Published online Feb 26, 2024. doi: 10.4330/wjc.v16.i2.73
Peer-review started: December 20, 2023
First decision: January 11, 2024
Revised: January 16, 2024
Accepted: February 1, 2024
Article in press: February 1, 2024
Published online: February 26, 2024
Processing time: 63 Days and 2.6 Hours
Point-of-care ultrasound (POCUS) of the internal jugular vein (IJV) offers a non-invasive means of estimating right atrial pressure (RAP), especially in cases where the inferior vena cava is inaccessible or unreliable due to conditions such as liver disease or abdominal surgery. While many clinicians are familiar with visually assessing jugular venous pressure through the internal jugular vein, this method lacks sensitivity. The utilization of POCUS significantly enhances the visualization of the vein, leading to a more accurate identification. It has been demonstrated that combining IJV POCUS with physical examination enhances the specificity of RAP estimation. This review aims to provide a comprehensive summary of the various sonographic techniques available for estimating RAP from the internal jugular vein, drawing upon existing data.
Core Tip: Point of care ultrasound of the internal jugular vein serves as a non-invasive tool to evaluate right atrial pressure. This is particularly useful when neck vein inspec
- Citation: Chayapinun V, Koratala A, Assavapokee T. Seeing beneath the surface: Harnessing point-of-care ultrasound for internal jugular vein evaluation. World J Cardiol 2024; 16(2): 73-79
- URL: https://www.wjgnet.com/1949-8462/full/v16/i2/73.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i2.73
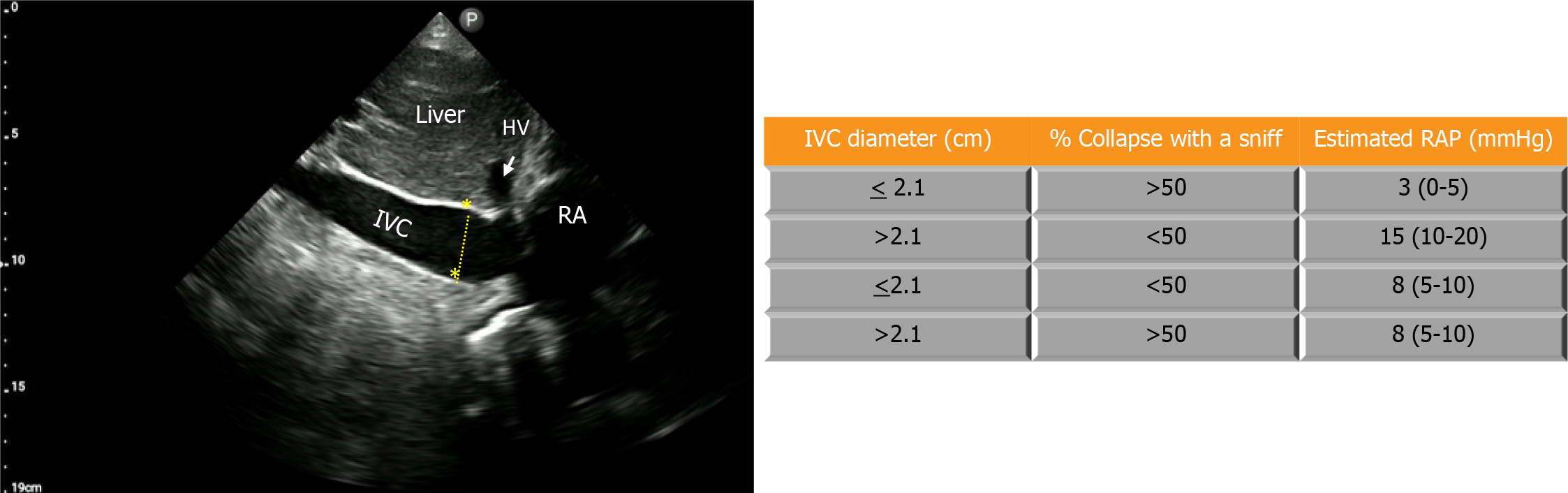
An accurate assessment of hemodynamic status at the bedside is of utmost importance in guiding proper management through altering blood volume and cardiac output, especially in critically ill patients. Central venous pressure (CVP) is a physiologic parameter that is used to assess cardiac preload within this evaluation. CVP is identical to right atrial pressure (RAP) in the absence of vena caval obstruction, and these terms are often used interchangeably. Assessing CVP clinically by performing a neck veins examination can be challenging at times and yield low sensitivity, especially in the elderly, obese, and short-necked patients[1-4]. The gold standard for measuring CVP is via inserting a central venous catheter (CVC) into the superior vena cava, however, this method is invasive, time-consuming, and can cause serious complications[4-6]. With the help of point-of-care ultrasound (POCUS), RAP can be non-invasively measured through various methods including using compression ultrasound on the forearm vein[7], evaluation of the inferior vena cava (IVC), and evaluation of the internal jugular vein (IJV). The most common method is the evaluation of IVC diameter and collapsibility[8,9] (Figure 1). However, the association between IVC parameters and RAP is moderate and lacks reliability in mechanically ventilated individuals or those