Published online Apr 28, 2023. doi: 10.4329/wjr.v15.i4.118
Peer-review started: December 27, 2022
First decision: February 21, 2023
Revised: February 28, 2023
Accepted: March 24, 2023
Article in press: March 24, 2023
Published online: April 28, 2023
Processing time: 120 Days and 17.6 Hours
The data obtained on the anatomical knowledge of the tracheobronchial system can be used for diagnosis, treatment and interventional interventions in areas such as anesthesia, thoracic surgery, pulmonary physiology.
To determine the tracheobronchial branching angles in pediatric and adult populations by using the multislice computed tomography (CT) and minimum intensity projection (MinIP) technique, which is a non-invasive method.
Our study was carried out retrospectively. Patients who underwent contrast and non-contrast CT examination, whose anatomically and pathophysiologically good tracheobronchial system and lung parenchyma images were obtained, were included in the study. Measurements were made in the coronal plane of the lung parenchyma. In the coronal plane, right main bronchus-left main bronchus angle, right upper lobe bronchus-intermedius bronchus angle, right middle lobe bronchus-right lower lobe bronchus angle, left upper lobe bronchus-left lower lobe bronchus angle were measured.
The study population consisted of 1511 patients, 753 pediatric (mean age: 13.4 ± 4.3; range: 1-18 years) and 758 adults (mean age: 54.3 ± 17.3; range: 19-94 years). In our study, tracheal bifurcation angle was found to be 73.3° ± 13.7° (59.6°-87°) in the whole population. In the pediatric group, the right-left main coronal level was found to be higher in boys compared to girls (74.6° ± 12.9° vs 71.2° ± 13.9°, P = 0.001). In the adult group, the right-left main coronal level was found to be lower in males compared to females (71.9° ± 12.9° vs 75.8° ± 14.7°, P < 0.001).
Our study, with the number of 1511 patients, is the first study in the literature with the largest number of patient populations including pediatric and adult demographic data, measuring the angle values of the tracheobronchial system using multislice CT and MinIP technique. Study data will not only be a guide during invasive procedures, but it can also guide studies to be done with imaging methods.
Core Tip: This study is one of the rare studies with the highest number of patient population and measurement values in the literature measuring the branching angles of the tracheobronchial tree using the minimum intensity projection technique with multislice computed tomography in pediatric and adult populations. In this study, a wide variety of branching angles of the tracheal bronchial tree, which were not reported in the literature, were reported. Anatomical knowledge of the tracheobronchial system is essential during the use of interventional fiberoptic bronchoscopy during various airway devices, intubation, airway maneuvers. These results guide interventional procedures and offer new methods for future studies.
- Citation: Kahraman Ş, Yazar MF, Aydemir H, Kantarci M, Aydin S. Detection of tracheal branching with computerized tomography: The relationship between the angles and age-gender. World J Radiol 2023; 15(4): 118-126
- URL: https://www.wjgnet.com/1949-8470/full/v15/i4/118.htm
- DOI: https://dx.doi.org/10.4329/wjr.v15.i4.118
Trachea is a cylindrical flexible tube that provides air passage between the larynx and the lung. Trachea bifurcation angle, it is measured by the interbronchial angle, which is the angle measured at the intersection of the central axes of the right and left main bronchus, or by the subcarinal angle, which is the angle at the intersection of the lower borders of the right and left main bronchus. Many cardiac and mediastinal pathologies can cause changes in tracheal bifurcation angle[1-4].
Examination of the tracheobronchial tree can be done with invasive and noninvasive methods such as bronchoscopy, bronchograms, computed tomography (CT), magnetic resonance imaging[2,3,5]. Most previous studies measured the subcarinal angle on chest radiographs using a goniometer[6,7]. Helical CT provides volumetric imaging of chest films and accurate measurement of the subcarinal angle at a workstation using the minimum intensity projection (MinIP) technique. Because the MinIP technique uses all the data in the volume of interest to create a one/two-dimensional image, it is a technique that enables the visualization of structures of low density (e.g. air) at this level. This technique allows us to accurately measure the subcarinal angle compared to the coronal multiplane reconstructed image[3,8].
Anatomical knowledge of the tracheobronchial system is essential when using interventional fiberoptic bronchoscopy during various airway devices (e.g., double-lumen endobronchial tube), intubation, airway maneuvers, airway reconstruction, and tracheobronchial tumor resection[9,10].
