Published online Feb 26, 2024. doi: 10.4330/wjc.v16.i2.67
Peer-review started: December 10, 2023
First decision: December 19, 2023
Revised: December 21, 2023
Accepted: January 15, 2024
Article in press: January 15, 2024
Published online: February 26, 2024
Processing time: 72 Days and 11.9 Hours
Physical inactivity remains in high levels after cardiac surgery, reaching up to 50%. Patients present a significant loss of functional capacity, with prominent muscle weakness after cardiac surgery due to anesthesia, surgical incision, duration of cardiopulmonary bypass, and mechanical ventilation that affects their quality of life. These complications, along with pulmonary complications after surgery, lead to extended intensive care unit (ICU) and hospital length of stay and significant mortality rates. Despite the well-known beneficial effects of cardiac rehabilitation, this treatment strategy still remains broadly underutilized in patients after cardiac surgery. Prehabilitation and ICU early mobilization have been both showed to be valid methods to improve exercise tolerance and muscle strength. Early mobilization should be adjusted to each patient’s functional capacity with progressive exercise training, from passive mobilization to more active range of motion and resistance exercises. Cardiopulmonary exercise testing remains the gold standard for exercise capacity assessment and optimal pres
Core Tip: Cardiac rehabilitation is a medically supervised program designed to maintain or improve cardiovascular health, and should be considered as an important treatment strategy in patients after cardiac surgery. It has multiple beneficial effects on functional capacity, endothelial and skeletal muscle function, and quality of life. Recent advances have been made in cardiac rehabilitation during the last decades, including the use of artificial intelligence, simulation, telemedicine and virtual cardiac rehabilitation that improve compliance. As a result, reduced hospital readmissions and decreased healthcare costs are being observed in the modern healthcare systems.
- Citation: Kourek C, Dimopoulos S. Cardiac rehabilitation after cardiac surgery: An important underutilized treatment strategy. World J Cardiol 2024; 16(2): 67-72
- URL: https://www.wjgnet.com/1949-8462/full/v16/i2/67.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i2.67
Cardiac surgery includes a variety of procedures with coronary artery by-pass grafting, valve replacement, aortic/mitral/tricuspid valve replacement or reconstruction, heart transplantation and Bentall surgery being the most frequent among them. Patients present a loss of cognitive and exercise capacity[1], muscle mass[2] and quality of life[3,4] after cardiac surgery due to anesthesia, surgical incision, duration of cardiopulmonary bypass, and mechanical ventilation[5]. These complications, along with pulmonary complications after surgery, lead to extended intensive care unit (ICU) and hospital length of stay and significant mortality rates[5]. Physical inactivity remains high after cardiac surgery, reaching up to 49% in these patients[6]. Moreover, physical inactivity, even late after cardiac surgery, is associated with increased long-term mortality[6].
Cardiac rehabilitation is designed to improve cardiovascular health in patients with cardiovascular diseases and is recommended by guidelines as Class IA[7,8]. In cardiac surgery, cardiac rehabilitation is associated with a lower 2-year mortality[9]. Despite the well-known beneficial effects of cardiac rehabilitation after cardiac surgery, this treatment strategy still remains underutilized due to low rates of referrals, adherence and compliance. The aim of the present editorial is to highlight the role of cardiac rehabilitation in cardiac surgery and demonstrate the most recent advances in this field.
