Published online Oct 24, 2019. doi: 10.5306/wjco.v10.i10.340
Peer-review started: May 14, 2019
First decision: August 16, 2019
Revised: August 22, 2019
Accepted: September 20, 2019
Article in press: September 20, 2019
Published online: October 24, 2019
Processing time: 167 Days and 16.8 Hours
Black women are known to have a higher risk of aggressive endometrial cancers. Little data exist about the role of nativity as a determinant of survival outcomes in women with this disease.
Our objective was to evaluate a population of Haitian immigrants with endometrial cancer in an urban setting using the Florida Cancer Data System (FCDS).
A search of FCDS identified 107 women born in Haiti and who received treatment for invasive endometrial cancer in Miami-Dade County between 1989 and 2013. Clinicopathologic data were extracted to describe the cohort and assess associations with overall survival. Statistical analyses were performed using Cox proportional hazards models, the log-rank test, and the Kaplan-Meier method, with significance set at P ≤ 0.05.
Median age at diagnosis was 65 years. 63.9% of the patients had a type II, high-grade, histology, and 52.6% presented with extrauterine metastatic disease. Nearly three quarters had health insurance. Within the entire cohort, only presence of extrauterine disease was associated with worse overall survival [Hazard ratio (HR) = 2.70, 95% confidence interval (CI): 1.31-5.57, P = 0.007]. However, after stratification by histologic grade, both age (HR = 0.88, 95%CI: 0.81-0.96, P = 0.002) and extrauterine disease (HR = 2.49, 95%CI: 1.01-6.21, P = 0.049) were independently associated with worse survival, but only in women with type II malignancies.
Urban Haitian women with endometrial cancer have a high burden of aggressive histologies. Additional investigation to explain the etiology of these findings is needed.
Core tip: Black women of Haitian nativity have a higher prevalence of type II endometrial cancers than previously reported in other large, population-based studies performed in the United States. Further investigation into the genetic, epigenetic, and behavioral determinations of this observed health outcome is necessary.
- Citation: Schlumbrecht M, Bussies P, Huang M, Kobetz E, George S. Endometrial cancer among a cohort of urban Haitian immigrants. World J Clin Oncol 2019; 10(10): 340-349
- URL: https://www.wjgnet.com/2218-4333/full/v10/i10/340.htm
- DOI: https://dx.doi.org/10.5306/wjco.v10.i10.340
Endometrial cancer is the most common gynecologic malignancy in the United States, with nearly 62000 cases diagnosed annually[1]. Cancers of the endometrium are categorized as either low-grade or high-grade depending on specific pathologic features[2]. Low-grade, or type I tumors, have glandular endometrioid histologies, and usually arise in the setting of hyperestrogenism. In contrast, high-grade, or type II tumors, develop in the setting of aggressive driver mutations, metastasize early, and are relatively refractory to treatment. It has been well described that minority women, especially black women, have a higher risk for these aggressive tumors, with worse outcomes, as compared to white women[3,4]. In fact, the proportion of type II histologies among black women is nearly twice that of white women, with significant disparities in subsequent cancer deaths[5,6]. The full etiology of these findings has yet to be elucidated. Recent data have suggested, however, that among black women with type II endometrial cancer, nativity plays a role in determining endometrial cancer outcomes, and that women born in the Caribbean, despite limitations in access to care, have favorable survival in comparison to United States-born black women[7].
The black population in the United States is quite diverse. One in ten is foreign born, and of the non-Hispanic blacks in the United States, over 50% are Caribbean nationals[8,9]. The largest contributor to Caribbean black immigrations is Haiti. Between 1980 and 2015, the population of Haitian immigrants in the United States increased more than 7-fold to 676000, with the largest communities settling in Miami-Dade and Broward counties in South Florida and Kings county in New York[10,11]. While Haitian immigrants account for < 2% of the entire United States foreign-born population[11], they represent a large group with unique health habits and approaches to medical care[12,13]. As we continue to develop robust personalized cancer programs, understanding disease processes within unique subpopulations of patients is crucial. Our objective was to evaluate patterns of endometrial cancer among Haitian immigrants in Miami-Dade County, and determine factors that affect survival outcomes in these women.
