Published online Feb 24, 2019. doi: 10.5306/wjco.v10.i2.75
Peer-review started: October 17, 2018
First decision: November 27, 2018
Revised: December 31, 2018
Accepted: January 23, 2019
Article in press: January 23, 2019
Published online: February 24, 2019
Processing time: 128 Days and 9 Hours
The treatment of metastatic colorectal cancer (mCRC) relies of chemotherapy. The efficacy of the standard FOLFIRI-therapy could be improved by a modification of the regimen by splitting the dose of irinotecan on day 1 and day 3 in the FOLFIRI3 regimen.
To determine safety and efficacy of FOLFIRI3 regimen.
This is a monocentric retrospective study evaluating the efficacy and safety of the FOLFIRI3 regimen given alone or in combination with bevacizumab or aflibercept in patients with previously treated mCRC.
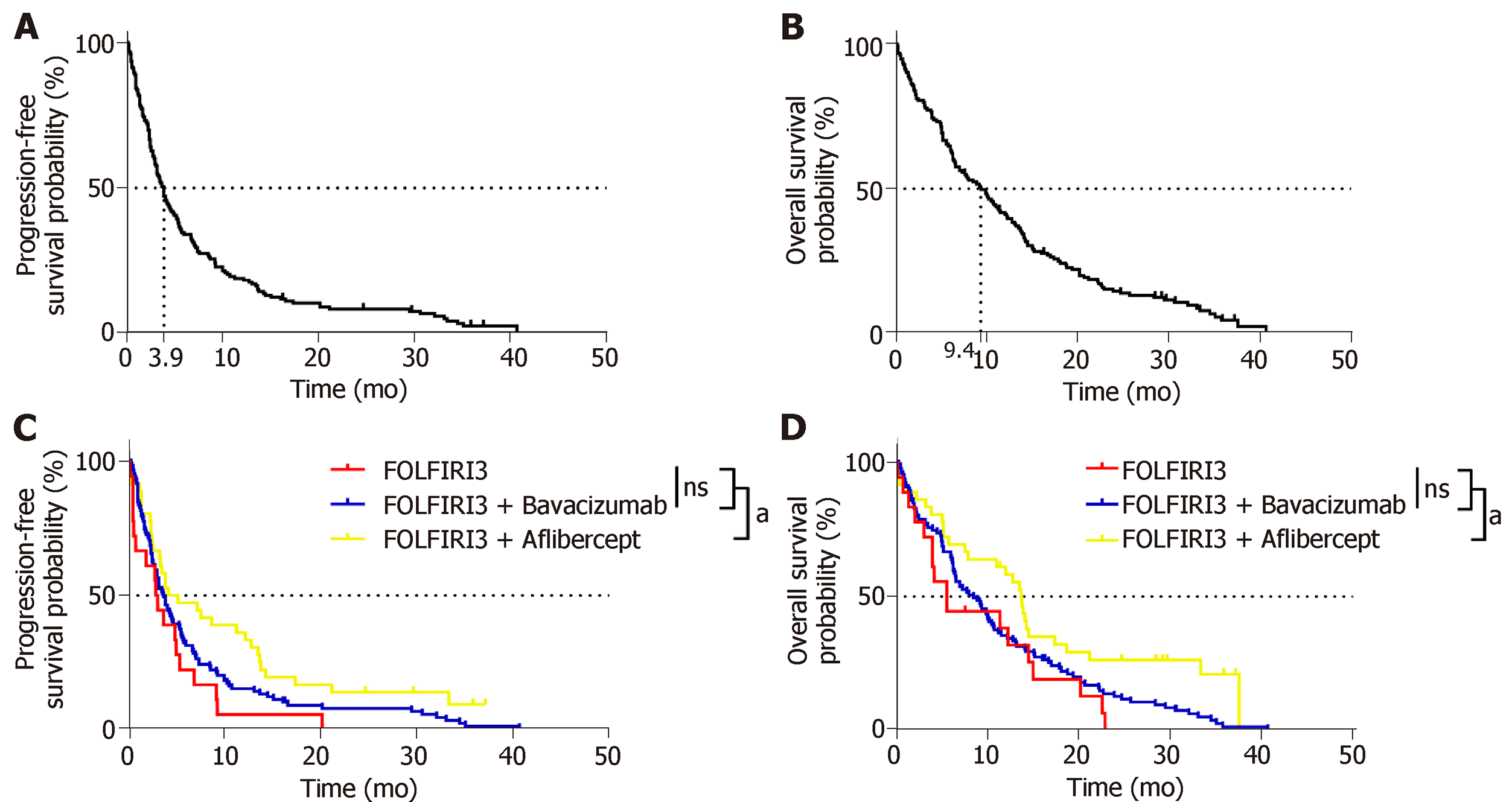
One hundred and fifty-three consecutive patients were included (18 treated with FOLFIRI3, 99 with FOLFIRI3 plus bevacizumab and 36 with FOLFIRI3 plus aflibercept). The overall response rate (ORR) and disease control rate were 51% and 62%, respectively. Similar ORRs were observed in all 3 cohorts. Median progression-free survival (PFS) and overall survival (OS) were 3.9 mo (95%CI: 3.2-4.9) and 9.4 mo (95%CI: 6.6-12), respectively. Median PFS and OS values were improved in the FOLFIRI3 plus aflibercept group. The most common grade 3-4 adverse events were diarrhoea (21.6%) and neutropenia (11.8%), and these toxicities were more frequent in the FOLFIRI3 plus aflibercept group. According to the multivariate Cox proportional model, previous surgery of metastasis and aflibercept were associated with outcomes.
The modification of the FOLFIRI regimen impacted treatment response of mCRC patients. The addition of an antiangiogenic agent, in particular aflibercept, enhanced the clinical benefit and improved survival.
