Published online Jun 28, 2015. doi: 10.4329/wjr.v7.i6.134
Peer-review started: January 7, 2015
First decision: March 6, 2015
Revised: April 20, 2015
Accepted: May 5, 2015
Article in press: May 6, 2015
Published online: June 28, 2015
Processing time: 161 Days and 20.7 Hours
Medical imaging and interventional radiology sustained prompt changes in the last few years, mainly as a result of technology breakthroughs, rise in workload, deficit in workforce and globalization. Risk is considered to be the chance or possibility of incurring loss or of a negative event happening that may cause injury to patients or medical practitioners. There are various causes of risks leading to harm and injury in radiology departments, and it is one of the objectives of this paper to scrutinize some of the causes. This will drive to consideration of some of the approaches that are used in managing risks in radiology. This paper aims at investigating risk management in radiology, and this will be achieved through a thorough assessment of the risk control measures that are used in the radiology department. It has been observed that the major focus of risk management in such medical setting is to reduce and eliminate harm and injury to patients through integration of various medical precautions. The field of Radiology is rapidly evolving due to technology advances and the globalization of healthcare. This ongoing development will have a great impact on the level of quality of care and service delivery. Thus, risk management in radiology is essential in protecting the patients, radiologists, and the medical organization in terms of capital and widening of the reputation of the medical organization with the patients.
Core tip: This paper serves as a review of risk management in radiology. It investigates the potential sources of risk within radiology departments and proposes measures that may potentially mitigate these risks. A major focus of risk management is to reduce harm and injury to patients and personnel and it aims to improve the outcomes from radiology departments. Risk management in radiology is essential in protecting the patients, radiologists, and the medical organization.
- Citation: Craciun H, Mankad K, Lynch J. Risk management in radiology departments. World J Radiol 2015; 7(6): 134-138
- URL: https://www.wjgnet.com/1949-8470/full/v7/i6/134.htm
- DOI: https://dx.doi.org/10.4329/wjr.v7.i6.134
Medical imaging and interventional radiology have sustained dramatic changes in the last few years, mainly as a result of technological breakthroughs, the rise in workload, a deficit in the workforce and globalisation. Consequently there is an expanding concern about standards of care, maintaining patient safety and the management of risk in radiology.
People understand the concepts of risk and risk management in a medical setting in different ways. Risk is considered to be the possibility of incurring loss or of a negative event occurring that may cause injury to patients or medical practitioners[1]. One cannot predict all risks. That is to say, injury to patients may occur even in the best hospitals where patients receive high-quality services and treatments. Then risk management refers to the various approaches that medical practitioners and professionals integrate to reduce risk[2]. This is a proactive concept that involves practices such as identification of risk, quantification and evaluation of risk and consideration of measures that can be used to eliminate or control risk in a medical setting. All those involved in providing healthcare services participate in risk management. This includes management of the medical centres obligated to provide adequate facilities, staff, resources, financial support and equipment, thus helping professionals and nursing practitioners reduce the odds of harm’s occurring[3].
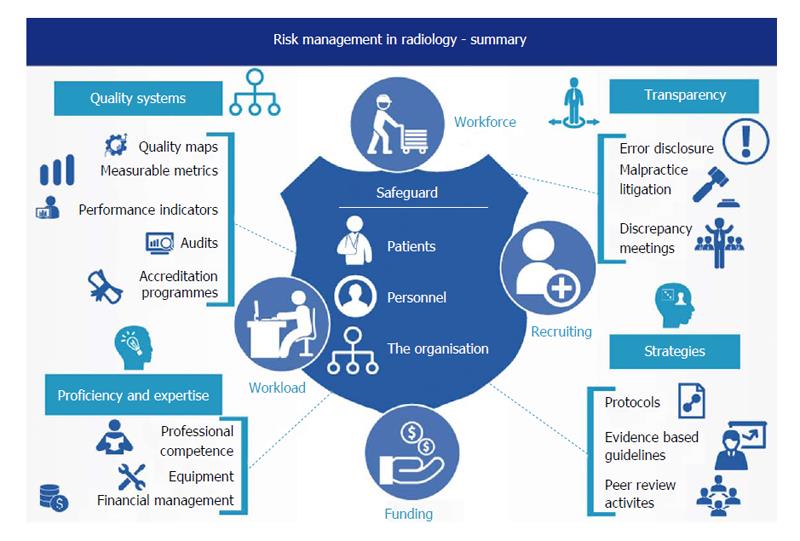
This paper aims at investigating risk management in radiology through a thorough assessment of the risk control measures that are used in the radiology department[4]. The major focus of risk management in such medical settings is to reduce and eliminate harm and injury to patients through the incorporation of various medical precautions[5]. As depicted in Figure 1 risks leading to harm and injury in radiology departments stem from various causes. One objective of this paper is to scrutinise some of these. This will expand into the consideration of some of the approaches healthcare practitioners implement to manage risk in radiology.