Data on endometrial cancer were obtained from Florida Cancer Data System (FCDS), the state cancer registry. All reportable malignant cancer cases in the state of Florida must be reported to FCDS by legislative mandate. FCDS is nationally certified by the North American Association of Cancer Registries, has been collecting data since 1981, and includes reporting from 230 hospitals within the state.
This study was completed under a larger, state-approved institutional review board protocol for abstraction of FCDS data. The FCDS database was searched for a cohort of women diagnosed with endometrial cancer (ICD-0 C54.1), with data further restricted by county (Miami-Dade = 86) and country of birth (Haiti = 242). Data were extracted from 1989-2013 and represented the most up-to-date entries from FCDS. Of the more than 26000 women with endometrial cancer in the FCDS, data on the women who met the specific inclusion criteria were provided to the investigators. All women were ≥ 18 years of age. Extracted variables included age at diagnosis, tumor histology, date of diagnosis, date of death or last follow-up, vital status, tobacco use, receipt of chemotherapy, radiation, or surgery, positivity of lymph nodes and number of positive lymph nodes, presence of extrauterine metastasis, and type of insurance. Presence of extrauterine metastasis acted as a surrogate for low-stage vs high-stage disease, as tumor outside of the uterus is what characterized stage III and IV disease by the International Federation of Obstetrics and Gynecology systems. Histologic codes were used to classify patients into low-grade (low + moderate differentiation) and high-grade (poorly differentiated + anaplastic). Histologic subtypes were cross-referenced with the grading codes to ensure appropriate designation as high-grade/low-grade subtypes. Age and number of positive lymph nodes were evaluated as continuous variables, while all others were coded as binary (yes/no) for analyses. Overall survival was defined as time from date of diagnosis to death (all-cause).
Statistical analyses were performed using STATA IC 14.2 (StataCorp, College Station, TX, United States). To avoid bias, all patients were included in the analyses, even when missing specific data points, and all available data were included. Summary statistics were used to describe the patient cohort. Univariable and multivariable Cox proportional hazards regression, the log-rank test, and the Kaplan-Meier method were utilized to assess survival outcomes, with 95% confidence interval (CI) generated. To avoid inadvertently eliminating potential confounding factors affecting survival, stepwise backwards multivariable regression analyses included covariates with P values ≤ 0.10 from the univariable models. All tests were two-sided, with significance set at P < 0.05.
Over the study interval, 107 patients were identified who met inclusion criteria. Patient demographics are shown in Table 1. The median age was 65 years, and more than half of the patients had private insurance coverage. The majority of women were never smokers. Nearly two-thirds (63.9%) of the patients had high-grade disease, and 21.1% had positive lymph nodes at diagnosis. The number of positive lymph nodes ranged from 1-15 in these women, with a median of four. Surgery was included as a component of the treatment plan in 81.3% of patients, with similar proportions receiving chemotherapy (30.8%) and radiation (30.8%). More than half of the patients had extrauterine disease at the time of diagnosis. At the end of the study period, 41 patients had active disease, and 41 patients had died.
| Variable | n = 107 (%) |
| Age at diagnosis | |
| Median (range) | 65 (39-90) |
| Insurance | |
| None | 24 (26.1) |
| Government | 17 (18.5) |
| Private | 51 (55.4) |
| Tobacco use | |
| Current/Former | 15 (14) |
| Never | 92 (86) |
| Histologic grade | |
| Low-grade | 35 (36.1) |
| High-grade | 62 (63.9) |
| Surgery performed | |
| Yes | 87 (81.3) |
| No | 20 (18.7) |
| Chemotherapy | |
| Yes | 33 (30.8) |
| No/Unknown | 74 (69.2) |
| Radiation | |
| Yes | 33 (30.8) |
| No/Unknown | 74 (69.2) |
| Positive lymph nodes | |
| Yes | 12 (21.1) |
| No/Unknown | 45 (78.9) |
| Number of positive lymph nodes | |
| Median (range) | 4 (1-15) |
| Extrauterine disease | |
| Yes | 50 (52.6) |
| No | 45 (47.4) |
Table 2 shows the proportional hazards models for overall survival in the cohort. In the univariable model, both chemotherapy [Hazard ratio (HR) = 1.98, 95%CI: 1.00-3.92, P = 0.05] and extrauterine disease (HR = 2.81, 95%CI: 1.38-5.74, P = 0.005) were negatively associated with overall survival, while histologic grade (HR = 1.89, 95%CI: 0.93-3.83, P = 0.08) trended towards a negative effect. In the multivariate model, only extrauterine disease (HR = 2.70, 95%CI: 1.31-5.57, P = 0.007) remained independently predictive of worse survival. Age, surgery, radiation, tobacco use, and type of health insurance had no associations with overall survival.
