Copyright
©The Author(s) 2025.
World J Radiol. Oct 28, 2025; 17(10): 108804
Published online Oct 28, 2025. doi: 10.4329/wjr.v17.i10.108804
Published online Oct 28, 2025. doi: 10.4329/wjr.v17.i10.108804
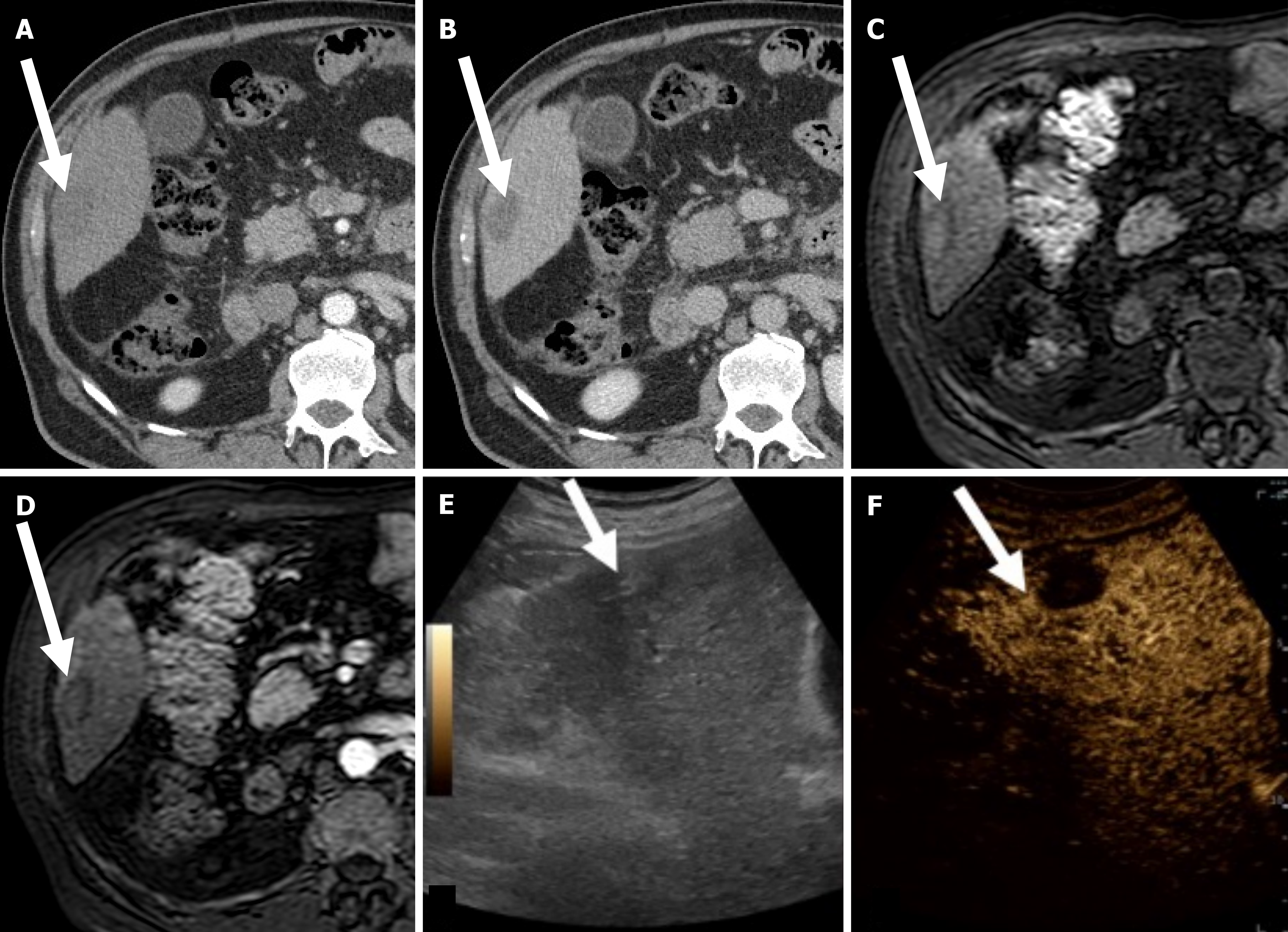
Figure 1 Successful hepatocellular carcinoma radiofrequency ablation in a 69-year-old woman with hepatitis C virus-related cirrhosis.
