Published online Nov 24, 2022. doi: 10.5306/wjco.v13.i11.907
Peer-review started: July 28, 2022
First decision: September 5, 2022
Revised: September 8, 2022
Accepted: November 6, 2022
Article in press: November 6, 2022
Published online: November 24, 2022
Processing time: 115 Days and 7.9 Hours
Epidemiological studies of chronic pancreatitis (CP) and its association with pancreatic ductal adenocarcinoma (PDAC) are limited. Understanding demo
To evaluate the ethno-racial risk factors for CP and its association with PDAC. The secondary aim was to evaluate hospitalization outcomes in patients admitted with CP and PDAC.
This retrospective cohort study used the 2016 and 2017 National Inpatient Sample databases. Patients included in the study had ICD-10 codes for CP and PDAC. The ethnic, socioeconomic, and racial backgrounds of patients with CP and PDAC were analyzed.
Hospital admissions for CP was 29 per 100000, and 2890 (0.78%) had PDAC. Blacks [adjusted odds ratio (aOR) 1.13], men (aOR 1.35), age 40 to 59 (aOR 2.60), and being overweight (aOR 1.34) were significantly associated with CP (all with P < 0.01). In patients with CP, Whites (aOR 1.23), higher income, older age (aOR 1.05), and being overweight (aOR 2.40) were all significantly associated with PDAC (all with P < 0.01). Men (aOR 1.81) and Asians (aOR 15.19) had significantly increased mortality (P < 0.05). Hispanics had significantly increased hospital length of stay (aOR 5.24) (P < 0.05).
Based on this large, nationwide analysis, black men between 40-59 years old and overweight are at significantly increased risk for admission with CP. White men older than 40 years old and overweight with higher income were found to have significant associations with CP and PDAC. This discrepancy may reflect underlying differences in healthcare access and utilization among different socioeconomic and ethno-racial groups.
Core Tip: What is known chronic pancreatitis (CP) and pancreatic ductal adenocarcinoma (PDAC) rates are rising. Pancreatitis admissions costed 133 million dollars, and accounted for the 3rd leading cause of hospital admissions. There is lack of data identifying those at highest risk for admissions with CP and PDAC. What we found Black men between 40-59 years old and overweight are at significantly increased risk for admission with CP. White men with higher income were found to have significantly increased risk for admissions with CP and PDAC. Asians/Pacific Islanders had the highest risk for mortality from CP and PDAC.
- Citation: Lew D, Kamal F, Phan K, Randhawa K, Cornwell S, Bangolo AI, Weissman S, Pandol SJ. Epidemiologic risk factors for patients admitted with chronic pancreatitis and pancreatic ductal adenocarcinoma in the United States. World J Clin Oncol 2022; 13(11): 907-917
- URL: https://www.wjgnet.com/2218-4333/full/v13/i11/907.htm
- DOI: https://dx.doi.org/10.5306/wjco.v13.i11.907
The overall incidence of chronic pancreatitis (CP) is increasing worldwide, and accounts for significant healthcare utilization and costs. In the United States, CP hospital admissions costed 133 million dollars, and pancreatitis accounted for the 3rd leading cause of hospital admissions among gastrointestinal diseases in 2015[1]. The most common reason for CP-related admission is abdominal pain, but other complications can develop including pancreatic ductal adenocarcinoma (PDAC). PDAC is currently the fourth leading cause of cancer-related deaths in the United States and is projected to become the second leading cause by 2030[2]. CP is the major risk factor for developing PDAC[3-5].
There have been few epidemiological studies available for CP[6-14], and fewer studies for CP and PDAC[3,15-18]. Ethnic and socioeconomic factors including insurance status, median income, type and hospital factors are lacking.
Herein, we utilize hospital discharges from a large nationwide database to examine the demographic, ethno-racial, socioeconomic, and hospital factors associated with hospitalizations for CP and its association with PDAC. We also sought to determine the association between ethnicity/race on hospitalization outcomes in patients admitted with CP and PDAC.
This retrospective cohort study utilized the 2016 and 2017 National Inpatient Sample (NIS) databases. The NIS is a database of inpatient stays derived from billing data based upon discharge abstracts. As such, it contains de-identified clinical and nonclinical elements at both the patient and hospital level. The NIS 2016 database contains data from 7.1 million hospital stays in 4575 hospitals in 47 states, while the 2017 database contains data from 7.1 million hospital stays in 4584 hospitals in 48 states. Using the combination of the NIS 2016 and 2017 databases allowed for inclusion of a greater total number of cases/patients.
