Published online Sep 22, 2025. doi: 10.4291/wjgp.v16.i3.106482
Revised: April 29, 2025
Accepted: July 3, 2025
Published online: September 22, 2025
Processing time: 204 Days and 14.7 Hours
Routine assessment of solid gastric emptying is challenging due to the prolonged test duration and complex meal preparation. Replacing solid test meals with easily prepared, commercially available semisolid meals and shortening the test duration can significantly enhance the feasibility and practicality of gastric emptying evaluations.
To compare the gastric emptying and antral motility of solid vs semi-solid meals of similar volume and nutritional consistency, and to assess the feasibility of meal substitution and reduction in test duration during the solid gastric emptying assessment.
Thirty healthy volunteers (17 males, age: 29.4 ± 6.0 years, body mass index: 23.4 ± 2.94 and 13 females, age: 37.2 ± 11.9 years, body mass index: 22.9 ± 4.34) un
Mean and median antral areas, gastric emptying rates, gastric residual ratios, and motility index at each time point were almost similar between meals for up to 3 hours. At the end of 4 hours, the mean emptied percentage of the semisolid meal and solid meal was 81.1% and 70.6%, respectively. The emptying rate of the semisolid meal at 90 minutes significantly correlated with that of 240 minutes. There was no correlation between the solid meal emptying rates at 90 minutes and 240 minutes.
Gastric emptying, residual antral cross-sectional area and antral motility of a semisolid meal are almost similar to that of a solid meal of the same nutritional value until three hours post-ingestion. A semisolid test meal can effectively substitute a solid test meal during ultrasound assessment of gastric emptying, without compromising the validity of the results. Additionally, the ease of preparation and administration of semisolid meals enhances the overall feasibility of gastric emptying assessments.
Core Tip: Semisolids are commonly believed to empty from the stomach faster than solids, with a significantly shorter lag time. However, using semisolid and solid meals of identical volume and nutritional composition, we demonstrated that gastric emptying rates and antral motor activities were comparable for both meal types up to three hours post-ingestion, with similar half-emptying times. Real-time ultrasonography using a pre-prepared, commercially available, and culturally acceptable semisolid test meal proved to be a reliable and valid method for assessing gastric emptying. This approach offers an effective alternative to traditional solid meal gastric emptying measurements.
- Citation: Amarasiri L, de Silva M, de Silva HJ, Devanarayana NM. Comparison of gastric emptying of solid and semi-solid meals using real-time ultrasonography in healthy Sri Lankan adults. World J Gastrointest Pathophysiol 2025; 16(3): 106482
- URL: https://www.wjgnet.com/2150-5330/full/v16/i3/106482.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v16.i3.106482
The study of the gastric emptying of a solid meal is invaluable in diseases such as gastroesophageal reflux disease, functional gastrointestinal disorders and diseases associated with autonomic neuropathy, such as diabetes mellitus[1]. With lifestyle changes, such diseases are on the rise and more and more patients present with abdominal complaints related to delayed gastric emptying, hence the need for objective testing of gastric motility before treatment.
Real-time ultrasonography is a simple, non-invasive and valid method for assessing gastric emptying and antral motility after either a liquid or a solid meal[2,3]. Yet, the methods currently employed to assess solid gastric emptying are based on the time taken by a solid meal to exit the stomach and are time-consuming, taking up to 4 hours[2], which makes it difficult to be used as a routine diagnostic test, especially in children. Therefore, a reduction of the time spent on the gastric emptying assessment test would be invaluable in clinical practice in terms of convenience to the patients and laboratory staff, as well as in research, which will significantly improve the participation of subjects. In addition, the preparation of a solid test meal is cumbersome in laboratory settings.
