Published online Oct 26, 2025. doi: 10.4330/wjc.v17.i10.110072
Revised: June 11, 2025
Accepted: September 1, 2025
Published online: October 26, 2025
Processing time: 149 Days and 1.3 Hours
Heart failure (HF) is characterized by unbalanced oxygen demand and supply and impaired exercise capacity, which substantially affects the quality of life and prognosis of patients with HF. Cardiac rehabilitation is an effective intervention for improving exercise intolerance in patients with cardiovascular diseases, including HF. However, cardiac rehabilitation is not always accessible to these patients because a restricted number of hospitals offer cardiac rehabilitation, and access to these hospitals is limited to those who require rehabilitation. Although pharmacological interventions may help improve exercise capacity in patients with HF, evidence for this intervention is scarce. This mini-review summarizes the available research on the effects of pharmacological therapies on improving exercise capacity.
Core Tip: Heart failure (HF) affects quality of life and prognosis in patients with HF. Although cardiac rehabilitation is an effective intervention to improve exercise intolerance in patients with HF. Cardiac rehabilitation is not always accessible because of restricted access for those who need rehabilitation. Evidence on pharmacological interventions to improve exercise capacity in patients with HF is scarce. This mini-review summarizes available evidence on the effects of pharmacological therapy for HF on improving exercise capacity.
- Citation: Naito R. Pharmacological interventions to enhance exercise capacity in patients with heart failure. World J Cardiol 2025; 17(10): 110072
- URL: https://www.wjgnet.com/1949-8462/full/v17/i10/110072.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i10.110072
Heart failure (HF) is accompanied by exercise intolerance owing to impaired cardiac function, limited pulmonary reserve, and comorbidities, such as anemia, diabetes mellitus, impaired kidney function, and frailty[1,2]. Regardless of the etiology of HF, dyspnea and fatigue are the leading limiting symptoms that may impair exercise capacity and quality of life. Exercise intolerance and impaired cardiac reserve in patients with HF may further limit exercise capacity and cause pulmonary congestion and systemic edema, thereby creating a continuous vicious cycle of decompensation, hospitalization for worsening HF, and exercise intolerance. Exercise intolerance occurs in patients with HF through impaired left ventricular contractility, reduced β-adrenergic responsiveness to workload, elevated systemic vascular resistance, and insufficient peripheral arterial vasodilator response to exercise[2,3].
Exercise capacity can be assessed both subjectively and objectively. Subjective assessment includes symptoms such as dyspnea on exertion and the patients perceived exertion (i.e., the Borg scale)[4]. Objective measurements include peak oxygen consumption or oxygen consumption at the anaerobic threshold, exercise duration, and metabolic equivalents obtained by exercise testing. The standard exercise testing to evaluate exercise capacity is cardiopulmonary exercise testing with respiratory gas analysis, and alternative methods are the 6-minute walking distance (6MWD) test and exercise stress tests using an ergometer or treadmill[5,6]. Multiple factors determine the peak oxygen consumption, which represents exercise capacity. As shown in the following equation: (1) Oxygen consumption = cardiac output multiplied by the oxygen content difference between arterial oxygen content and mixed venous oxygen content; (2) Cardiac output; (3) Pulmonary diffusing capacity; (4) Oxygen-carrying capacity of the blood; and (5) Skeletal muscle characteristics affect peak oxygen consumption[7].
Recent advances in medical therapy for HF have had a prognostic impact in patients with HF[8]. Specifically, the combination of sodium-glucose co-transporter 2 inhibitors (SGLT2 inhibitors), angiotensin receptor neprilysin inhibitor (ARNI), mineralocorticoid receptor antagonists (MRA), and beta-blockers are essential HF medications. Evidence for each drug has accumulated, and the international guidelines for HF management recommend the use of these drugs in patients with HF, especially those with reduced left ventricular ejection fraction (EF)[9,10].