| Variable | Univariable | Multivariable |
| HR (95%CI), P value | HR (95%CI), P value | |
| Age at diagnosis (continuous) | 0.97 (0.92-1.01), 0.16 | |
| Histologic grade | ||
| Low | -- | -- |
| High | 1.89 (0.93-3.83), 0.08 | 1.41 (0.68-2.96), 0.36 |
| Surgery | ||
| No | -- | |
| Yes | 0.56 (0.23-1.34), 0.20 | |
| Chemotherapy | ||
| No | -- | -- |
| Yes | 1.98 (1.00-3.92), 0.05 | 1.50 (0.72-3.12), 0.28 |
| Radiation | ||
| No | -- | |
| Yes | 0.63 (0.32-1.23), 0.18 | |
| Tobacco use | ||
| Never | -- | |
| Ever | 1.10 (0.46-2.63), 0.84 | |
| Site of disease | ||
| Uterine confined | -- | -- |
| Extrauterine | 2.81 (1.38-5.74), 0.005 | 2.70 (1.31-5.57), 0.007 |
| Insurance status | ||
| Uninsured | -- | |
| Government insurance | 0.88 (0.58-1.33), 0.55 | |
| Private insurance | 1.14 (0.43-3.02), 0.80 |
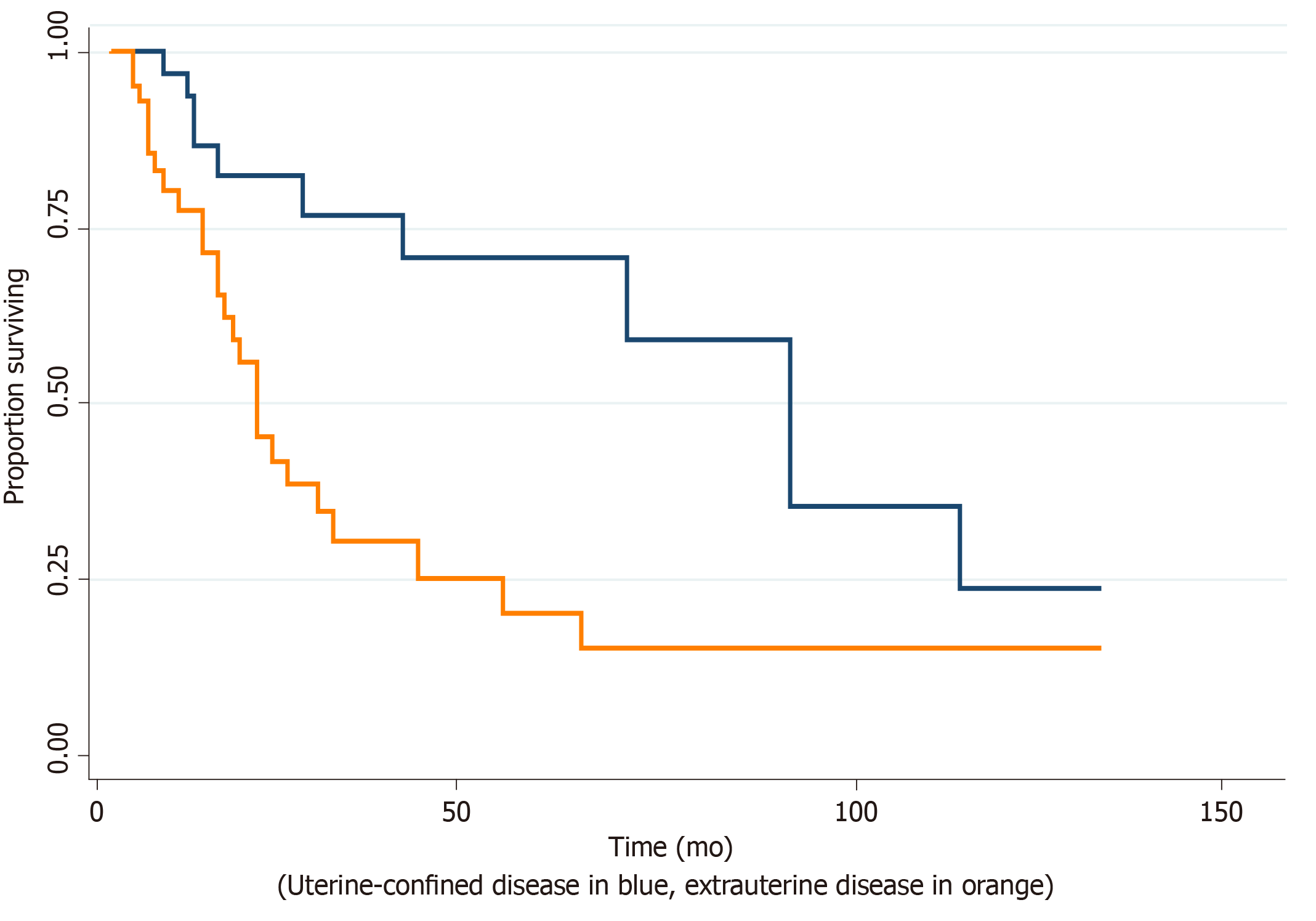
Because of the previously well-described negative associations between grade and survival outcomes in endometrial cancer, additional survival analyses were performed with stratification by grade (Table 3). Among type I histologies, there were no individual variables which were predictive of outcome, though extrauterine disease trended towards a negative association (HR = 2.96, 95%CI: 0.86-10.19, P = 0.08). Among women with type II histologies, older age (HR = 0.89, 95%CI: 0.83-0.95, P = 0.001) and extrauterine disease (HR = 2.75, 95%CI: 1.12-6.78, P = 0.03) were predictive of overall survival in the