Published online Nov 26, 2025. doi: 10.4330/wjc.v17.i11.110899
Revised: July 7, 2025
Accepted: October 24, 2025
Published online: November 26, 2025
Processing time: 156 Days and 14.6 Hours
With rising angiography costs and risks, we explored whether a 5-minute femoral ultrasound can predict patients that actually require angiography.
To detect associations between atherosclerosis of peripheral arteries and coronary stenosis in patients with coronary heart disease (CHD).
The study included a total of 218 patients (63 ± 10.9 years of age; 54% male) with CHD subjected to coronary angiography and routine diagnostic assessment, including ultrasound imaging to assess the extent of peripheral atherosclerotic lesions. Receiver operating characteristic analysis and binomial logistic regression were used to detect the associations.
We demonstrated for the first time that the presence of atherosclerotic plaque with ≥ 70% stenosis in femoral arteries was associated with significant coronary stenosis, with 93% sensitivity and 90% specificity, and thus can be used as an additional diagnostic marker for coronary stenosis. The data indicated associations between femoral artery atherosclerosis and atherosclerotic lesions of coronary arteries, with a high correlation coefficient r = 0.8 (P < 0.05). The presence of an atherosclerotic plaque in the femoral arteries with ≥ 30% or ≥ 70% stenosis was associated with a 30- or 70-fold higher odds ratio of coronary stenosis, respectively.
For resource-limited clinics, our findings suggest skipping carotids - femoral ultrasound alone may suffice to rule out severe CHD. Ultrasound imaging femoral artery atherosclerosis provides a simplified approach for patient stratification.
Core Tip: With rising angiography costs and risks, we explored whether a 5-minute femoral ultrasound could predict who truly needs it. We have analyzed associations between atherosclerosis of peripheral arteries detected by ultrasound and coronary stenosis detected by angiography with evaluation of the extent of coronary lesions using the Gensini score. A femoral plaque ≥ 70% flagged severe coronary stenosis as reliably as many blood tests (area under curve 0.93 with 93% sensitivity and 90% specificity), like troponin for myocardial infarction.
- Citation: Gumanova NG, Vasilyev DK, Mols AAA, Drapkina OM, Kiselev AR. Femoral artery plaque: A simple ultrasound clue for severe coronary stenosis. World J Cardiol 2025; 17(11): 110899
- URL: https://www.wjgnet.com/1949-8462/full/v17/i11/110899.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i11.110899
Cardiovascular diseases (CVDs) remain the leading cause of death in Russian Federation and other additional. Coronary artery disease (CAD) is the main pathology that results from atherosclerotic lesions of coronary arteries. Coronary angiography is a widely used golden standard method of invasive coronary heart disease (CHD) diagnosis. However, coronary angiography is not always available and has certain drawbacks, including specific equipment and supplies, and X-ray-equipped operating room, low but still significant rate of complications due to invasiveness of the procedure, and high rate of discrepancies between general clinical symptoms of CAD and actual detected lesions. Advanced patient stratification strategies may thus be complex and introduce unneeded errors in the process. To exclude the errors and simplify stratifications, the use of a non-invasive ultrasound imaging during initial patient evaluation enables the assessment of the presence of atherosclerotic lesions in peripheral arteries and enables prediction of coronary lesions with a high accuracy. Cardiologists routinely check carotids; however, the femoral artery, which is often easier to assess, remains an overlooked window into coronary risk. The literature data about associations between femoral lesions detected by ultrasound and coronary lesions detected by angiography are very scarce[1]. For instance, a large scale study “transcatheter aortic valve implantation” where peripheral artery disease (PAD) and CAD were evaluated in the context of access strategy and complication prediction, does not provide finding on direct link between PAD and CAD[2]. A cluster-randomized study FAMILIA trial investigating genetic and environmental factors in CVDs, including PAD and CAD, found that providing participants with information about the presence of atherosclerosis (via vascular ultrasound) significantly improved the effectiveness of lifestyle interventions. However, the study did not explore the relationship between atherosclerosis in the coronary and femoral arteries[3]. A hypothesis of whether femoral plaque ≥ 70% is a viable target for predicting severe coronary stenosis has not been tested. Thus, the aim of the present study was to estimate whether associations between PAD and CAD can be used to reliably predict the presence of coronary atherosclerosis based on the data of ultrasound imaging of the femoral arteries.