The rapid expansion of services, the globalization of healthcare and the imbalance between workload and workforce are a few of the factors that may threaten the standards of health services as well as patient safety[6]. There is a rising demand for radiologists and for 24/7 services. Therefore, international teleradiology is leading the globalisation occurring in the field of radiology[7].
To meet the expectations of quality services, systems should be put in place to pave the way for higher standards of care. Quality systems are effective risk control measures, hence the importance of professional organisations to lead, establish, uphold and improve them[8]. Quality improvement measures range from quality maps, measurable metrics and performance indicators to audits and accreditation programmes. These collective efforts may decrease a department’s risk and benefit patients[9].
Risk management in radiology is primarily developed and fostered to help safeguard patients, working personnel and the entire organisation. Protection of the organisation is largely grasped in terms of finance management and potential drawbacks linked to unreliable results that could damage its reputation[10].
Managers and clinicians in the radiology department should focus on improving the general quality of care medical staff deliver to patients. Radiology professionals subject themselves to risk every time they perform a procedure because some of the techniques and instruments they use in scanning and imaging are complex[11]. Thus, players in the healthcare setting must work carefully and diligently to ensure that they minimise health risk to patients and to themselves. In practice, inherent hazards to safety and quality manifest in relation to personnel availability, workload and financial predicaments. They consist of insubstantial funding for new equipment in the workplace, difficulty retaining professionals, the escalating complexity of the work, the increasing workload, difficulty recruiting due to a national shortage of medical staff and the lessening budget that is not keeping up with current of demands.
Radiology professionals must persuade administrators and managers that standards of care relate closely to performance metrics like workload, diagnostic precision and patient safety concerns[12]. Thus, managers must make sensible decisions about resource allocation and performance expectations to mirror this reality and curtail risks[10].
All health professionals must identify some of the issues that tend to cause harm to patients in advance and work on them before subjecting the patient to potentially faulty processes[13]. The concept of ALARP, or “as low as reasonably practicable”, essentially refers to the assessment of risk, and the comparison of this risk with the amount of time, money and resources needed to address it. It is used throughout the healthcare system and is particularly important when it comes to radiology.When assessing whether a risk is ALARP, it is essential to compare the measures being proposed with those that would normally be used, also known as “good practice”. Good practice is decided upon after detailed discussion with stakeholders. However, good practice is not always enough, and if an issue is particularly complicated, or if no good practice has yet been formulated for the issue, it is often necessary to revert back to the “first principle”. In sum, ALARP is about calculating the amount of risk attached to measures, and assessing how difficult, in terms of resources, controlling this risk is. It offers those who use it a great deal of flexibility, as it involves the setting of goals, thus allowing room to manoeuvre if necessary.
Risk management allows radiologists to focus on measures for reducing potential risk. This ensures that medical staff follow appropriate and relevant protocols and guidelines to reduce risk in radiology departments[14].
Recent studies on malpractice suits[15] revealed that amongst the most frequent causes of legal claims against radiology professionals were: diagnostic errors followed by procedural complications, poor communication with the referring doctor and poor physician-patient rapport[16]. Risk management is a crucial instrument in preventing and limiting adverse events and errors in medical settings[17].
The most common medical errors encountered in malpractice suits are vascular injuries and complications after needle biopsies in interventional radiology[18], missed or delayed cancer diagnosis especially in imaging of the breast[19] and missing diagnosis in skeletal radiology[17]. A major objective in risk management is the reduction of litigation and the associated costs. The magnitude of these costs should suffice to argue that avoiding the problems that may cause lawsuits positively impacts the patients and radiologists[20].
The reduction of errors in a radiology department is attainable if all parties in the department are aware of and up to date with all the methods and protocols involved in risk reduction[21].