univariable analyses. These relationships were maintained in the multivariable model, with both age (HR = 0.88, 95%CI: 0.81-0.96, P = 0.002) and extrauterine disease (HR = 2.49, 95%CI: 1.01-6.21, P = 0.049) remaining predictive of changes in survival outcomes. The median overall survival for patients with type I histologies was 110 mo vs 23 mo with type II histology (log-rank P = 0.07).
| Variable | Type I | Type II | ||
| Univariable | Multivariable | Univariable | Multivariable | |
| Age at diagnosis (continuous) | 1.04 (0.94-1.14), P = 0.47 | -- | 0.89 (0.83-0.95), P = 0.001 | 0.88 (0.81-0.96), P = 0.002 |
| Surgery | ||||
| No | -- | -- | -- | -- |
| Yes | Not calculated | 0.70 (0.26-1.86), P = 0.47 | ||
| Chemotherapy | ||||
| No | -- | -- | -- | -- |
| Yes | 1.26 (0.27-5.98), P = 0.77 | 1.99 (0.84-4.71), P = 0.12 | ||
| Radiation | ||||
| No | -- | -- | -- | -- |
| Yes | 0.33 (0.07-1.56), P = 0.17 | 0.52 (0.23-1.17), P = 0.12 | ||
| Tobacco use | ||||
| Never | -- | -- | -- | -- |
| Ever | 1.97 (0.24-16.03), P = 0.52 | 0.69 (0.26-1.84), P = 0.46 | ||
| Site of disease | ||||
| Uterine confined | -- | -- | -- | -- |
| Extrauterine | 2.96 (0.86-10.19), P = 0.08 | 2.75 (1.12-6.78), P = 0.03 | 2.49 (1.01-6.21), P = 0.049 | |
| Insurance status | ||||
| Uninsured | -- | -- | -- | -- |
| Government insurance | 1.22 (0.41-3.69), P = 0.72 | 0.86 (0.54-1.37), P = 0.53 | ||
| Private insurance | 3.69 (0.41-33.34), P = 0.25 | 0.74 (0.21-2.61), P = 0.64 | ||