Although extending longevity has been a major issue in medicine, ways of improving the quality of life should also be sought for patient satisfaction and healthy societies[11,12]. Several factors affect the quality of life, such as health literacy, socioeconomic status, multimorbidity, social support, and access to healthcare in patients with non-communicable diseases such as HF[13,14]. A vicious cycle of limited functional reserve, exercise intolerance, and impaired quality of life in patients with HF makes it difficult to intervene appropriately to combat deteriorating exercise capacity.
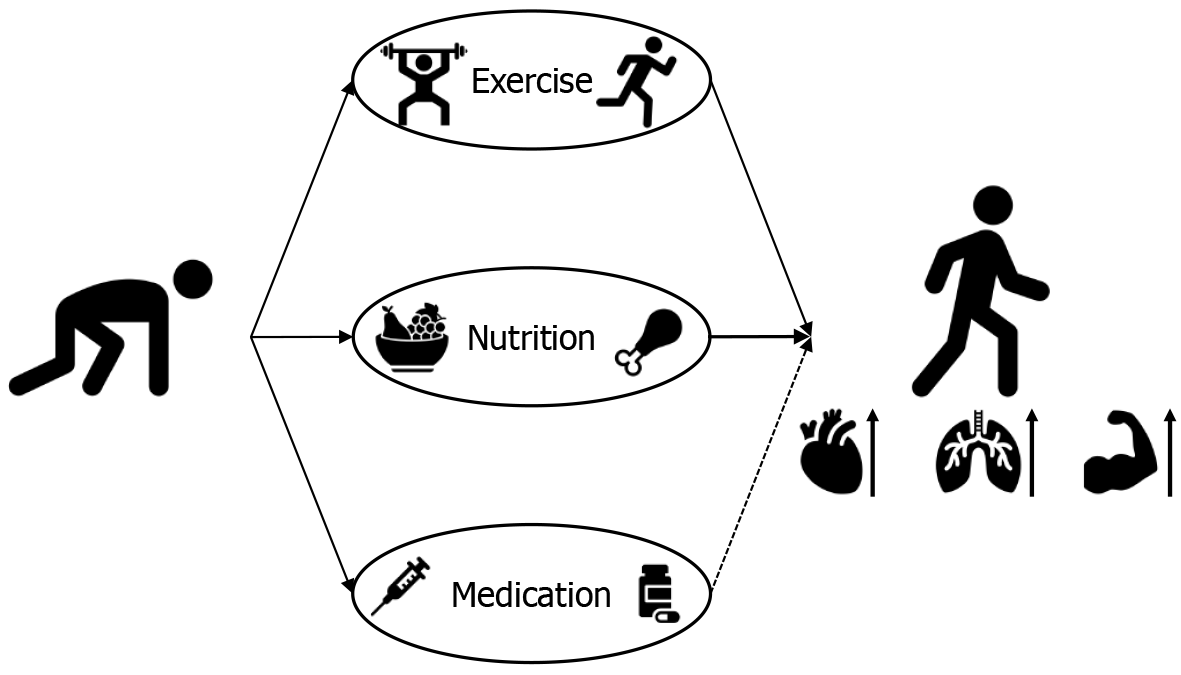
In the general population, exercise is the only established effective method to improve exercise tolerance and simultaneously yield beneficial effects in patients with HF[15,16]. Cardiac rehabilitation is available in some countries, including Japan, for patients with cardiovascular disease, including HF, but it is not widely available owing to limited access to cardiac rehabilitation facilities. Moreover, patients with HF may not necessarily be grateful to perform physical activities or exercises. Nutritional interventions and medical therapy may be alternative approaches for improving exercise tolerance. However, there is currently no drug of choice for this purpose. In this review, the literature and clinical studies on pharmacological approaches to improve exercise capacity in patients with HF are surveyed.