The cross-sectional study enrolled male and female patients sequentially, applying the inclusion criteria: The age over 25 years and clinical symptoms of CHD as described previously[4,5]. All patients were subjected to coronary angiography according to the recommendations of European Society of Cardiology, and stenting was performed if indicated[6].
Single-center design may limit generalization; however, strict exclusion criteria used in the present study ensured unbiased comparisons. Exclusion criteria were as follows: Myocardial infarction within 6 months before enrollment, acute inflammatory diseases, chronic kidney failure stage III or higher with the glomerular filtration rate less than 60 mL/minute/1.73 m2, decompensated diabetes mellitus type I or II with glycated hemoglobin levels over 7.5%, left ventricular ejection fraction below 40%, oncological diseases, familiar hypercholesterolemia, hematological diseases, and immune and autoimmune diseases.
All enrolled patients signed an informed consent. An Independent Ethics Committee of National Center for Preventive Medicine approved the protocol of the present study, approval No. 01-01/17. The study was performed in compliance with The Helsinki Declaration.
Patient examination included blood pressure and heart rate tests, other evaluations, and coronary angiography were performed as described by us previously[4,5]. The extent of coronary lesions was evaluated using the Gensini score assessed by the Advantage Workstation version 4.4[7,8].
Peripheral atherosclerosis of the brachiocephalic and femoral arteries and the volume of the corresponding plaques were evaluated by ultrasound imaging in the B-mode on a duplex scanner at 9-11 MHz frequency using linear probes (GE Vivid 7 run by TruScan raw)[4,5] due to scientific indications. Lesions of the brachiocephalic arteries were assessed as follows: Brachiocephalic arteries with no lesions, mild stenosis with the degree of stenosis < 60%, and severe or hemodynamically significant stenosis ≥ 60% according to the guidelines of the European Society of Cardiology[9]. Lesions of the femoral arteries were assessed as follows: Femoral arteries with no lesions, mild stenosis with a degree of stenosis < 70%, and severe stenosis ≥ 70%[10]. Two vascular sonography specialists, which were blinded to angiography results, performed all scans using a standardized protocol to minimize variability.
Smoking status was assessed as follows: 0, never smoked; 1, smoking in the past; 2, present smoker. Statin treatment was recorded both before and after hospital admission. Type 2 diabetes was diagnosed when the glycated hemoglobin test (the glycated hemoglobin test) was 6.5% or higher on two separate tests.
SPSS version 23 software were used. The size and power of the comparisons were estimated using an online calculator Sampsize (https://sampsize.sourceforge.net/iface/s2.html#nm; accessed on September 10, 2021) to ensure the group sizes are sufficient to detect the differences. Kolmogorov-Smirnov criterion was used for test of normality of the distributions. The data are shown as the mean ± SD. Two-tailed non-parametric analysis of variance, Kruskal-Wallis and Mann-Whitney tests, were used to compare the groups. A receiver operating characteristic curve and Odds ratio (OR) with an area under curve (AUC) with 95% confidence interval were calculated, as appropriate. Multivariate logistic regression was proved with Wald test. The χ2 statistic corresponded to the difference in -2 log-likelihoods between the final model and a reduced model. Reduced model was formed by omitting an effect from the final model. The null hypothesis was that all parameters of that effect are zero. The P values < 0.05 were considered significant.