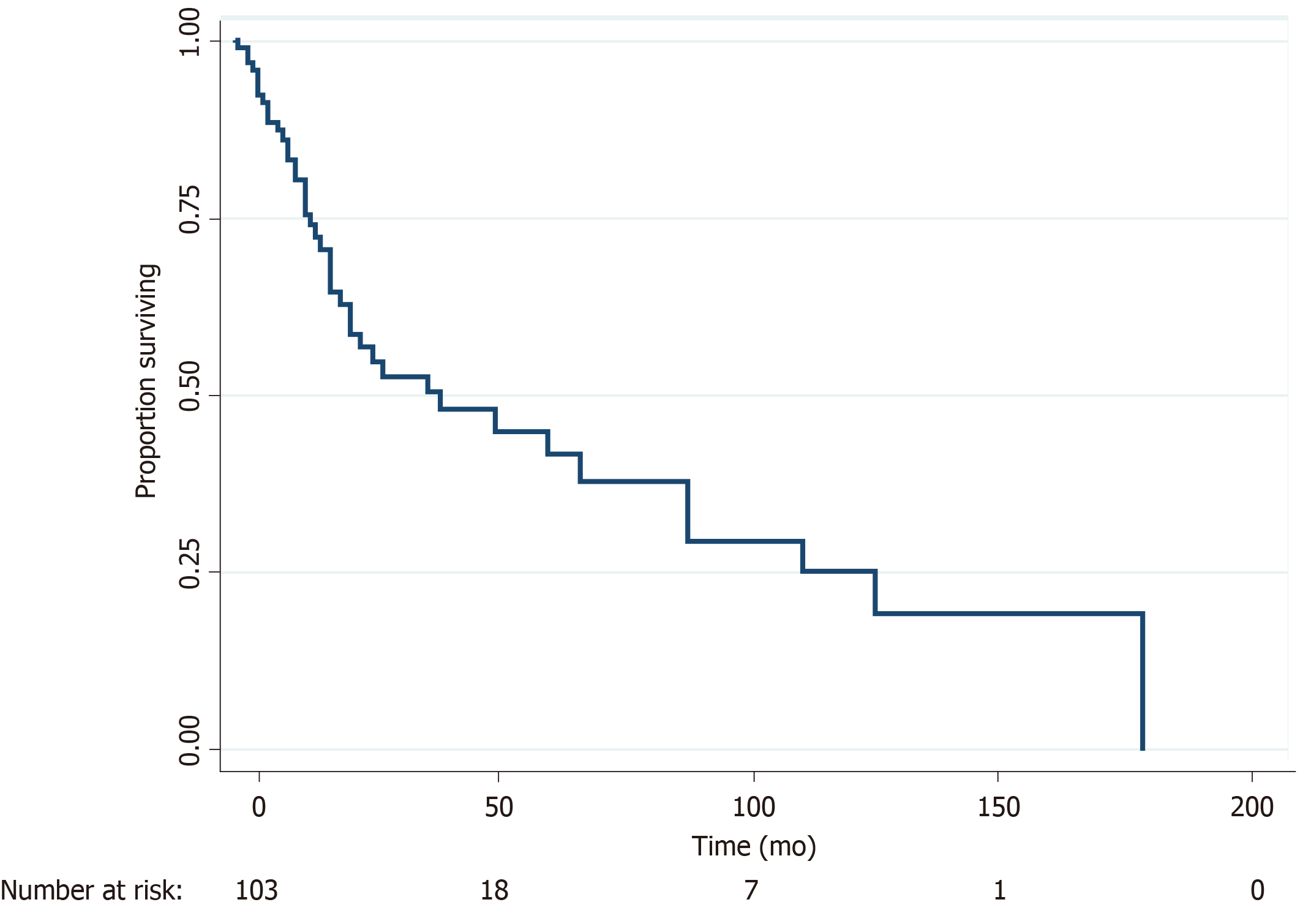
Graphic depiction of survival in the cohort is shown in Figure 1. The median overall survival for the cohort was 38.8 mo (range 0-176 mo), with a 5-year overall survival of 41.2%. When further evaluated by presence of risk factors associated with disease progression and dissemination, significant differences in overall survival were seen. Among women with positive pathologic lymph nodes, median survival was 16 mo vs 67 mo in those with negative lymph nodes (log-rank P = 0.022) (Figure 2). Even more profound differences were seen in overall survival when patients were classified by the presence of any extrauterine disease. Women with disease confined to the uterus had a median survival of 88 mo. In contrast, among those with tumor which had spread outside of the uterus, median survival was only 19 mo (log-rank P = 0.003) (Figure 3).
The rate of endometrial cancer is increasing globally. While much of this is related to the growing epidemic of obesity, it is important to recognize the diversity of this disease and other factors that may be influencing disease propagation and development. The incidence rate of endometrial cancer is growing faster among non-Hispanic black women than other racial groups[6]. Understanding the role of nativity and shared experience beyond just race is understudied, but likely relevant. Here we present the first data on endometrial cancer in women of Haitian descent.
