P. Role of Indocyanine Green Angiography in Free Flap Surgery: A Comparative Outcome Analysis of a Single-Center Large Series of 877 Consecutive Free Flaps. Indian J Plast Surg. 2023;56:208-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 17. | Goodman CM, Cohen V, Thornby J, Netscher D. The life span of silicone gel breast implants and a comparison of mammography, ultrasonography, and magnetic resonance imaging in detecting implant rupture: a meta-analysis. Ann Plast Surg. 1998;41:577-85; discussion 585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Brown SL, Middleton MS, Berg WA, Soo MS, Pennello G. Prevalence of rupture of silicone gel breast implants revealed on MR imaging in a population of women in Birmingham, Alabama. AJR Am J Roentgenol. 2000;175:1057-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 101] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Sukhotko A, Covantsev S, Bumbu A, Kovaleva M, Zakurdaev E. Surgical treatment after augmentation mammoplasty with polyacrylamide hydrogel. Folia Med (Plovdiv). 2024;66:578-582. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Mayer HF, Coloccini A, Viñas JF. Three-Dimensional Printing in Breast Reconstruction: Current and Promising Applications. J Clin Med. 2024;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 21. | Hummelink S, Verhulst AC, Maal TJJ, Ulrich DJO. Applications and limitations of using patient-specific 3D printed molds in autologous breast reconstruction. Eur J Plast Surg. 2018;41:571-576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Tomita K, Yano K, Hata Y, Nishibayashi A, Hosokawa K. DIEP Flap Breast Reconstruction Using 3-dimensional Surface Imaging and a Printed Mold. Plast Reconstr Surg Glob Open. 2015;3:e316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Lohman RF, Ozturk CN, Ozturk C, Jayaprakash V, Djohan R. An Analysis of Current Techniques Used for Intraoperative Flap Evaluation. Ann Plast Surg. 2015;75:679-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 24. | Sorotos M, Firmani G, Tornambene R, Marrella D, Paolini G, Santanelli di Pompeo F. DIEP flap perfusion assessment using microdialysis versus Doppler ultrasonography: A comparative study. Microsurgery. 2024;44:e31097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/