Patients included in the study carried a primary diagnosis of CP based on ICD-10 codes (K86.0, K86.1, K90.3). The demographics and ethnic/racial profiles of those with CP were compared to the general population and examined for any associations. Subsequently, all patients with CP were then evaluated for PDAC based on ICD-10 diagnostic codes C25.0-C25.9. The demographic and ethnic/racial profiles of those with only CP were compared to the ethnic/racial profiles of those who also had PDAC and were examined for any associations. Finally, we analyzed the associations between ethnicity/race and hospitalization outcomes in patients admitted for PDAC.
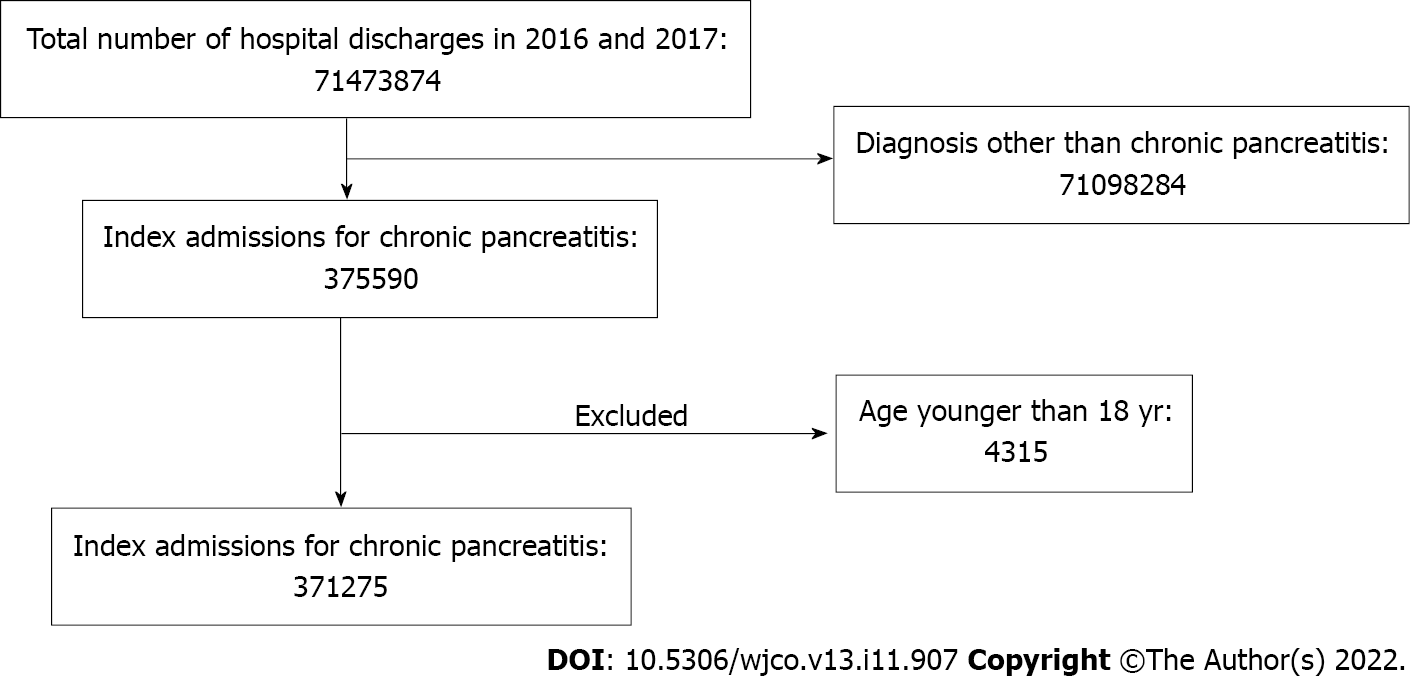
Inclusion and exclusion criteria are shown in Figure 1. Institutional Review Board approval was not required for this study as it was performed using de-identified and nationally available data.
The estimated national population during 2016-2017 was obtained from the United States Census Bureau (www.census.gov).