Several important points are appreciated from our data, the most important of which is the large proportion of women with type II endometrial cancers. In other population-based studies completed within the United States, the proportion of black women with type II histologies is reported to be between 29% and 43%, a stark contrast to the 63.9% of Haitian women in our cohort with high-grade histologies[5,6,14]. While there are limitations in cross-study comparisons, it should be noted that these data were evaluated using the Surveillance, Epidemiology, and End Results Program, which does not include states with significant Afro-Caribbean representations[5,6], or from Health Care Financing Administration data files with representation from the western United States[14]. Other studies which have evaluated populations inclusive of more women with either African or Afro-Caribbean roots have demonstrated similar findings to ours. For example, Creque et al[15] evaluated a cohort of women in Brooklyn, nearly two-thirds of which had Afro-Caribbean ancestry, and found that 59.3% of women had high-grade cancers. In a single-institution study completed in Miami, the proportion of women with endometrial cancer of Afro-Caribbean nativity with a type II endometrial histology was 72.2%[7]. It is clear that women from the Caribbean, including the population of Haitian immigrants in our current study, demonstrate a higher proportion of type II endometrial cancer than black women elsewhere in the United States. Additional study into the etiology of disease in these women and mediators of disease development is required.
More than 52% of the women presented with extrauterine disease in this cohort. This proportion is greater than the 42.9% reported among non-Hispanic black women in other large series[6]. Stage at presentation is a complex issue, but should be evaluated through a number of lenses, one of which is genetic determinants of aggressive disease. Based on data from The Cancer Genome Atlas, the most frequently mutated gene among black women is TP53. TP53 is a tumor suppressor gene present in the majority of type II endometrial cancer histologies. In the tumors of black women with a TP53 mutation, it has been reported that there are more than double the number of somatic copy number variations associated with tumor aggressiveness as compared with white women[16,17]. Additionally, tumors from black women more frequently demonstrate amplifications of chr1q, a region that codes for a family of S100A proteins[16]. These proteins are associated with higher recurrence rates in breast cancer, as well as activation of the epithelial-to-mesenchymal transition, a driver of metastasis, in endometrial malignancies[16,18]. At present, there have been no studies to evaluate tumor-level genomics in Haitian women, so the roles of these genes are unknown. Whole exome sequencing may be of use to identify molecular drivers of disease and metastasis, and potentially assist in optimization of oncologic treatment planning.
When examining disparities in care between immigrants and United States-nationals, a number of sociodemographic factors are typically evaluated as mediators of outcome. Access to care, and specifically insurance acquisition, is a frequent limitation in immigrant populations, and may explain delays in disease diagnosis and stage shifts for foreign-nationals. Inability to find enrollment offices, language barriers confounding communication with enrollers, and perceived discrimination against immigrants have all been identified as barriers to insurance enrollment[19-21]. These obstacles prevent access to primary care and cancer screenings, with subsequent negative downstream effects[22,23]. Interestingly, in our population of women, nearly 74% of women had coverage either through private insurance (55.4%) or federal/state programs (18.5%). These findings reflect Miami-Dade County census bureau data, which reported that among the Haitian immigrant population, approximately 79% have insurance coverage[11]. While Haitian immigrants are three times more likely to be uninsured than persons born in the United States, they have higher rates of public/government insurance coverage than other immigrants in the county[11]. In evaluating this population to understand why women present at late stages, it is thus insufficient to attribute stage shifts to socioeconomic factors alone, and that tumor biology and genetics warrant equal attention.
Our study has several limitations. As the data were acquired from a large tumor registry, it is subject to the inherent biases associated with such databases. Data entry error, inconsistency in reporting, and heterogeneity in reporting sites are all potential confounders. The sample size was very low, and over the long duration inclusive of our study, it is highly likely that the numbers of Haitian women with endometrial cancer are underreported. This may be due in part to a hesitation of Haitian patients to declare their immigrant status and place of birth. It has been well-documented that legal status and preoccupations about both disclosure and deportation are of significant concern for immigrants[24]. As such, the small cohort limited statistical analyses; larger populations may provide better and more accurate associations between clinicodemographic variables and outcome. Even so, this is the first report of endometrial cancer in Haitian women. It generates a number of additional questions regarding etiology of disease, cancer risk, and modifiers of outcome, which should be further explored. Additionally, since Miami-Dade County has the highest number of Haitian immigrants nationally in an urban setting, these data may be applicable to other centers where Haitian immigrant women may be residing.