To overcome the shortcomings of using a solid meal as a test meal, a newer, shorter version of the conventional method (90-minute gastric emptying) has been developed by a group of Swedish investigators. They used real-time ultrasonography to determine gastric antral cross-sectional area in a single section of the stomach, defining the gastric emptying rate (GER) as the percentage reduction in antral cross-sectional area from 15 minutes (area of maximal antral dilation) to 90 minutes after the ingestion of a standardized nutrient semisolid breakfast meal (300 g rice pudding, 330 kcal). This is a convenient method for estimating gastric emptying[4]. However, due to variations in the types of diets consumed and genetic factors, gastric emptying is likely to vary between different populations with different food habits. Therefore, it is not possible to introduce techniques and test meals developed in Western countries directly to other regions of the world, including the Sri Lankan population.
The gastric emptying of a solid and semi-solid meal is somewhat similar. After ingestion of a semi-solid or solid meal, there is an initial delay called the “lag phase”, followed by an emptying phase that approximates a linear pattern. The lag phase depends on the time taken to redistribute food from the proximal to the distal stomach and the mixing and grinding of solid food into small particles in the distal stomach[5,6]. The lag phase is considered to be shorter for a semi-solid meal than for a solid meal. However, no studies have been conducted to compare the exact difference in lag phase and emptying times of solid and semisolid meals of similar nutritional composition.
Various test meals have been employed in the past to measure gastric emptying by ultrasonography. The caloric content, volume, and consistency of solid meals should have been designed to conform to the usual breakfast of a par
This study was carried out with three objectives. The main objectives of this study were to compare distal stomach emptying of solid and semisolid meals of similar volume and nutritional consistency and to assess the validity of replacing solid gastric emptying with a semisolid meal that is similar in caloric content to a typical Sri Lankan breakfast, yet easy to prepare. The other objective was to assess the validity of measuring solid gastric emptying using the pre
The study was conducted at the Gastroenterology Research Laboratory of the Faculty of Medicine, University of Kelaniya, Ragama, Sri Lanka. Subject recruitment and data collection were conducted from December 2014 to January 2018.
Thirty healthy adult volunteers were recruited for the study using a convenient sampling technique after obtaining written informed consent.
Inclusion criteria: (1) Healthy adults aged 18 to 40 years; and (2) Who give informed written consent for participation in the study.
Exclusion criteria: (1) Presence of a chronic disease or taking long-term medication for an illness; (2) Presence of symptoms related to the gastrointestinal tract; (3) Acute illness during the 2 weeks preceding the laboratory testing; (4) Previous surgery involving the gastrointestinal tract; and (5) Using medication affecting gastric motility during the period of study. The presence of gastrointestinal symptoms was assessed by a previously validated gastroesophageal reflux disease symptom questionnaire[8].
Each subject was given two different test meals in random order on two separate days, one week apart, as breakfast. The calorie content of each meal was approximately 350 kcal and consisted of around 60% carbohydrate, 30% fat and 10% protein. Both meals were ingested within 10 minutes, along with 300 mL of water.
The solid meal (mung kiribath, mung bean cooked with rice and milk; 349 kcal; 82 g) contained 52 g of carbohydrate, 10 g of protein and 11 g of fat. The mung bean (24 g) was soaked with water overnight and then microwaved with rice (40 g) and 250 mL of water, on medium-high for 15 minutes. Then, evaporated milk powder (25 g), sugar (20 g) and butter (5 g) were added to make it more palatable and to achieve the required calorie content.
The semi-solid meal (Nestum Mung; 347 kcal; 82 g) contained 52 g of carbohydrate, 10 g of protein and 11 g of fat. This was a commercially prepared cereal (Nestum Mung 32 g), which was mixed with water (250 mL), evaporated milk powder (25 g), sugar (20 g) and butter (5 g) in similar proportions as for the solid meal.
Female subjects were examined during the follicular phase of the menstrual cycle to avoid any influence of the hormonal changes during the cycle. No participants were recruited during religious fasting or a dietary intervention. All study participants were advised to refrain from caffeine, nicotine or alcohol for 8 hours before assessing gastric motility. Drugs affecting gastric motility (e.g., anticholinergics, narcotics, prokinetics and erythromycin) were stopped for 48 hours prior to the test.