The present cross-sectional study included a total of 216 patients (63 ± 10.9 years of age; 54% male). General characteristics of the cohort are presented in Table 1. The data indicated that the groups with and without coronary lesions had similar baseline characteristics excluding sex and glucose level. Men were overrepresented in the high-Gensini group (60.5% vs 43%, P = 0.036), likely reflecting known sex disparities in CAD severity. Mean Gensini index value in the cohort was 57.0 ± 38.4 (from 0 to 197). Gensini score 0 corresponded to minor coronary lesions in 76 (34.9%) patients (coronary stenosis < 25%)[7]. Coronary atherosclerosis was detected in 71 (32.6%) patients. Multiple vascular lesions, including stenosis of the main left coronary artery in combination with more than 50% stenosis of other major coronary arteries, was detected in 71 (32.6%) patients. A total of 71 (32.6%) patients were subjected to planned revascularization during coronary angiography, including 4 (5.2%) patients with Gensini score 0 and 143 patients with Gensini score higher than 1. In general, 97.3% patients had significant coronary lesions because Gensini score was higher than 10. This was a reason that 58% of cohort has statin treatment and low level of cholesterol as a result (Table 1).
| Parameters | Baseline characteristics | P value | ||
| Total cohort (n = 218) | Patients with Gensini score 0 (n = 76) | Patients with Gensini score > 0 (n = 142) | ||
| Sex (men%) | 53 | 43 | 60.5 | 0.036 |
| Age | 62.6 (10.9) | 60.5 (11.9) | 63.5 (10.1) | - |
| BMI, kg/m2 | 29.9 (5.8) | 29.4 (5.6) | 30.1 (5.1) | - |
| Smoking (0/1/2)1% | 45/13/42 | 50/14/36 | 42/9/46 | - |
| DMT2% | 21.3 | 14.2 | 25.6 | 0.05 |
| Waist circumference, cm | 93.0 (11.5) | 92.1 (12.2) | 93.7 (12.3) | - |
| Systolic blood pressure, mm Hg | 129.5 (12.7) | 126.53 (11.5) | 131.1 (14.3) | 0.02 |
| Diastolic blood pressure, mm Hg | 71.8 (7.8) | 71.8 (7.6) | 73.5 (8.6) | - |
| Biochemical markers | ||||
| Total cholesterol, mmol/L | 4.32 (1.10) | 4.49 (1.13) | 4.24 (1.08) | - |
| Triglycerides, mmol/L | 1.50 (0.76) | 1.54 (0.85) | 1.47 (0.72) | - |
| LDL cholesterol, mmol/L | 2.50 (0.90) | 2.62 (0.97) | 2.43 (0.91) | - |
| HDL cholesterol, mmol/L | 1.15 (0.31) | 1.18 (0.32) | 1.12 (0.30) | - |
| Glucose, mmol/L | 6.32 (1.68) | 5.85 (1.35) | 6.60 (1.78) | 0.0001 |
| Statin treatment at enrollment% | 58.2 | 32.3 | 72.3 | 0.0001 |
Angiographic characteristics of all circulation pools in patients of the total cohort were as follows: 42 (15%) patients had insignificant lesions in all circulation pools (coronary and peripheral circulation including brachiocephalic and femoral); 95 (34%) patients had moderate lesions; and 144 (51%) patients had severe lesions. In the case of coronary circulation, 76 (35%) patients had insignificant coronary lesions (Gensini score 0); 63 (29%) patients had moderate coronary lesions, with Gensini score from 1 to 36; and 79 (36%) patients had severe coronary lesions, with Gensini score over 36. In the case of brachiocephalic circulation, 41 (19%) patients had insignificant lesions; 156 (72%) patients had moderate lesions with stenosis less than 60%; and 21 (10%) patients had severe lesions with stenosis over 60%. In the case of femoral circulation, 69 (32%) patients had insignificant lesions; 85 (40%) patients had moderate lesions with stenosis less than 70%; and 60 (28%) patients had severe lesions with stenosis over 70%.