Previous studies were insufficient for the pediatric population[11-14]. In 2018, Fernandes et al[3] found the mean subcarinal angle of 69.75° ± 3.38° (range 66.37°-73.13°) in the measurements made with thorax CT and MinIP technique on 193 patients aged 20-60 years. Parry et al[5] in the measurements made with thorax CT and MinIP technique on 552 patients aged 9-85 years in 2019, they found the mean subcarinal angle to be statistically significantly larger in women than in men (78.90° ± 11.04° vs 67.60° ± 14.55°, P < 0.05). In 2018, Fernandes et al[3] and Parry et al[5] although the measurement methods are similar in his studies in 2019, the number of patients and measurement parameters are limited. In addition, the relationship between age and gender and the subcarinal angle was not clarified.
The aim of our study is to determine the tracheobronchial branching angles in pediatric and adult individuals with a high sample size population by using the multislice CT and MinIP technique, which is a non-invasive method, and to eliminate the above-mentioned literature deficiencies.
Our institutional review board gave its approval to this retrospective study. Ethics committee did not require informed consent, as our study was retrospective.
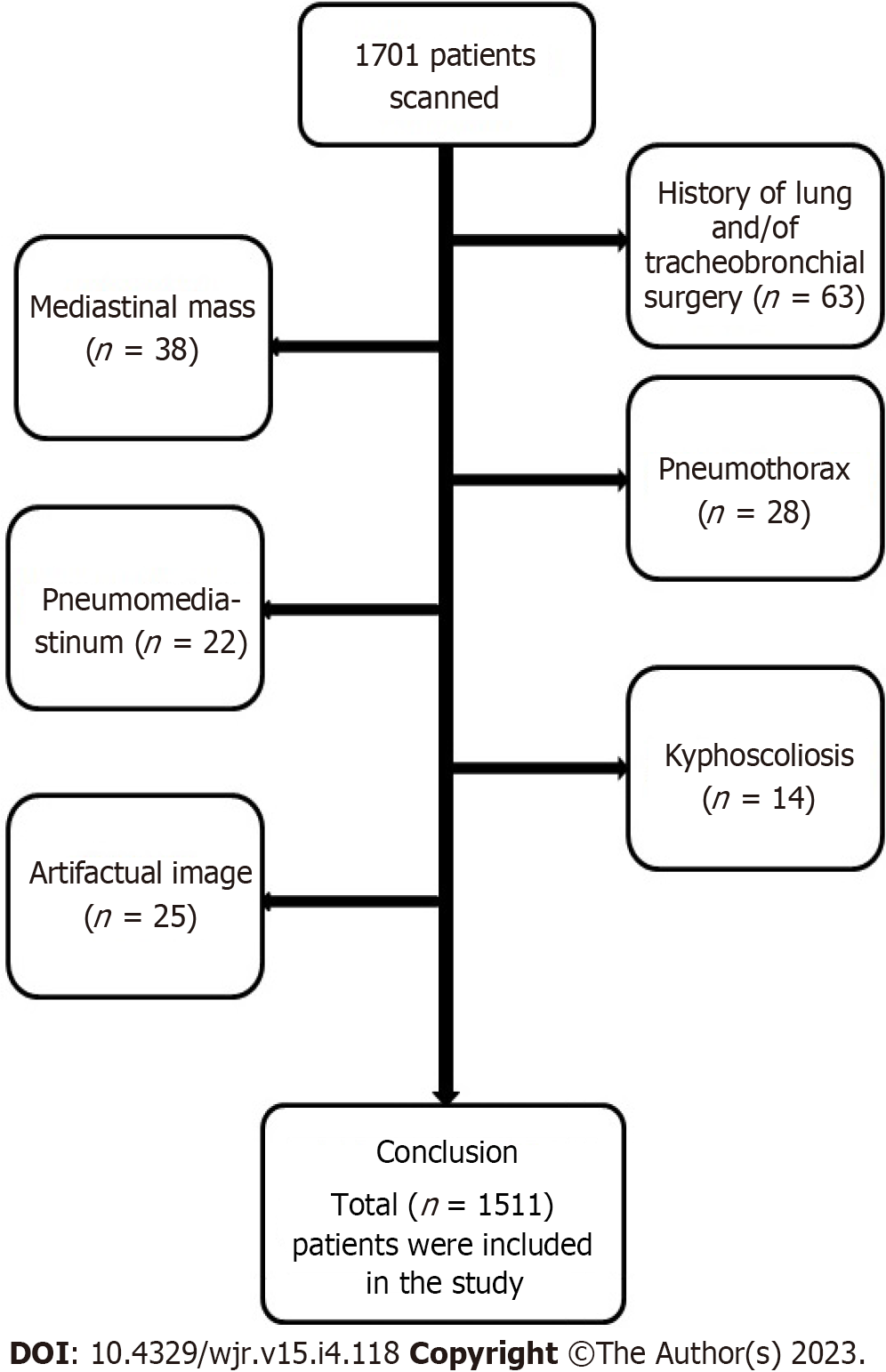
A total of 1511 patients, including 753 pediatrics and 758 adults, were included in our study, (patients who do not obey breath commands enough to prevent image formation, tracheobronchial surgery or tracheal intubation history), patients with pneumothorax, pneumomediastinum as a result of trauma, patients with pathology that may cause mediastinal changes (mediastinal mass, mediastinal LAP, severe cardiomegaly), musculoskeletal deformity patients (scoliosis, kyphosis) and patients with diaphra
Patients who were unable to obtain good image quality (for example, those who were unable to hold their breath or who had motion artifacts) were excluded from the study. Thoracic CT scans were also performed in pediatric patients of all ages in order to produce the best image in the shortest amount of time. Images with poor image quality and coinciding with the expiratory phase were excluded from the study.