A summary of a systematic review and meta-analysis of guideline-directed medical therapy for HF in relation to exercise capacity in patients with HF is provided in Table 1[17-19].
| Ref. | Agent used | Inclusion criteria | Number of clinical trials | Number of participants | Duration of follow-up | Outcomes | Results | Quality assessment tool |
| Gao et al[17], 2024 | SGLT2i | RCTs published up to July 31, 2023 | 4 | 250 | 3-12 months | Peak VO2 | Significant improvement for SGLT2i | The risk of bias 2 for the included RCTs |
| 7 | 1457 | 3-9 months | 6MWD | Significant improvement | ||||
| Fukuta et al[18], 2019 | Mineralocorticoid receptor antagonist | RCTs published up to December 31, 2017 | 3 | 633 | 6-12 months | Peak VO2 | No significant difference | The Jadad quality scale for the included RCTs |
| 4 | 594 | 6-12 months | 6MWD | No significant difference | ||||
| Bhattacharjee et al[19], 2023 | Angiotensin receptor neprilysin inhibitor | RCT published from January 1, 2010 to January 1, 2023 | 1 | 52 | 12-24 weeks | Peak VO2 | No significant difference | The risk of bias for the included RCTs and the Grading of Recommendations, Assessment, Development, and Evaluations framework for the quality of evidence for the primary outcome |
| 2 | 673 | 12-24 weeks | 6MWD | No significant difference |
SGLT2 inhibitors reduce cardiovascular events such as incident cardiovascular death and HF hospitalization[20-22]. Because SGLT2 inhibitors promote urinary glucose excretion, sodium excretion, and water diuresis, they may reduce cardiac workload by decreasing the circulating plasma volume through diuresis, which can also reduce blood pressure and peripheral vascular resistance. The beneficial effects of SGLT2 inhibitors, other than diuresis, include increased cardiac energy production through increased cardiac ketone utilization, glucose oxidation, and fatty acid oxidation, which may be exerted by increasing the efficiency of energy utilization in the heart. SGLT2 inhibitors may improve exercise tolerance through cardiac energy utilization. A systematic review and meta-analysis of 17 studies, including 23523 patients with HF, reported that patients receiving SGLT2 inhibitors experienced significant increases in peak oxygen consumption compared to the control group[17]. In the meta-analysis, four studies included peak oxygen consumption as an outcome, and seven studies assessed the 6MWD. SGLT2 inhibitor therapy was associated with significant improvement in peak oxygen consumption [mean difference (MD): 1.61 mL/kg/minute; 95%CI: 0.59-2.63, P = 0.002] and 6MWD (MD: 13.09 m; 95%CI: 1.20-24.97, P = 0.03). This finding is of interest in that it shows that pharmacological therapy may improve exercise tolerance in patients with HF.
MRAs have both favorable prognostic and preventive effects on myocardial hypertrophy and fibrosis, which can cause left ventricular diastolic dysfunction[23,24]. The improvement in left ventricular diastolic function provided by MRAs potentially enhances exercise capacity in patients with HF. A meta-analysis of six clinical trials including 755 patients with HF with preserved left ventricular EF examined the effects of MRAs on left ventricular diastolic function, exercise capacity, and quality of life in HF with preserved EF[18]. In the meta-analysis, three trials reported the results on peak oxygen consumption, and four trials reported on the 6MWD. Although MRAs improve left ventricular diastolic function and decrease left ventricular mass, changes in exercise capacity assessed by peak oxygen consumption [weighted MD (WMD) (95%CI): 0.866 (-0.744 to 2.477), P = 0.29] and 6MWD also do not significantly differ between MRAs and the control group [WMD (95%CI): -11.9 (-26.2 to 2.26), P = 0.1].
Clinical trials of ARNI have shown prognostic benefits in individuals with HF and reduced EF. The drug increases the left ventricular EF[25,26] and could potentially improve peripheral vasodilation and blood flow to the skeletal muscle through its inhibitory effect on neprilysin, which potentially improves exercise capacity in patients with HF. A systematic review of eight randomized clinical trials of ARNI in HF with reduced EF reported the results of descriptive analysis of exercise capacity, because the included trials had disparities in reporting the effects of ARNI on peak oxygen consumption and 6MWD[19]. The review reported that ARNI, compared to enalapril, did not improve exercise capacity, expressed as peak oxygen consumption or 6MWD.