Data indicated a high Spearmen correlation between atherosclerotic lesions of the femoral and coronary arteries (r = 0.8; P < 0.05). A correlation between lesions in the coronary and brachiocephalic circulation pools was significant but had substantially lower coefficient (r = 0.5; P < 0.05).
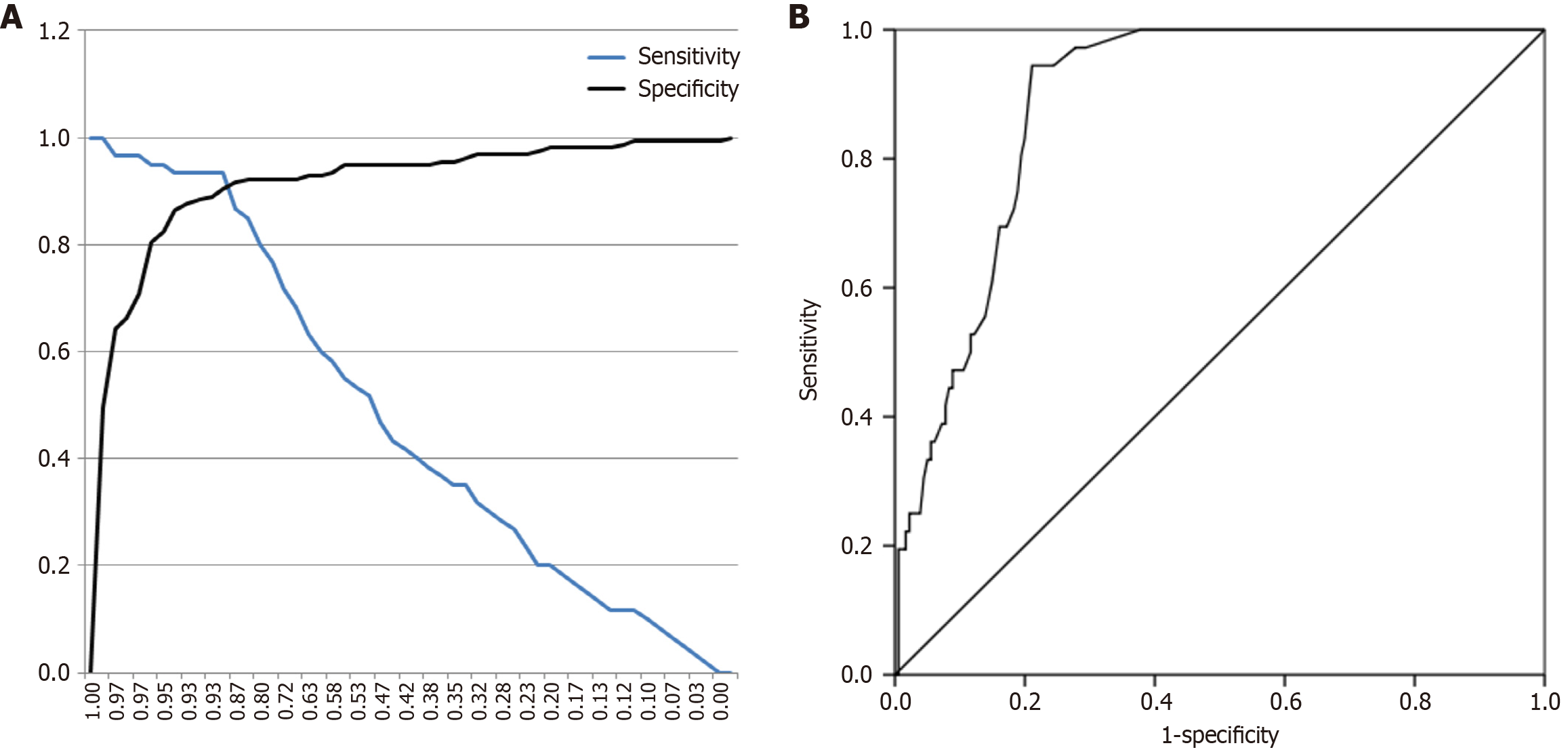
Considering this high correlation, we performed detailed analysis of the associations between coronary and femoral lesions detected by angiography and ultrasound imaging, respectively, to determine the threshold values for atherosclerotic lesions of the femoral arteries corresponding to the best specificity and sensitivity values of associations with coronary lesions. We used receiver operating characteristic analysis and assumed the extent of atherosclerotic lesions of the femoral arteries as two separate sets of independent binary variables (severity of the lesions below or above 30% and below and above 70%), while Gensini score for coronary lesions was a dependent continuous variable. Alternatively, for the same two sets of independent variables, we used multiple coronary lesions as another binary dependent variable with threshold of 50% stenosis in at least one major coronary vessel, including the right coronary artery and the left main coronary artery, which branches into the left anterior descending artery and the left circumflex artery.