A: On computed tomography obtained 1 month after radiofrequency ablation (RFA) the treated area (arrow) is slightly hyperattenuating on unenhanced phase due to coagulative necrosis; B: On corresponding hepatic arterial phase (HAP) the treated area shows no enhancement; C: On magnetic resonance imaging (MRI) obtained 2 months after RFA the treated area is slightly hyperintense on unenhanced T1-weighted image due to coagulative necrosis; D: On corresponding HAP the treated area shows no enhancement; E: On gray-scale ultrasound image obtained immediately after MRI the treated area is heterogeneously and slightly hyperechoic (arrow); F: Corresponding contrast enhanced ultrasound image achieved 18 seconds after injection shows no a hyperenhancement (arrow).
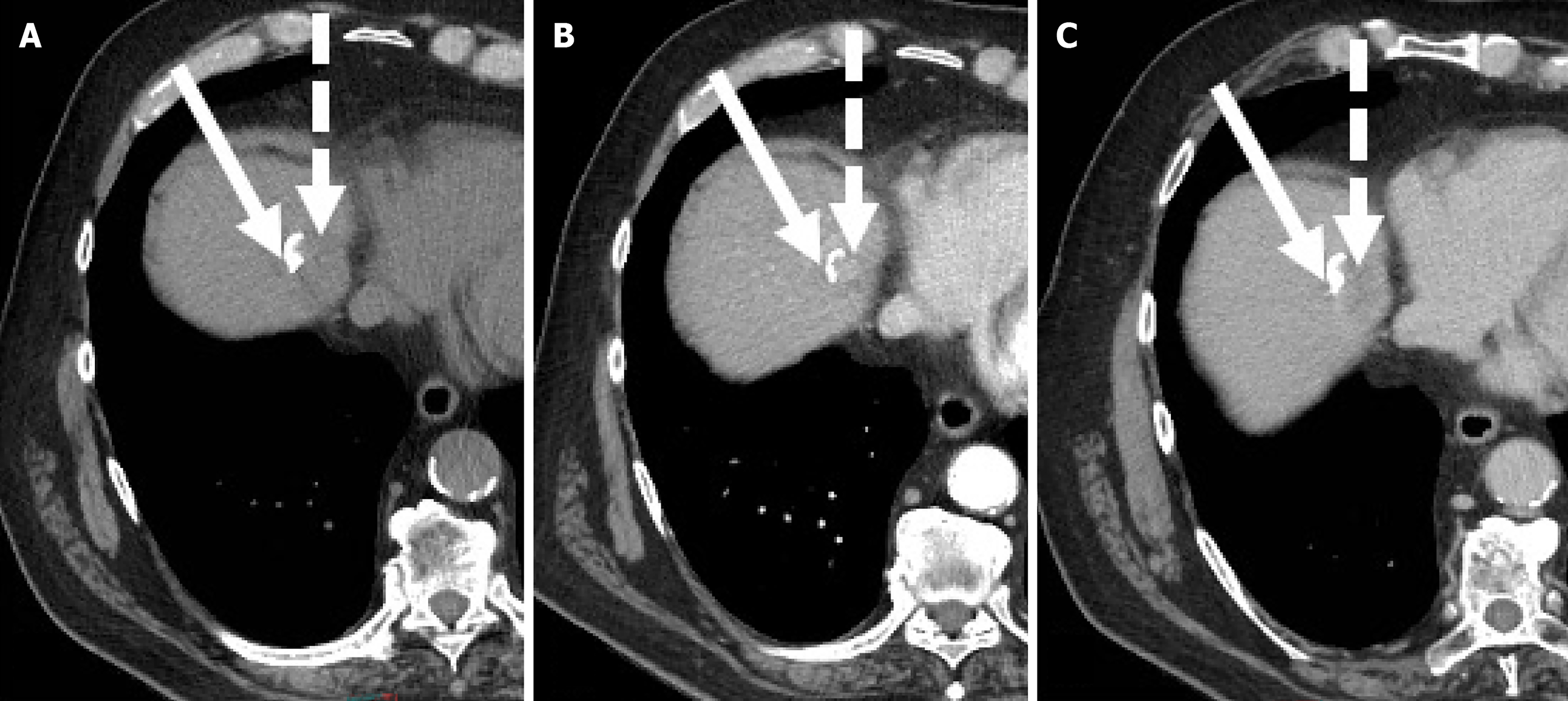
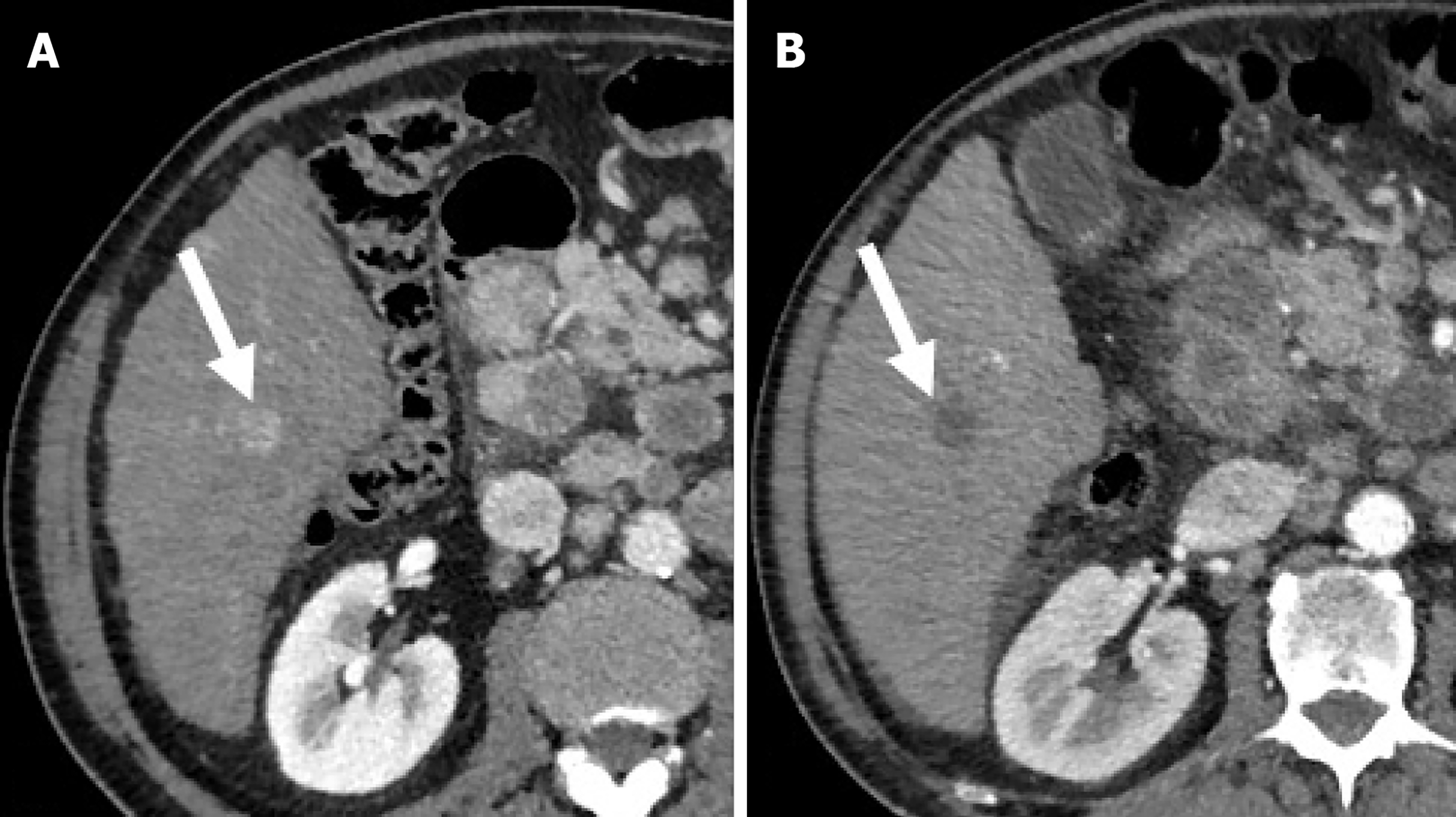
Figure 2 Residual hepatocellular carcinoma after trans-arterial chemoembolization in a 72-year-old man with hepatitis C virus-related hepatic cirrhosis.
A: On unenhanced computed tomography obtained one month after trans-arterial chemoembolization the residual tumor (dotted arrow) shows no Lipiodol retention and the necrotic tumor (arrow) shows homogeneous Lipiodol retention; B: On hepatic arterial phase the residual tumor shows enhancement and the necrotic tumor shows no enhancement; C: On delayed phase the residual tumor shows wash-out.