with abdominal compartment syndrome[10]. Moreover, imaging the IVC can be challenging in situations like morbidly obese individuals, those unable to recline, patients with cirrhosis, ascites, or those who have undergone recent abdominal surgery[11]. Owing to its location and convenient accessibility, IJV POCUS presents a viable alternative in such instances. Unlike visual inspection, where identifying the vein can be difficult in many cases, POCUS makes the IJV easily visible, saving time for physicians and improving the accuracy of the examination[12,13].
Multiple techniques have been described to assess CVP by IJV ultrasound. Based on available data, these methods encompass measuring the vertical height of the blood column in the IJV[13-16], utilizing the IJV height-to-width ratio (aspect ratio)[17,18], IJV collapsibility index (IJV-CI)[13,17,19-22], IJV distensibility index[23], measuring the maximal anteroposterior diameter of the IJV (AP-IJV Dmax)[18,24], calculating the difference in the percentage of the IJV cross-sectional area (IJV-CSA) or diameter before and after the Valsalva maneuver[25,26], and combining IJV vertical height with right atrial depth measured with echocardiography[27,28].
The first technique, pioneered by Lipton[14], uses POCUS to visualize the height of the blood column in the IJV above the sternal angle of Louis where a venous collapse is seen (the ‘wine bottle’ or ‘paint brush’ appearance), thereby being able to measure the height of the IJV more accurately than compared to only performing neck veins examination (Figure 2). The height is then added to the hypothesized right atrial depth below the sternum of 5 cm to calculate the RAP, abiding by the doctrine of Sir Thomas Lewis, who first proposed the use of neck veins examination in 1930. This method’s accuracy is questionable, owing to the presumed right atrial depth of 5 cm, which is proven to be inaccurate[27,29]. In a study by Deol et al[30] ultrasound-assisted assessment of the column height underestimated CVP by 4.7 cm H2O, whereas visual inspection underestimated it by 6.1 cm H2O. Moreover, this approach can be time consuming as it requires two tools to assess the height of the column from the sternal angle (e.g., two rulers, a pen and a ruler, or a tongue depressor and a ruler or tape, commonly employed by physicians at the bedside), further compromising measurement accuracy[31].
The second technique uses the height-to-width ratio (aspect ratio) to estimate the CVP as a binary variable (e.g., </> 10 mmHg), without precisely quantifying it. The transducer is positioned at the level of the cricoid cartilage in the transverse plane, then the height (anteroposterior diameter) and the width (transverse diameter) are measured to obtain the aspect ratio. A ratio of < 0.75 has shown to correlate with RAP of < 10 mmHg with a sensitivity and specificity of 62% and 67% respectively in one study[17]. This method yields mixed results, and its utility is currently not well-demonstrated[18].