Core tip: This retrospective study suggests that modified FOLFIRI with injection of irinotecan at day 1 and 3 is interesting for patients with previously treated metastatic colorectal cancer. Surprisingly the efficacy of the FOLFIRI3-aflibercept seems superior the FOLFIRI3 alone or in combination with bevacizumab. Prospective randomized trial comparing FOLFIRI-aflibercept to FOLFIRI3-aflibercept in second line are warranted.
- Citation: Devaux M, Gerard L, Richard C, Bengrine-Lefevre L, Vincent J, Schmitt A, Ghiringhelli F. Retrospective evaluation of FOLFIRI3 alone or in combination with bevacizumab or aflibercept in metastatic colorectal cancer. World J Clin Oncol 2019; 10(2): 75-85
- URL: https://www.wjgnet.com/2218-4333/full/v10/i2/75.htm
- DOI: https://dx.doi.org/10.5306/wjco.v10.i2.75
Metastatic colorectal cancer (mCRC) is a common disease in western countries[1]. In the absence of resection of all metastatic and primary tumours, the treatment of mCRC remains palliative. The standard of care involves chemotherapeutic protocols that include fluoropyrimidine in combination with oxaliplatin or irinotecan. Anti EGFR mAb and antiangiogenic drugs such as bevacizumab and aflibercept can be used in combination with chemotherapy to improve response rate, progression free survival and overall survival (OS)[2]. Recently, regorafenib and TAS-102 were developed as new therapeutic options upon failure of classical chemotherapeutic regimens[3,4]. In most mCRC patients, doublet chemotherapy using fluoropyrimidine-based chemotherapy with either irinotecan (FOLFIRI) or oxaliplatin (FOLFOX) in combination with anti EGFR or an antiangiogenic agent is considered the standard first-line of treatment. Second-line drug selection mainly depends on the regimen used in the first-line chemotherapy. Chemotherapy is frequently used in combination with antiangiogenic agents (bevacizumab, aflibercept, ramucirumab) or anti-EGFR agents when the RAS mutation is present[5-10].
Previous reports proposed that the standard FOLFIRI regimen could be optimized by splitting the dose of irinotecan into two days. Half of the total dose is administered on day 1 prior to 5-FU dosing and the other half of the dose is administered on day 3 after 5-FU dosing. This protocol was named FOLFIRI3 regimen[11]. Despite their similarities, the FOLFIRI3 regimen benefits from an increased response rate compared to the classical FOLFIRI regimen[11,12]. A previous report suggests that FOLFIRI3 plus bevacizumab could also be used to improve the response rate and overcome resistance to previous treatment with FOLFIRI[13].
Recently, aflibercept was approved as a second-line chemotherapy in combination with FOLFIRI for mCRC patients whose cancer progressed after oxaliplatin based chemotherapy. This treatment is a new second-line chemotherapeutical option in addition to the previously established[8], but association with of aflibercept with FOLFIRI3 was not reported and compared with FOLFIRI3 or FOLFIRI3 plus bevacizumab.
In this retrospective study, we report a large cohort of patients treated with the FOLFIRI3 regimen and compare the safety and efficacy of FOLFIRI3 alone and in combination with bevacizumab or aflibercept.
This study was a retrospective, monocentric study performed at Centre Georges François Leclerc, Dijon France.
Study includes all consecutive patients treated with the FOLFIRI3 regimen for mCRC in our centre. From January, 2008 to December, 2017, patients were identified through the chemotherapy prescription computer software programme used at the cancer centre (CHIMIO®, Computer Engineering). The database was declared to the National French Commission for bioinformatics data and patient liberty (CNIL). The study was performed in agreement with French regulations with approval from the local institutional review boards. A general informed consent was signed by all cancer patients at the time of their first hospitalization in the cancer centre, enabling patient clinical and biological data analysis in this cohort study. Demographics, cancer history, toxicity according to the Common Toxicity Criteria [Common Toxicity Criteria (CTC) v2.0 (http://cancer.gov/)], and treatment outcomes, as well as pathological, clinical, biological, and radiological data [tumour response according to the Response Evaluation Criteria in Solid Tumours (RECIST) v1.1 criteria], were retrospectively collected from medical records. To be evaluable, all patients must have received at least four cycles of chemotherapy. Patients were classified as follows: complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD). For statistical analysis, the best tumour response was selected. Patients with either CR, PR, or SD were classified as responders and patients with PD as non-responders.
Patients were treated with bevacizumab at a dose of 5 mg/kg on day 1 every two weeks. The FOLFIRI3 regimen was given every 14 d as follows: on day 1, irinotecan 100 mg/m² as a 1-h infusion, running concurrently with leucovorin 200 mg/m2 as a 2-h infusion via a Y-connector, followed by 5-FU 2000 mg/m2 as a 46-h infusion using an electric pump. On day 3, irinotecan 100 mg/m2 as a 1-h infusion was repeated, at the end of the 5-FU infusion. Bevacizumab was given as a 30 min infusion every 2 wk at 5mg/kg. Aflibercept was given as a 1-h infusion every 2 wk at 4 mg/kg.
All patients were followed until death, loss to follow-up, or termination of the study (or whichever occurred first). The objective response rate (ORR) was defined as the proportion of patients having either a CR or PR according to RECIST version 1.1. The disease control rate (DCR) was defined as the percentage of patients who achieved CR, PR or SD. Progression-free survival (PFS) was defined as the time between the treatment start date and the date of disease progression or death from any cause. Patients who were alive without PD at the time of the final analysis were censored. OS was defined as the time between the date and the date of patient death from any cause or to the last date the patient was known to be alive. Patients still alive at the time of the analysis were excluded. Disease characteristics were examined using the χ2 test or Fisher’s exact test for qualitative variables and the Kruskal-Wallis rank sum test for continuous variables, as appropriate. Univariate and multivariate survival analyses were performed using the Cox regression model. Survival probabilities were estimated using the Kaplan-Meier method. OS and PFS medians were calculated with the reverse Kaplan-Meier method and survival curves were compared using the log-rank test. Patients were categorized into one of two cohorts according to their irinotecan status (irinotecan-naïve and those who were previously treated with irinotecan). Patients were also categorized into one of three cohorts according to the treatment regimen they received: FOLFIRI3 alone, FOLFIRI3 plus bevacizumab and FOLFIRI3 plus aflibercept. Data analysis was performed using the statistical software R (http://www.R-project.org/) and representations were made with Prism 7 (GraphPad, San Diego, CA, United States). All tests were two-sided, and P-values < 0.05 were considered statistically significant.