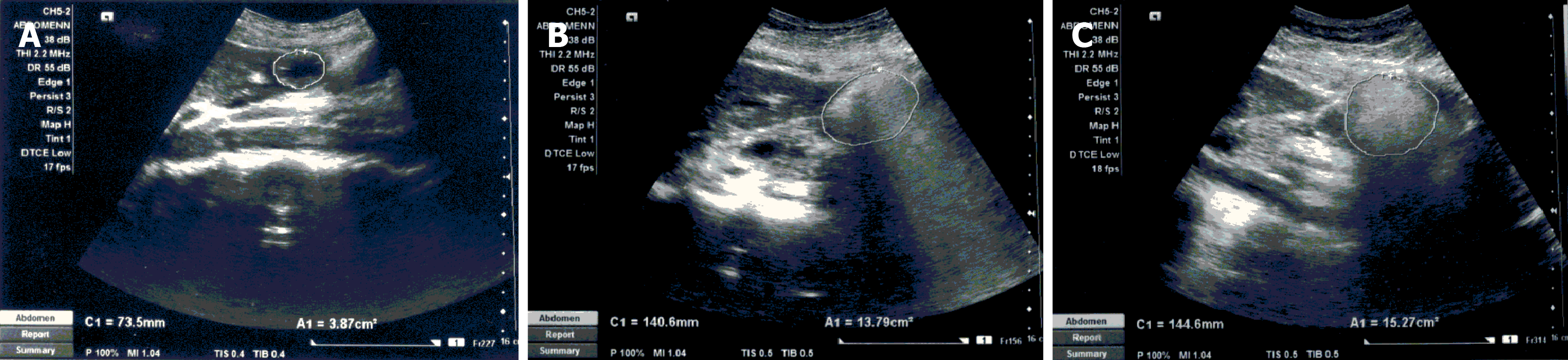
The gastric motility assessments were performed in the morning after an overnight fast of 8 hours. The subjects were examined by real-time ultrasonography performed with a high-resolution real-time scanner (SIEMENS ACUSON X300, Thailand) with a 3.5 MHz convex array transducer with facilities to record and playback. Gastric motility assessments in all patients commenced between 8:00 am and 8:30 am. Both gastric motility measurements of each patient were made by the same examiner, who was blinded with respect to the test meal. The subjects were examined in a semi-recumbent position and rested in a seated position in between measurements. The antrum, superior mesenteric artery and abdominal aorta were simultaneously visualized by the transducer (Figure 1). The record-and-playback technique was employed to enhance measurement accuracy.
Measurement of the gastric motility was done using a previously described standardized ultrasound method[2]. The cross-sectional area of the antrum and frequency and amplitude of antral contractions were measured during the fasting period (0 minute) and at 5 minutes, 15 minutes, 30 minutes, 45 minutes, 60 minutes,90 minutes, 120 minutes, 180 minutes and 240 minutes after ingestion of each test meal. At each time point, the antral cross-sectional area was estimated by tracing the mucosal side of the antrum with an in-built caliper and the frequency of antral contractions was taken as the number of contractions per consecutive 3 minutes. The amplitude was calculated from the maximum reduction of the antral area for each contraction. For each subject and type of test meal, the gastric motility parameters were calculated as follows.
For the conventional method: GERn = [(cross-sectional area at each point of observation-fasting cross-sectional area/cross-sectional area at 5 minute-fasting cross-sectional area) - 1] × 100. Gastric residual ratio (GRR) = (cross-sectional area at each point of observation-fasting cross-sectional area/cross-sectional area at 5 minutes-fasting cross-sectional area) × 100.
For the simplified method: GER90 = [(cross-sectional area at 90 minutes/cross-sectional area at 15 minutes) - 1] × 100.
For the antral motility assessment: Amplitude of antral contractions = [(cross-sectional area at relaxation - cross-sectional area at contraction)/cross-sectional area at relaxation]/100. Antral motility index = amplitude of antral contractions × frequency of antral contractions/100.