One can manage litigation risk in a radiology department through a number of approaches. Healthcare professionals should set up and follow high standards of care, employ prudence when using devices off label[22,23], improve communication skills with colleagues and patients[24] and obtain professional liability insurance.
Stakeholders, including radiologists, must possess competence and significant knowledge and skills in working with all the implements within the radiology department as a way of reducing the number of errors[25]. Every radiologist should be conscious of error sources, particularly those typically constituting origins of litigation[26]. Medical staff must unveil and emphasise error pitfalls to prevent the recurrence of inaccuracies[27].
In the future, various factors will shape radiological malpractice: the emergence of new imaging techniques, innovation in image processing, new protocols scientific societies publish and guidelines professional organisations delineate[28]. To minimise risk, medical staff should cultivate a safety culture in every radiology department and perceive feedback on a possible error as a learning experience[29]. The radiologists and other key players in the department need to understand that their practice and performance significantly contribute to the trust patients place in them[30]. Radiologists need to provide good standards of practice and care and show respect for a patient[31].
Disclosing radiological errors to patients stands out as the most demanding challenge a radiologist may encounter. With a misguided error disclosure approach, radiologists risk not meeting professional norms in addition to creating erratic and unsafe practice patterns[32].
Failure to acknowledge responsibility and achieve transparency around errors subverts patient safety. Despite this, risk management concerns about litigation have long precluded the endorsement of standards around error disclosure. More recently, risk managers have emphasised that clear disclosure after radiological errors is crucial to risk management and can reduce exposure to liability[33].
Medical practitioners in the department must ensure that they keep their knowledge and skills updated. To achieve competencies and proficiency in their areas of expertise, radiologists must perform their duties within the limits of their understanding and competence[34]. This allows them to do what they understand best, thus reducing the probability of causing danger, harm or injury to patients[8]. The requirement is closely related to the recommendation that the radiologists need to maintain high trust and confidentiality with their clients through the establishment of a professional relationship[35]. Moreover, workers attain competence in a medical setting if they comprehend and appreciate the benefits of collaborating with other professionals in their field[36]. This implies that to reduce risk in radiology departments, doctors need to work as a team, combine their knowledge and skills and, more importantly, share their experience as a way of promoting excellence in their field[37].
Modern radiology is greatly reliant on the application of state-of-the-art diagnostic and therapeutic devices, but such state-of-the-art technology carries risk. To avoid the risk associated with the use of faulty devices in the radiology sector, quality assurance departments must be diligent in ensuring that all the equipment used is in good condition and of high quality[38].
Risk management relating to the use of therapeutic devices requires all professionals to possess sufficient knowledge, skills and technical ability to operate the devices, recognise when they break down and identify inaccurate results.
Through integration of appropriate skills and operational strategies in radiology, professionals can guarantee the highest accuracy. The attainment of excellent results and a foolproof reporting procedure highlights a department’s competence, indicating the department’s use of protocols and guidelines focused on reducing operational and decisional risk[39].
Integrated teamwork among radiologists would support risk reduction and prevent any issue that may cause harm or injury to patients through inadequate reporting, resulting in unreliable results[40]. Radiologists must justify their individual decisions and actions. To be able to manage risk in the radiology sector, practitioners need to learn from previous mistakes and, more importantly, scrutinise critical clinical situations and near misses. Physicians are prone to making errors, but integrating certain operational decisions and measures would reduce the rate of errors and near misses[41].
Risk management is founded on the idea that mistakes happen and processes and procedures sometimes go wrong. Therefore, holding regular meetings where medical staff can report and evaluate discrepancies, errors and near misses is crucial[42]. Discrepancy meetings are invaluable in medical practice and offer the opportunity to assess current practice and highlight areas that might need improvement[11]. The Royal College of Radiologists recommends that all radiologists attend discrepancy meetings and morbidity and mortality meetings. Evidence of attendance may be required to support the revalidation process, so doctors should carry out personal reflections[43]. Inappropriate conduct, such as unethical handling of a patient’s records and intentional carelessness, is a contributing factor to errors. However, medical staff can mitigate this factor through adherence to department and/or organisational procedures and protocols[39].