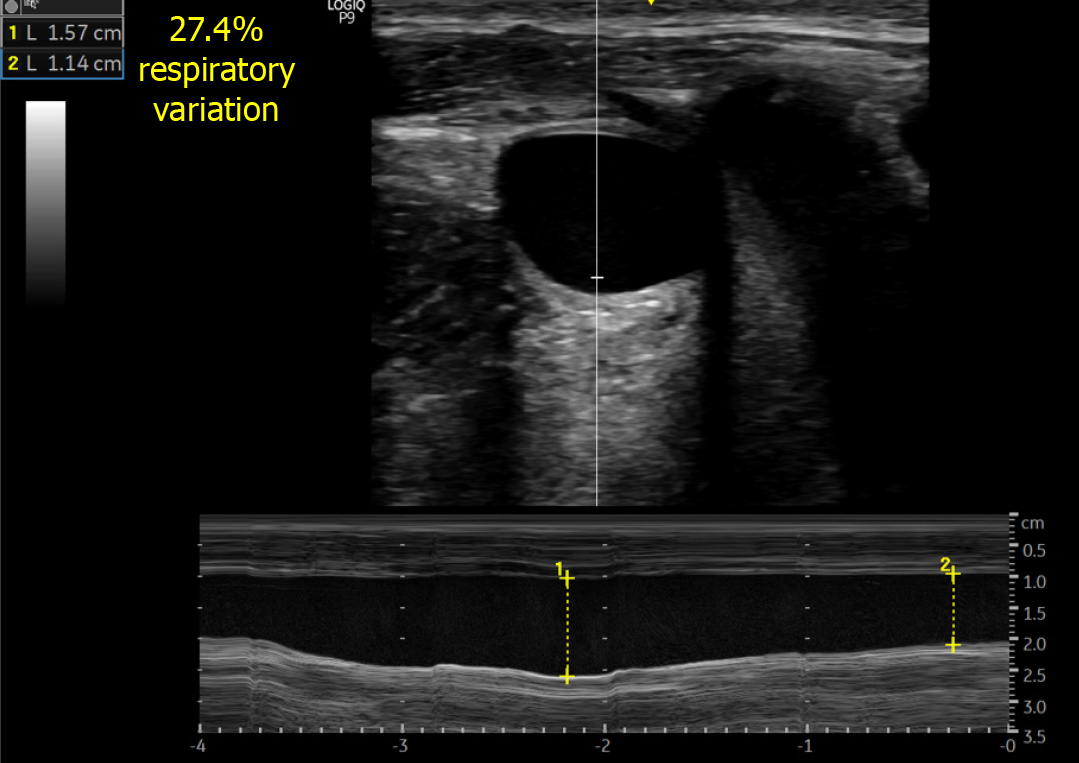
The third technique uses the collapsibility index of IJV (IJV-CI) to estimate RAP. The IJV-CI is calculated by its respiratory variation, (IJVmax – IJVmin)/IJVmax expressed in percentage (Figure 3). The actual RAP cannot be quantified, but studies[13,21,22] have shown that an IJV-CI of approximately ≤ 30% signifies an elevated CVP of ≥ 8 mmHg, demonstrating good sensitivity and specificity. Worthy of particular mention, in a study by Leal-villarreal et al[21] in patients with cirrhosis, IJV-CI (anteroposterior diameter 2 cm above the sternoclavicular joint) ≤ 24.8% was better at predicting a CVP ≥ 8 mmHg with 100% sensitivity and 97.1% specificity outperforming IVC POCUS. In this cohort, IVC POCUS was unattainable in 18% of the cases correlating with our real-life experience in cirrhotic patients.
The fourth technique uses the IJV distensibility index to predict the fluid responsiveness in patients undergoing mechanical ventilation. IJV is imaged at the cricoid cartilage level in the transverse plane and the distensibility index is calculated by (IJVmax – IJVmin)/IJVmin, expressed in percentage. In one study, an IJV distensibility index of > 18% before volume challenge (7 mL/kg crystalloid) had an 80% sensitivity and 85% specificity to predict fluid responsiveness[23]. While this technique does not quantify the RAP, it could be a valuable adjunct to other hemodynamic parameters in assessing fluid status in mechanically ventilated patients.
The fifth technique uses the IJV maximal anteroposterior diameter (AP-IJV Dmax) to predict the RAP whether it is low (< 8 mmHg) or high. Similar to the second technique of acquiring the aspect ratio, the transducer is positioned transversely 2 cm above the clavicle, at end-expiration and the diameter is collected to correlate with RAP. It has been shown that AP-IJV Dmax has the best correlation with RAP, the best validity in predicting its values, and a very good inter-rater reliability[24] along with its accuracy in predicting low RAP of < 8 mmHg[18].