To avoid the day-to-day variation in fasting antral size, for comparison of solid and semisolid meals, the antral cross-sectional area at each time point was taken after deducting the fasting antral cross-sectional area of that particular day (e.g., cross-sectional area at 15 minutes = measured cross-sectional area at 15 minutes - fasting cross-sectional area). As the maximal antral cross-sectional area was seen at 5 minutes post-ingestion, it was used to calculate GER and GRR at each time point.
At an 80% power (1 - β = 0.80) and a 5% significance level (α = 0.05), to detect a difference of GER of 10% between two meals, the minimum sample required for this crossover study was 22. Statistical analyses were conducted using PSPP version 2.0.1 (Free Software Foundation, Inc., http://fsf.org/). Median gastric motility parameters were compared using the nonparametric Wilcoxon signed-rank test. The GRR and GER were calculated for both the semi-solid and solid meals and correlated using the Spearman correlation coefficient. A P < 0.05 was considered statistically significant.
Ethical approval was obtained from the Ethics Review Committee of the Faculty of Medicine, University of Kelaniya. All participants gave written informed consent. All procedures conformed to the Declaration of Helsinki.
A total of 30 subjects were recruited in the study. Of them, 17 (56.6%) were males (mean age: 29.4 ± 6.0 years, body mass index: 23.4 ± 2.94), and 13 were females (mean age: 37.2 ± 11.9 years, body mass index: 22.9 ± 4.34). None of them had chronic gastrointestinal disorders, nor symptoms related to the gastrointestinal tract during the previous 3 months.
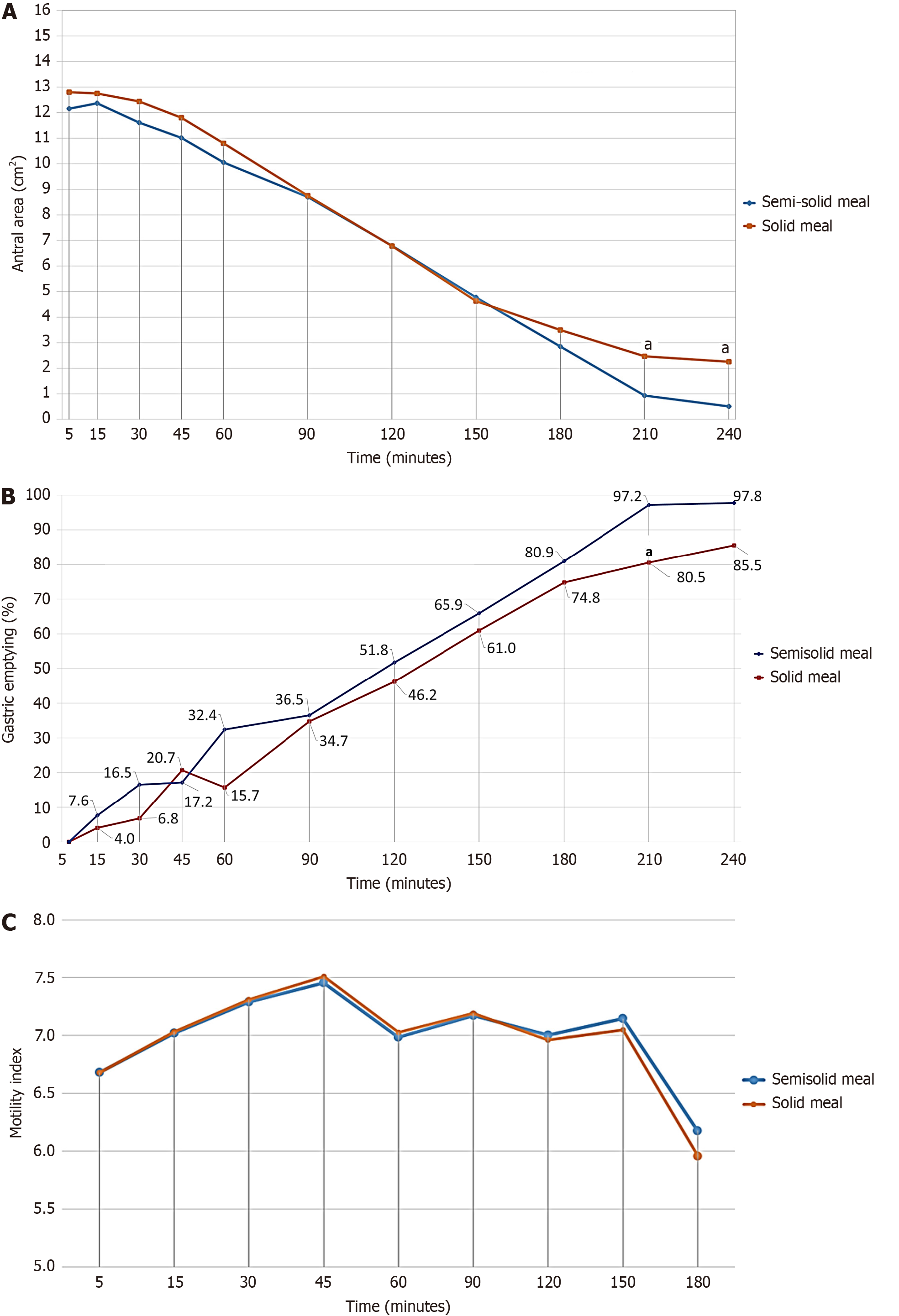
Figure 2A shows the median residual gastric antral areas after ingesting solid and semisolid meals. Gastric residual antral area following both meals showed a similar biphasic pattern for the first 3 hours after the meal, with a lag phase of 60 minutes. The half-emptying time was approximately 120 minutes for both meals. The median GER of both meals did not differ significantly up to 3 hours post-ingestion, after which the solid meal emptying was slower (Figure 2B). At the end of 4 hours, the mean percentage emptying of the semisolid meal was 81.1%, and of the solid meal, it was 70.6%. In the