Patient demographics included age, gender, race, median household income, primary expected payer, hospital bed size, hospital teaching status, hospital region, and urban location. Burden of comorbidities was assessed using the Charlson comorbidity index.
The primary outcomes were the ethno-racial factors associated with CP hospital admissions as compared to the general population and the ethno-racial factors associated between CP and PDAC. Secondary outcomes were the associations between ethnicity/race and hospitalization outcomes (mortality, hospital length of stay (LOS), expenses), in patients admitted with CP and PDAC.
Statistical analyses were performed using STATA, version 16.0 (StataCorp., College Station, Texas, United States). Weighting of patient-level observations was implemented. Univariate analysis was initially performed to calculate unadjusted odds ratio and determine confounders significantly associated with the outcomes. Multivariate regression analysis was used to adjust for potential confounders. Multivariate regression model was then built by including all confounders that were found to be significant by univariate analysis, to calculate an adjusted odds ratio (aOR). Logistic regression was used for binary outcomes and linear regression was used for continuous outcomes. Proportions were compared using Fisher’s exact test, and continuous variables were compared using Student’s t-test. All P-values were two-sided, with 0.05 as the threshold for statistical significance. Calculated rates of hospital admissions per 100000 population was performed using the United States Census Bureau national population estimates.
In our sample (NIS 2016-2017) of 14.2 million admissions, 371275 (2.6%) adult patients were found to have a diagnosis of CP. The mean age was 57.72 years, and most patients were white (64.82%) men (55.76%). Medicare was the primary payer insurance (40.2%). The majority of admissions were in teaching hospitals (69.54%). Additional patient and hospital characteristics are presented in Table 1. Overall hospitalization rate for 2016 and 2017 was 29 per 100000 (95%CI: 57.9-58.2).
| Variable | n = 371275 |
| Race | |
| White | 64.82% |
| Black | 22.35% |
| Hispanic | 8.4% |
| Asian or Pacific Islander | 1.31% |
| Native American | 0.87% |
| Other | 2.25% |
| Gender | |
| Women | 44.24% |
| Men | 55.76% |
| Age | |
| Mean age, years | 52.72 |
| Age 18-39 yr | 21.63% |
| Age 40-59 yr | 49.84% |
| Age 60-79 yr | 24.26% |
| Age > 80 yr | 4.28% |
| Insurance provider | |
| Medicare | 40.2% |
| Medicaid | 30.28% |
| Private | 22.53% |
| Uninsured | 6.99% |
| Charlson comorbidity index | |
| 0 | 24.09% |
| 1 | 25.97% |
| 2 | 17.37% |
| 3 or more | 32.58% |
| Median income in patient zip code | |
| $1–$38999 | 36.17% |
| $39000–$47999 | 26.11% |
| $48000–$62999 | 21.78% |
| $63000 | 15.94% |
| Hospital region | |
| Northwest | 17.54% |
| Midwest | 24.63% |
| South | 40.23% |
| West | 17.6% |
| Hospital location | |
| Rural | 8.29% |
| Urban | 91.71% |
| Hospital size | |
| Small | 19% |
| Medium | 28.34% |
| Large | 52.65% |
| Type of hospital | |
| Teaching | 69.54% |
| Non-teaching | 30.46% |
On multivariate regressions analysis, men (aOR 1.35), Blacks (aOR 1.13), age between 40 and 59 years old (aOR 2.60), and body mass index (BMI) between 25 and 29.9 (aOR 1.34) were at higher risk of developing CP as compared to the general population (P < 0.01). On the contrary, women (aOR 0.65), Hispanics (aOR 0.63) or Asian/Pacific Islanders (aOR 0.50) and those above 80 years old (aOR 0.46) had a significantly decreased likelihood of having CP as compared to the general population (all with P < 0.01) (Table 2).