In our study, people with diseases that disrupt the anatomy and physiology of the tracheobronchial system, infective or inflammatory processes, lung cancer, significant pneumonia or collapse, and respiratory system diseases in all patient groups (adults and children) were not included in the study.
Inclusion criteria for the study; excluding the exclusion criteria, the tracheobronchial system and lung parenchyma images of the anatomically and pathophysiologically good quality were obtained in patients who underwent CT with or without contrast for any reason (Figure 1).
This study consists of contracted and non-contrast thoracic CT examinations with a double tube 256 slice Somatom Definition Flash device (Siemens Healthcare, Forchheim, Germany). The images of the patients were evaluated using the Siemens Somatom Sensation-Syngo via software program from the PACS (Picture Archiving Communication System) archive on coronal planes and using the MinIP technique.
Shooting parameters and lung parenchyma images were obtained by adjusting tube voltage 120 kV, automatic tube current modulation 100-250 mAs, section thickness 1.25 mm, pitch 1.4, gantry rotation time 0.5-1 sec, FOV 455 mm. Images were acquired with adequate inspiration and in the supine position. In contrast-enhanced thorax shots, the dose was administered by administering a total of 100-120 mL of contrast material at a rate of 4 mL/sec.
Then, the images in the PACS system were measured in the coronal plane using the 25 mm MinIP technique in the Siemens (Syngo.via, Siemens Healthineers, Erlangen, Germany) software program.
Measurements were taken by 2 independent radiologists and verified by a partner radiologist. All radiologists then reviewed any discrepancies between the measurements. All investigators were blind to the age of the patients until the measurements were analysed.
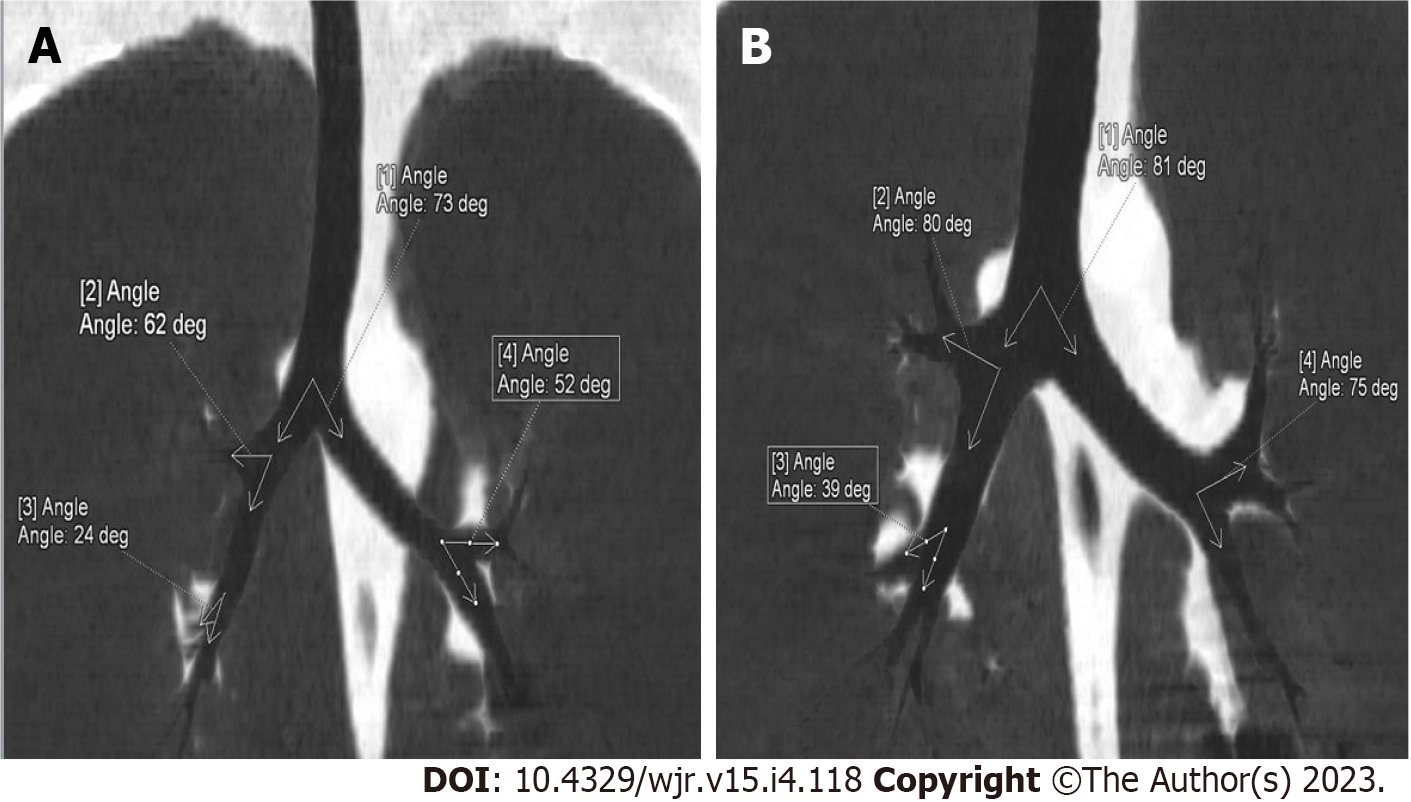
At the same time, demographic data (age, gender) of the patients were recorded. Measurements were made using the 25 mm MinIP technique obtained in the lung parenchyma window in the coronal plane via program. Right main bronchus-left main bronchus angle, right upper lobe bronchus-intermedius bronchus angle, right middle lobe bronchus-right lower lobe bronchus angle, left upper lobe bronchus-left lower lobe bronchus angle measurements were made in the coronal plane. It was measured as the angle at the junction of the line passing through the center of the bronchi on the long axis (Figure 2).