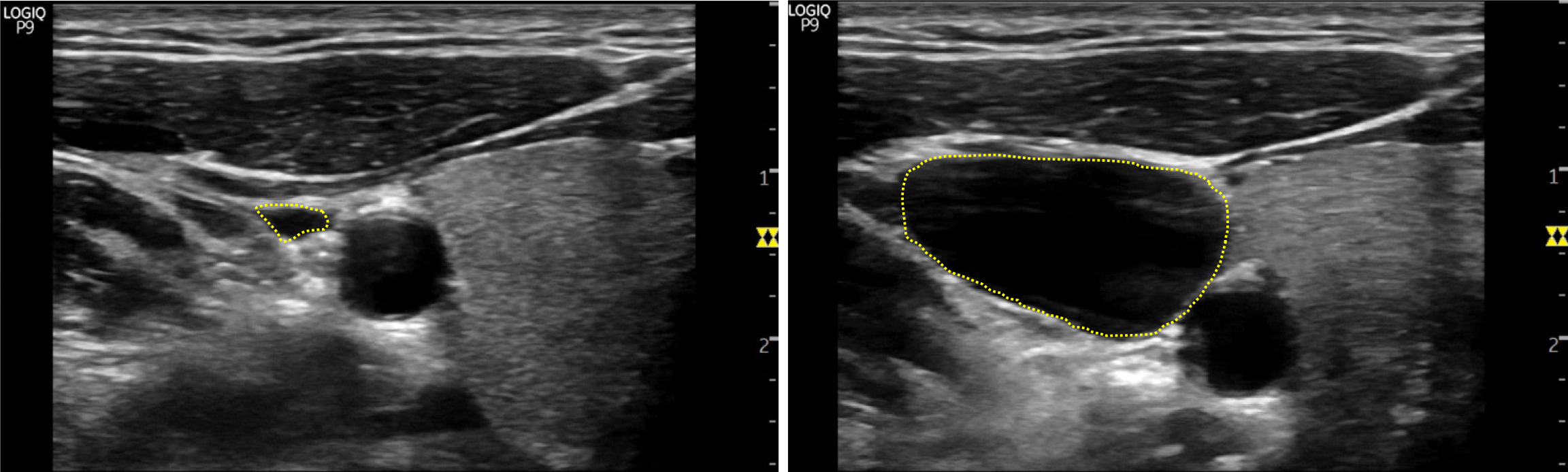
The sixth technique uses the difference in the percentage of the IJV cross-sectional area (IJV-CSA) before and after the Valsalva maneuver to assess for RAP. The Valsalva maneuver increases the IJV-CSA by about 20%-30% in patients with normal RAP, and it is assumed that in volume-overloaded patients with a decrease in venous compliance, the increase in IJV-CSA will be blunted. This technique measures the patient’s IJV-CSA at the vertical column height where a venous collapse is seen and re-measures that same parameter while the patient performs the Valsalva maneuver, then calculates the difference in the percentage of the IJV-CSA (Figures 4 and 5). One study[25] found that a < 17% increase in IJV-CSA with Valsalva predicted elevated RAP (≥ 12 mmHg) with 90% sensitivity, 74% specificity, and a 94% negative predictive value. Alternatively, the ratio between maximum IJV diameter during Valsalva maneuver and diameter at rest (JVD ratio) < 4 has also shown to predict elevated RAP[26].