| Classification | P value | |
| Age | aOR 0.98 | < 0.01 |
| Age 18-39 yr | Reference | |
| Age 40-59 yr | aOR 2.60 | < 0.01 |
| Age 60-79 yr | aOR 0.96 | 0.37 |
| Age > 80 yr | aOR 0.46 | < 0.01 |
| BMI: 18-24.9 | Reference | |
| BMI: 25-29.9 | aOR 1.34 | < 0.01 |
| BMI: 30-39.9 | aOR 0.62 | < 0.01 |
| Women | aOR 0.65 | < 0.01 |
| Whites | Reference | |
| Blacks | 1.13 | < 0.01 |
| Hispanics | 0.63 | < 0.01 |
| Asians/Pacific Islanders | 0.50 | < 0.01 |
| Native Americans | 1.05 | 0.31 |
| Other | 0.67 | < 0.01 |
Of the 371275 adult patients admitted with a primary diagnosis of CP, 2890 (0.78%) also had PDAC. Patients with PDAC and CP were significantly older (P < 0.05), White (P < 0.01), had Medicare as the primary insurance (P < 0.01), were from a higher income population (P < 0.01), were admitted to teaching hospitals (P < 0.01), and had a higher burden of comorbidities (P < 0.01) (Table 3). Overall hospitalization rate for 2016 and 2017 was 0.45 per 100000 (95%CI: 0.44-0.47).
| Variable | CP without PDAC (n = 368385) | CP with PDAC (n = 2890) | P value |
| Race | < 0.01 | ||
| Whites | 64.75% | 74.22% | |
| Blacks | 22.4% | 16.76% | |
| Hispanics | 8.43% | 4.97% | |
| Asians or Pacific Islanders | 1.31% | 1.29% | |
| Native Americans | 0.87% | 0.37% | |
| Other | 2.25% | 2.39% | |
| Gender | |||
| Women | 44.27% | 40.31% | 0.07 |
| Men | 55.73% | 59.69% | |
| Age | |||
| Mean age, years | 52.61 | 66.32 | < 0.05 |
| Age 18-39 yr | 21.78% | 19% | |
| Age 40-59 yr | 50.02% | 26.99% | |
| Age 60-79 yr | 23.97% | 60.03% | |
| Age > 80 yr | 4.23% | 11.07% | |
| Insurance provider | < 0.01 | ||
| Medicare | 40.04% | 60.64% | |
| Medicaid | 30.44% | 10.73% | |
| Private | 22.5% | 26.48% | |
| Uninsured | 7.03% | 2.15% | |
| Charlson comorbidity index | < 0.01 | ||
| 0 | 24.28% | 0 | |
| 1 | 26.17% | 0 | |
| 2 | 17.35% | 19.38% | |
| 3 or more | 32.2% | 80.62% | |
| Median income in patient zip code | < 0.01 | ||
| $1–$38999 | 36.24% | 28.22% | |
| $39000–$47999 | 26.1% | 26.81% | |
| $48000–$62999 | 21.78% | 21.34% | |
| $63000 | 15.88% | 23.63% | |
| Hospital region | 0.68 | ||
| Northwest | 17.53% | 19.38% | |
| Midwest | 24.64% | 23.53% | |
| South | 40.25% | 38.24% | |
| West | 17.59% | 18.86% | |
| Hospital location | < 0.01 | ||
| Rural | 8.34% | 1.56% | |
| Urban | 91.66% | 98.44% | |
| Hospital size | < 0.01 | ||
| Small | 19.08% | 8.65% | |
| Medium | 28.43% | 16.78% | |
| Large | 52.48% | 74.57% | |
| Type of hospital | |||
| Teaching | 69.41% | 86.16% | < 0.01 |
| Non-teaching | 30.59% | 13.84% |
On multivariate regressions analysis, older age (greater than 40 years old) (aOR 1.05), and BMI between 25 and 29.9 (aOR 2.40) had a higher risk of developing PDAC in patients with CP (all with P < 0.01). On the contrary, women (aOR 0.77), Blacks (aOR 0.77) and Hispanics (aOR 0.66) were associated with a significantly decreased likelihood of PDAC in patients with CP (all with P < 0.01) (Table 4).
| Classification | P value | |
| Age | aOR 1.05 | < 0.01 |
| Age 18-39 yr | Reference | |
| Age 40-59 yr | aOR 6.79 | < 0.01 |
| Age 60-79 yr | aOR 24.17 | < 0.01 |
| Age > 80 yr | aOR 21.02 | < 0.01 |
| BMI: 18-24.9 | Reference | |
| BMI: 25-29.9 | aOR 2.40 | < 0.01 |
| Female | aOR 0.77 | < 0.01 |
| White | Reference | |
| Black | aOR 0.77 | < 0.05 |
| Hispanic | aOR 0.66 | < 0.05 |
| Asian or Pacific Islander | aOR 0.69 | 0.36 |
| Native American | aOR 0.68 | 0.60 |
| Other | aOR 0.97 | 0.94 |
Men (aOR 1.81) and Asians/Pacific Islanders (aOR 15.19) had the highest mortality among patients with PDAC and CP (all with P < 0.05). Hispanics had the highest hospital LOS (aOR 5.24), charges (adjusted coefficient $87285), and costs (adjusted coefficient $15212) amongst patients with PDAC and CP (all with P < 0.05). Gender was not found to be a significant contributing factor for hospital expenses.