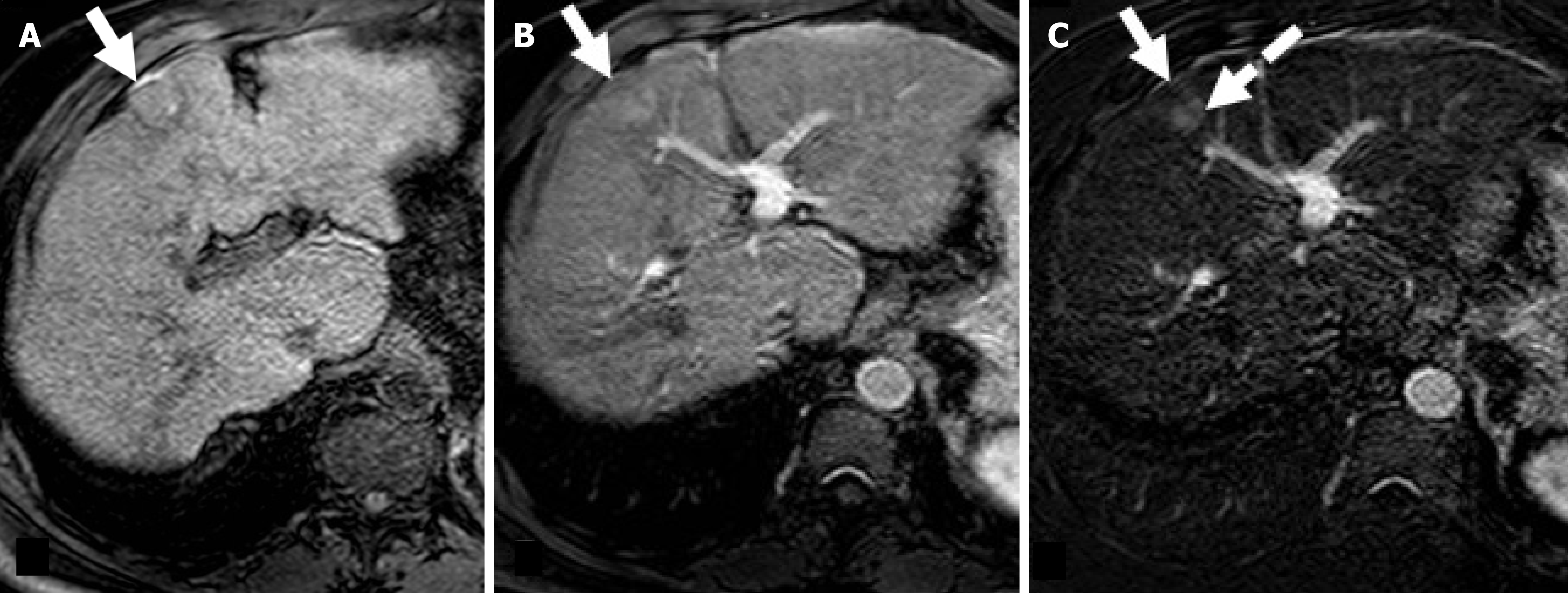
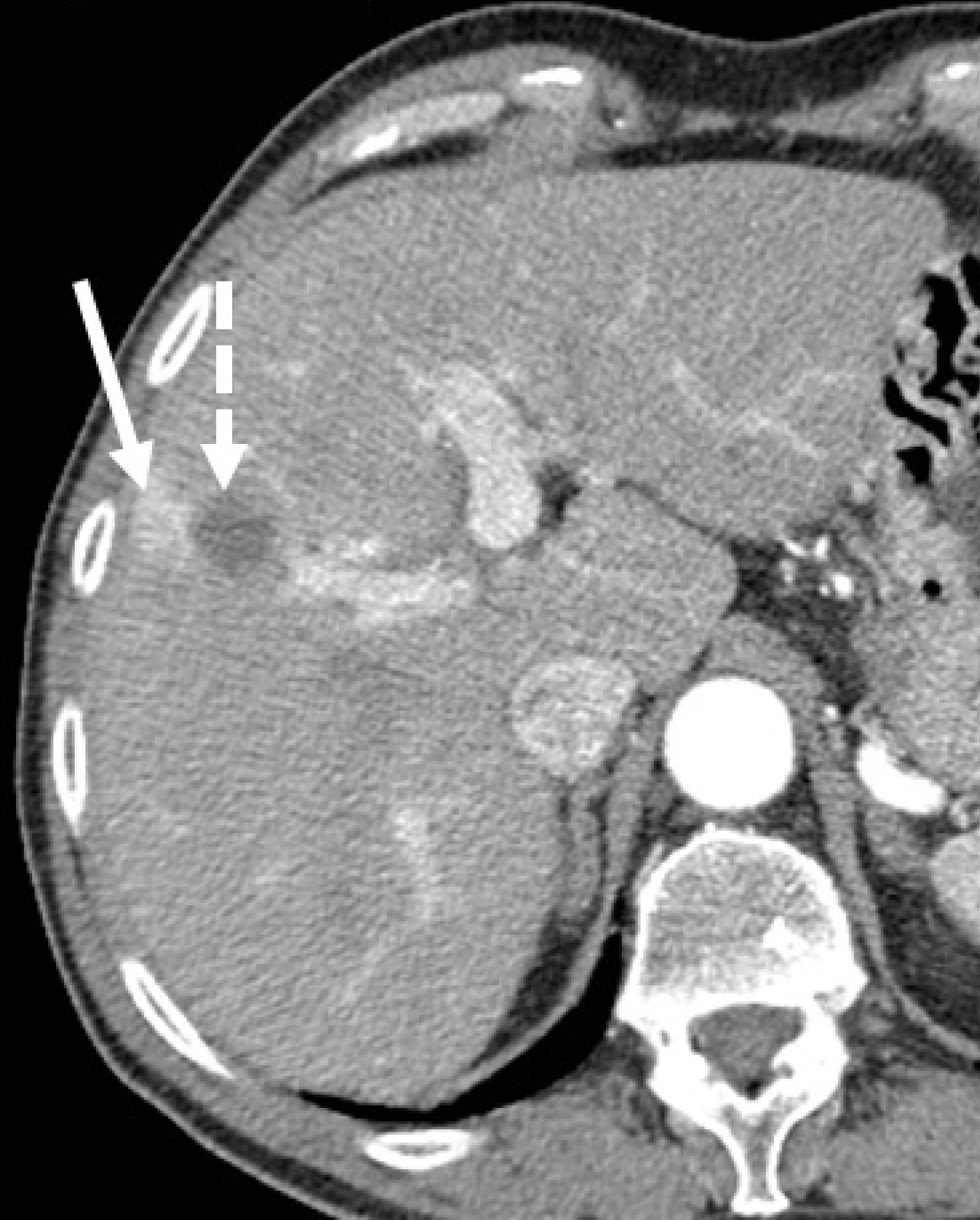
Figure 3 Residual hepatocellular carcinoma after radiofrequency ablation in a 68-year-old man with hepatitis C virus-related hepatic cirrhosis.
A: On magnetic resonance imaging obtained one month after radiofrequency ablation the treated area (arrow) shows slight hyperintensity on unenhanced T1-weighted due to coagulative necrosis; B: On corresponding hepatic arterial phase (HAP) image the treated area shows heterogenous hyperintensity; C: Subtracted HAP image shows enhancement in the posterior portion of the treated area (dotted arrow) suggesting residual tumor enhancement.