Early mobilization should be considered as an important preventive and treatment method for ICU acquired weakness in patients after cardiac surgery. Despite its safety, feasibility, beneficial effects on exercise capacity[10] and its association with reduced length of ICU stay[11], more studies are required in order to provide confirming evidence[12]. Early mobilization should be adjusted to each patient’s functional capacity, initiating from passive mobilization such as stretching, splinting, passive movements and neuromuscular electrical stimulation (NMES), and increasing the functional status with simple active range of motion and resistance exercises including sitting in a chair, leg press, squats from sitting position, walking, biking on an exercise bike, walking on stairs and inspiratory muscle training[13,14]. Passive mobilization and NMES are usually implemented in intubated patients under mechanical ventilation, high-risk patients with hemodynamic instability or patients with reduced consciousness while active-assisted range-of motion exercises, inspiratory muscle training and resistance exercises are implemented in those who need mobilization after cardiac surgery, with satisfactory level of consciousness[13,14]. In general, early mobilization has been shown safe and feasible in cardiovascular diseases[15-17] and critically ill patients[18], as well as in other medical conditions such as subarachnoid hemorrhage and external ventricular drain[19], continuous renal replacement therapy[20] and sepsis[21,22]. Beyond all its beneficial effects, early mobilization of cardiac surgery patients requires close monitoring in the ICU due to possible side effects, including significant hemodynamic changes[23]. As a result, expert multidisciplinary team approach and indi
Prehabilitation is another novel modality of rehabilitation defined as a process of improving functional capability of a patient prior to a surgical procedure. Recent studies have demonstrated that prehabilitation seems to improve functional capacity and enhance postoperative recovery in patients undergoing cardiothoracic surgery[25,26]. Moreover, prehabilitation contributes to better quality of life in patients with stable coronary artery disease awaiting cardiac surgery[27]. Growing evidence supports prehabilitation even in patients with advanced heart failure or extracorporeal membrane oxygenation as a bridge to left ventricle assist device or heart or lung transplantation. In these cases, prehabilitation should be performed daily for approximately 60 min including airway clearance techniques and ventilation in prone and supine position when required, and in-bed active-assisted range of motion exercises including sitting at the bedside, standing balance and tolerance, rolling, stretching, positioning in bed, strengthening and reconditioning exercises in the supine position, bedside cycling, inspiratory muscle training, out-of-bed activities such as standing at the bedside, strength of standing force, sitting on the edge of the bed and transfer from bed to chair, exercises in the sitting position on the edge of the bed, aerobic training on a cycle ergometer or a treadmill and inspiratory muscle training according to patient's functional capacity[14].
Exercise prescription is a quite complex procedure, especially in patients after cardiac surgery. The most difficult part is to establish the beneficial “dose” of exercise in order to achieve the maximum beneficial results and avoid harmful effects. Clinical assessment and risk stratification via transthoracic echocardiography and cardiopulmonary exercise testing (CPET) are required prior to participation in such rehabilitation programs. CPET is the gold standard for the prescription of maximum aerobic exercise intensity[28]. Monitoring of heart rate (HR) dynamics and ventilation, as well as metabolic parameters such as oxygen uptake (VO2) and carbon dioxide output (VCO2), provides objective measurements of res
During the last decade, recent advances have been made in cardiac rehabilitation. Rapidly-advanced technology is the cornerstone in the future of cardiac rehabilitation. Wearables such as fitness bands and smartwatches that monitor heart rhythm during exercise in order to detect arrhythmias are used by 5% to 11% of the world’s adult population[31]. Intelligent computing including artificial intelligence (AI) and complex modeling are now increasingly used in biologic systems so that to create individualized rehabilitation programs[32]. Specifically, AI could estimate and quantify risk assessment of patients before and after cardiac surgery via special algorithms, using CPET, anaerobic threshold quantification, biomarkers and frailty parameters. Moreover, it could be a useful tool to predict mortality and morbidity[33], and detect dysrhythmias in electrocardiography during rehabilitation with promising results in accuracy and speed of interpretation[34,35], as well as in more advanced imaging such as echocardiography[36] and magnetic resonance imaging[37]. Other significant variables, including simulation and telemedicine, could be valuable for solving access problems due to disparities, disabilities, long physical distance from health care centers, and lack of expertise and spe
Cardiac rehabilitation, with its traditional form, is an individualized, patient-centered program. However, the future of cardiac rehabilitation will include more options for participants with in-person visits, virtual one-on-one visits, virtual group visits, and asynchronous exercise with or without remote monitoring[40]. The choice whether the participation will include exclusively one delivery mode or a hybrid of 2 or more delivery modes depends on many variables related with the participants, such as their physical status, their opportunity of participation, the distance from the rehabilitation facilities, etc.