A data visualization technique called MinIP makes it possible to find low-density structures in a given volume. The algorithm projects the voxel with the lowest attenuation value across all views in the volume onto a 2D image, using all the data in the volume of interest to create a single bidimensional image.
Right main bronchus-left main bronchus angle (interbronchial angle) right left main coronal, right upper lobe bronchi-intermedius bronchus angle right upper-intermedius (coronal), right middle lobe bronchus-right lower lobe bronchus angle right middle-lower (coronal), left upper lobe bronchus-left lower lobe bronchial angle is abbreviated as left upper-lower (coronal).
Statistical analyses of collected data were conducted using IBM SPSS Statistics for Windows 20.0 (IBM Corp., Armonk, NY, USA). Determination of the normally distributed data was conducted using the Kolmogorov-Smirnov test. Numerical variables that had normal distribution were expressed as the mean ± SD, while those with non-normal distribution were expressed as the median (min-max). The categorical variables were expressed as numbers and percentages. For comparisons between groups, the Student T test or Mann-Whitney U test were used according to normality distribution. Categorical variables were expressed as numbers and percentages, and comparisons between groups were evaluated with Chi-square and Fisher's Exact tests. Spearman correlation analysis was used for the relationship between age and angels. P < 0.05 was taken as statistical significance.
The study population was 753 pediatrics (49.5%) (mean age: 13.4 ± 4.3 years; range: 1-18 years) and 758 adults (mean age: 54.3 ± 17.3 years; range: 19-94 years) consisted of 1511 patients. Gender distributions were similar in pediatric and adult patient groups. Right-left main coronal, right upper-intermedius coronal and left upper-lower coronal levels did not differ in pediatric and adult patient groups, right middle-lower coronal levels were found to be lower in the pediatric group compared to the adult group (36.9 ± 12.2 vs 42 .4 ± 12.3, P < 0.001) (Table 1).