semisolid meal, GER at 90 minutes significantly correlated with the GER at 240 minutes (r = 0.594, P = 0.042). There was no such correlation in the solid meal between 90-minute and 240-minute GERs (r = 0.055, P = 0.852). The median GRR (Table 1) and antral motility index (Figure 2C) at each time point did not differ significantly between the two meals. GER of the two meals showed a significant positive correlation up to three hours of post-ingestion (Table 2).
| Time after ingestion | Gastric residual ratios (%) | ||
| Semisolid meal | Solid meal | P value1 | |
| 5 minutes | 100.00 | 100.00 | 1.000 |
| 15 minutes | 96.90 ± 2.78 | 93.28 ± 5.10 | 0.959 |
| 30 minutes | 94.57 ± 3.02 | 86.28 ± 5.18 | 0.992 |
| 45 minutes | 84.41 ± 3.61 | 85.10 ± 4.84 | 0.491 |
| 60 minutes | 87.00 ± 4.25 | 73.68 ± 4.05 | 0.090 |
| 90 minutes | 72.02 ± 4.32 | 68.86 ± 4.40 | 0.766 |
| 120 minutes | 60.69 ± 3.66 | 55.32 ± 4.16 | 0.349 |
| 150 minutes | 44.43 ± 3.48 | 49.32 ± 3.38 | 0.318 |
| 180 minutes | 33.79 ± 3.08 | 37.53 ± 2.84 | 0.294 |
| 210 minutes | 19.52 ± 2.70 | 28.43 ± 3.54 | 0.016 |
| 240 minutes | 18.90 ± 2.79 | 29.34 ± 5.66 | 0.110 |
| Time after ingestion | Correlation coefficient | P value1 |
| 5 minutes | - | - |
| 15 minutes | 0.325 | 0.079 |
| 30 minutes | 0.203 | 0.283 |
| 45 minutes | 0.600 | < 0.001 |
| 60 minutes | 0.572 | 0.001 |
| 90 minutes | 0.628 | < 0.001 |
| 120 minutes | 0.521 | 0.003 |
| 150 minutes | 0.500 | 0.005 |
| 180 minutes | 0.412 | 0.026 |
| 210 minutes | 0.237 | 0.244 |
| 240 minutes | 0.309 | 0.355 |
The current study was carried out to increase the feasibility of testing gastric emptying and antral motility of solids by means of a comparable semi-solid meal, using safe and non-invasive real-time ultrasonography. In this study, the pattern of gastric emptying and gastric motility parameters were not significantly different between the solid and semisolid meals up to 3 hours following ingestion of the test meal. However, total gastric emptying time was shorter after ingestion of the semisolid meal with the same nutritional composition, volume and calorie content. In addition, the GER at 90 minutes following a semisolid meal significantly correlated with gastric emptying at 240 minutes, but no such correlation was observed following a solid meal.