The data of Table 2 indicate that atherosclerotic lesions of the femoral arteries over 30% were associated with significantly higher OR (30-fold higher) of coronary stenosis over 50% in at least one major coronary vessel compared with that in patients with femoral stenosis below 30%. Atherosclerotic lesions of femoral arteries over 70% were associated with 70-fold higher OR of coronary stenosis (Gensini score ≥ 41) compared with that in patients with femoral atherosclerosis below 70% (Table 3). In the study cohort, Gensini score ≥ 41 corresponded to the upper quartile of severity of coronary lesions. Calculations of the Gensini score assume that stenosis of a coronary artery by 25% and 50% correspond to 1 point and 2 points, respectively[7]. Atherosclerotic lesions of the femoral arteries over 70% were associated with severe coronary atherosclerosis (Gensisni ≥ 41) as a binary variable adjusted for other assessed factors, including sex, age, statin therapy, etc. (Table 4) with OR = 9.67 (95% confidence interval: 4.16-22.45; P < 0.0001). So atherosclerotic lesions of femoral arteries over 70% is independently associated with severe coronary stenosis. Femoral plaque ≥ 70% was able to predict severe coronary stenosis as reliably as many blood tests (AUC = 0.93 is similar to AUC for troponin I in patients with myocardial infarction).
| ROC | AUC/OR | P value | 95%CI | Sensitivity | Specificity | |
| Lower | Upper | |||||
| Atherosclerosis of femoral arteries, threshold at 30% | 0.91 | 0.0001 | 0.86 | 0.95 | 0.83 | 0.84 |
| Threshold of femoral lesions at 30%; n = 131/12 and 19/52 | 29.87 | 0.0001 | 13.54 | 65.89 | - | - |
| ROC | AUC/OR | P value | 95%CI | Sensitivity | Specificity | |
| Lower | Upper | |||||
| Threshold for Gensini score cut off 41 | 0.93 | 0.0001 | 0.89 | 0.97 | 0.93 | 0.90 |
| Threshold for Gensini score cut off 41; n = 141/13 and 8/52 | 70.5 | 0.0001 | 27.63 | 179.82 | - | - |
| Independent variables | B | SE | Hypothesis test | 95% Wald CI | |||
| Wald χ2 | df | Sig. | Lower | Upper | |||
| Sex | 1.19 | 0.05 | 5.72 | 1 | 0.017 | 1.24 | 8.79 |
| Age | -0.06 | 0.02 | 80.51 | 1 | 0.004 | 0.90 | 0.97 |
| Smoking status1 | -0.13 | 0.24 | 0.31 | 1 | 0.57 | 0.53 | 10.41 |
| DM type 2 | -0.13 | 0.46 | 0.08 | 1 | 0.77 | 0.34 | 20.18 |
| Body mass index | 0.01 | 0.05 | 0.10 | 1 | 0.75 | 0.91 | 10.13 |
| Waist circumference | -0.01 | 0.02 | 0.47 | 1 | 0.49 | 0.94 | 10.02 |
| Systolic blood pressure | -0.01 | 0.01 | 10.13 | 1 | 0.28 | 0.94 | 10.01 |
| Diastolic blood pressure | 0.01 | 0.02 | 0.13 | 1 | 0.71 | 0.95 | 10.07 |
| Statin treatment at enrollment | -1.42 | 0.41 | 11.76 | 1 | 0.001 | 0.11 | 0.54 |
| Femoral atherosclerosis ≥ 70% | -1.42 | 0.53 | 4.99 | 1 | 0.025 | 0.11 | 0.86 |
Thus, atherosclerotic lesions of the femoral arteries can be used to assess the severity of coronary artery stenosis with 93% accuracy, 93% sensitivity, and 90% specificity. The OR for the presence of severe coronary stenosis increases 70-fold in patients with femoral atherosclerotic lesions exceeding 70% (P = 0.0001) (Figure 1). The overall assessment of all combinations is presented in Table 5 to further justify the conclusions.