The clinical datasets collected and/or analyzed during the current study are available from the corresponding author on reasonable request.
Between January 2008 and December 2017, a total of 153 patients received at least one injection of the FOLFIRI3 regimen at the Department of Medical Oncology, Georges-Francois Leclerc Cancer Centre, Dijon, France. Eighteen received the FOLFIRI3 regimen, 99 received bevacizumab plus the FOLFIRI3 regimen and 36 received aflibercept plus FOLFIRI3. The main clinical characteristics of patients included in this retrospective study are shown in Table 1. The study included 84 males and 69 females and median age was 64 years (range 33-86). The performance status of this population was good with only 14% of patients having an ECOG performance status of 2. Only 29% of the patients had a right-side tumour. RAS and/or BRAF mutations were observed in 53% of the assessable samples. All patients had previously received at least one line of systemic chemotherapy. Only 28 (18%) of the patients were irinotecan-naïve. 28% of the patients previously received bevacizumab, and 30% were previously treated with an EGFR therapy. Patients receiving either FOLFIRI3, bevacizumab plus FOLFIRI3 or aflibercept plus FOLFIRI3 did not differ in their clinical characteristics (Table 1).
| Characteristic | Folfiri 3 (n = 18) | Bevacizumab folfiri 3 (n = 99) | Aflibercept folfiri 3 (n = 36) | All (n = 153) | Comparison betweentreatments test P-value |
| Median age, yr (range) | 62.5 (44-83) | 64 (38-86) | 66 (33-83) | 64 (33-86) | 0.33 |
| Gender | |||||
| Male | 14 (67) | 50 (51) | 22 (61) | 84 (55) | 0.31 |
| Female | 6 (33) | 49 (49) | 14 (39) | 69 (45) | |
| Who performance status | |||||
| 0 | 2 (11) | 12 (12) | 6 (17) | 20 (13) | 0.47 |
| 1 | 11 (61) | 75 (76) | 25 (69) | 111 (73) | |
| 2 | 5 (28) | 12 (12) | 5 (14) | 22 (14) | |
| Primary location | |||||
| Right colon | 3 (17) | 33 (33) | 8 (22) | 44 (29) | 0.51 |
| Left colon | 9 (50) | 38 (39) | 15 (42) | 62 (41) | |
| Rectum | 6 (33) | 28 (28) | 13 (36) | 47 (30) | |
| Initial cancer status | |||||
| Synchronous | 14 (88) | 26 (26) | 20 (56) | 46 (30) | 0.09 |
| Metachronous | 4 (22) | 73 (74) | 16 (44) | 107 (70) | |
| Number of metastases | |||||
| 0 and 1 | 6 (33) | 29 (29) | 9 (25) | 44 (29) | 0.40 |
| 2 | 8 (40) | 45 (46) | 12 (33) | 65 (42) | |
| 3 and more | 4 (22) | 25 (25) | 15 (42) | 44 (29) | |
| Surgery of primary | |||||
| No | 7 (39) | 38 (38) | 14 (39) | 59 (39) | 1.00 |
| Yes | 11 (61) | 61 (62) | 22 (61) | 94 (61) | |
| Surgery of metastases | |||||
| No | 14 (78) | 78 (79) | 28 (88) | 120 (81) | 0.53 |
| Yes | 4 (22) | 21 (21) | 4 (12) | 29 (19) | |
| Unknown | - | - | 4 | 4 | |
| Line of therapy | |||||
| Second | 5 (28) | 17 (17) | 4 (12) | 26 (17) | 0.52 |
| Third | 3 (17) | 22 (22) | 11 (31) | 36 (24) | |
| More | 10 (55) | 60 (61) | 21 (57) | 91 (59) | |
| Irinotecan chemotherapy-naive | |||||
| No | 13 (72) | 81 (82) | 31 (86) | 125 (82) | 0.46 |
| Yes | 5 (28) | 18 (18) | 5 (14) | 28 (18) | |
| RAS/BRAF mutation status | |||||
| Not mutated | 11 (69) | 36 (44) | 16 (44) | 63 (47) | 0.18 |
| At least one mutated | 5 (31) | 46 (56) | 20 (56) | 71 (53) | |
| Unknown | 2 | 17 | - | 19 | |
| Best overall response | |||||
| PD | 3 (17) | 8 (8) | 0 (0) | 11 (7) | 0.20 |
| SD | 1 (5) | 9 (9) | 7 (19) | 17 (11) | |
| PR | 11 (61) | 48 (48.5) | 15 (42) | 74 (48) | |
| CR | 0 (0) | 3 (3) | 1 (3) | 4 (3) | |
| NE | 3 (17) | 31 (31.5) | 13 (36) | 47 (31) | |
| Median PFS, mo (95%CI) | 3.0 (0.8-6.9) | 3.7 (3.0-5.3) | 4.7 (3.3-12.8) | 3.9 (3.2-4.9) | - |
| Median OS, mo (95%CI) | 5.6 (4.0-20.2) | 8.5 (6.4-10.7) | 13.7 (7.9-18.7) | 9.4 (6.6-12.0) | - |
A total of 1517 cycles of chemotherapy were administered (median 7; range 1–42). One toxic death was reported due to primary tumour perforation followed by haemorrhagic syndrome and septic shock. Bleeding syndrome (digestive or epistaxis) was observed in 12 patients, all treated with antiangiogenic therapies. The most frequent toxicity was a digestive toxicity, grade 3-4 diarrhoea, which occurred in 33 patients (21.6%). Haematological toxicities mainly involved neutropenia. The main toxic events are listed in Table 2. Aflibercept plus the FOLFIRI3 regimen appeared to have increased toxicity compared to the other chemotherapy regimens with both diarrhoea and neutropenia showing increased incidence.