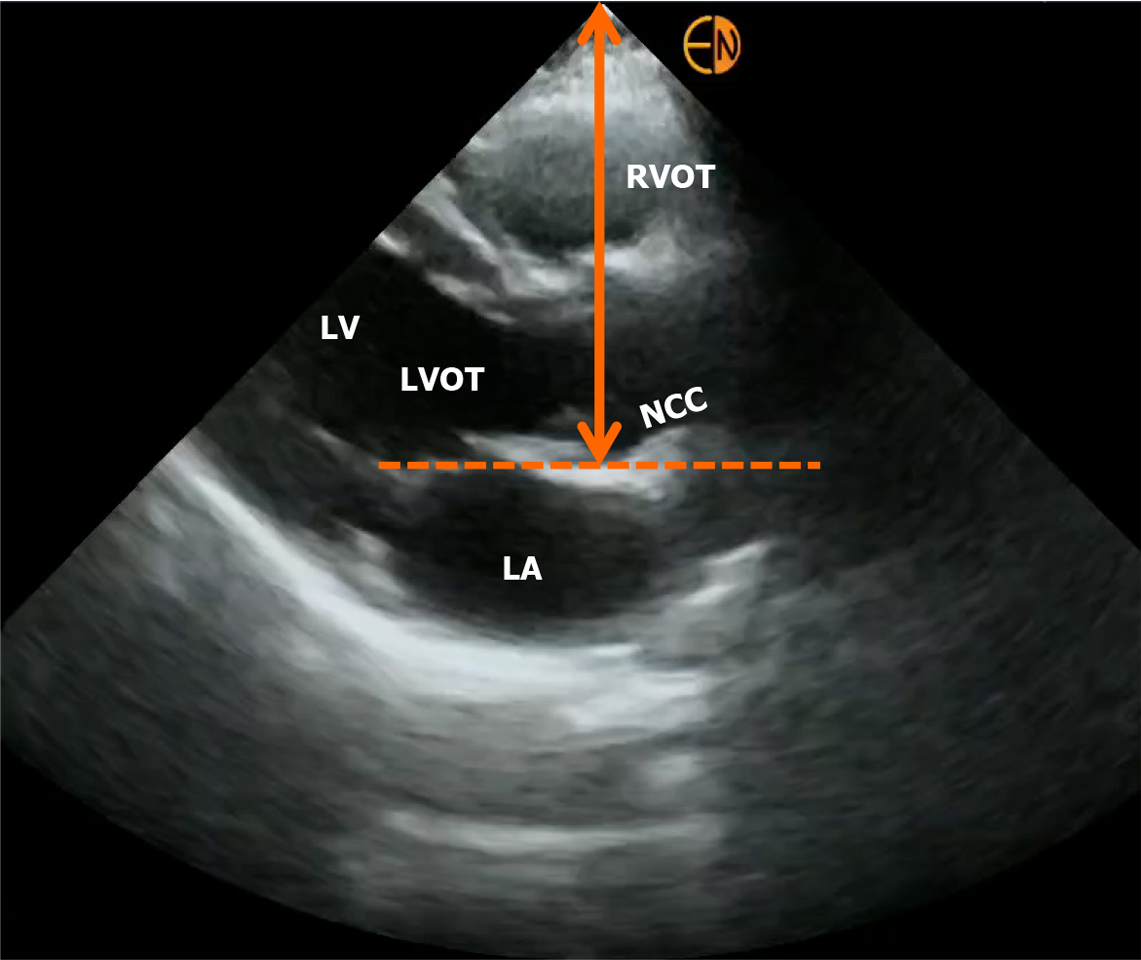
Another recently described technique uses the IJV vertical height combined with right atrial depth measured with echocardiography to quantify the RAP. While similar to the first technique in principle, this approach enhances accuracy by directly measuring the right atrial depth instead of relying on the assumed 5 cm. It involves marking the highest point of the venous collapse (wine bottle sign) and then performing a focused cardiac ultrasound to visualize the heart in long axis (parasternal long axis view). Right atrial depth is measured from the surface to the location of the non-coronary cusp of the aortic valve attachment to the posterior left ventricular outflow tract (Figure 6). The two parameters, the column height, and the right atrial depth, are then added together for an estimation of the RAP in cm H2O, later converted to mmHg. This method predicted actual RAP within 3 mmHg 74% of the time when compared to cardiac catheterization-derived value[27].
In an alternative technique described by Xing et al[28], the initial step of measuring the height of collapse point is the same but the right atrial depth is calculated using an adjusted apical 4-chamber view with the right atrium in the center of the view, where distance between the transducer contact point and the center of the right atrium is recorded. A pencil and a ruler are then used in relation to the transducer to derive the surface projection of the center of the right atrium. The RAP is then estimated by adding the IJV column height to the right atrial depth. This technique demonstrates a substantial correlation and high accuracy, with a mean difference of 0.22 mmHg in RAP compared to CVC. Nevertheless, it lacks practicality in a clinical setting where swift assessment is essential, as it involves multiple operators and the use of various measuring instruments.
With respect to estimation of RAP using IJV POCUS in mechanically ventilated patients, there is limited data. One noteworthy study is by Hilbert et al[32] in a cohort of 47 patients, where they evaluated the ratio between IJV diameter in the 30° and 0° head position (30/0 ratio). A 30/0 ratio of < 0.45 indicated a low CVP, whereas a cutoff of > 0.65 predicted a CVP ≥ 10 mmHg with reasonable accuracy.