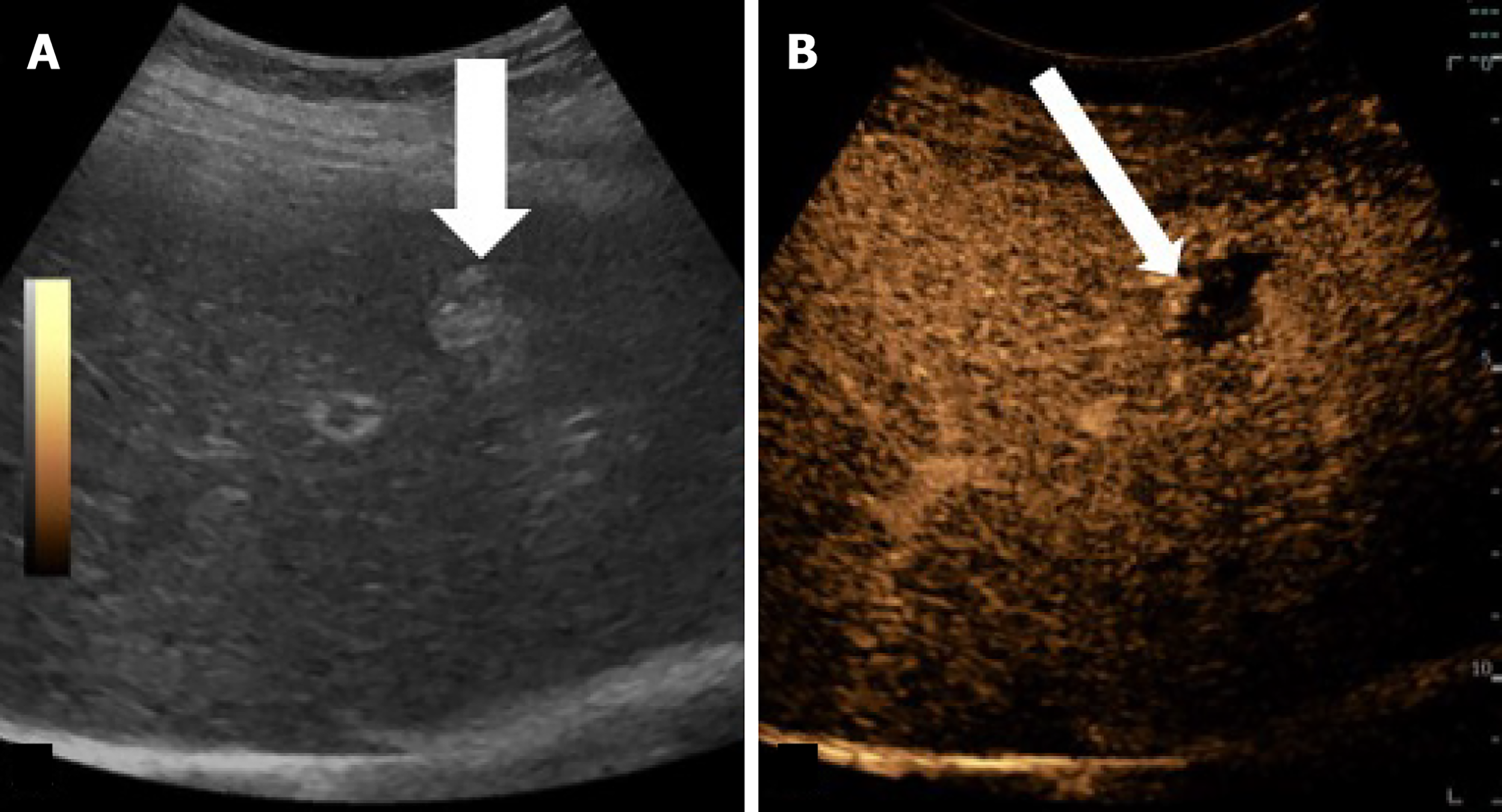
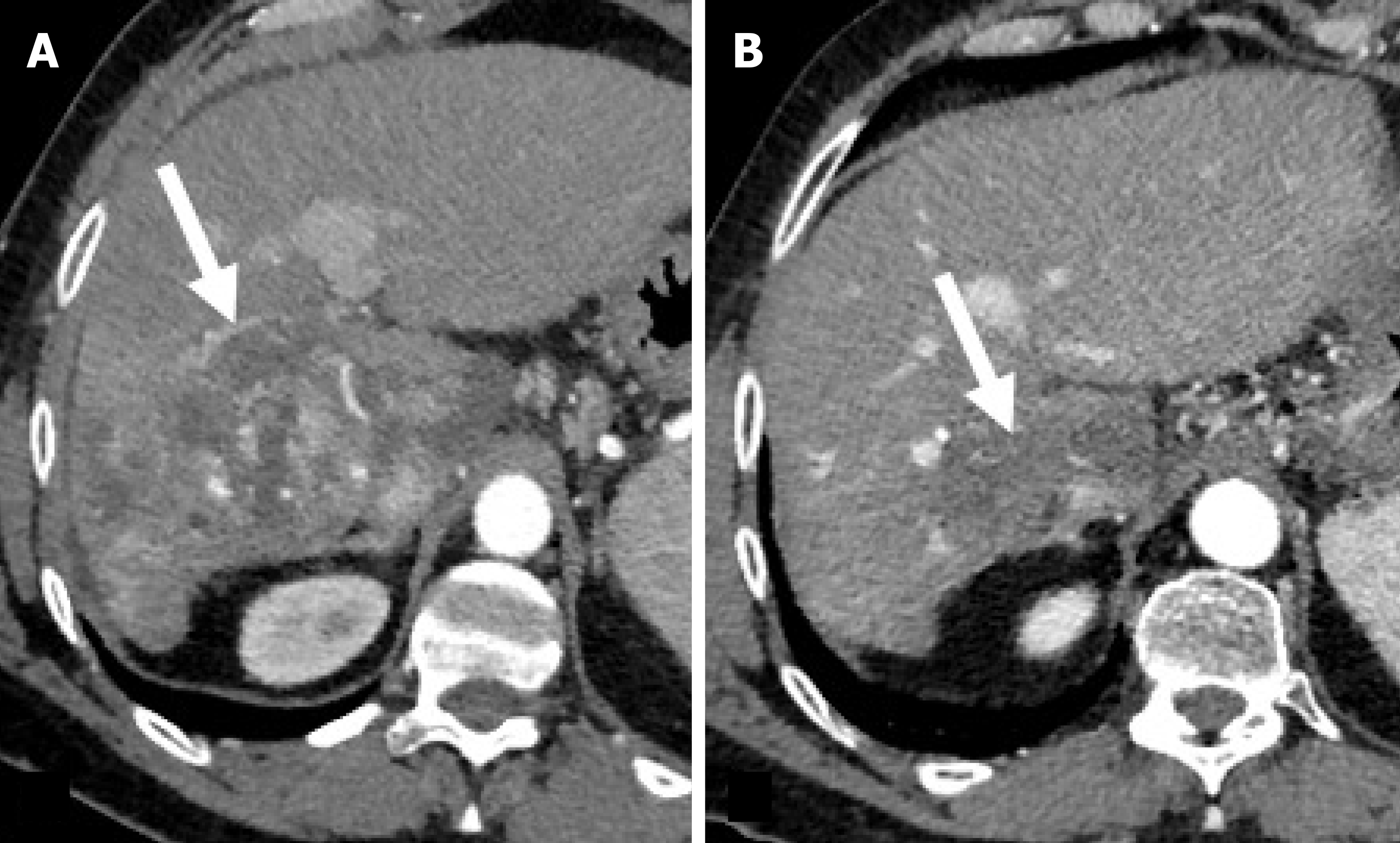
Figure 4 Recurrent hepatocellular carcinoma after radiofrequency ablation in an 82-year-old woman with hepatitis C virus-related cirrhosis.
A: On gray-scale ultrasound image obtained one year after radiofrequency ablation the treated area is hyperechoic nodule (arrow); B: Corresponding contrast enhanced ultrasound image achieved 18 s after injection shows a nodular are of hepatic arterial phase hyperenhancement (arrow).
Figure 5 Hepatocellular carcinoma treated with antiagiogenetic therapy in a 65-year-old man with hepatitis C virus-related hepatic cirrhosis.
A: On pretreatment arterial phase computed tomography (CT), hepatocellular carcinoma (HCC) shows homogeneous enhancement (arrow); B: On hepatic arterial phase CT obtained 2 months after start of treatment, HCC shows disappearance of enhancement and no change in size.
Figure 6 Perfusion alteration after hepatocellular carcinoma radiofrequency ablation in a 62-year-old man with hepatitis C virus-related cirrhosis.
Hepatic arterial phase computed tomography (CT) obtained 1 month after treatment shows an enhancing area (solid arrow) lateral to the ablated zone (dotted arrow). This area showed no venous wash-out and disappeared on subsequent CT follow-up (images not shown).
Figure 7 Hepatocellular carcinoma treated with trans-arterial radioembolization in a 60-year-old man with hepatitis C virus-related hepatic cirrhosis.
A: On hepatic arterial phase (HAP) computed tomography (CT) obtained 3 months after treatment, hepatocellular carcinoma (HCC) shows persistent enhancement (arrow); B: On HAP CT obtained 6 months after start of treatment, HCC shows almost-complete disappearance of enhancement and decrease in size.
- Citation: Agnello F, Taibbi A, Galia M, Orlando A, Gagliardo C, Bartolotta TV. Hepatocellular carcinoma treatment response: Imaging findings and criteria. World J Radiol 2025; 17(10): 108804
- URL: https://www.wjgnet.com/1949-8470/full/v17/i10/108804.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i10.108804