In this study, the maximum antral area was reached at 5 minutes post-ingestion for both meals, and there was no significant difference in the timings. A previous study conducted on Sri Lankan adults, which used bread and dhal curry as the test meal, also demonstrated a maximum antral size at 5 minutes[9]. However, the 15-minute post-ingestion ma
Solid foods need to undergo mechanical digestion and should be broken down into particles less than 2 mm in size before being emptied from the stomach[11]. The semisolid meal we used in this study was already in powdered form and did not need mechanical digestion; therefore, it could be emptied immediately after ingestion. Hence, we expected that the gastric emptying of the semisolid meal would be faster than that of a solid meal. However, in the present study, gastric emptying parameters, including antral areas, GERs, GRRs, and the motility index, did not show significant differences between the solid and semisolid meals during serial measurements within the first three hours post-ingestion. In addition, the GERs of the solid and semisolid meals positively correlated up to 3 hours post-ingestion. Thereafter, the gastric emptying of the solid test meal was slower. The gastric half-emptying time is the time when 50% of the gastric contents have emptied. The half-emptying time was almost similar (120 minutes) for both meals. At the end of 4 hours, the mean emptied percentage of the semisolid meal was more than that of the solid meal (81.1% vs 70.6%).
Both solid and semisolid gastric emptying (GE) patterns in our study subjects showed the biphasic pattern previously described for solid gastric emptying[6,12]. Within the first 60 minutes after ingestion of both solid and semisolid meals, the reduction in GRR was smaller compared to the next 3 hours, indicating a 60-minute lag phase. This was followed by a fast, near-linear pattern of reduction in GRR, depicting the rapid gastric emptying phase. Since the semisolid meal we used in this study did not need mechanical digestion, we expected a significantly shorter lag phase for the semisolid meal. However, our findings indicate that the lag phase does not differ depending on the consistency of the meal. No previous study has compared solid and semisolid meals of the same volume and nutritional consistency. Previous studies have described a longer lag phase for a solid test meal and a relatively shorter lag phase for a liquid meal[5,13]. In those studies, the composition, volume and nutritional values of the solid and liquid meals were different, and their effects on differences in lag phases have not been considered.
Our results show that the consistency (whether solid or semisolid) of a test meal does not significantly influence the main gastric motility parameters such as gastric antral size, GER, antral motility index and GRR until the final stages of gastric emptying. Therefore, semisolid test meals could successfully replace the use of solid test meals during assessment of gastric emptying. In addition, 90 minutes GER of the semisolid meal significantly correlated with the 240 minutes GER. However, the lack of such correlation between 90-minute and 240-minute GER indicates that the 90-minute GER is not a reliable indicator of the measurement of solid gastric emptying.