The field of radiology is rapidly evolving due to technological advances and the globalisation of healthcare. This ongoing development greatly affects the quality of care and service delivery. Doctors and professional organisations should display initiative and oversee and tackle challenging conditions in an effective manner to safeguard patient safety and standards of care. The quality of a radiological report relies on the various important steps outlined above. The essence of risk management is to survey all potential reasons for an inaccurate report in advance so that procedures can be put in place to prevent them. More importantly, the medical organisation offering radiology services needs to allow innovation and responsive measures that can improve radiology. Thus, risk management in radiology is essential in protecting the patients, radiologists and medical organisation (i.e., protecting the organisation’s capital and its reputation with patients).
| 1. | Messano GA, De Bono V, Di Folco F, Marsella LT. Past and present of risk management in healthcare. Ig Sanita Pubbl. 2014;70:423-430. [PubMed] |
| 2. | Robinson PJ, Wilson D, Coral A, Murphy A, Verow P. Variation between experienced observers in the interpretation of accident and emergency radiographs. Br J Radiol. 1999;72:323-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 117] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 3. | Nitrosi A, Bertolini M, Sghedoni R, Notari P, Pattacini P, Corazza A, Iori M. RIS-PACS, patient safety, and clinical risk management. Radiol Med. 2015;120:498-503. [PubMed] |
| 4. | Orders AB, Wright D. Expanding the scope of practice for radiology managers: radiation safety duties. Radiol Manage. 2003;25:40-47. [PubMed] |
| 5. | Paterick TE. Risk management principles for physicians. J Med Pract Manage. 2014;29:216-218. [PubMed] |
| 6. | Olisemeke B, Chen YF, Hemming K, Girling A. The effectiveness of service delivery initiatives at improving patients’ waiting times in clinical radiology departments: a systematic review. J Digit Imaging. 2014;27:751-778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Gunderman R. Teleradiology: The Importance of Communication. Virtual Mentor. 2014;16:960-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Mendiratta-Lala M, Eisenberg RL, Steele JR, Boiselle PM, Kruskal JB. Quality initiatives: measuring and managing the procedural competency of radiologists. Radiographics. 2011;31:1477-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Lau L. Leadership and management in quality radiology. Biomed Imaging Interv J. 2007;3:e21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | The European Society of Radiology. Risk management in Radiology in Europe. Available from: http://www.myesr.org/html/img/pool/ESR_2006_IV_Riskmanagement_Web.pdf. |
| 11. | Chakraverty S, Wright J. Adverse events in British hospitals. “Errors meetings” in radiology did not identify errors leading to complaints and litigation. BMJ. 2001;322:1425-1426; author reply 1427. [PubMed] |
| 12. | Bruno MA, Nagy P. Fundamentals of quality and safety in diagnostic radiology. J Am Coll Radiol. 2014;11:1115-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 13. | Kruskal JB, Eisenberg R, Sosna J, Yam CS, Kruskal JD, Boiselle PM. Quality initiatives: Quality improvement in radiology: basic principles and tools required to achieve success. Radiographics. 2011;31:1499-1509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | The Royal College of Radiologists. Good practice guide for clinical radiologists. Available from: http://www.rcr.ac.uk/docs/radiology/pdf/BFCR(12)1_GoodPractice.pdf. |
| 15. | Halpin SF. Medico-legal claims against English radiologists: 1995-2006. Br J Radiol. 2009;82:982-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Wallis A, McCoubrie P. The radiology report--are we getting the message across? Clin Radiol. 2011;66:1015-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Cannavale A, Santoni M, Mancarella P, Passariello R, Arbarello P. Malpractice in radiology: what should you worry about? Radiol Res Pract. 2013;2013:219259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Mavroforou A, Giannoukas A, Mavrophoros D, Michalodimitrakis E. Physicians’ liability in interventional radiology and endovascular therapy. Eur J Radiol. 2003;46:240-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | van Breest Smallenburg V, Setz-Pels W, Groenewoud JH, Voogd AC, Jansen FH, Louwman MW, Tielbeek AV, Duijm LE. Malpractice claims following screening mammography in The Netherlands. Int J Cancer. 2012;131:1360-1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Berlin L. Radiologic errors and malpractice: a blurry distinction. AJR Am J Roentgenol. 2007;189:517-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 80] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Cannavale A, Santoni M, Passariello R, Arbarello P. Risk management in radiology. Radiol Manage. 2013;35:14-19; quiz 20-21. [PubMed] |