Beta-blockers are essential HF medications with mortality benefits through the reduction in heart rate, systolic blood pressure, and myocardial contractility, resulting in a decrease in myocardial oxygen consumption, whereas the negative chronotropic effects of the agents can impair exercise tolerance. The withdrawal of beta-blockers is associated with an increase in peak oxygen consumption in patients with HF and a preserved EF[27,28]. A systematic review and meta-analysis of the effects of beta-blocker withdrawal on exercise capacity in patients with HF and preserved EF is ongoing[29].
Ivabradine is a unique pharmacological agent that specifically reduces heart rate and potentially improves cardiac overload in patients with HF[30]. The findings on the effects of ivabradine treatment on exercise capacity in patients with HF are inconsistent. Although a meta-analysis of four randomized controlled trials shows that ivabradine did not significantly change exercise capacity expressed by peak oxygen consumption (three trials included the MD of 1.02 and the 95%CI of -2.51 to 4.56) and 6MWD (only one trial included the MD of -3.80 and the 95%CI of -22.03 to 14.43) in individuals with HF and preserved EF[31], the meta-analysis of six other randomized controlled trials and one subgroup analysis shows that addition of ivabradine to standard HF therapy increased exercise capacity measured by exercise duration (MD of 8.52 and the 95%CI of 0.09-16.94) in patients with HF and reduced EF, although the results were from two trials of the six trials[32]. The inconsistent results of the two meta-analyses can be explained by different populations with different types of HF (reduced or preserved left ventricular EF). The measurements of exercise capacity also differed between the two meta-analyses, which may have undermined the validity of the findings.
A clinical trial focusing on the effect of imeglimin on exercise capacity is ongoing[33]. Imeglimin, a novel antidiabetic agent, lowers blood glucose by suppressing gluconeogenesis in the liver, increasing glucose utilization in skeletal mu
This article summarized the available evidence on HF medications for the enhancement of exercise capacity and described other candidate drugs that may positively affect exercise capacity in patients with HF. An alternative approach to physical activity and exercise to improve exercise tolerance is desired for a subset of patients and the general popu
| 1. | Cattadori G, Segurini C, Picozzi A, Padeletti L, Anzà C. Exercise and heart failure: an update. ESC Heart Fail. 2018;5:222-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 145] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 2. | Del Buono MG, Arena R, Borlaug BA, Carbone S, Canada JM, Kirkman DL, Garten R, Rodriguez-Miguelez P, Guazzi M, Lavie CJ, Abbate A. Exercise Intolerance in Patients With Heart Failure: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73:2209-2225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 329] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 3. | Reddy YNV, Rikhi A, Obokata M, Shah SJ, Lewis GD, AbouEzzedine OF, Dunlay S, McNulty S, Chakraborty H, Stevenson LW, Redfield MM, Borlaug BA. Quality of life in heart failure with preserved ejection fraction: importance of obesity, functional capacity, and physical inactivity. Eur J Heart Fail. 2020;22:1009-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377-381. [PubMed] |
| 5. | ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6981] [Cited by in RCA: 8640] [Article Influence: 360.0] [Reference Citation Analysis (0)] |
| 6. | Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, Forman D, Franklin B, Guazzi M, Gulati M, Keteyian SJ, Lavie CJ, Macko R, Mancini D, Milani RV; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Peripheral Vascular Disease; Interdisciplinary Council on Quality of Care and Outcomes Research. Clinician's Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:191-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1144] [Cited by in RCA: 1502] [Article Influence: 93.9] [Reference Citation Analysis (0)] |
| 7. | Bassett DR Jr, Howley ET. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med Sci Sports Exerc. 2000;32:70-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1095] [Cited by in RCA: 1315] [Article Influence: 50.6] [Reference Citation Analysis (0)] |