In this nationwide cohort study, we found black men who were overweight had a significantly increased likelihood of being admitted with CP. These findings are consistent with previous studies, most likely due to alcoholic CP, though our current study is not able to definitively elucidate the cause of CP[14]. Our hospitalization rates for CP is much higher compared to the study by Yang et al[13], which also used the NIS database from 1988-2004 and found an incident rate of 7.0-8.1 per 100000 population[13]. Similarly, population-based studies from Olmsted County, MN, United States found an incident rate of 4.05 per 100000 population from 1997-2006 and Allegheny County, PA, United States found incident rate of 7.75 per 100000 population[11,12]. Our findings of an increased incidence rate may reflect recent trends in increased hospitalizations with pancreatitis being the 3rd most common reason for hospitalization in 2015 among gastrointestinal diseases[1]. This is likely due in part to increased use of cross-sectional imaging for the evaluation of abdominal pain in adults[19]. Another possible explanation is that our findings may be more of a reflection of prevalence rate rather than incidence rate. In 2014, Lévy et al[20] summarized 11 studies and found a prevalence rate ranging up to 41.76 per 100000 population[20]. Additionally, patients with CP are reported to have good overall survival despite complications with reported 10-year survival rate of 70%[17]. Taken together, our increased hospitalization rate is likely due to increased diagnosis of CP and longevity of patients with CP.
Other novel demographic findings from our study include the findings that patients with CP-related admissions had predominantly Medicare insurance and were from lower median income families. Additionally, we found patients were more likely to be admitted to teaching hospitals in large urban centers, predominantly in the Southern part of the United States. A potential reason for this finding may correlate with the South having the highest prevalence of obesity at 30% and higher. Furthermore, non-Hispanic Blacks were found to have the highest prevalence of obesity[21]. Our hope is that future studies can use our findings to further evaluate the exact association of CP-related admissions in this high-risk population in an effort to improve patient outcomes and decrease healthcare expenditures. While our study is not able to elucidate the reason for admission, it is presumed that abdominal pain is most likely the cause given extensive findings from previous studies[14,22]. Given that it is well established that abdominal pain is chronic, persistent, and can lead to significant impairment in quality of life including high rates of unemployment as well as recurrent hospitalizations and healthcare expenditure, future research in this area is needed[23,24]. The findings from our study can be used in future studies to target those patients at higher risk for CP-related hospitalizations to improve patient outcomes and limit healthcare expenditures.