As more is learned about endometrial cancer in minority patients, it is becoming clearer that evaluation of racial subpopulations, especially among black women, will be increasingly important. Understanding variations in genetic determinants of disease, epigenetic modifications present from environmental exposure or life habits, and the social context of the disease is needed. Nativity as a mediator of both risk and outcome should also be explored. Among Haitian women with endometrial cancer, there is a clear departure from the typical patterns seen among United States-blacks in terms of histologic distribution and stage at presentation. Clinicians should be aware of this risk, particularly when the Haitian patient presents with symptoms of a gynecologic cancer, such as postmenopausal bleeding. A lower threshold to order imaging to rule out metastasis, as well as early tumor marker acquisition, should be considered. Knowledge of this disease pattern may also impact counseling, as with only few exceptions, high-grade endometrial cancer will require chemotherapy. Further work with this population in the form of community advocacy, patient education, and physician awareness should be encouraged as a way to identify improved strategies for screening, prevention, and treatment.
Endometrial cancer is the most common gynecologic cancer. Aggressive, type II histologies are known to disproportionately affect black women, but further risk stratification within this group has not been performed.
Miami-Dade County in South Florida is the home to the largest cohort of Haitian immigrants in the United States. A recent single-institution review was performed to evaluate if Caribbean-born black women had different outcomes. Haitian women were under-represented in that study, so the decision was made to utilize a larger state registry to evaluate the burden of disease in this group.
The primary objective was to describe a cohort of urban Haitian immigrant women with endometrial cancer and evaluate disease patterns as they compare to other populations of black women.
Utilizing the Florida Cancer Data System, a retrospective cohort study was performed following STROBE guidelines.
Sixty-three point nine percent of the patients had a type II, high-grade, histology, and 52.6% presented with extrauterine metastatic disease. After stratification by histologic grade, both age [Hazard ratio (HR) = 0.88, 95% confidence interval (CI): 0.81-0.96, P = 0.002] and extrauterine disease (HR = 2.49, 95%CI: 1.01-6.21, P = 0.049) were independently associated with worse survival, but only in women with type II malignancies.
A greater proportion of Haitian women have type II endometrial cancer compared to other black populations in the United States. Prognostic variables for type II histologies were similar to previous reports.
The roles of nativity, ancestry, and acculturation in defining endometrial cancer risk are poorly understood in black women. Our results demonstrate that Haitian women have a greater burden of aggressive endometrial cancer than previously reported among black women. Additional research on the hereditary, somatic, and environmental causes of these findings is required.
The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System under contract with the Florida Department of Health (DOH). The views expressed herein are those of the author(s), and do not necessarily reflect those of the contractor or DOH.
| 1. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13300] [Cited by in RCA: 15624] [Article Influence: 2232.0] [Reference Citation Analysis (11)] |
| 2. | Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1609] [Cited by in RCA: 1745] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 3. | Schlumbrecht M, Baeker Bispo JA, Balise RR, Huang M, Slomovitz B, Kobetz E. Variation in type II endometrial cancer risk by Hispanic subpopulation: An exploratory analysis. Gynecol Oncol. 2017;147:329-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Olson SH, Atoria CL, Cote ML, Cook LS, Rastogi R, Soslow RA, Brown CL, Elkin EB. The impact of race and comorbidity on survival in endometrial cancer. Cancer Epidemiol Biomarkers Prev. 2012;21:753-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Jamison PM, Noone AM, Ries LA, Lee NC, Edwards BK. Trends in endometrial cancer incidence by race and histology with a correction for the prevalence of hysterectomy, SEER 1992 to 2008. Cancer Epidemiol Biomarkers Prev. 2013;22:233-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Cote ML, Ruterbusch JJ, Olson SH, Lu K, Ali-Fehmi R. The Growing Burden of Endometrial Cancer: A Major Racial Disparity Affecting Black Women. Cancer Epidemiol Biomarkers Prev. 2015;24:1407-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 197] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 7. | Schlumbrecht M, Huang M, Hurley J, George S. Endometrial cancer outcomes among non-Hispanic US born and Caribbean born black women. Int J Gynecol Cancer. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Anderson M, Lopez G. Key facts about black immigrants in the U.S. 2018 Jan 24 [cited 20 April 2019]. In: Pew Research Center [Internet]. Fanktank. Available from: https://www.pewresearch.org/fact-tank/2018/01/24/key-facts-about-black-immigrants-in-the-u-s/. |