| 8. | Bauersachs J. Heart failure drug treatment: the fantastic four. Eur Heart J. 2021;42:681-683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 180] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 9. | Writing Committee Members; Kittleson MM, Breathett K, Ziaeian B, Aguilar D, Blumer V, Bozkurt B, Diekemper RL, Dorsch MP, Heidenreich PA, Jurgens CY, Khazanie P, Koromia GA, Van Spall HGC. 2024 Update to the 2020 ACC/AHA Clinical Performance and Quality Measures for Adults With Heart Failure: A Report of the American Heart Association/American College of Cardiology Joint Committee on Performance Measures. J Am Coll Cardiol. 2024;84:1123-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 10. | Beghini A, Sammartino AM, Papp Z, von Haehling S, Biegus J, Ponikowski P, Adamo M, Falco L, Lombardi CM, Pagnesi M, Savarese G, Metra M, Tomasoni D. 2024 update in heart failure. ESC Heart Fail. 2025;12:8-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 97] [Article Influence: 97.0] [Reference Citation Analysis (0)] |
| 11. | Kraai IH, Vermeulen KM, Luttik ML, Hoekstra T, Jaarsma T, Hillege HL. Preferences of heart failure patients in daily clinical practice: quality of life or longevity? Eur J Heart Fail. 2013;15:1113-1121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | Stevenson LW, Hellkamp AS, Leier CV, Sopko G, Koelling T, Warnica JW, Abraham WT, Kasper EK, Rogers JG, Califf RM, Schramm EE, O'Connor CM. Changing preferences for survival after hospitalization with advanced heart failure. J Am Coll Cardiol. 2008;52:1702-1708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 135] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Al-Noumani H, Al-Harrasi M, Al Zaabi O, Natarajan J. Predictors of health-related quality of life in patients with non-communicable diseases: A national cross-section study. Appl Nurs Res. 2022;64:151566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Naito R, McKee M, Leong D, Bangdiwala S, Rangarajan S, Islam S, Yusuf S. Social isolation as a risk factor for all-cause mortality: Systematic review and meta-analysis of cohort studies. PLoS One. 2023;18:e0280308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 61] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 15. | Alvarez P, Hannawi B, Guha A. Exercise And Heart Failure: Advancing Knowledge And Improving Care. Methodist Debakey Cardiovasc J. 2016;12:110-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Piepoli MF, Conraads V, Corrà U, Dickstein K, Francis DP, Jaarsma T, McMurray J, Pieske B, Piotrowicz E, Schmid JP, Anker SD, Solal AC, Filippatos GS, Hoes AW, Gielen S, Giannuzzi P, Ponikowski PP. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail. 2011;13:347-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 549] [Cited by in RCA: 506] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 17. | Gao M, Bhatia K, Kapoor A, Badimon J, Pinney SP, Mancini DM, Santos-Gallego CG, Lala A. SGLT2 Inhibitors, Functional Capacity, and Quality of Life in Patients With Heart Failure: A Systematic Review and Meta-Analysis. JAMA Netw Open. 2024;7:e245135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 47] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 18. | Fukuta H, Goto T, Wakami K, Kamiya T, Ohte N. Effects of mineralocorticoid receptor antagonists on left ventricular diastolic function, exercise capacity, and quality of life in heart failure with preserved ejection fraction: a meta-analysis of randomized controlled trials. Heart Vessels. 2019;34:597-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Bhattacharjee P, Khan Z. Sacubitril/Valsartan in the Treatment of Heart Failure With Reduced Ejection Fraction Focusing on the Impact on the Quality of Life: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Cureus. 2023;15:e48674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE; EMPA-REG OUTCOME Investigators. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015;373:2117-2128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7124] [Cited by in RCA: 8734] [Article Influence: 794.0] [Reference Citation Analysis (2)] |