A potential complication of CP is the development of PDAC. In our study, we found that 0.78% (approximately 0.39%/year) of patients with CP also carried a diagnosis of PDAC and that these patients were predominantly White men who were overweight and of older age. Our findings are similar to the 2014 Danish nationwide study by Bang et al[3], which found a 4.26% rate over a 15-year period (approximately 0.28%/year) of PDAC in CP patients occurring predominantly in older men[3]. While there is moderate amount of literature for the ethno-racial factors for CP and PDAC separately, there is limited data regarding ethno-racial factors specifically in patients with CP and PDAC. Bracci et al[25] in 2009 found in a multicenter study that majority of patients with PDAC were White men who were older, however, they did not provide demographic data specifically for PDAC in CP patients[25]. In a meta-analysis published in 2010 containing 22 studies, Raimondi et al[15] found a 13 fold increased risk for PDAC in CP patients but did not evaluate the ethno-racial factors[15]. A more recent meta-analysis published in 2017 by Kirkegård et al[4] also found an increased risk for PDAC in CP patients but again did not evaluate the ethno-racial factors[4]. To our knowledge, our study is the first to evaluate ethno-racial factors in patients with CP and PDAC. A major caveat to our findings is that we cannot definitively evaluate PDAC development as a progression of CP. Thus, there could be cases where PDAC occurred first and CP developed afterwards. However, current literature suggests the overwhelming likelihood of this occurring is extremely low and may actually be misclassifications given the similarities between the two diseases[4]. An interesting finding from our study was that we found that Blacks had a higher risk for having CP, but this did not translate into having a higher association with CP and PDAC. A potential explanation could be due to discrepancies in healthcare utilization given that our data showed patients with CP and PDAC were significantly more likely to have higher median incomes, lower rates of being uninsured, and high rates of being admitted to large urban teaching hospitals when compared to CP patients alone. Racial disparities have been shown for PDAC in blacks. Khawja et al[26] conducted an evidence-based review of PDAC in blacks and found significantly worse outcomes compared to whites. A 2019 review also showed blacks had worse outcomes, but also lower referral rates to see oncology or a surgeon and lower rates of surgical resection and adjuvant chemoradiation[26,27]. Potential reasons for this discrepancy include suboptimal patient communication, greater mistrust of the medical field, and unmeasured differences in morbidity/functional status. Future studies should further evaluate the accuracy of this finding and to evaluate the exact cause of this discrepancy if one exists. Another interesting finding from our study is that we found Asians/Pacific Islanders had an aOR 15.19. This is in contrast to recent data from the American Cancer Society, which showed Blacks had the highest risk of mortality at 15.0/100000 compared to 8.1/100000 with Asians/Pacific Islanders[2]. A possible explanation is that our study evaluated patients with PDAC and CP rather than all PDAC patients, though it is beyond the scope of this study as to why Asians/Pacific Islanders had the highest mortality. Finally, we found that Hispanics had the highest LOS and hospital expenses. Future studies should further evaluate these findings in an effort to identify reasons for increased mortality among Asians/Pacific Islanders and increased LOS and hospital expenses among Hispanics, respectively, to improve patient outcomes and decreased healthcare expenditures.
Limitations of this study include it being limited solely to inpatient encounters. Therefore, our study may not represent a complete epidemiological study given its lack of outpatient encounters. As mentioned previously, there are limitations associated with using the NIS database. We are not able to identify individual patients and review each patients’ charts, thus we are not able to identify the reason for CP-related admissions though current literature suggest most likely related to abdominal pain. Additionally, we are not able to determine if patients with CP progressed to PDAC or if PDAC occurred before CP, but again current literature suggests majority of patients develop PDAC after CP. Incidence of PDAC in CP is related to etiology of CP. Risk is significantly higher in hereditary pancreatitis than with alcohol related pancreatitis. As the etiology is not captured in the database it might introduce bias. Duration of CP could not be found, as longer history associated with increased risk. Findings may be applicable only to the population studied and cannot be generalized.
In conclusion, based on this large, nationwide analysis, there is an increased trend in hospitalization rates for CP, predominantly among black men between 40-59 years old who were overweight. In patients with CP, white men older than 40 years old who were overweight with higher income had a higher risk of PDAC. The observed disparity may be a consequence of the difference in healthcare access among different ethnic groups.
Chronic pancreatitis (CP) and pancreatic ductal adenocarcinoma (PDAC) rates are rising. Pancreatitis admissions costed 133 million dollars, and accounted for the 3rd leading cause of hospital admissions. There is lack of data identifying those at highest risk for admissions with CP and PDAC.
The main motivation of this study was to establish racial risk factors and their associations with PDAC.
This study had the objective to examine the demographic, ethno-racial, socioeconomic, and hospital factors associated with hospitalizations for CP and its association with PDAC.
This retrospective study used the 2016 and 2017 National Inpatient Sample databases. ICD-10 codes compatible with CP and PDAC were used in the study. The ethnic, socioeconomic, and racial backgrounds of patients with CP and PDAC were analyzed.
Hospital admissions for CP was 29 per 100000, and 2890 (0.78%) had PDAC. Blacks [adjusted odds ratio (aOR) 1.13], men (aOR 1.35), age 40 to 59 (aOR 2.60), and being overweight (aOR 1.34) were significantly associated with CP (all with P < 0.01). In patients with CP, Whites (aOR 1.23), higher income, older age (aOR 1.05), and being overweight (aOR 2.40) were all significantly associated with PDAC (all with P < 0.01). Men (aOR 1.81) and Asians (aOR 15.19) had significantly increased mortality (P < 0.05). Hispanics had significantly increased hospital length of stay (aOR 5.24) (P < 0.05).