| Variables (coronal) | Whole population, n = 1511 | Pediatric group, n = 753 | Adult group, n = 758 | P |
| Age (year) | 34.0 ± 24.0 | 13.4 ± 4.3 | 54.3 ± 17.3 | < 0.001 |
| Gender n (%) | ||||
| Male | 755 (50.0) | 371 (49.3) | 384 (50.7) | 0.589 |
| Female | 756 (50.0) | 382 (50.7) | 374 (49.3) | |
| Right-left main | 73.3 ± 13.7 | 72.9 ± 13.5 | 73.8 ± 13.9 | 0.190 |
| R upper-intermedius | 69 ± 12.8 | 69.7 ± 12.4 | 68.4 ± 13.2 | 0.062 |
| R middle-lower | 39.7 ± 12.5 | 36.9 ± 12.2 | 42.4 ± 12.3 | < 0.001 |
| L upper-lower | 58.4 ± 12.8 | 58.8 ± 12.8 | 57.9 ± 12.8 | 0.191 |
In the pediatric group, the right-left main coronal level was found to be higher in boys compared to girls (74.6 ± 12.9 vs 71.2 ± 13.9, P = 0.001), right upper-intermedius coronal, left upper-lower coronal, and right middle-lower coronal levels did not differ significantly in the pediatric group by gender (Table 2).
| Variables (coronal) | Pediatric, n = 753 | P | Adult, n = 758 | P | ||
| Male, n = 371 | Female, n = 382 | Male, n = 384 | Female, n = 374 | |||
| Age (year) | 13.1 ± 4.5 | 13.7 ± 4.1 | 0.055 | 53.4 ± 17.3 | 55.3 ± 17.4 | 0.117 |
| Right-left main | 74.6 ± 12.9 | 71.2 ± 13.9 | 0.001 | 71.9 ± 12.9 | 75.8 ± 14.7 | < 0.001 |
| R upper-intermedius | 68.8 ± 11.9 | 70.5 ± 12.7 | 0.067 | 68.7 ± 13 | 68.2 ± 13.4 | 0.563 |
| R middle-lower | 37.2 ± 11.9 | 36.6 ± 12.5 | 0.568 | 42.1 ± 12.1 | 42.8 ± 12.4 | 0.435 |
| L upper-lower | 58.7 ± 13.3 | 58.9 ± 12.4 | 0.790 | 58.3 ± 11.9 | 57.5 ± 13.7 | 0.379 |
In the adult group, the right-left main coronal level was found to be lower in males compared to females (71.9 ± 12.9 vs 75.8 ± 14.7, P < 0.001), right upper-intermedius coronal, left upper-lower coronal and right middle-lower coronal levels did not differ significantly by gender in the adult group (Table 2).
As the age increases, the tracheal bifurcation angle passing through the central axes of the right main bronchus and the left main bronchus in the coronal plane and the angle of the right middle lobe bronchus and right lower lobe bronchus in the coronal plane increase statistically significantly (Table 3).
| Variables (coronal) | r | P |
| Right-left main | 0.064 | 0.014 |
| R upper-intermedius | -0.098 | <0.001 |
| R middle-lower | 0.167 | <0.001 |
| L upper-lower | -0.070 | 0.007 |
While there are many studies evaluating the tracheal bifurcation angle with cadaver studies and chest radiographs, there are limited studies evaluating using CT. However, it was not detected except in the study conducted by Fernandes et al[3], in which 193 patients reported using CT with the MinIP technique were examined. In addition, our study Mi et al[9] except for the measurements made with thorax CT and MPR technique on 2107 patients aged 18-89 years in 2015, it has a larger patient population than previous studies in the literature measuring the angle values of the tracheobronchial system.
Our study is a study with the largest number of patient population in our country, which measures the angle values of the tracheobronchial system using multislice CT and MinIP technique, which is a noninvasive method, and includes both pediatric and adult demographic data.
Tracheal bifurcation angle, it is measured by the interbronchial angle, which is the angle measured at the intersection of the central axes of the right and left main bronchus, or by the subcarinal angle, which is the angle at the intersection of the lower borders of the right and left main bronchus[4]. In our study, we measured the tracheal bifurcation angles by measuring the interbronchial angle. The normal values of the tracheal bifurcation angle range from 40° to 99°, with an average value of 60°–65°[11]. In our study, we found the tracheal bifurcation angle of 73.3° ± 13.7° (range 59.6°-87°).
Karabulut et al[11] in 2005, found the mean interbronchial angle of 77° ± 13° in a study that measured the tracheal bifurcation angle with helical CT performed on 120 patients aged 17-85 years.