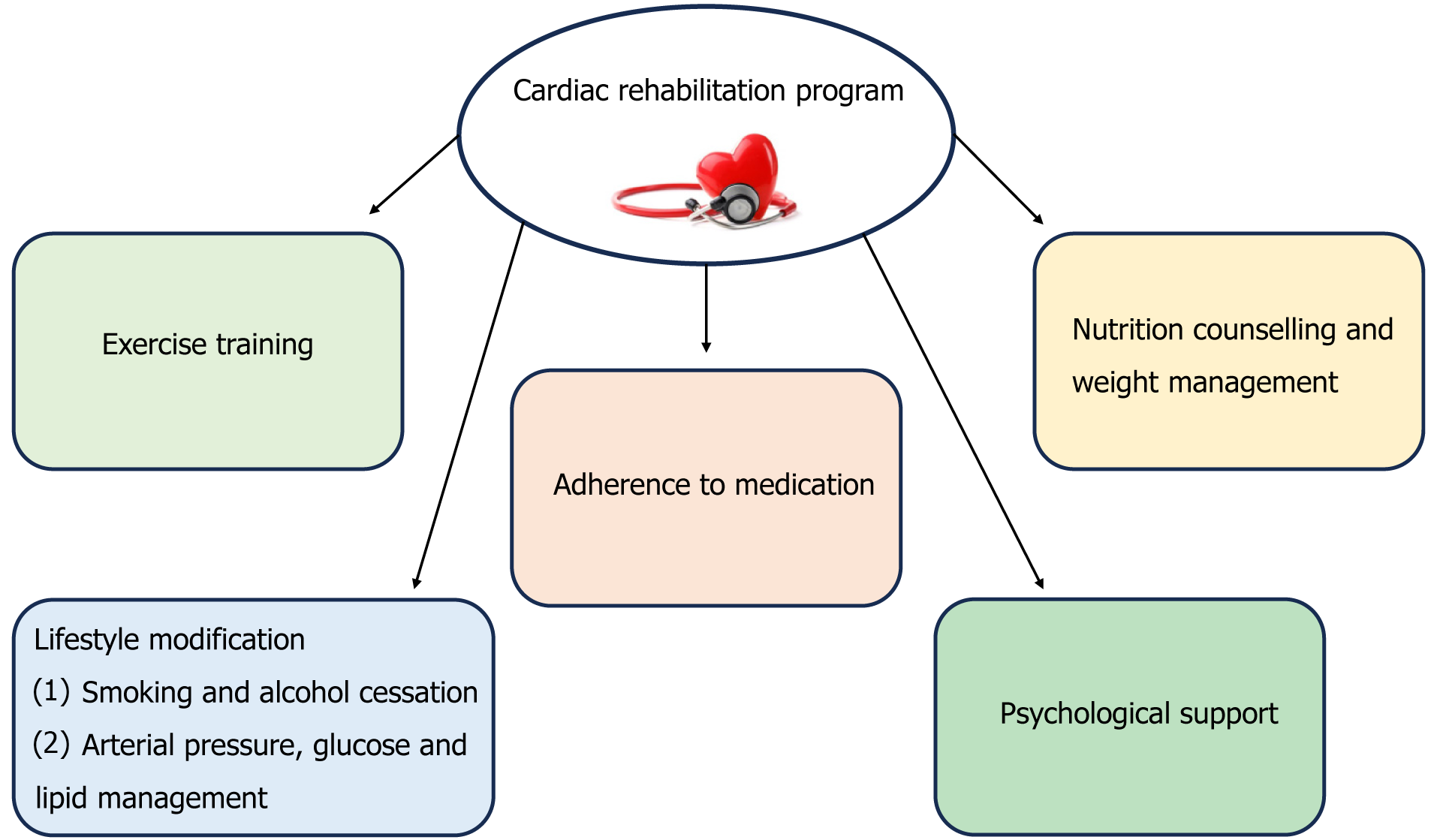
Finally, cardiac rehabilitation includes modification of previous lifestyle habits including smoking and alcohol cessation, loss of weight and medication adherence. Synchronous interventions via telemedicine could be used to improve access to these services, such as consultation with a registered dietitian or a behavioral therapist[40]. Core advances of a cardiac rehabilitation program are demonstrated in Figure 1.