There is an increased trend in hospitalization rates for CP, predominantly among black men between 40-59 years old who were overweight. Wealthy white men above the age of 40 had a higher PDAC diagnosis.
Black men between 40-59 years old and overweight are at significantly increased risk for admission with CP. White men with higher income were found to have significantly increased risk for admissions with CP and PDAC. Asians/Pacific Islanders had the highest risk for mortality from CP and PDAC.
| 1. | Peery AF, Crockett SD, Murphy CC, Lund JL, Dellon ES, Williams JL, Jensen ET, Shaheen NJ, Barritt AS, Lieber SR, Kochar B, Barnes EL, Fan YC, Pate V, Galanko J, Baron TH, Sandler RS. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology. 2019;156:254-272.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 776] [Cited by in RCA: 1122] [Article Influence: 160.3] [Reference Citation Analysis (2)] |
| 2. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13300] [Cited by in RCA: 15624] [Article Influence: 2232.0] [Reference Citation Analysis (11)] |
| 3. | Bang UC, Benfield T, Hyldstrup L, Bendtsen F, Beck Jensen JE. Mortality, cancer, and comorbidities associated with chronic pancreatitis: a Danish nationwide matched-cohort study. Gastroenterology. 2014;146:989-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 166] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 4. | Kirkegård J, Mortensen FV, Cronin-Fenton D. Chronic Pancreatitis and Pancreatic Cancer Risk: A Systematic Review and Meta-analysis. Am J Gastroenterol. 2017;112:1366-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 368] [Article Influence: 40.9] [Reference Citation Analysis (0)] |
| 5. | Munigala S, Kanwal F, Xian H, Agarwal B. New diagnosis of chronic pancreatitis: risk of missing an underlying pancreatic cancer. Am J Gastroenterol. 2014;109:1824-1830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 6. | Díte P, Starý K, Novotný I, Precechtelová M, Dolina J, Lata J, Zboril V. Incidence of chronic pancreatitis in the Czech Republic. Eur J Gastroenterol Hepatol. 2001;13:749-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Lankisch PG, Assmus C, Maisonneuve P, Lowenfels AB. Epidemiology of pancreatic diseases in Lüneburg County. A study in a defined german population. Pancreatology. 2002;2:469-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 127] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Lévy P, Barthet M, Mollard BR, Amouretti M, Marion-Audibert AM, Dyard F. Estimation of the prevalence and incidence of chronic pancreatitis and its complications. Gastroenterol Clin Biol. 2006;30:838-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 108] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 9. | Lin Y, Tamakoshi A, Matsuno S, Takeda K, Hayakawa T, Kitagawa M, Naruse S, Kawamura T, Wakai K, Aoki R, Kojima M, Ohno Y. Nationwide epidemiological survey of chronic pancreatitis in Japan. J Gastroenterol. 2000;35:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 70] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | O'Sullivan JN, Nobrega FT, Morlock CG, Brown AL Jr, Bartholomew LG. Acute and chronic pancreatitis in Rochester, Minnesota, 1940 to 1969. Gastroenterology. 1972;62:373-379. [PubMed] |
| 11. | Yadav D, Muddana V, O'Connell M. Hospitalizations for chronic pancreatitis in Allegheny County, Pennsylvania, USA. Pancreatology. 2011;11:546-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Yadav D, Timmons L, Benson JT, Dierkhising RA, Chari ST. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Am J Gastroenterol. 2011;106:2192-2199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 297] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 13. | Yang AL, Vadhavkar S, Singh G, Omary MB. Epidemiology of alcohol-related liver and pancreatic disease in the United States. Arch Intern Med. 2008;168:649-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 190] [Article Influence: 10.6] [Reference Citation Analysis (1)] |
