©2014 Baishideng Publishing Group Inc.
World J Clin Oncol. Dec 10, 2014; 5(5): 1002-1019
Published online Dec 10, 2014. doi: 10.5306/wjco.v5.i5.1002
Published online Dec 10, 2014. doi: 10.5306/wjco.v5.i5.1002
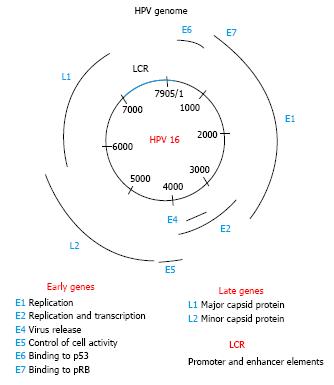
Figure 1 Human papilloma virus genome.
The genomic organization of the human papilloma virus 16 (HPV 16) is shown. The double strand DNA is close to 8000 base pairs. The early genes code for proteins involved in viral replication and transcription: E1, E2, E6, and E7 genes. The E4 and E5 genes are expressed a little later and have functions in immune evasion and virus release. The late genes code for the virus structural proteins: the major capsid protein L1, and the minor capsid protein L2. The E6 and E7 proteins of the high-risk HPV types have oncogenic properties. The long consensus repeat (LCR) sequence contains the promoter and enhancer elements of the virus.
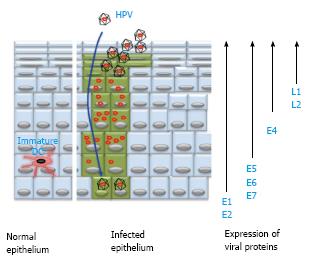
Figure 2 Papilloma virus replication is tissue specific.
The human papilloma virus (HPV) infects a keratinocyte in the basal layer of the epithelium after a micro trauma (a small cut of the epithelium that uncovers the basal membrane). The virus DNA is maintained in the proliferating cells at a low-copy number (E1 and E2 viral proteins are expressed). When the infected cells begin to differentiate into mature keratinocytes, the virus activates other genes (E4, E6, E7 viral proteins are expressed) and replicates its DNA to a high-copy number. In the top layers of the epithelium all viral proteins (including E4 and the capsid proteins L1 and L2) are expressed. Thousands of new virions are formed and released from the cells without causing cell death.
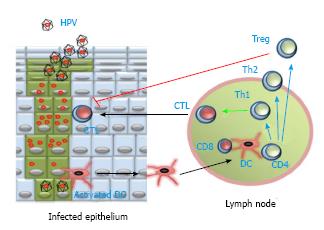
Figure 3 Cellular immune response against human papilloma virus.
Dendritic cells (DC) can take human papilloma virus (HPV) antigens from the infected epithelium, and then migrate (black arrows) to lymph nodes. There, DC present the processed antigen together with MHC class I and class II molecules, to CD8+ T cells and CD4+ T cells, respectively. CD4+ T cells proliferate and differentiate (blue arrows) into T helper cells, either Th1 or Th2, depending on the type of cytokines they produce. CD8+ T cells differentiate (blue arrow), with help (green arrow) from Th1 cells, into cytotoxic T cells (CTL). Then, CTL migrate (black arrow) back to the infected epithelium to destroy virus-infected cells. CD4+ T cells can also differentiate (blue arrow) into regulatory T cells (Treg), which inhibit (red line) the cytotoxic activity of CTL.
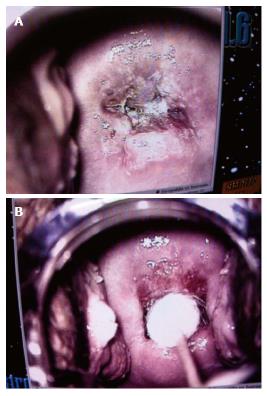
Figure 4 Conization of human papilloma virus cervical intraepithelial neoplasia 3 lesions.
Colposcopy of papillomavirus cervical intraepithelial neoplasia 3 lesions from a patient treated with conization. Photographs of cervix before (A) and immediately after conization (B).
Figure 5 Effects of vaccinia virus Ankara E2 on cervix and vulva.
Colposcopy of papillomavirus-induced intraepithelial lesions from patients treated with the therapeutic recombinant vaccinia virus Ankara E2. Photographs of (A) cervix with a cervical intraepithelial neoplasia 3 lesion, and (B) vulva with a condyloma lesion, before and after treatment. MVA: Modified vaccinia virus Ankara.
- Citation: Rosales R, Rosales C. Immune therapy for human papillomaviruses-related cancers. World J Clin Oncol 2014; 5(5): 1002-1019
- URL: https://www.wjgnet.com/2218-4333/full/v5/i5/1002.htm
- DOI: https://dx.doi.org/10.5306/wjco.v5.i5.1002