| Characteristic | Folfiri 3 (n = 18) | Bevacizumab folfiri 3 (n = 99) | Aflibercept folfiri 3 (n = 36) | All (n = 153) |
| Anemia | ||||
| No | 14 | 79 | 29 | 122 |
| Grade 1 | 2 | 10 | 5 | 17 |
| Grade 2 | 0 | 8 | 0 | 8 |
| Grade 3 | 2 | 1 | 2 | 5 |
| Grade 4 | 0 | 1 | 0 | 1 |
| Thrombopenia | ||||
| No | 17 | 91 | 31 | 139 |
| Grade 1 | 0 | 5 | 3 | 8 |
| Grade 2 | 0 | 2 | 0 | 2 |
| Grade 3 | 1 | 0 | 0 | 1 |
| Grade 4 | 0 | 1 | 2 | 3 |
| Neutropenia | ||||
| No | 13 | 87 | 26 | 126 |
| Grade 1 | 1 | 0 | 1 | 2 |
| Grade 2 | 2 | 1 | 4 | 7 |
| Grade 3 | 1 | 9 | 4 | 14 |
| Grade 4 | 1 | 2 | 1 | 4 |
| Diarrheoa | ||||
| No | 9 | 48 | 11 | 68 |
| Grade 1 | 2 | 18 | 8 | 28 |
| Grade 2 | 5 | 14 | 5 | 24 |
| Grade 3 | 2 | 14 | 11 | 27 |
| Grade 4 | 0 | 5 | 1 | 6 |
| Stomitis | ||||
| No | 13 | 83 | 27 | 123 |
| Grade 1 | 2 | 5 | 5 | 12 |
| Grade 2 | 2 | 8 | 4 | 14 |
| Grade 3 | 0 | 1 | 0 | 1 |
| Grade 4 | 1 | 2 | 0 | 3 |
| Nausea | ||||
| No | 17 | 81 | 28 | 126 |
| Grade 1 | 1 | 8 | 5 | 14 |
| Grade 2 | 0 | 10 | 3 | 13 |
| Vomiting | ||||
| No | 17 | 90 | 31 | 138 |
| Grade 1 | 0 | 3 | 4 | 7 |
| Grade 2 | 0 | 3 | 1 | 4 |
| Grade 3 | 1 | 3 | 0 | 4 |
| Hyperblood pressure | ||||
| No | 18 | 98 | 36 | 152 |
| Yes | 0 | 1 | 0 | 1 |
| Bleeding | ||||
| No | 17 | 95 | 30 | 142 |
| Yes | 1 | 4 | 6 | 11 |
| Venous thrombosis | ||||
| No | 18 | 97 | 36 | 151 |
| Yes | 0 | 2 | 0 | 2 |
| Digestive perforation | ||||
| No | 18 | 98 | 36 | 152 |
| Yes | 0 | 1 | 0 | 1 |
At the time of analysis, 142 patients (93%) had died with a median follow-up of 9.3 mo (range 0.2–40.7 mo).
Considering all patients included in the study, the ORR and DCR were 51% and 62%, respectively. In the irinotecan-experienced group, the ORR and DCR were 46% (13/28) and 64% (18/28), respectively. We then analysed the data according to the treatment regimen in the FOLFIRI3 alone group, we observed an ORR and DCR of 61% and 66%, respectively. In the bevacizumab plus FOLFIRI3 group, we observed an ORR and DCR of 51.5% and 60.5%, respectively. Finally, in the aflibercept plus FOLFIRI3 group, we observed an ORR and DCR of 45% and 64%, respectively. For the entire study population, median PFS and OS were 3.9 mo (95%CI: 3.2-4.9) and 9.4 mo (95%CI: 6.6-12), respectively. Irinotecan-naïve patients did not show significantly improved PFS or OS with median PFS of 5.2 mo vs 3.7 mo (log-rank test P = 0.15) and median OS of 12 mo vs 9.3 mo (log-rank test P = 0.38). Median PFS and OS were 3.0 mo (95%CI: 0.8-6.9) and 5.6 mo (95%CI: 4.0-20.2), 3.7 mo (95%CI: 3.0-5.3) and 8.5 mo (95%CI: 6.4-10.7), and 4.7 mo (95%CI: 3.3-12.8) and 13.7 mo (95%CI: 7.9-18.7) for FOLFIRI3, FOLFIRI3 plus bevacizumab and FOLFIRI3 plus aflibercept, respectively. Kaplan-Meier curves illustrating PFS and OS in the whole cohort are shown in Figures 1A and B while Figures 1C and D illustrate PFS and OS for the patient subgroups treated with FOLFIRI3, FOLFIRI3 plus bevacizumab and FOLFIRI3 plus aflibercept. The log-rank test shows significantly improved PFS and OS in the FOLFIRI3 plus aflibercept group. Using the Cox univariate model, good performance status, previous surgery of metastases, first through third line therapy and aflibercept usage were associated with better prognosis in terms of PFS. Good performance status and aflibercept usage were also associated with better prognosis in terms of OS (Table 3). Using the Cox multivariate model, only previous surgery of metastasis and aflibercept usage were associated with better prognosis in terms of PFS while good performance status and aflibercept usage were associated with better prognosis in terms of OS (Table 4).