| 14. | Wilcox CM, Sandhu BS, Singh V, Gelrud A, Abberbock JN, Sherman S, Cote GA, Al-Kaade S, Anderson MA, Gardner TB, Lewis MD, Forsmark CE, Guda NM, Romagnuolo J, Baillie J, Amann ST, Muniraj T, Tang G, Conwell DL, Banks PA, Brand RE, Slivka A, Whitcomb D, Yadav D. Racial Differences in the Clinical Profile, Causes, and Outcome of Chronic Pancreatitis. Am J Gastroenterol. 2016;111:1488-1496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 15. | Raimondi S, Lowenfels AB, Morselli-Labate AM, Maisonneuve P, Pezzilli R. Pancreatic cancer in chronic pancreatitis; aetiology, incidence, and early detection. Best Pract Res Clin Gastroenterol. 2010;24:349-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 402] [Cited by in RCA: 439] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 16. | Shelton CA, Umapathy C, Stello K, Yadav D, Whitcomb DC. Hereditary Pancreatitis in the United States: Survival and Rates of Pancreatic Cancer. Am J Gastroenterol. 2018;113:1376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 72] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 17. | Lowenfels AB, Maisonneuve P, Cavallini G, Ammann RW, Lankisch PG, Andersen JR, Dimagno EP, Andrén-Sandberg A, Domellöf L. Pancreatitis and the risk of pancreatic cancer. International Pancreatitis Study Group. N Engl J Med. 1993;328:1433-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1255] [Cited by in RCA: 1154] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 18. | Malka D, Hammel P, Maire F, Rufat P, Madeira I, Pessione F, Lévy P, Ruszniewski P. Risk of pancreatic adenocarcinoma in chronic pancreatitis. Gut. 2002;51:849-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 309] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 19. | Wang RC, Kornblith AE, Grupp-Phelan J, Smith-Bindman R, Kao LS, Fahimi J. Trends in Use of Diagnostic Imaging for Abdominal Pain in U.S. Emergency Departments. AJR Am J Roentgenol. 2021;216:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Lévy P, Domínguez-Muñoz E, Imrie C, Löhr M, Maisonneuve P. Epidemiology of chronic pancreatitis: burden of the disease and consequences. United European Gastroenterol J. 2014;2:345-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 21. | CDC. National Center for Health Statistics-Adult Obesity Prevalence Maps. [cited 10 July 2022]. Available from: https://www.cdc.gov/obesity/data/prevalence-maps.html. |
| 22. | Wilcox CM, Yadav D, Ye T, Gardner TB, Gelrud A, Sandhu BS, Lewis MD, Al-Kaade S, Cote GA, Forsmark CE, Guda NM, Conwell DL, Banks PA, Muniraj T, Romagnuolo J, Brand RE, Slivka A, Sherman S, Wisniewski SR, Whitcomb DC, Anderson MA. Chronic pancreatitis pain pattern and severity are independent of abdominal imaging findings. Clin Gastroenterol Hepatol. 2015;13:552-60; quiz e28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 140] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 23. | Mullady DK, Yadav D, Amann ST, O'Connell MR, Barmada MM, Elta GH, Scheiman JM, Wamsteker EJ, Chey WD, Korneffel ML, Weinman BM, Slivka A, Sherman S, Hawes RH, Brand RE, Burton FR, Lewis MD, Gardner TB, Gelrud A, DiSario J, Baillie J, Banks PA, Whitcomb DC, Anderson MA; NAPS2 Consortium. Type of pain, pain-associated complications, quality of life, disability and resource utilisation in chronic pancreatitis: a prospective cohort study. Gut. 2011;60:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 242] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 24. | Pezzilli R, Morselli-Labate AM, Frulloni L, Cavestro GM, Ferri B, Comparato G, Gullo L, Corinaldesi R. The quality of life in patients with chronic pancreatitis evaluated using the SF-12 questionnaire: a comparative study with the SF-36 questionnaire. Dig Liver Dis. 2006;38:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Bracci PM, Wang F, Hassan MM, Gupta S, Li D, Holly EA. Pancreatitis and pancreatic cancer in two large pooled case-control studies. Cancer Causes Control. 2009;20:1723-1731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Khawja SN, Mohammed S, Silberfein EJ, Musher BL, Fisher WE, Van Buren G 2nd. Pancreatic cancer disparities in African Americans. Pancreas. 2015;44:522-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 92] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 27. | Noel M, Fiscella K. Disparities in Pancreatic Cancer Treatment and Outcomes. Health Equity. 2019;3:532-540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 114] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Kalayarasan R, India; Tan CL, China; Zhao CF, China S-Editor: Fan JR L-Editor: A P-Editor: Fan JR