The results of our study showed similar results with Karabulut et al[11] study and literature. The tracheal bifurcation angle may widen due to various mediastinal and cardiac pathologies, for example (subcarinal mass, lobar collapse, left atrial enlargement, generalized cardiomegaly, pericardial effusion)[4,15]. Tracheal bifurcation angle may decrease after pulmonary lobectomy[16]. Therefore, since the tracheal bifurcation angle is in a wide range and may change due to mediastinal and cardiac pathologies, diseases with mediastinal and cardiac pathologies and disrupting the anatomy and physiology of the tracheobronchial system were not included in our study. In our study, measurements were made during the inspiration phase because the tracheal bifurcation angle narrows due to the downward extension of the lungs in inspiration and expands with upward displacement of the lungs in expiration[3].
The first studies measuring the tracheal bifurcation angle (interbronchial angle) were made towards the end of the 19th century by Kamel et al[17] on cadavers and found the average angle of 70°[10,17]. Adriani et al[10] found the average tracheal bifurcation angle (interbronchial angle) of 110° in infantar. Kubota et al[12] found the tracheal bifurcation angle of 80° on average using chest radiography in their study on infants and children aged 0-13 years. Alavi et al[13] in their study of children up to 16 years of age, they found the tracheal bifurcation angle to range from 52° to 78° using chest radiography.
Ulusoy et al[14] in their study using multislice CT, found that the right bronchial angle was smaller than the left in their study in the 0-18 age range. Ulusoy et al[14] calculated the mean right subcarinal angle as 34.5º ± 8.1º degrees and the mean left subcarinal angle as 38.1º ± 8.9º. Although the mean right and left subcarinal angles were not significant in all age groups except the 0-18 age group, they were measured higher in women than in men[14]. In our study, the tracheal bifurcation angle, which is the sum of the right subcarinal angle and the left subcarinal angle, was used and our method was similar. In our study, the tracheal bifurcation angle passing through the central axes of the right main bronchus and left main bronchus in the coronal plane was found to be statistically significantly higher in boys compared to girls in our study (74.6º ± 12.9º vs 71.2º ± 13.9º, P = 0.001). The high number of cases and measurement parameters in our study suggest that our study is more reliable. The angle of the right upper lobe bronchus and the right intermedius bronchus in the coronal plane, the angle of the left upper lobe bronchus and the left lower lobe bronchus in the coronal plane, and the angle values of the right middle lobe bronchus and the right lower lobe bronchus in the coronal plane are the first measurements in the literature using the MinIP technique. However, no significant differentiation was deceted for these measurements.
Karabulut et al[11] in 2005, the mean interbronchial angle was 77° ± 13° and the mean subcarinal angle was 73° ± 16° in the study of 120 patients aged 17-85 years, measuring the tracheal bifurcation angle with helical CT. They found an excellent correlation between the interbronchial angle and the subcarinal angle (r = 0.88, P < 0.001). They found that the interbronchial angle and subcarinal angle, which are tracheal bifurcation angles, were statistically significantly larger in females compared to males[11].
Murray et al[7] reported higher interbronchial and subcarinal angles in female patients in the measurements made using chest radiography on 122 patients with an age range of 27-85 years, but they were not statistically significant. Karabulut et al[11] study conducted in 2005 and our study contradicts previous studies measuring the tracheal bifurcation angle with chest radiography, which reported that the angle of tracheal bifurcation was independent of gender[13,18,19]. Measurements with CT can be considered to be more reliable and accurate since it is possible to evaluate the anatomy of the tracheobronchial system in multiplanar (axial, sagittal and coronal) planes.
Mi et al[9] found the subcarinal angle, known as the sum of the right bronchial angle and the left bronchial angle, to be statistically significantly larger in women than in men, in the measurements made using thorax CT and MPR techniques on 2107 patients aged 18-89 years in 2015, similar to our study (80.1° ± 13.4° vs 75.1° ± 13.4°).
Khade et al[2] in 2016, found the mean subcarinal angle of 79.92° ± 11.6° (range 68.32°-91.52°) in 110 patients aged 10-70 years, measuring the subcarinal angle with thorax CT. Khade et al[2] in contrast to our study, found the subcarinal angle to be statistically insignificantly larger in men than in women (80.01° ± 12.53° vs 79.75° ± 9.99°, P = 0.902).
In 2018, Fernandes et al[3] found the mean subcarinal angle of 69.75° ± 3.38° (range 66.37° - 73.13°) in the measurements made with thorax CT and MinIP technique on 193 patients aged 20-60 years. Fernandes et al[3] found the subcarinal angle to be statistically insignificantly larger in women than in men (69.90° ± 4.07° vs 69.63° ± 2.75°, P = 0.589). Fernandes et al[3] found the mean subcarinal angle to be statistically significantly greater in the 20-40 age group than in the 41-60 age group (70.38° ± 3.85° vs 69.25° ± 2.88°, P = 0.02).