| Characteristic | Progression-free survival | Overall survival | ||||
| Hazard ratio | 95%CI | P-value | Hazard ratio | 95%CI | P-value | |
| Age, yr | ||||||
| Continuous | 0.999 | 0.984; 1.016 | 0.98 | 1.002 | 0.986; 1.018 | 0.81 |
| Gender | ||||||
| Female | 1 | 1 | ||||
| Male | 0.827 | 0.597; 1.145 | 0.25 | 0.898 | 0.645; 1.251 | 0.53 |
| Who performance status | ||||||
| 0 | 1 | 1 | ||||
| 1 | 1.569 | 0.926; 2.660 | 0.09 | 2.039 | 0.143; 3.639 | 0.02 |
| 2 | 2.827 | 0.473; 5.428 | 0.002 | 5.335 | 2.647; 10.75 | < 0.01 |
| Primary location | ||||||
| Right colon | 1 | 1 | ||||
| Left colon | 0.979 | 0.660; 1.454 | 0.92 | 0.945 | 0.634; 1.410 | 0.78 |
| Rectum | 1.018 | 0.671; 1.545 | 0.93 | 1.029 | 0.673; 1.572 | 0.90 |
| Initial cancer status | ||||||
| Synchronous | 1 | 1 | ||||
| Metachronous | 0.815 | 0.572; 1.162 | 0.26 | 0.839 | 0.583; 1.208 | 0.34 |
| No. of metastastatic sites | ||||||
| 1 | 1 | 1 | ||||
| 2 | 1.225 | 0.823; 1.823 | 0.32 | 1.241 | 0.824; 1.870 | 0.30 |
| ≥ 3 | 1.361 | 0.883; 2.098 | 0.16 | 1.490 | 0.954; 2.326 | 0.08 |
| Surgery of primary | ||||||
| No | 1 | 1 | ||||
| Yes | 0.789 | 0.564; 1.104 | 0.17 | 0.799 | 0.568; 1.124 | 0.20 |
| Surgery of metastases | ||||||
| No | 1 | 1 | ||||
| Yes | 0.592 | 0.388; 0.903 | 0.01 | 0.725 | 0.475; 1.107 | 0.13 |
| Line of therapy | ||||||
| Second | 1 | 1 | ||||
| Third | 1.055 | 0.615; 1.812 | 0.85 | 1.126 | 0.646; 1.962 | 0.68 |
| More | 1.728 | 1.060; 2.816 | 0.03 | 1.531 | 0.931; 2.517 | 0.09 |
| Treatment | ||||||
| FOLFIRI | 1 | 1 | ||||
| FOLFIRI3 + Bevacizumab | 1.055 | 0.615; 1.812 | 0.85 | 0.791 | 0.471; 1.329 | 0.38 |
| FOLFIRI3 + Aflibercept | 1.728 | 1.060; 2.816 | 0.03 | 0.470 | 0.255; 0.866 | 0.02 |
| Irinotecan chemotherapy-naive | ||||||
| 1 | 1 | |||||
| No vs yes | 0.731 | 0.474; 1.127 | 0.15 | 0.838 | 0.539; 1.303 | 0.43 |
| RAS/BRAF mutation status | ||||||
| Not mutated | 1 | 1 | ||||
| Mutated | 0.910 | 0.641; 1.293 | 0.60 | 0.986 | 0.690; 1.408 | 0.94 |
| Characteristic | Progression-free survival | Overall survival | ||||
| Hazard ratio | 95%CI | P-value | Hazard ratio | 95%CI | P-value | |
| Age, yr | ||||||
| Continuous | 0.990 | 0.968; 1.012 | 0.36 | 0.988 | 0.968; 1.007 | 0.22 |
| Gender | ||||||
| Female | 1 | 1 | ||||
| Male | 1.003 | 0.673; 1.497 | 0.99 | 0.992 | 0.655; 1.502 | 0.97 |
| Who performance status | ||||||
| 0 | 1 | 1 | ||||
| 1 | 1.588 | 0.832; 3.034 | 0.16 | 2.157 | 1.086; 4.284 | 0.03 |
| 2 | 2.165 | 0.925; 5.068 | 0.08 | 4.865 | 2.061; 11.49 | < 0.001 |
| Primary location | ||||||
| Right colon | 1 | 1 | ||||
| Left colon | 0.953 | 0.589; 1.541 | 0.84 | 0.919 | 0.556; 1.520 | 0.74 |
| Rectum | 1.054 | 0.634; 1.752 | 0.84 | 0.879 | 0.525; 1.470 | 0.62 |
| Initial cancer status | ||||||
| Synchronous | 1 | 1 | ||||
| Metachronous | 0.862 | 0.554; 1.340 | 0.51 | 0.887 | 0.562; 1.398 | 0.60 |
| Number of metastastatic sites | ||||||
| 1 | 1 | 1 | ||||
| 2 | 1.040 | 0.640; 1.692 | 0.87 | 1.085 | 0.654; 1.798 | 0.75 |
| ≥ 3 | 1.347 | 0.796; 2.279 | 0.27 | 1.449 | 0.847; 2.476 | 0.18 |
| Surgery of primary | ||||||
| No | 1 | 1 | ||||
| Yes | 0.947 | 0.622; 1.442 | 0.80 | 0.893 | 0.575; 1.387 | 0.61 |
| Surgery of metastases | ||||||
| No | 1 | 1 | ||||
| Yes | 0.562 | 0.342; 0.924 | 0.02 | 0.754 | 0.458; 1.241 | 0.27 |
| Line of therapy | ||||||
| Second | 1 | 1 | ||||
| Third | 0.878 | 0.421; 1.832 | 0.73 | 0.944 | 0.441; 2.020 | 0.88 |
| More | 1.340 | 0.655; 2.740 | 0.42 | 1.155 | 0.548; 2.432 | 0.71 |
| Treatment | ||||||
| FOLFIRI3 | 1 | 1 | ||||
| FOLFIRI3 + Bevacizumab | 0.547 | 0.304; 0.983 | 0.04 | 0.647 | 0.354; 1.180 | 0.16 |
| FOLFIRI3 + Aflibercept | 0.354 | 0.181; 0.694 | 0.002 | 0.367 | 0.184; 0.729 | 0.004 |
| Irinotecan chemotherapy-naive | ||||||
| No | 1 | 1 | ||||
| Yes | 0.979 | 0.548; 1.748 | 0.94 | 1.114 | 0.609; 2.038 | 0.73 |
| RAS/BRAF mutation status | ||||||
| Not mutated | 1 | 1 | ||||
| Mutated | 1.045 | 0.679; 1.611 | 0.84 | 1.232 | 0.784; 1.935 | 0.37 |
This retrospective study is the largest to date reporting FOLFIRI3 regimen efficacy in mCRC. It is also the first study comparing efficacy and safety of the FOLFIRI3 regimen alone or in combination with bevacizumab or aflibercept. This study demonstrates the safety of these three regimens in heavily pre-treated patients with good performance status. The combination of FOLFIRI3 plus aflibercept gives a higher rate of toxic events as a significant number of the patients in this cohort (33%) presented severe diarrhoea in comparison to 11% and 19% in the FOLFIRI3 or FOLFIRI3 plus bevacizumab cohorts. The frequency of severe diarrhoea was also more prevalent than what has been previously reported in the VELOUR study, where only 19% of patients had grade 3 or higher diarrhoea[8]. A similar level of diarrhoea was observed in the recent retrospective study of Carola, in