| Extent of stenosis in femoral arteries (%) | OR for coronary stenosis | Extent of stenosis at least one coronary vessel (%) | Prognostic accuracy (%) |
| 30 | 30 | ≥ 50 | 91 |
| 70 | 70 | ≥ 70 | 93 |
CHD is the main underlying cause of acute coronary events that contribute to cardiovascular mortality in developed countries[11]. Atherosclerotic lesions of coronary arteries are the main pathological process of CHD. Manifestations of acute events are site-specific and depend on localization of atherosclerotic plaques[1]. In Multi-Ethnic Study of Atherosclerosis study addressed to compare predictive utilities of coronary artery calcium presence, carotid artery plaque presence, and high intima media thickness for incident CVD events was shown that femoral plaques were more strongly associated with CVDs risk factors and atherosclerosis in the coronary and aortic arteries than carotid plaques[12]. Thus, therapeutic strategies of the treatments of CVDs also depend on plaque location. Former or current smoking status may affect plaques prevalence in femoral arteries than in carotid arteries[12]. Recent progress resulted in understanding of the molecular mechanisms of atherogenesis in great detail. However, prediction of the localization of the lesions and local pathways involved in the formation of plaques in specific regions are poorly understood. Certain risk factors, such as smoking and diabetes[1], have differential effects on risk of atherosclerosis depending on vascular regions. Peripheral atherosclerosis may depend on hereditary factors, while male sex is associated with a higher risk of lesions in the coronary and carotid regions[1]. Localization contributes to the morphology and stability of an atherosclerotic plaque. For example, carotid plaques have higher lipid content, while coronary plaques are enriched in fibrous components and lipid particles, and femoral plaques predominantly include fibrous calcification[13]. These factors are relevant for clinical intervention strategies, which are less efficient in carotid arteries. Moreover, reactivity to statin treatment may differ depending on localization of atherosclerotic lesions even in the same individual patient[1]. Our findings show that femoral artery atherosclerosis (over 70%) is independently associated with severe coronary artery stenosis, even after adjusting for statin treatment at the enrollment (Table 4). The BioImage (BioImage Study: A Clinical Study of Burden of Atherosclerotic Disease in an At-Risk Population, NCT00738725) a prospective study evaluating cross-sectional associations among imaging and circulating biomarkers and their ability to predict near-term 3-year atherothrombotic events in asymptomatic subjects revealed that detection of subclinical carotid or coronary atherosclerosis improves risk predictions and reclassification compared with conventional risk factors in cost-effective manner[14].
