Published online Aug 15, 2016. doi: 10.4291/wjgp.v7.i3.296
Peer-review started: March 24, 2016
First decision: May 16, 2016
Revised: June 2, 2016
Accepted: July 14, 2016
Article in press: July 18, 2016
Published online: August 15, 2016
Processing time: 140 Days and 3.7 Hours
A Dieulafoy's lesion is a dilated, aberrant, submucosal vessel that erodes the overlying epithelium without evidence of a primary ulcer or erosion. It can be located anywhere in the gastrointestinal tract. We describe a case of massive gastrointestinal bleeding from Dieulafoy’s lesions in the duodenum. Etiology and precipitating events of a Dieulafoy’s lesion are not well known. Bleeding can range from being self-limited to massive life- threatening. Endoscopic hemostasis can be achieved with a combination of therapeutic modalities. The endoscopic management includes sclerosant injection, heater probe, laser therapy, electrocautery, cyanoacrylate glue, banding, and clipping. Endoscopic tattooing can be helpful to locate the lesion for further endoscopic re-treatment or intraoperative wedge resection. Therapeutic options for re-bleeding lesions comprise of repeated endoscopic hemostasis, angiographic embolization or surgical wedge resection of the lesions. We present a 63-year-old Caucasian male with active bleeding from the two small bowel Dieulafoy’s lesions, which was successfully controlled with epinephrine injection and clip applications.
Core tip: Small bowel Dieulafoy’s lesion is a rare entity that can cause severe life threatening gastrointestinal hemorrhage. It is difficult to diagnose and treat a small bowel Dieulafoy’s lesion by initial endoscopy unlike most gastric Dieulafoy’s lesions. We report a rare presentation of small bowel Dieulafoy’s lesions in a 63-year-old male. The hemorrhage was successfully controlled by epinephrine injection and clip applications. We also reviewed small bowel Dieulafoy’s lesion studies and reports in the literature.
- Citation: Sathyamurthy A, Winn JN, Ibdah JA, Tahan V. Culprit for recurrent acute gastrointestinal massive bleeding: “Small bowel Dieulafoy’s lesions” - a case report and literature review. World J Gastrointest Pathophysiol 2016; 7(3): 296-299
- URL: https://www.wjgnet.com/2150-5330/full/v7/i3/296.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v7.i3.296
Dieulafoy’s lesion (DL) is a dilated, aberrant, submucosal vessel that erodes the overlying epithelium without evidence of a primary ulcer or erosion[1]. Dieulafoy's lesions account for 0.5% to 14% of all acute upper gastrointestinal bleeding events[2,3]. They develop throughout the gastrointestinal tract. However, approximately 98% of the lesions occur in the stomach and 80% of the gastric lesions are located in the proximal lesser curvature[4]. Although bleeding from small bowel DLs is rare[3], it may cause recurrent life-threatening, massive acute gastrointestinal bleeding[5]. Endoscopic tattooing can be helpful in locating the lesions for further re-treatment such as bowel resection when endoscopic treatments fail[6]. There are limited data regarding endoscopic treatment of small bowel DLs. We report an unusual case of small bowel DLs that we encountered in our clinical practice.
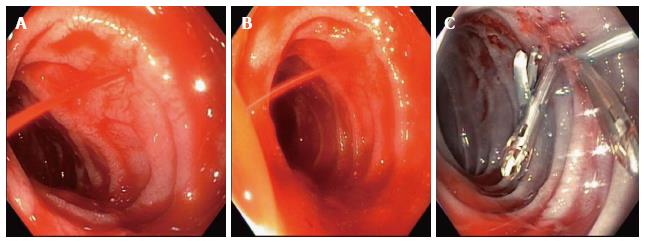
A 63-year-old Caucasian male who had: (1) an end-stage renal disease on hemodialysis; (2) radiation for squamous cell carcinoma of the throat; (3) gastrostomy tube insertion; (4) an episode of deep vein thrombosis (DVT) diagnosed a month prior to clinical presentation and on warfarin anticoagulation; (5) a recent diagnosis of invasive adenocarcinoma of the ascending colon; and (6) a history of intermittent melena/hematochezia with known duodenal bulb ulcers for which Helicobacter pylori eradication therapy was carried out one year prior to presentation. The patient presented with acute blood loss anemia and melena. Upon initial admission, he underwent two upper endoscopies with injection of epinephrine, deployment of hemostatic clips, and application of thermal cautery for duodenal bulb ulcers, then coil embolization of the gastroduodenal artery by interventional radiology. Despite these therapeutic interventions, he continued bleeding. Subsequently, he underwent tagged red blood cell scan to locate the source of bleeding, which was non-informative. He then had a colonoscopy, which revealed a previously noted an oozing friable and ulcerated colonic mass with a diameter of 2.5 cm that was treated with epinephrine. Further management of the colonic mass was deferred to the surgical oncology team due to the patient’s on-going bleeding and co-morbidities, the patient experienced no further bleeding during the hospitalization and were subsequently discharged without anticoagulation. However, 2 d following discharge, the patient presented again with anemia and melena. He was re-admitted for recurrent upper gastrointestinal bleeding. We performed an urgent esophagogastroduodenoscopy (EGD) on admission which revealed two DLs 5 cm distal to the previous clips on the posterior wall of the second part of the duodenum. One of these DLs was a spurting artery while the other was oozing. They were treated with 5 mL epinephrine injection followed by placement of four clips, which successfully controlled the massive bleeding (Figure 1). Subsequent superior mesenteric angiograms demonstrated no active gastrointestinal hemorrhage. No further episodes of bleeding reported after the patient’s discharge. The patient did not re-bleed during the same hospitalization for 5 d. He was discharged on hospice in view of his recurrent bleeding episodes and overall poor prognosis, then to home 2 d later.