Cardiac rehabilitation is a complex and multicomponent procedure that requires a multidisciplinary approach and includes physical activity promotion, health education, cardiovascular risk management and psychological support, personalized to the individual needs of patients after cardiac surgery. CPET remains the gold standard method for the prescription of optimal aerobic exercise intensity. Recent advances in cardiac rehabilitation have been made during the last decade, including the use of AI, simulation, telemedicine, and virtual cardiac rehabilitation that have improved adherence and compliance, and reduced hospital readmission, with decreased associated healthcare cost. However, new innovations are required in order to increase rates of patients’ participation and create ideal individualized protocols for each patient.
| 1. | Corrêa B, Cardoso DM. Functional capacity and mental state of patients undergoing cardiac surgery. Fisioter mov. 2017;30:805-811. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Dimopoulos S, Raidou V, Elaiopoulos D, Chatzivasiloglou F, Markantonaki D, Lyberopoulou E, Vasileiadis I, Marathias K, Nanas S, Karabinis A. Sonographic muscle mass assessment in patients after cardiac surgery. World J Cardiol. 2020;12:351-361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Cordeiro ALL, Mascarenhas HC, Landerson L, Araújo JDS, Borges DL, Melo TA, Guimarães A, Petto J. Inspiratory Muscle Training Based on Anaerobic Threshold on the Functional Capacity of Patients After Coronary Artery Bypass Grafting: Clinical Trial. Braz J Cardiovasc Surg. 2020;35:942-949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Westerdahl E, Jonsson M, Emtner M. Pulmonary function and health-related quality of life 1-year follow up after cardiac surgery. J Cardiothorac Surg. 2016;11:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Wang YC, Huang CH, Tu YK. Effects of Positive Airway Pressure and Mechanical Ventilation of the Lungs During Cardiopulmonary Bypass on Pulmonary Adverse Events After Cardiac Surgery: A Systematic Review and Meta-Analysis. J Cardiothorac Vasc Anesth. 2018;32:748-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Kim SH, Cha S, Kang S, Han K, Paik NJ, Kim WS. High prevalence of physical inactivity after heart valve surgery and its association with long-term mortality: A nationwide cohort study. Eur J Prev Cardiol. 2021;28:749-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM, Evers LR, Fang JC, Fedson SE, Fonarow GC, Hayek SS, Hernandez AF, Khazanie P, Kittleson MM, Lee CS, Link MS, Milano CA, Nnacheta LC, Sandhu AT, Stevenson LW, Vardeny O, Vest AR, Yancy CW. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e895-e1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1618] [Cited by in RCA: 1656] [Article Influence: 414.0] [Reference Citation Analysis (0)] |
| 8. | McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599-3726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8225] [Cited by in RCA: 8621] [Article Influence: 1724.2] [Reference Citation Analysis (1)] |
| 9. | Bauer TM, Yaser JM, Daramola T, Mansour AI, Ailawadi G, Pagani FD, Theurer P, Likosky DS, Keteyian SJ, Thompson MP. Cardiac Rehabilitation Reduces 2-Year Mortality After Coronary Artery Bypass Grafting. Ann Thorac Surg. 2023;116:1099-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Kanejima Y, Shimogai T, Kitamura M, Ishihara K, Izawa KP. Effect of Early Mobilization on Physical Function in Patients after Cardiac Surgery: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 11. | Raidou V, Dimopoulos S, Chatzivasiloglou F, Kourek C, Tsagari V, Pitsolis T, Papadopoulos K, Kriaras I, Tasouli A, Nanas S, Karabinis A. Early mobilization is associated with decreased mechanical ventilation and ICU length of stay following cardiac surgery. Health Res J. 2021;7:184-193. [DOI] [Full Text] |