which 38% of patients experienced severe diarrhoea events[14]. Our group previously reported the association between severe diarrhoea induced by aflibercept and microscopic colitis[15,16]. Aflibercept inhibits placental growth factor (PIGF), which prevents colonic ischaemia and, consequently, induces colitis. In preclinical models, the absence of PIGF promotes dextran sodium sulphate-induced colonic mucosal angiogenesis and increases mucosal hypoxia[17]. Other toxicities such as neutropenia and stomatitis occurred at similar rates across all three chemotherapy regimens[8,18,19]. Few cases of febrile neutropenia were observed probably because 65% of the patients received prophylactic G-CSF treatment. In addition, only 18% of the patients were irinotecan-naïve. Such data may result from selection bias, since only patients who had few prior toxic events while being treated with irinotecan were included and further treated with the FOLFIRI3 regimen.
Irinotecan hinders DNA replication by inhibiting type I topoisomerase. Inhibition of type I topoisomerase induce single strand DNA breaks. After this initial DNA damage, failure to repair the DNA breaks results in increased apoptosis. Preclinical studies show that the anti-proliferative activity of 5-FU in combination with irinotecan is schedule dependent[20-22]. For example, several studies showed that delayed administration of irinotecan increases FOLFIRI cytotoxicity. Likewise, the FOLFIRI2 regimen (irinotecan delivery post 5-FU injection) induced promising objective responses but suffered from major haematological toxicity[23]. In contrast, FOLFIRI3 has an improved toxicity profile and previous studies showed that this regimen is active in mCRC resistant to FOLFIRI. Furthermore, in the absence of a targeted agent, response rates range from 17 to 23%, with median PFS of 4-7 mo and median OS of 9-12 mo[11,12,24].
In a similar setting, our group previously reported that FOLFIRI3 plus bevacizumab resulted in a 53% response rate and median PFS and OS of 7 and 13 mo, respectively. Importantly, these results did not differ from the FOLFIRI3 results without a targeted therapy[13]. A recent retrospective report on the usage of FOLFIRI3 in combination with aflibercept demonstrated a response rate of 35%[14]. Results were improved in irinotecan-naïve patients in comparison to the irinotecan-experienced cohort with median PFS and OS of 11.3 mo and 17.0 mo, respectively, for the irinotecan-naïve group and 5.7 mo and 14.3 mo for the irinotecan-experienced group. Our study mainly involved patients that were previously treated with irinotecan and, in the FOLFIRI3 plus aflibercept cohort, only 5 of the 36 patients were irinotecan-naïve. In this cohort, median PFS and OS were 4.7 mo and 13.7 mo, respectively. This study supports the hypothesis that aflibercept increases the efficacy of the FOLFIRI3 regimen. The main limitation of this study is the retrospective design with a relatively low number of patients per cohort.
The FOLFIRI3 regimen demonstrates efficacy and safety in patients previously treated with irinotecan and is an alternative strategy for multi-treated patients. The combination of aflibercept and FOLFIRI3 appears more efficacious than FOLFIRI3 alone or in combination with bevacizumab. A randomized trial comparing FOLFIRI3 plus bevacizumab vs FOLFIRI3 plus aflibercept should be conducted to validate this hypothesis.
FOLFIRI3 is a modification of the classical FOLFIRI regimen with injection of irinotecan at day 1 and 3. This treatment is used as second or further line in many French Centre’s based of previous retrospective data. This chemotherapeutic regimen could be used alone or in combination with antiangiogenic agent but comparison of efficacy of FOLFIRI3, FOLFIRI3 bevacizumab and FOLFIRI3 aflibercept has never been performed.
Our objective was to compared efficacy and toxicity of FOLFIRI3, FOLFIRI3 bevacizumab and FOLFIRI3 aflibercept regimen.
The main objective of the study is to evaluate the safety and efficacy of the FOLFIRI3-used alone or in combination with bevaicuzmab or aflibercept.
This is a monocentric retrospective study evaluating the efficacy and safety of the FOLFIRI3 regimen given alone or in combination with bevacizumab or aflibercept in patients with previously treated metastatic colorectal cancer (mCRC).
One hundred and fifty-three consecutive patients were included (18 treated with FOLFIRI3, 99 with FOLFIRI3 plus bevacizumab and 36 with FOLFIRI3 plus aflibercept). Median progression-free survival (PFS) and overall survival (OS) were 3.9 mo (95%CI: 3.2-4.9) and 9.4 mo (95%CI: 6.6-12), respectively. Median PFS and OS values were improved in the FOLFIRI3 plus aflibercept group. Grade 3-4 adverse events (diarrhoea and neutropenia) were more frequent in the FOLFIRI3 plus aflibercept group.