Notably, femoral and ileal circulation develops atherosclerotic lesions during the early stages of atherogenesis[12]. The results of the present study indicated that the presence of femoral atherosclerotic lesions (≥ 70%) was associated with a very high risk of coronary lesions, which result in CHD. These results are in good agreement with another study that demonstrated that a higher intima media thickness ≥ 0.83 mm in the femoral artery was associated with coronary artery stenosis of over 50%, with 72.1% sensitivity and 61.1% specificity in patients with stable ischemic heart disease[15]. Femoral arteries may be considered a stress test for systemic atherosclerosis because mechanical strain due to walking may accelerate plaque formation, thus mirroring coronary risk. Modern diagnostic strategies are evolving toward more safe and accessible approaches. Invasive coronary angiography remains the gold standard of cardiovascular diagnostics. However, noninvasive ultrasound imaging is also evolving to achieve better resolution and prognostic accuracy, including, for example, the capability to assess calcification of femoral and carotid artery plaques linked to overall prognosis[16]. For clinicians with limited resources, our findings suggest a possibility of bypassing the scanning of the carotids because femoral ultrasound alone may be sufficient in ruling out severe CAD. Thus, the use of noninvasive ultrasound greatly enhances accessibility of modern diagnostic methods and simplifies patient stratification for coronary angiography, while also providing the benefit or evaluation of the whole circulation.
We found that atherosclerotic lesions of the femoral arteries detected by noninvasive ultrasound imaging were strongly associated with coronary lesions detected by invasive coronary angiography in patients with CHD. Thus, atherosclerotic lesions over 70% in the femoral arteries can be used for diagnosis of severe stenosis in the coronary circulation to enhance stratification of patients for coronary angiography.
The authors are grateful for editing of English to Dr. Alexander Kots.
| 1. | Jarauta E, Laclaustra M, Villa-Pobo R, Langarita R, Marco-Benedi V, Bea AM, León-Latre M, Casasnovas JA, Civeira F. Three Dimensional Carotid and Femoral Ultrasound is not Superior to Two Dimensional Ultrasound as a Predictor of Coronary Atherosclerosis Among Men With Intermediate Cardiovascular Risk. Eur J Vasc Endovasc Surg. 2020;59:129-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Ueshima D, Barioli A, Nai Fovino L, D'Amico G, Fabris T, Brener SJ, Tarantini G. The impact of pre-existing peripheral artery disease on transcatheter aortic valve implantation outcomes: A systematic review and meta-analysis. Catheter Cardiovasc Interv. 2020;95:993-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Fernandez-Jimenez R, Jaslow R, Bansilal S, Diaz-Munoz R, Fatterpekar M, Santana M, Clarke-Littman A, Latina J, Soto AV, Hill CA, Al-Kazaz M, Samtani R, Vedanthan R, Giannarelli C, Kovacic JC, Bagiella E, Kasarskis A, Fayad ZA, Fuster V. Different Lifestyle Interventions in Adults From Underserved Communities: The FAMILIA Trial. J Am Coll Cardiol. 2020;75:42-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Gumanova NG, Vasilyev DK, Bogdanova NL, Havrichenko YI, Drapkina OM. P-, E-, and H-cadherins differ in their relationships with coronary stenosis, cardiovascular outcomes, and unplanned recurrent revascularization. J Mol Cell Cardiol Plus. 2024;9:100091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Gumanova NG, Vasilyev DK, Bogdanova NL, Drapkina OM. Serum Level of Cadherin-P (CDH3) Is a Novel Predictor of Cardiovascular Events Related to Atherosclerosis in a 3-Year Follow-Up Study. J Clin Med. 2024;13:6293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Task Force Members; Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, Bugiardini R, Crea F, Cuisset T, Di Mario C, Ferreira JR, Gersh BJ, Gitt AK, Hulot JS, Marx N, Opie LH, Pfisterer M, Prescott E, Ruschitzka F, Sabaté M, Senior R, Taggart DP, van der Wall EE, Vrints CJ; ESC Committee for Practice Guidelines, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S; Document Reviewers, Knuuti J, Valgimigli M, Bueno H, Claeys MJ, Donner-Banzhoff N, Erol C, Frank H, Funck-Brentano C, Gaemperli O, Gonzalez-Juanatey JR, Hamilos M, Hasdai D, Husted S, James SK, Kervinen K, Kolh P, Kristensen SD, Lancellotti P, Maggioni AP, Piepoli MF, Pries AR, Romeo F, Rydén L, Simoons ML, Sirnes PA, Steg PG, Timmis A, Wijns W, Windecker S, Yildirir A, Zamorano JL. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949-3003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2772] [Cited by in RCA: 3036] [Article Influence: 233.5] [Reference Citation Analysis (1)] |
| 7. | Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1273] [Cited by in RCA: 1550] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 8. | Gumanova NG, Gavrilova NE, Chernushevich OI, Kots AY, Metelskaya VA. Ratios of leptin to insulin and adiponectin to endothelin are sex-dependently associated with extent of coronary atherosclerosis. Biomarkers. 2017;22:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Aboyans V, Ricco JB, Bartelink MEL, Björck M, Brodmann M, Cohnert T, Collet JP, Czerny M, De Carlo M, Debus S, Espinola-Klein C, Kahan T, Kownator S, Mazzolai L, Naylor AR, Roffi M, Röther J, Sprynger M, Tendera M, Tepe G, Venermo M, Vlachopoulos C, Desormais I; ESC Scientific Document Group. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39:763-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1435] [Cited by in RCA: 2387] [Article Influence: 341.0] [Reference Citation Analysis (0)] |
| 10. | Gao M, Hua Y, Zhao X, Jia L, Yang J, Liu B. Optimal Ultrasound Criteria for Grading Stenosis of the Superficial Femoral Artery. Ultrasound Med Biol. 2018;44:350-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, Naghavi M, Mensah GA, Murray CJ. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 706] [Cited by in RCA: 844] [Article Influence: 76.7] [Reference Citation Analysis (0)] |
| 12. | Gepner AD, Young R, Delaney JA, Tattersall MC, Blaha MJ, Post WS, Gottesman RF, Kronmal R, Budoff MJ, Burke GL, Folsom AR, Liu K, Kaufman J, Stein JH. Comparison of coronary artery calcium presence, carotid plaque presence, and carotid intima-media thickness for cardiovascular disease prediction in the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging. 2015;8:e002262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 220] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 13. | Jovin DG, Sumpio BE, Greif DM. Manifestations of human atherosclerosis across vascular beds. JVS Vasc Insights. 2024;2:100089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Baber U, Mehran R, Sartori S, Schoos MM, Sillesen H, Muntendam P, Garcia MJ, Gregson J, Pocock S, Falk E, Fuster V. Prevalence, impact, and predictive value of detecting subclinical coronary and carotid atherosclerosis in asymptomatic adults: the BioImage study. J Am Coll Cardiol. 2015;65:1065-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 370] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 15. | Fernández-Friera L, Peñalvo JL, Fernández-Ortiz A, Ibañez B, López-Melgar B, Laclaustra M, Oliva B, Mocoroa A, Mendiguren J, Martínez de Vega V, García L, Molina J, Sánchez-González J, Guzmán G, Alonso-Farto JC, Guallar E, Civeira F, Sillesen H, Pocock S, Ordovás JM, Sanz G, Jiménez-Borreguero LJ, Fuster V. Prevalence, Vascular Distribution, and Multiterritorial Extent of Subclinical Atherosclerosis in a Middle-Aged Cohort: The PESA (Progression of Early Subclinical Atherosclerosis) Study. Circulation. 2015;131:2104-2113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 418] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 16. | Genkel V, Kuznetsova A, Kolyadich M, Lebedev E, Rusanova S, Stolbushkina O, Shaposhnik I. Intima-media thickness of the common femoral arteries as a marker for coronary atherosclerosis in patients with coronary artery disease. Clin Pharmacol Ther. 2020;29:44-48. [DOI] [Full Text] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/