In essence, IJV POCUS serves as a quick, non-invasive bedside tool for assessing RAP. However, the diversity in techniques requires cautious interpretation, avoiding overestimation of accuracy. Interpretation of IJV POCUS in the appropriate clinical context is crucial. Additionally, CVP is not a surrogate for volume status but just one component in bedside hemodynamic assessment, to be considered alongside other variables. For instance, Figure 7 presents an algorithm for hemodynamic assessment in cirrhotic patients with acute kidney injury, utilizing IJV for fluid tolerance assessment[33]. Future research should compare various techniques in different clinical settings to establish a standardized, practical method for routine use.
| 1. | Assavapokee T, Thadanipon K. Examination of the Neck Veins. N Engl J Med. 2020;383:e132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Jang T, Aubin C, Naunheim R, Char D. Ultrasonography of the internal jugular vein in patients with dyspnea without jugular venous distention on physical examination. Ann Emerg Med. 2004;44:160-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Donahue SP, Wood JP, Patel BM, Quinn JV. Correlation of sonographic measurements of the internal jugular vein with central venous pressure. Am J Emerg Med. 2009;27:851-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Baumann UA, Marquis C, Stoupis C, Willenberg TA, Takala J, Jakob SM. Estimation of central venous pressure by ultrasound. Resuscitation. 2005;64:193-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, Marqué S, Thuong M, Pottier V, Ramakers M, Savary B, Seguin A, Valette X, Terzi N, Sauneuf B, Cattoir V, Mermel LA, du Cheyron D; 3SITES Study Group. Intravascular Complications of Central Venous Catheterization by Insertion Site. N Engl J Med. 2015;373:1220-1229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 401] [Cited by in RCA: 496] [Article Influence: 45.1] [Reference Citation Analysis (0)] |
| 6. | Kusminsky RE. Complications of central venous catheterization. J Am Coll Surg. 2007;204:681-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 242] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 7. | Thalhammer C, Aschwanden M, Odermatt A, Baumann UA, Imfeld S, Bilecen D, Marsch SC, Jaeger KA. Noninvasive central venous pressure measurement by controlled compression sonography at the forearm. J Am Coll Cardiol. 2007;50:1584-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685-713; quiz 786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4670] [Cited by in RCA: 5497] [Article Influence: 343.6] [Reference Citation Analysis (0)] |
| 9. | Dipti A, Soucy Z, Surana A, Chandra S. Role of inferior vena cava diameter in assessment of volume status: a meta-analysis. Am J Emerg Med. 2012;30:1414-1419.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 177] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 10. | Ciozda W, Kedan I, Kehl DW, Zimmer R, Khandwalla R, Kimchi A. The efficacy of sonographic measurement of inferior vena cava diameter as an estimate of central venous pressure. Cardiovasc Ultrasound. 2016;14:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 122] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 11. | Koratala A, Kazory A. Point of Care Ultrasonography for Objective Assessment of Heart Failure: Integration of Cardiac, Vascular, and Extravascular Determinants of Volume Status. Cardiorenal Med. 2021;11:5-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 12. | Davison R, Cannon R. Estimation of central venous pressure by examination of jugular veins. Am Heart J. 1974;87:279-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 43] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Nik Muhamad NA, Safferi RS, Robertson CE. Internal Jugular Vein Height and Inferior Vena Cava Diameter Measurement using Ultrasound to Determine Central Venous Pressure: A Correlation Study. Med J Malaysia. 2015;70:63-66. [PubMed] |