The diameters of a DL vessels vary from 1 mm to 5 mm, which are about 10 times those of mucosal capillaries. They are usually located on the lesser curvature side of the gastroesophageal junction, although other areas of the gastrointestinal tract can be involved, including small intestines as in our case[3,7]. Etiology and precipitating events are not well known. Non-steroidal anti-inflammatory drugs may cause mucosal atrophy and ischemia[6]. Usually, the patients are males with co-morbidities such as coronary artery disease, diabetes, hypertension, chronic kidney disease, and alcohol abuse. Intensity of bleeding can vary from self-limited to life-threatening. The DL can be difficult to identify and it should be considered in the differential diagnosis of gastrointestinal bleeding without an obvious source.
Bleeding from small bowel DLs may be life-threatening and was treated only surgically before 1990[8]. The first published report of bleeding from small bowel DLs in 1978 involved 2 cases that were surgically treated[9]. Goldenberg et al[10] were the first to report a case of successful treatment of bleeding from duodenal DLs with a dual therapy with epinephrine injection and electrocoagulation. Recently, Lipka et al[3] recommended mechanical clipping as the therapy of choice since their three cases were successfully treated with clips after thermal therapy and/or radiological embolization failed. Furthermore, endoscopic hemostasis can be successfully achieved with a combination of epinephrine injection, hemostatic clip placement, bipolar coagulation, thermal coagulation, band ligation, argon plasma coagulation, and cyanoacrylate[10-13]. Endoscopic tattooing can be helpful in locating the lesions for endoscopic retreatment or intraoperative wedge resection. Therapeutic options for re-bleeding include repeat endoscopic hemostasis, angiographic embolization, or surgical wedge resection of the lesions. In general, endoscopic and angiographic interventions are initial attempted in controlling bleeding from DLs while a surgical approach is carried out if the others fail[12-16].
Table 1 summarizes the five case studies/reports about the management of the small bowel Dieulafoy’s lesions that were predominantly located in the jejunum. The bleeding was controlled with endoscopic interventions which reduced the need for surgery[3,12,18-20].
| Ref. | Dieulafoy’s Lesion (n) | Incidence (%) | Duodenum DL (n) | Jejunum DL (n) | Ileum DL (n) | Endoscopic treatment | Repeated endoscopic treatment | Surgery needed (n) |
| Lipka et al[3] | 8 | 2.6 | 1 | 7 | 0 | 8/8; Epi, bipolar, clips, APC | 1 | 0 |
| Prachayakul et al[17] | 5 | 4.31 | 0 | 5 | 0 | 5/5; Epi, clips, APC | 0 | 0 |
| Dulic-Lakovic et al[12] | 10 | 3.5 | 0 | 9 | 1 | 10/10; Epi, APC, clips | 3 | 2 |
| Chen et al[18] | 4 | 2.6 | 0 | 4 | 0 | 4/4; Epi and clips | 1 | 1 |
| Kozan et al[19] | 1 | N/A | 0 | 1 | 0 | 0 | 0 | 1 |
| Han et al[20] | 1 | N/A | 0 | 1 | 0 | 0 | 0 | 1 |
| Present report | 2 DLs in 1 case | N/A | 2 | 0 | 0 | 2/2; Epi and clips | 0 | 0 |
In conclusion, our case report and the current limited literature demonstrate that early aggressive endoscopic hemostasis of the small bowel DLs can be a successful alternative to surgery, with a low rate of re-bleeding.
A 63-year-old male who was on hemodialysis for end stage renal disease and warfarin for recent deep vein thrombosis, received radiation for squamous cell carcinoma of the throat, had gastrostomy tube insertion, had invasive adenocarcinoma of ascending colon, and had Helicobacter pylori eradication therapy for duodenal bulb ulcers. He presented with massive gastrointestinal hemorrhage.
Massive hemorrhage from the Dieulafoy’s lesions at the distal duodenum.
Hemorrhage from peptic ulcers or erosions, colon cancer, diverticuli, arteriovenous malformation, and aorto-enteric fistula.
The patient was admitted to the intensive care unit with an acute hemoglobin drop of 5 g/dL.
Upper endoscopy revealed active hemorrhage from the small bowel Dieulafoy’s lesions.
Submucosal epinephrine injection and placement of four clips’ application successfully controlled the hemorrhage.
Previous small bowel Dieulafoy’s lesion reports and studies were summarized in Table 1. The present report underlined the importance of the dual treatment for a successful outcome.