Real-time ultrasonography is a preferred method of measuring GE as it is simple and non-invasive, with minimal discomfort to patients. Previous studies have shown a close correlation in gastric emptying simultaneously measured by scintigraphy and ultrasonography[4]. This technique has also shown a good inter-observer agreement[14]. The main disadvantages of using ultrasound techniques to measure solid gastric emptying were difficulty in preparing a culturally acceptable test meal in the laboratory, the need to perform ultrasound scanning for a long duration (minimum of 4 hours after a meal) and the need for well-trained staff. These are the main limitations of using this method as a routine diag
A group of Swedish investigators validated a shorter version (90-minute gastric emptying) of the conventional method[4]. The test meal used in that study could not be directly applied to Sri Lankan patients. In the present study, we attempted to replace the conventional long-duration solid GE test with a shorter version of the test using the semi-solid test meal acceptable to the Sri Lankan population. The reduction of the test time from 4 hours to one and a half hours and validation of commercially prepared, culturally acceptable, nutritious and palatable test meals would be more convenient to patients and laboratory staff and is also likely to improve the participation of subjects in related research activities. However, the median GER at 90 minutes observed in our study (36.5%) was lower than that reported in a previous study (63%)[4]. This difference in gastric emptying at 90 minutes may be attributed to several factors, including variations in the nutritional content, fat composition, and volume of the test meal, as well as genetic, cultural, and environmental differences across populations and regions. A previous study conducted in Sri Lanka using the same ultrasound technique assessed solid gastric emptying in both asthmatic patients and healthy controls. The gastric emptying parameters reported in healthy controls in that study (e.g., half emptying time of 119 minutes, GER at 210 minutes of 71.8%, and a residual ratio at 90 minutes of 60%) closely resemble those observed in our current study, despite differences in the specific test meal used[9]. Importantly, the test meal in the previous study, like ours, reflected a typical Sri Lankan breakfast. These similarities suggest that the solid gastric emptying patterns reported in our study are representative of the physiological norm in healthy Sri Lankan individuals.
This study has several limitations. First, the real-time ultrasound techniques employed allowed assessment of gastric emptying in the distal stomach but did not evaluate proximal gastric accommodation. Second, the gastric emptying of solid and semisolid meals was measured 1 week apart, making it difficult to rule out day-to-day variations in gastric motility completely. Nevertheless, using the record-and-playback technique and assessments conducted by the same investigator enhances the validity and consistency of the findings. Third, Helicobacter pylori (H. pylori) infection has been reported to reduce the number of gastric pacemaker cells, leading to delayed gastric emptying[15]. The infection is highly prevalent in Sri Lanka, affecting approximately 70% of the population[16]. Although we did not assess H. pylori status in our study participants, we compared gastric motility within the same individuals following solid and semisolid meals. Therefore, any potential effect of H. pylori infection on gastric motility would be consistent across both meal types and unlikely to influence the comparative results. Last, we used a safe and non-invasive ultrasound technique to assess the gastric emptying after solid and semisolid meals, instead of scintigraphy, which is the gold standard. However, ultrasound techniques have been previously compared with scintigraphy and shown to be accurate in measuring gastric emptying[4,17-19]. The technique we used has been compared with the 13C-octanoic acid breath test and shown to be accurate[20].
This study demonstrates that solid and semisolid meals with identical nutrient composition, volume, and caloric content exhibit comparable antral distension, GERs and antral motility patterns up to 3 hours post-ingestion, with similar half-emptying times and lag phases. Real-time ultrasonography using a pre-prepared, commercially available, culturally acceptable semisolid meal provides a reliable, valid, and practical alternative to solid meal gastric emptying assessments. The ease of preparation and enhanced feasibility of the semisolid meal further support its use in clinical and research settings.
We acknowledge Mrs. J. Liyanage, Technical Officer, Department of Physiology, Faculty of Medicine, University of Kelaniya, for her technical assistance.