| 9. | Zong J, Batalova J. Caribbean Immigrants in the United States. Migration policy institute. 2019; Available from: https://www.migrationpolicy.org/article/caribbean-immigrants-united-states. |
| 10. | Rebecca Sohmer, David Jackson, Bruce Katz, David Warren. The Haitian Community in Miami-Dade: A Growing the Middle Class Supplement. Brookings Institution Metropolitan Policy Program. 2005: 1-12. . |
| 11. | Jennifer Schulz, Jeanne Batalova. Haitian Immigrants in the United States. Migration policy institute 2017. Available from: http://www.migrationpolicy.org/article/haitian-immigrants-united-states. |
| 12. | Seay JS, Mandigo M, Kish J, Menard J, Marsh S, Kobetz E. Intravaginal practices are associated with greater odds of high-risk HPV infection in Haitian women. Ethn Health. 2017;22:257-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Seay JS, Carrasquillo O, Campos NG, McCann S, Amofah A, Pierre L, Kobetz E. Cancer Screening Utilization Among Immigrant Women in Miami, Florida. Prog Community Health Partnersh. 2015;9:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Setiawan VW, Pike MC, Kolonel LN, Nomura AM, Goodman MT, Henderson BE. Racial/ethnic differences in endometrial cancer risk: the multiethnic cohort study. Am J Epidemiol. 2007;165:262-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 87] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Creque A, Taioli E, Attong-Rogers A, Ragin C. Disparities in uterine cancer survival in a Brooklyn cohort of black women. Future Oncol. 2010;6:319-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Guttery DS, Blighe K, Polymeros K, Symonds RP, Macip S, Moss EL. Racial differences in endometrial cancer molecular portraits in The Cancer Genome Atlas. Oncotarget. 2018;9:17093-17103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Dubil EA, Tian C, Wang G, Tarney CM, Bateman NW, Levine DA, Conrads TP, Hamilton CA, Maxwell GL, Darcy KM. Racial disparities in molecular subtypes of endometrial cancer. Gynecol Oncol. 2018;149:106-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 74] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 18. | Xie R, Schlumbrecht MP, Shipley GL, Xie S, Bassett RL, Broaddus RR. S100A4 mediates endometrial cancer invasion and is a target of TGF-beta1 signaling. Lab Invest. 2009;89:937-947. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Hearst AA, Ramirez JM, Gany FM. Barriers and facilitators to public health insurance enrollment in newly arrived immigrant adolescents and young adults in New York state. J Immigr Minor Health. 2010;12:580-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Perry M, Kannel S, Burciaga Valdez R, Chang C. Medicaid and children, overcoming barriers to enrollment. 2000 Jan [cited 20 April 2019]. The Kaiser commission on Medicaid and the Uninsured. Available from: https://www.kff.org/wp-content/uploads/2013/01/medicaid-and-children-overcoming-barriers-to-enrollment-report.pdf. |
| 21. | Flores G, Abreu M, Brown V, Tomany-Korman SC. How Medicaid and the State Children's Health Insurance Program can do a better job of insuring uninsured children: the perspectives of parents of uninsured Latino children. Ambul Pediatr. 2005;5:332-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Echeverria SE, Carrasquillo O. The roles of citizenship status, acculturation, and health insurance in breast and cervical cancer screening among immigrant women. Med Care. 2006;44:788-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 118] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 23. | Siddiqi A, Zuberi D, Nguyen QC. The role of health insurance in explaining immigrant versus non-immigrant disparities in access to health care: comparing the United States to Canada. Soc Sci Med. 2009;69:1452-1459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 85] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Cavazos-Rehg P, Zayas L, Spitznagel E. Legal status, emotional well-being and subjective health status of Latino immigrants. J Natl Med Assoc. 2007;99:1126-1131. [PubMed] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited Manuscript
Specialty type: Oncology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pergialiotis V S-Editor: Tang JZ L-Editor: A E-Editor: Liu MY