In a study by Kamel et al[17] in 2009 on tracheal morphology with CT and cadaver dissection, they found the mean subcarinal angle on thorax CT of 60 patients to be greater in women than in men (81° ± 20° vs 76° ± 20°).
Parry et al[5] in the measurements made with thorax CT and MinIP technique on 552 patients aged 9-85 years in 2019, they found the mean subcarinal angle to be statistically significantly greater in women than in men, similar to our study (78.90° ± 11.04° vs 67.60° ± 14.55°, P < 0.05).
In the current study, we measured the branching angles of the tracheobronchial tree (tracheal bifurcation angle passing through the central axes of the right main bronchus and left main bronchus in the coronal plane, the angle of the right upper lobe bronchus and the right intermedius bronchus in the coronal plane, the angle of the right middle lobe bronchus and the right lower lobe bronchus, the angle of the left upper lobe bronchus and the left lower lobe bronchus in the coronal plane) in both adult and pediatric patients. This study is one of the rare studies in the literature with the highest number of patient population and different measurement angles.
The data of other studies examining the relationship between age and tracheobronchial angle are contradictory. In 2018, Fernandes et al[3] found the mean subcarinal angle in the 20-40 age group statistically significantly higher than the 41-60 age group in the measurements made with thorax CT and MinIP technique on 193 patients with an age range of 20-60 years (70.38° ± 3.85° vs 69.25° ± 2.88°, P = 0.02). Khade et al[2] in 2016, in a study that measured the subcarinal angle with thorax CT on 110 patients with an age range of 10-70 years, they did not find any correlation with age and gender. Chunder et al[20] in his study conducted in 2015 on 60 cadaver specimens, the mean subcarinal angles in the 0–15 years, 16–25 years, 26–40 years, 41–55 years, and > 55 age groups were 61.4°, 52.9°, 49.2°, 48.2° and 48.2° in women, respectively; 54°, 64.3°, 56.4°, 58.4°, 57.1° and 59.5° found in males. They concluded that there was a decrease in the subcarinal angle with increasing age, except for patients aged > 55 years[20]. In our study, the trachea bifurcation angle passing through the central axes of the right main bronchus and the left main bronchus in the coronal plane, and the angle of the right middle lobe bronchus and right lower lobe bronchus in the coronal plane increase statistically with increasing age. It may have occurred due to the variability of the angle due to inspiration-expiration, various mediastinal and cardiac pathologies, measurement technique. In addition, the characteristics of the study populations such as age, gender and race may affect the results. There is a need for further studies measuring with similar methods in more standardized populations to clarify this issue.
Our study is the first study in the literature to measure the angle values of the tracheobronchial system using the multislice CT and MinIP technique with the number of 1511 patients and to have the largest patient population including both pediatric and adult demographic data. In addition, unlike previous studies, we measured all branching angles of the tracheobronchial tree and assessed their relationship with age and gender.
In our study, tracheal bifurcation angle was found to be 73.3° ± 13.7° (59.6° - 87°) in the whole population. The tracheal bifurcation angle and the angle of the right middle lobe bronchus and the right lower lobe bronchus in the coronal plane increase statistically with increasing age.
This study is one of the few in the literature that uses the minimum intensity projection (MinIP) technique with multislice computed tomography (CT) to measure the branching angles of the tracheobronchial tree in pediatric and adult populations.
Our study is the first study in the literature to measure the angle values of the tracheobronchial system using the multislice CT and MinIP technique with the number of 1511 patients and to have the largest patient population including both pediatric and adult demographic data.
Our study's objectives are to fill the gaps in the literature by measuring the tracheobronchial branching angles in a large sample size population of pediatric and adult patients using the non-invasive multislice CT and MinIP technology.
This study was carried out retrospectively. Patients who underwent contrast and non-contrast CT examination, whose anatomically and pathophysiologically good tracheobronchial system and lung parenchyma images were obtained, were included in the study. In the coronal plane, right main bronchus-left main bronchus angle, right upper lobe bronchus-intermedius bronchus angle, right middle lobe bronchus-right lower lobe bronchus angle, left upper lobe bronchus-left lower lobe bronchus angle were measured.
In our study, tracheal bifurcation angle was found to be 73.3° ± 13.7° (59.6°-87°) in the whole population. In the pediatric group, the right-left main coronal level was found to be higher in boys compared to girls. In the adult group, the right-left main coronal level was found to be lower in males compared to females.