| 12. | Chen B, Xie G, Lin Y, Chen L, Lin Z, You X, Xie X, Dong D, Zheng X, Li D, Lin W. A systematic review and meta-analysis of the effects of early mobilization therapy in patients after cardiac surgery. Medicine (Baltimore). 2021;100:e25314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 13. | Kourek C, Karatzanos E, Nanas S, Karabinis A, Dimopoulos S. Exercise training in heart transplantation. World J Transplant. 2021;11:466-479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 14. | Kourek C, Nanas S, Kotanidou A, Raidou V, Dimopoulou M, Adamopoulos S, Karabinis A, Dimopoulos S. Modalities of Exercise Training in Patients with Extracorporeal Membrane Oxygenation Support. J Cardiovasc Dev Dis. 2022;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Chen S, Lester L, Piper GL, Toy B, Saputo M, Chan W, Fischer MG, Gidea C, Kon ZN, Moazami N, Smith DE. Safety and Feasibility of an Early Mobilization Protocol for Patients with Femoral Intra-Aortic Balloon Pumps as Bridge to Heart Transplant. ASAIO J. 2022;68:714-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 16. | Kakutani N, Fukushima A, Kinugawa S, Yokota T, Oikawa T, Nishikawa M, Nakamura R, Tsukada T, Mori S, Yoshida I, Anzai T. Progressive Mobilization Program for Patients With Acute Heart Failure Reduces Hospital Stay and Improves Clinical Outcome. Circ Rep. 2019;1:123-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Semsar-Kazerooni K, Dima D, Valiquette J, Berube-Dufour J, Goldfarb M. Early Mobilization in People With Acute Cardiovascular Disease. Can J Cardiol. 2021;37:232-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Alaparthi GK, Gatty A, Samuel SR, Amaravadi SK. Effectiveness, Safety, and Barriers to Early Mobilization in the Intensive Care Unit. Crit Care Res Pract. 2020;2020:7840743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 19. | Young B, Moyer M, Pino W, Kung D, Zager E, Kumar MA. Safety and Feasibility of Early Mobilization in Patients with Subarachnoid Hemorrhage and External Ventricular Drain. Neurocrit Care. 2019;31:88-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Mayer KP, Hornsby AR, Soriano VO, Lin TC, Cunningham JT, Yuan H, Hauschild CE, Morris PE, Neyra JA. Safety, Feasibility, and Efficacy of Early Rehabilitation in Patients Requiring Continuous Renal Replacement: A Quality Improvement Study. Kidney Int Rep. 2020;5:39-47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Sakai Y, Yamamoto S, Karasawa T, Sato M, Nitta K, Okada M, Takeshige K, Ikegami S, Imamura H, Horiuchi H. Effects of early rehabilitation in sepsis patients by a specialized physical therapist in an emergency center on the return to activities of daily living independence: A retrospective cohort study. PLoS One. 2022;17:e0266348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 22. | Hickmann CE, Castanares-Zapatero D, Deldicque L, Van den Bergh P, Caty G, Robert A, Roeseler J, Francaux M, Laterre PF. Impact of Very Early Physical Therapy During Septic Shock on Skeletal Muscle: A Randomized Controlled Trial. Crit Care Med. 2018;46:1436-1443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 86] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 23. | Cassina T, Putzu A, Santambrogio L, Villa M, Licker MJ. Hemodynamic challenge to early mobilization after cardiac surgery: A pilot study. Ann Card Anaesth. 2016;19:425-432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Malone D, Ridgeway K, Nordon-Craft A, Moss P, Schenkman M, Moss M. Physical Therapist Practice in the Intensive Care Unit: Results of a National Survey. Phys Ther. 2015;95:1335-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 25. | Fernández-Costa D, Gómez-Salgado J, Castillejo Del Río A, Borrallo-Riego Á, Guerra-Martín MD. Effects of Prehabilitation on Functional Capacity in Aged Patients Undergoing Cardiothoracic Surgeries: A Systematic Review. Healthcare (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Kamarajah SK, Bundred J, Weblin J, Tan BHL. Critical appraisal on the impact of preoperative rehabilitation and outcomes after major abdominal and cardiothoracic surgery: A systematic review and meta-analysis. Surgery. 2020;167:540-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 27. | Steinmetz C, Bjarnason-Wehrens B, Baumgarten H, Walther T, Mengden T, Walther C. Prehabilitation in patients awaiting elective coronary artery bypass graft surgery - effects on functional capacity and quality of life: a randomized controlled trial. Clin Rehabil. 2020;34:1256-1267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 28. | Price KJ, Gordon BA, Bird SR, Benson AC. A review of guidelines for cardiac rehabilitation exercise programmes: Is there an international consensus? Eur J Prev Cardiol. 2016;23:1715-1733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 291] [Article Influence: 29.1] [Reference Citation Analysis (1)] |