The modification of FOLFIRI regimen had an impacton mCRC patients’ treatment response. The addition of an antiangiogenic agent, in particular aflibercept, enhanced the clinical benefit and improved survival.
Prospective randomized trial comparing FOLFIRI-aflibercept to FOLFIRI3-aflibercept are warranted.
| 1. | Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20108] [Cited by in RCA: 20722] [Article Influence: 1883.8] [Reference Citation Analysis (23)] |
| 2. | Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, Aranda Aguilar E, Bardelli A, Benson A, Bodoky G, Ciardiello F, D'Hoore A, Diaz-Rubio E, Douillard JY, Ducreux M, Falcone A, Grothey A, Gruenberger T, Haustermans K, Heinemann V, Hoff P, Köhne CH, Labianca R, Laurent-Puig P, Ma B, Maughan T, Muro K, Normanno N, Österlund P, Oyen WJ, Papamichael D, Pentheroudakis G, Pfeiffer P, Price TJ, Punt C, Ricke J, Roth A, Salazar R, Scheithauer W, Schmoll HJ, Tabernero J, Taïeb J, Tejpar S, Wasan H, Yoshino T, Zaanan A, Arnold D. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27:1386-1422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2286] [Cited by in RCA: 2540] [Article Influence: 254.0] [Reference Citation Analysis (41)] |
| 3. | Grothey A, Van Cutsem E, Sobrero A, Siena S, Falcone A, Ychou M, Humblet Y, Bouché O, Mineur L, Barone C, Adenis A, Tabernero J, Yoshino T, Lenz HJ, Goldberg RM, Sargent DJ, Cihon F, Cupit L, Wagner A, Laurent D; CORRECT Study Group. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:303-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2194] [Cited by in RCA: 2213] [Article Influence: 170.2] [Reference Citation Analysis (0)] |
| 4. | Mayer RJ, Van Cutsem E, Falcone A, Yoshino T, Garcia-Carbonero R, Mizunuma N, Yamazaki K, Shimada Y, Tabernero J, Komatsu Y, Sobrero A, Boucher E, Peeters M, Tran B, Lenz HJ, Zaniboni A, Hochster H, Cleary JM, Prenen H, Benedetti F, Mizuguchi H, Makris L, Ito M, Ohtsu A; RECOURSE Study Group. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med. 2015;372:1909-1919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 1064] [Article Influence: 96.7] [Reference Citation Analysis (0)] |
| 5. | Tournigand C, André T, Achille E, Lledo G, Flesh M, Mery-Mignard D, Quinaux E, Couteau C, Buyse M, Ganem G, Landi B, Colin P, Louvet C, de Gramont A. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol. 2004;22:229-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2282] [Cited by in RCA: 2214] [Article Influence: 100.6] [Reference Citation Analysis (1)] |
| 6. | Giantonio BJ, Catalano PJ, Meropol NJ, O'Dwyer PJ, Mitchell EP, Alberts SR, Schwartz MA, Benson AB, Eastern Cooperative Oncology Group Study E3200. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007;25:1539-1544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1806] [Cited by in RCA: 1738] [Article Influence: 91.5] [Reference Citation Analysis (2)] |
| 7. | Bennouna J, Sastre J, Arnold D, Österlund P, Greil R, Van Cutsem E, von Moos R, Viéitez JM, Bouché O, Borg C, Steffens CC, Alonso-Orduña V, Schlichting C, Reyes-Rivera I, Bendahmane B, André T, Kubicka S; ML18147 Study Investigators. Continuation of bevacizumab after first progression in metastatic colorectal cancer (ML18147): a randomised phase 3 trial. Lancet Oncol. 2013;14:29-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 760] [Cited by in RCA: 919] [Article Influence: 65.6] [Reference Citation Analysis (0)] |
| 8. | Van Cutsem E, Tabernero J, Lakomy R, Prenen H, Prausová J, Macarulla T, Ruff P, van Hazel GA, Moiseyenko V, Ferry D, McKendrick J, Polikoff J, Tellier A, Castan R, Allegra C. Addition of aflibercept to fluorouracil, leucovorin, and irinotecan improves survival in a phase III randomized trial in patients with metastatic colorectal cancer previously treated with an oxaliplatin-based regimen. J Clin Oncol. 2012;30:3499-3506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 933] [Cited by in RCA: 1055] [Article Influence: 75.4] [Reference Citation Analysis (0)] |
| 9. | Tabernero J, Yoshino T, Cohn AL, Obermannova R, Bodoky G, Garcia-Carbonero R, Ciuleanu TE, Portnoy DC, Van Cutsem E, Grothey A, Prausová J, Garcia-Alfonso P, Yamazaki K, Clingan PR, Lonardi S, Kim TW, Simms L, Chang SC, Nasroulah F; RAISE Study Investigators. Ramucirumab versus placebo in combination with second-line FOLFIRI in patients with metastatic colorectal carcinoma that progressed during or after first-line therapy with bevacizumab, oxaliplatin, and a fluoropyrimidine (RAISE): a randomised, double-blind, multicentre, phase 3 study. Lancet Oncol. 2015;16:499-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 649] [Cited by in RCA: 689] [Article Influence: 62.6] [Reference Citation Analysis (0)] |