Dieulafoy’s lesion is a dilated aberrant submucosal vessel that erodes the overlying epithelium without evidence of a primary ulcer or erosion. Small bowel Dieulafoy’s lesion is rare but can cause life-threatening hemorrhage.
Small bowel Dieulafoy’s lesion hemorrhage is rare. When it is diagnosed, early aggressive endoscopic approach can be a successful alternative to extensive surgical resection.
The strongest point of this manuscript is reporting on a very rare diagnosis, successfully solved. The manuscript is concise and clear. The pictures are illustrative. The English language is fairly good. The experience presented in the manuscript could improve the readers’ practice.
| 1. | Lee YT, Walmsley RS, Leong RW, Sung JJ. Dieulafoy’s lesion. Gastrointest Endosc. 2003;58:236-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 138] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Stark ME, Gostout CJ, Balm RK. Clinical features and endoscopic management of Dieulafoy’s disease. Gastrointest Endosc. 1992;38:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 95] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Lipka S, Rabbanifard R, Kumar A, Brady P. A single-center United States experience with bleeding Dieulafoy lesions of the small bowel: diagnosis and treatment with single-balloon enteroscopy. Endosc Int Open. 2015;3:E339-E345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Baettig B, Haecki W, Lammer F, Jost R. Dieulafoy’s disease: endoscopic treatment and follow up. Gut. 1993;34:1418-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 98] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Parra-Blanco A, Takahashi H, Méndez Jerez PV, Kojima T, Aksoz K, Kirihara K, Palmerín J, Takekuma Y, Fuijta R. Endoscopic management of Dieulafoy lesions of the stomach: a case study of 26 patients. Endoscopy. 1997;29:834-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 66] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Jeon HK, Kim GH. Endoscopic Management of Dieulafoy’s Lesion. Clin Endosc. 2015;48:112-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 7. | Pollack R, Lipsky H, Goldberg RI. Duodenal Dieulafoy’s lesion. Gastrointest Endosc. 1993;39:820-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Choudari CP, Palmer KR. Dieulafoy’s lesion of the duodenum; successful endoscopic therapy. Endoscopy. 1993;25:371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Matuchansky C, Babin P, Abadie JC, Payen J, Gasquet C, Barbier J. Jejunal bleeding from a solitary large submucosal artery. Report of two cases. Gastroenterology. 1978;75:110-113. [PubMed] |
| 10. | Goldenberg SP, DeLuca VA, Marignani P. Endoscopic treatment of Dieulafoy’s lesion of the duodenum. Am J Gastroenterol. 1990;85:452-454. [PubMed] |
| 11. | Lara LF, Sreenarasimhaiah J, Tang SJ, Afonso BB, Rockey DC. Dieulafoy lesions of the GI tract: localization and therapeutic outcomes. Dig Dis Sci. 2010;55:3436-3441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Dulic-Lakovic E, Dulic M, Hubner D, Fuchssteiner H, Pachofszky T, Stadler B, Maieron A, Schwaighofer H, Püspök A, Haas T. Bleeding Dieulafoy lesions of the small bowel: a systematic study on the epidemiology and efficacy of enteroscopic treatment. Gastrointest Endosc. 2011;74:573-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (2)] |
| 13. | Iacopini F, Petruzziello L, Marchese M, Larghi A, Spada C, Familiari P, Tringali A, Riccioni ME, Gabbrielli A, Costamagna G. Hemostasis of Dieulafoy’s lesions by argon plasma coagulation (with video). Gastrointest Endosc. 2007;66:20-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Mumtaz R, Shaukat M, Ramirez FC. Outcomes of endoscopic treatment of gastroduodenal Dieulafoy’s lesion with rubber band ligation and thermal/injection therapy. J Clin Gastroenterol. 2003;36:310-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Nadal E, Burra P, Senzolo M. Cyanoacrylate injection to treat recurrent bleeding from Dieulafoy’s lesion. Gastrointest Endosc. 2013;78:964-965.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | D’Imperio N, Papadia C, Baroncini D, Piemontese A, Billi P, Dal Monte PP. N-butyl-2-cyanoacrylate in the endoscopic treatment of Dieulafoy ulcer. Endoscopy. 1995;27:216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Prachayakul V, Deesomsak M, Aswakul P, Leelakusolvong S. The utility of single-balloon enteroscopy for the diagnosis and management of small bowel disorders according to their clinical manifestations: a retrospective review. BMC Gastroenterol. 2013;13:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Chen TH, Chiu CT, Lin WP, Su MY, Hsu CM, Chen PC. Application of double-balloon enteroscopy in jejunal diverticular bleeding. World J Gastroenterol. 2010;16:5616-5620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Kozan R, Gülen M, Yılmaz TU, Leventoğlu S, Yılmaz E. Massive lower gastrointestinal bleeding from a jejunal Dieulafoy lesion. Ulus Cerrahi Derg. 2014;30:225-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Han MS, Park BK, Lee SH, Yang HC, Hong YK, Choi YJ. [A case of Dieulafoy lesion of the jejunum presented with massive hemorrhage]. Korean J Gastroenterol. 2013;61:279-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Serban DE, Vradelis S, Wang BM S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