The tracheal bifurcation angle and the angle of the right middle lobe bronchus and the right lower lobe bronchus in the coronal plane increase statistically with increasing age.
The date of this data will not only be a guide during invasive procedures, but it can also guide studies to be done with imaging methods.
| 1. | Choorat S, Totanarungroj K, Muangman N. Assessment of normal subcarinal angle on chest radiographs in adult Thai population. Siriraj Med J. 2008;60:264-266. |
| 2. | Khade B, Waheed AR, Yadav N, Diwan CV. Study of sub carinal angle of human trachea by computerized tomography. Int J Anat Res. 2016;4:2828-2832. [DOI] [Full Text] |
| 3. | Fernandes SF, Pradhan A. Estimation of subcarinal angle using minimum intensity projection in computed tomography. Asian J Pharm Clin Res. 2018;11:383-385. [DOI] [Full Text] |
| 4. | Bedair R, Iriart X. EDUCATIONAL SERIES IN CONGENITAL HEART DISEASE: Tetralogy of Fallot: diagnosis to long-term follow-up. Echo Res Pract. 2019;6:R9-R23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 5. | Parry AH, Wani AH, Shiekh Y, Gojwari TA. Determination of subcarinal angle of trachea using computed tomography. Int J Res Med Sci. 2019;7:1527. [DOI] [Full Text] |
| 6. | Lin C, Lee JH, Hsieh CM. The correlation between subcarinal angle and left atrial volume. Acta Cardiol Sin. 2012;67:15-96. |
| 7. | Murray JG, Brown AL, Anagnostou EA, Senior R. Widening of the tracheal bifurcation on chest radiographs: value as a sign of left atrial enlargement. AJR Am J Roentgenol. 1995;164:1089-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Perandini S, Faccioli N, Zaccarella A, Re T, Mucelli RP. The diagnostic contribution of CT volumetric rendering techniques in routine practice. Indian J Radiol Imaging. 2010;20:92-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 9. | Mi W, Zhang C, Wang H, Cao J, Li C, Yang L, Guo F, Wang X, Yang T. Measurement and analysis of the tracheobronchial tree in Chinese population using computed tomography. PLoS One. 2015;10:e0123177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 10. | Adriani J, Griggs TS. An improved endotracheal tube for pediatric use. Anesthesiology. 1954;15:466-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Karabulut N. CT assessment of tracheal carinal angle and its determinants. Br J Radiol. 2005;78:787-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (3)] |
| 12. | Kubota Y, Toyoda Y, Nagata N, Kubota H, Sawada S, Murakawa M, Fujimori M. Tracheo-bronchial angles in infants and children. Anesthesiology. 1986;64:374-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 29] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 13. | Alavi SM, Keats TE, O'Brien WM. The angle of tracheal bifurcation: its normal mensuration. Am J Roentgenol Radium Ther Nucl Med. 1970;108:546-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Ulusoy M, Uysal II, Kıvrak AS, Ozbek S, Karabulut AK, Paksoy Y, Dogan NU. Age and gender related changes in bronchial tree: a morphometric study with multidedector CT. Eur Rev Med Pharmacol Sci. 2016;20:3351-3357. [PubMed] |
| 15. | Dwivedi G, Mahadevan G, Jimenez D, Frenneaux M, Steeds RP. Reference values for mitral and tricuspid annular dimensions using two-dimensional echocardiography. Echo Res Pract. 2014;1:43-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (2)] |
| 16. | Kakeda S, Kamada K, Aoki T, Watanabe H, Nakata H. Postsurgical change in the tracheal bifurcation angle after upper lobectomy: radiographic evaluation. Acad Radiol. 2003;10:644-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 17. | Kamel KS, Lau G, Stringer MD. In vivo and in vitro morphometry of the human trachea. Clin Anat. 2009;22:571-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Haskin PH, Goodman LR. Normal tracheal bifurcation angle: a reassessment. AJR Am J Roentgenol. 1982;139:879-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Coppola V, Vallone G, Coscioni E, Coppola M, Maraziti G, Alfinito M, Di Benedetto G. [Normal value of the tracheal bifurcation angle and correlation with left atrial volume]. Radiol Med. 1998;95:461-465. [PubMed] |
| 20. | Chunder R, Guha R. A morphometric study of human subcarinal angle in different age groups in both sexes and its clinical implications. Indian Journal of Basic and Applied Medical Research. 2015;4:424-430. |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu Y; Shariati MBH, Iran; Tovar JA, Spain S-Editor: Liu XF L-Editor: A P-Editor: Zhao S