| 29. | Gielen S, Mezzani A, Hambrecht R, Saner H. Cardiac rehabilitation. In: Camm AJ, Lüscher TF, Serruys PW, editors. The ESC Textbook of Cardiovascular Medicine Oxford. Oxford: Oxford University Press, 2009: 919-954. [DOI] [Full Text] |
| 30. | Passantino A, Dalla Vecchia LA, Corrà U, Scalvini S, Pistono M, Bussotti M, Gambarin FI, Scrutinio D, La Rovere MT. The Future of Exercise-Based Cardiac Rehabilitation for Patients With Heart Failure. Front Cardiovasc Med. 2021;8:709898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 31. | Deloitte. Global Mobile Consumer Trends 2017. [cited 8 July 2020]. Available from: https://www2.deloitte.com/il/en/pages/technology-media-and-telecommunications/articles/global-mobile-consumer-survey.html. |
| 32. | Lobdell KW, Appoo JJ, Rose GA, Ferguson B, Chatterjee S. Technological advances to enhance recovery after cardiac surgery. J Hosp Manag Health Policy. 2021;5:30. [DOI] [Full Text] |
| 33. | Allyn J, Allou N, Augustin P, Philip I, Martinet O, Belghiti M, Provenchere S, Montravers P, Ferdynus C. A Comparison of a Machine Learning Model with EuroSCORE II in Predicting Mortality after Elective Cardiac Surgery: A Decision Curve Analysis. PLoS One. 2017;12:e0169772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 118] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 34. | Al'Aref SJ, Anchouche K, Singh G, Slomka PJ, Kolli KK, Kumar A, Pandey M, Maliakal G, van Rosendael AR, Beecy AN, Berman DS, Leipsic J, Nieman K, Andreini D, Pontone G, Schoepf UJ, Shaw LJ, Chang HJ, Narula J, Bax JJ, Guan Y, Min JK. Clinical applications of machine learning in cardiovascular disease and its relevance to cardiac imaging. Eur Heart J. 2019;40:1975-1986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 289] [Article Influence: 48.2] [Reference Citation Analysis (0)] |
| 35. | Retson TA, Besser AH, Sall S, Golden D, Hsiao A. Machine Learning and Deep Neural Networks in Thoracic and Cardiovascular Imaging. J Thorac Imaging. 2019;34:192-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 36. | Alsharqi M, Woodward WJ, Mumith JA, Markham DC, Upton R, Leeson P. Artificial intelligence and echocardiography. Echo Res Pract. 2018;5:R115-R125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 122] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 37. | Arafati A, Hu P, Finn JP, Rickers C, Cheng AL, Jafarkhani H, Kheradvar A. Artificial intelligence in pediatric and adult congenital cardiac MRI: an unmet clinical need. Cardiovasc Diagn Ther. 2019;9:S310-S325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 38. | Lear SA, Singer J, Banner-Lukaris D, Horvat D, Park JE, Bates J, Ignaszewski A. Randomized trial of a virtual cardiac rehabilitation program delivered at a distance via the Internet. Circ Cardiovasc Qual Outcomes. 2014;7:952-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 39. | Kaiser Permanente. Cardiac Rehabilitation: Outpatient Program. 2020. [cited 9 July 2020]. Available from: https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.cardiac-rehabilitation-outpatient-program.hw230413. |
| 40. | Beatty AL, Beckie TM, Dodson J, Goldstein CM, Hughes JW, Kraus WE, Martin SS, Olson TP, Pack QR, Stolp H, Thomas RJ, Wu WC, Franklin BA. A New Era in Cardiac Rehabilitation Delivery: Research Gaps, Questions, Strategies, and Priorities. Circulation. 2023;147:254-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 114] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Rehabilitation
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eid N, Malaysia S-Editor: Chen YL L-Editor: A P-Editor: Zhang YL