| 14. | Lipton B. Estimation of central venous pressure by ultrasound of the internal jugular vein. Am J Emerg Med. 2000;18:432-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 72] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Siva B, Hunt A, Boudville N. The sensitivity and specificity of ultrasound estimation of central venous pressure using the internal jugular vein. J Crit Care. 2012;27:315.e7-315.11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Jenkins S, Knowles P, Briffa N. Portable ultrasound assessment of jugular venous pressure is an accurate method for estimating volaemic status in patients with cardiac disease. J Ultrasound. 2022;25:939-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 17. | Prekker ME, Scott NL, Hart D, Sprenkle MD, Leatherman JW. Point-of-care ultrasound to estimate central venous pressure: a comparison of three techniques. Crit Care Med. 2013;41:833-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Parenti N, Bastiani L, Tripolino C, Bacchilega I. Ultrasound imaging and central venous pressure in spontaneously breathing patients: a comparison of ultrasound-based measures of internal jugular vein and inferior vena cava. Anaesthesiol Intensive Ther. 2022;54:150-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 19. | Unluer EE, Kara PH. Ultrasonography of jugular vein as a marker of hypovolemia in healthy volunteers. Am J Emerg Med. 2013;31:173-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Wang MK, Piticaru J, Kappel C, Mikhaeil M, Mbuagbaw L, Rochwerg B. Internal jugular vein ultrasound for the diagnosis of hypovolemia and hypervolemia in acutely ill adults: a systematic review and meta-analysis. Intern Emerg Med. 2022;17:1521-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 21. | Leal-Villarreal MAJ, Aguirre-Villarreal D, Vidal-Mayo JJ, Argaiz ER, García-Juárez I. Correlation of Internal Jugular Vein Collapsibility With Central Venous Pressure in Patients With Liver Cirrhosis. Am J Gastroenterol. 2023;118:1684-1687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 22. | Vaidya GN, Kolodziej A, Stoner B, Galaviz JV, Cao X, Heier K, Thompson M, Birks E, Campbell K. Bedside ultrasound of the internal jugular vein to assess fluid status and right ventricular function: The POCUS-JVD study. Am J Emerg Med. 2023;70:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Guarracino F, Ferro B, Forfori F, Bertini P, Magliacano L, Pinsky MR. Jugular vein distensibility predicts fluid responsiveness in septic patients. Crit Care. 2014;18:647. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 24. | Parenti N, Scalese M, Palazzi C, Agrusta F, Cahill J, Agnelli G. Role of Internal Jugular Vein Ultrasound Measurements in the Assessment of Central Venous Pressure in Spontaneously Breathing Patients: A Systematic Review. J Acute Med. 2019;9:39-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 25. | Simon MA, Kliner DE, Girod JP, Moguillansky D, Villanueva FS, Pacella JJ. Detection of elevated right atrial pressure using a simple bedside ultrasound measure. Am Heart J. 2010;159:421-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Pellicori P, Shah P, Cuthbert J, Urbinati A, Zhang J, Kallvikbacka-Bennett A, Clark AL, Cleland JGF. Prevalence, pattern and clinical relevance of ultrasound indices of congestion in outpatients with heart failure. Eur J Heart Fail. 2019;21:904-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 27. | Istrail L, Kiernan J, Stepanova M. A Novel Method for Estimating Right Atrial Pressure With Point-of-Care Ultrasound. J Am Soc Echocardiogr. 2023;36:278-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 28. | Xing CY, Liu YL, Zhao ML, Yang RJ, Duan YY, Zhang LH, Sun XD, Yuan LJ, Cao TS. New method for noninvasive quantification of central venous pressure by ultrasound. Circ Cardiovasc Imaging. 2015;8:e003085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 29. | Kovacs G, Avian A, Olschewski A, Olschewski H. Zero reference level for right heart catheterisation. Eur Respir J. 2013;42:1586-1594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 120] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 30. | Deol GR, Collett N, Ashby A, Schmidt GA. Ultrasound accurately reflects the jugular venous examination but underestimates central venous pressure. Chest. 2011;139:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Mondal H, Mondal S, Das D, Alam N, Saha K. Reliability of a Jugular Venous Pressure Scale in Cardiovascular Clinical Examination. J Clin Prev Cardiol. 2020;9:61-66. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 32. | Hilbert T, Ellerkmann RK, Klaschik S, Putensen C, Thudium M. The Use of Internal Jugular Vein Ultrasonography to Anticipate Low or High Central Venous Pressure During Mechanical Ventilation. J Emerg Med. 2016;50:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Koratala A, Reisinger N. Point of Care Ultrasound in Cirrhosis-Associated Acute Kidney Injury: Beyond Inferior Vena Cava. Kidney360. 2022;3:1965-1968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Uz Zaman M, Pakistan S-Editor: Gong ZM L-Editor: A P-Editor: Zhao S