| 10. | Peeters M, Price TJ, Cervantes A, Sobrero AF, Ducreux M, Hotko Y, André T, Chan E, Lordick F, Punt CJ, Strickland AH, Wilson G, Ciuleanu TE, Roman L, Van Cutsem E, Tzekova V, Collins S, Oliner KS, Rong A, Gansert J. Randomized phase III study of panitumumab with fluorouracil, leucovorin, and irinotecan (FOLFIRI) compared with FOLFIRI alone as second-line treatment in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28:4706-4713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 709] [Cited by in RCA: 763] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 11. | Mabro M, Artru P, André T, Flesch M, Maindrault-Goebel F, Landi B, Lledo G, Plantade A, Louvet C, de Gramont A. A phase II study of FOLFIRI-3 (double infusion of irinotecan combined with LV5FU) after FOLFOX in advanced colorectal cancer patients. Br J Cancer. 2006;94:1287-1292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Chibaudel B, Maindrault-Gœbel F, Bachet JB, Louvet C, Khalil A, Dupuis O, Hammel P, Garcia ML, Bennamoun M, Brusquant D, Tournigand C, André T, Arbaud C, Larsen AK, Wang YW, Yeh CG, Bonnetain F, de Gramont A. PEPCOL: a GERCOR randomized phase II study of nanoliposomal irinotecan PEP02 (MM-398) or irinotecan with leucovorin/5-fluorouracil as second-line therapy in metastatic colorectal cancer. Cancer Med. 2016;5:676-683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 13. | Ghiringhelli F, Vincent J, Guiu B, Chauffert B, Ladoire S. Bevacizumab plus FOLFIRI-3 in chemotherapy-refractory patients with metastatic colorectal cancer in the era of biotherapies. Invest New Drugs. 2012;30:758-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Carola C, Ghiringhelli F, Kim S, André T, Barlet J, Bengrine-Lefevre L, Marijon H, Garcia-Larnicol ML, Borg C, Dainese L, Steuer N, Richa H, Benetkiewicz M, Larsen AK, de Gramont A, Chibaudel B. FOLFIRI3-aflibercept in previously treated patients with metastatic colorectal cancer. World J Clin Oncol. 2018;9:110-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Ghiringhelli F, Vincent J, Beltjens F, Bengrine L, Ladoire S. Fluorouracil, leucovorin and irinotecan associated with aflibercept can induce microscopic colitis in metastatic colorectal cancer patients. Invest New Drugs. 2015;33:1263-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Miehlke S, Madisch A, Kupcinskas L, Petrauskas D, Böhm G, Marks HJ, Neumeyer M, Nathan T, Fernández-Bañares F, Greinwald R, Mohrbacher R, Vieth M, Bonderup OK; BUC-60/COC Study Group. Budesonide is more effective than mesalamine or placebo in short-term treatment of collagenous colitis. Gastroenterology. 2014;146:1222-30.e1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 17. | Hindryckx P, Waeytens A, Laukens D, Peeters H, Van Huysse J, Ferdinande L, Carmeliet P, De Vos M. Absence of placental growth factor blocks dextran sodium sulfate-induced colonic mucosal angiogenesis, increases mucosal hypoxia and aggravates acute colonic injury. Lab Invest. 2010;90:566-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Venook AP, Niedzwiecki D, Lenz HJ, Innocenti F, Fruth B, Meyerhardt JA, Schrag D, Greene C, O'Neil BH, Atkins JN, Berry S, Polite BN, O'Reilly EM, Goldberg RM, Hochster HS, Schilsky RL, Bertagnolli MM, El-Khoueiry AB, Watson P, Benson AB, Mulkerin DL, Mayer RJ, Blanke C. Effect of First-Line Chemotherapy Combined With Cetuximab or Bevacizumab on Overall Survival in Patients With KRAS Wild-Type Advanced or Metastatic Colorectal Cancer: A Randomized Clinical Trial. JAMA. 2017;317:2392-2401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 507] [Cited by in RCA: 723] [Article Influence: 80.3] [Reference Citation Analysis (0)] |
| 19. | Cremolini C, Loupakis F, Antoniotti C, Lupi C, Sensi E, Lonardi S, Mezi S, Tomasello G, Ronzoni M, Zaniboni A, Tonini G, Carlomagno C, Allegrini G, Chiara S, D'Amico M, Granetto C, Cazzaniga M, Boni L, Fontanini G, Falcone A. FOLFOXIRI plus bevacizumab versus FOLFIRI plus bevacizumab as first-line treatment of patients with metastatic colorectal cancer: updated overall survival and molecular subgroup analyses of the open-label, phase 3 TRIBE study. Lancet Oncol. 2015;16:1306-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 613] [Cited by in RCA: 838] [Article Influence: 76.2] [Reference Citation Analysis (0)] |
| 20. | Banerjee D, Gorlick R, Liefshitz A, Danenberg K, Danenberg PC, Danenberg PV, Klimstra D, Jhanwar S, Cordon-Cardo C, Fong Y, Kemeny N, Bertino JR. Levels of E2F-1 expression are higher in lung metastasis of colon cancer as compared with hepatic metastasis and correlate with levels of thymidylate synthase. Cancer Res. 2000;60:2365-2367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Guichard S, Cussac D, Hennebelle I, Bugat R, Canal P. Sequence-dependent activity of the irinotecan-5FU combination in human colon-cancer model HT-29 in vitro and in vivo. Int J Cancer. 1997;73:729-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Mans DR, Grivicich I, Peters GJ, Schwartsmann G. Sequence-dependent growth inhibition and DNA damage formation by the irinotecan-5-fluorouracil combination in human colon carcinoma cell lines. Eur J Cancer. 1999;35:1851-1861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 78] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 23. | Mabro M, Louvet C, André T, Carola E, Gilles-Amar V, Artru P, Krulik M, de Gramont A; GERCOR. Bimonthly leucovorin, infusion 5-fluorouracil, hydroxyurea, and irinotecan (FOLFIRI-2) for pretreated metastatic colorectal cancer. Am J Clin Oncol. 2003;26:254-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Bidard FC, Tournigand C, André T, Mabro M, Figer A, Cervantes A, Lledo G, Bengrine-Lefevre L, Maindrault-Goebel F, Louvet C, de Gramont A. Efficacy of FOLFIRI-3 (irinotecan D1,D3 combined with LV5-FU) or other irinotecan-based regimens in oxaliplatin-pretreated metastatic colorectal cancer in the GERCOR OPTIMOX1 study. Ann Oncol. 2009;20:1042-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country of origin: France
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Barreto SG, Kanat O, Tomizawa M S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