| 1. | Camilleri M, Hasler WL, Parkman HP, Quigley EM, Soffer E. Measurement of gastrointestinal motility in the GI laboratory. Gastroenterology. 1998;115:747-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 199] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 2. | Haruma K, Kusunoki H, Manabe N, Kamada T, Sato M, Ishii M, Shiotani A, Hata J. Real-time assessment of gastroduodenal motility by ultrasonography. Digestion. 2008;77 Suppl 1:48-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Bolondi L, Bortolotti M, Santi V, Calletti T, Gaiani S, Labò G. Measurement of gastric emptying time by real-time ultrasonography. Gastroenterology. 1985;89:752-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 313] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 4. | Darwiche G, Almér LO, Björgell O, Cederholm C, Nilsson P. Measurement of gastric emptying by standardized real-time ultrasonography in healthy subjects and diabetic patients. J Ultrasound Med. 1999;18:673-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 87] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Camilleri M, Malagelada JR, Brown ML, Becker G, Zinsmeister AR. Relation between antral motility and gastric emptying of solids and liquids in humans. Am J Physiol. 1985;249:G580-G585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 75] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Siegel JA, Urbain JL, Adler LP, Charkes ND, Maurer AH, Krevsky B, Knight LC, Fisher RS, Malmud LS. Biphasic nature of gastric emptying. Gut. 1988;29:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 262] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 7. | Wickramanayake LW. Requirements of Energy and Protein. In: Wickramanayake TW. Food and Nutrition. 3rd ed. Colombo: Hector Kobbekaduwa Agrarian Research and Training Institute, 1996: 30-55. |
| 8. | Amarasiri LD, Pathmeswaran A, De Silva AP, Dassanayake AS, Ranasinha CD, De Silva J. Comparison of a composite symptom score assessing both symptom frequency and severity with a score that assesses frequency alone: a preliminary study to develop a practical symptom score to detect gastro-oesophageal reflux disease in a resource-poor setting. Eur J Gastroenterol Hepatol. 2010;22:662-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 9. | Amarasiri WA, Pathmeswaran A, de Silva AP, Dassanayake AS, Ranasinha CD, de Silva HJ. Gastric motility following ingestion of a solid meal in a cohort of adult asthmatics. J Neurogastroenterol Motil. 2013;19:355-365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Darwiche G, Björgell O, Almér LO. The addition of locust bean gum but not water delayed the gastric emptying rate of a nutrient semisolid meal in healthy subjects. BMC Gastroenterol. 2003;3:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Kong F, Singh RP. Disintegration of solid foods in human stomach. J Food Sci. 2008;73:R67-R80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 379] [Cited by in RCA: 399] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 12. | Hellström PM, Grybäck P, Jacobsson H. The physiology of gastric emptying. Best Pract Res Clin Anaesthesiol. 2006;20:397-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 146] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 13. | Collins PJ, Houghton LA, Read NW, Horowitz M, Chatterton BE, Heddle R, Dent J. Role of the proximal and distal stomach in mixed solid and liquid meal emptying. Gut. 1991;32:615-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 131] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Irvine EJ, Tougas G, Lappalainen R, Bathurst NC. Reliability and interobserver variability of ultrasonographic measurement of gastric emptying rate. Dig Dis Sci. 1993;38:803-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 59] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Liu B, Dong J, Wang S, Yu H, Li Z, Sun P, Zhao L. Helicobacter pylori causes delayed gastric emptying by decreasing interstitial cells of Cajal. Exp Ther Med. 2021;22:663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Fernando N, Holton J, Vaira D, DeSilva M, Fernando D. Prevalence of Helicobacter pylori in Sri Lanka as determined by PCR. J Clin Microbiol. 2002;40:2675-2676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Hveem K, Jones KL, Chatterton BE, Horowitz M. Scintigraphic measurement of gastric emptying and ultrasonographic assessment of antral area: relation to appetite. Gut. 1996;38:816-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 136] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 18. | Benini L, Sembenini C, Heading RC, Giorgetti PG, Montemezzi S, Zamboni M, Di Benedetto P, Brighenti F, Vantini I. Simultaneous measurement of gastric emptying of a solid meal by ultrasound and by scintigraphy. Am J Gastroenterol. 1999;94:2861-2865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Gomes H, Hornoy P, Liehn JC. Ultrasonography and gastric emptying in children: validation of a sonographic method and determination of physiological and pathological patterns. Pediatr Radiol. 2003;33:522-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Aoki S, Haruma K, Kusunoki H, Hata J, Hara M, Yoshida S, Tanaka S, Chayama K. Evaluation of gastric emptying measured with the 13C-octanoic acid breath test in patients with functional dyspepsia: comparison with ultrasonography. Scand J Gastroenterol. 2002;37:662-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/