| 21. | Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR; CANVAS Program Collaborative Group. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med. 2017;377:644-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4498] [Cited by in RCA: 5663] [Article Influence: 629.2] [Reference Citation Analysis (0)] |
| 22. | Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Ruff CT, Gause-Nilsson IAM, Fredriksson M, Johansson PA, Langkilde AM, Sabatine MS; DECLARE–TIMI 58 Investigators. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med. 2019;380:347-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4652] [Cited by in RCA: 4526] [Article Influence: 646.6] [Reference Citation Analysis (0)] |
| 23. | Suzuki G, Morita H, Mishima T, Sharov VG, Todor A, Tanhehco EJ, Rudolph AE, McMahon EG, Goldstein S, Sabbah HN. Effects of long-term monotherapy with eplerenone, a novel aldosterone blocker, on progression of left ventricular dysfunction and remodeling in dogs with heart failure. Circulation. 2002;106:2967-2972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 152] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Susic D, Varagic J, Ahn J, Matavelli L, Frohlich ED. Long-term mineralocorticoid receptor blockade reduces fibrosis and improves cardiac performance and coronary hemodynamics in elderly SHR. Am J Physiol Heart Circ Physiol. 2007;292:H175-H179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR; PARADIGM-HF Investigators and Committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4078] [Cited by in RCA: 4981] [Article Influence: 415.1] [Reference Citation Analysis (0)] |
| 26. | Ganesananthan S, Shah N, Shah P, Elsayed H, Phillips J, Parkes A, Morgan A, Yousef Z. Real-world treatment switching to sacubitril/valsartan in patients with heart failure with reduced ejection fraction: A cohort study. Open Heart. 2020;7:e001305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Palau P, Seller J, Domínguez E, Sastre C, Ramón JM, de La Espriella R, Santas E, Miñana G, Bodí V, Sanchis J, Valle A, Chorro FJ, Llácer P, Bayés-Genís A, Núñez J. Effect of β-Blocker Withdrawal on Functional Capacity in Heart Failure and Preserved Ejection Fraction. J Am Coll Cardiol. 2021;78:2042-2056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 176] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 28. | Palau P, de la Espriella R, Seller J, Santas E, Domínguez E, Bodí V, Sanchis J, Núñez E, Bayés-Genís A, Bertomeu-González V, Meyer M, Núñez J. β-Blocker Withdrawal and Functional Capacity Improvement in Patients With Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2024;9:392-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 43] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 29. | Fukuta H, Goto T, Kamiya T. Effects of beta-blocker withdrawal in patients with heart failure with preserved ejection fraction: A protocol for systematic review and meta-analysis. PLoS One. 2023;18:e0294347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Koruth JS, Lala A, Pinney S, Reddy VY, Dukkipati SR. The Clinical Use of Ivabradine. J Am Coll Cardiol. 2017;70:1777-1784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 112] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 31. | Conceição LSR, Gois C, Fernandes RES, Souza DS, Júnior MBG, Carvalho VO. Effect of ivabradine on exercise capacity in individuals with heart failure with preserved ejection fraction. Heart Fail Rev. 2021;26:157-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 32. | Bryan Richard S, Huang B, Liu G, Yang Y, Luo S. Impact of ivabradine on the cardiac function of chronic heart failure reduced ejection fraction: Meta-analysis of randomized controlled trials. Clin Cardiol. 2021;44:463-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 33. | Naito R. Exploratory trial to examine the effectiveness of Imetriamine in diabetic-associated heart failure. [accessed 2025 August 13]. In: Japan Registry of Clinical trials. Available from: https://jrct.mhlw.go.jp/latest-detail/jRCTs031220712. |
| 34. | Hallakou-Bozec S, Vial G, Kergoat M, Fouqueray P, Bolze S, Borel AL, Fontaine E, Moller DE. Mechanism of action of Imeglimin: A novel therapeutic agent for type 2 diabetes. Diabetes Obes Metab. 2021;23:664-673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 131] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/