| 22. | Zvavanjanja RC, Odetoyinbo TO, Rowlands PC, Healey A, Abdelsalam H, Powell S, Evans JC, Hughes ML, Gould DA, McWilliams RG. Off label use of devices and drugs in interventional radiology. Clin Radiol. 2012;67:239-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Society of Interventional Radiology. SIR Policy on Off-Label Use. Available from: http://www.sirweb.org/clinical/cpg/SIR_Off-label_use_statement11-18-07.pdf. |
| 24. | Gunderman RB, Brown BP. Teaching interpersonal and communication skills. Acad Radiol. 2012;19:1589-1590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Whang JS, Baker SR, Patel R, Luk L, Castro A. The causes of medical malpractice suits against radiologists in the United States. Radiology. 2013;266:548-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 143] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 26. | Baker SR, Whang JS, Luk L, Clarkin KS, Castro A, Patel R. The demography of medical malpractice suits against radiologists. Radiology. 2013;266:539-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | The Royal College of Radiologists. Standards for the NPSA and RCR Safety Checklist for Radiological Interventions. London: The Royal College of Radiologists 2010; . |
| 28. | Sokol DK. Law, ethics, and the duty of care. BMJ. 2012;345:e6804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Pinto A, Brunese L. Spectrum of diagnostic errors in radiology. World J Radiol. 2010;2:377-383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 144] [Cited by in RCA: 128] [Article Influence: 8.0] [Reference Citation Analysis (5)] |
| 30. | Quinn MA, Wilcox A, Orav EJ, Bates DW, Simon SR. The relationship between perceived practice quality and quality improvement activities and physician practice dissatisfaction, professional isolation, and work-life stress. Med Care. 2009;47:924-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 31. | Kaldjian LC, Jones EW, Wu BJ, Forman-Hoffman VL, Levi BH, Rosenthal GE. Disclosing medical errors to patients: attitudes and practices of physicians and trainees. J Gen Intern Med. 2007;22:988-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 109] [Article Influence: 5.7] [Reference Citation Analysis (3)] |
| 32. | Hannawa AF. “Explicitly implicit”: examining the importance of physician nonverbal involvement during error disclosures. Swiss Med Wkly. 2012;142:w13576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 33. | Brown SD, Lehman CD, Truog RD, Browning DM, Gallagher TH. Stepping out further from the shadows: disclosure of harmful radiologic errors to patients. Radiology. 2012;262:381-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287:226-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1587] [Cited by in RCA: 1390] [Article Influence: 57.9] [Reference Citation Analysis (0)] |
| 35. | Gunderman RB, Beckman ES. Confidentiality: an essential element of professionalism. AJR Am J Roentgenol. 2012;199:W683-W685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 36. | Alkasab TK, Harvey HB, Gowda V, Thrall JH, Rosenthal DI, Gazelle GS. Consensus-oriented group peer review: a new process to review radiologist work output. J Am Coll Radiol. 2014;11:131-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Chandy J, Goodfellow T, Vohrah A. Clinical governance in action: radiology. Hosp Med. 2000;61:326-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 38. | European Society of Radiology (ESR). Renewal of radiological equipment. Insights Imaging. 2014;5:543-546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 39. | Association of Healthcare Technology Providers for Imaging, Radiotherapy and Care. Declining investment in Radiology Equipment stores up problems for the NHS. Available from: http://www.axrem.org.uk/Axrem_Editorial_on_Stats_11th_October_2013_FINAL.pdf. |
| 40. | The Royal College of Radiologists. Specialty standards and supporting information for revalidation. London: The Royal College of Radiologists 2010; . |
| 41. | Driscoll DO, Halpenny D, Guiney M. Radiological error--an early assessment of departmental radiology discrepancy meetings. Ir Med J. 2012;105:172-174. [PubMed] |
| 42. | Brady A, Laoide RÓ, McCarthy P, McDermott R. Discrepancy and error in radiology: concepts, causes and consequences. Ulster Med J. 2012;81:3-9. [PubMed] |
| 43. | The Royal College of Radiologists. Personal reflection on discrepancies and adverse events. London: The Royal College of Radiologists 2010; . |
P- Reviewer: Chen F, Kilickesmez O, Kara PO S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/