Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.109952
Revised: June 24, 2025
Accepted: July 31, 2025
Published online: September 27, 2025
Processing time: 113 Days and 1.8 Hours
Ileocecal laterally spreading tumors (LSTs) complicated by appendiceal tubular adenoma are rare and challenging to diagnose because of the absence of typical symptoms and specific diagnostic signs. Traditionally, the primary treatment has been laparoscopic appendectomy (LA).
A 63-year-old female presented with changes in bowel habits. Colonoscopy revealed an ileocecal LST. The patient underwent endoscopic submucosal di
Ileocecal LSTs with appendiceal tubular adenomas are traditionally treated with LA. endoscopic submucosal dissection can also yield favorable outcomes.
Core Tip: Ileocecal laterally spreading tumors with appendiceal tubular adenoma are rare and hard to diagnose due to nonspecific symptoms. Traditionally treated by laparoscopic appendectomy, new research shows endoscopic submucosal dissection can be effective. This case innovatively applied sequential endoscopic submucosal dissection for high-grade dysplastic lesions at the appendiceal orifice, followed by appendectomy preserving the ileocecal valve. This approach improved postoperative quality of life and presents a novel strategy for deep-seated appendiceal lesions, addressing visualization challenges in deep lumen extension.
- Citation: Huang YH, Ma L, Cao B, Zhang YJ, Gao Q, Zhu ZM, Qiao XL, Wang L, He BG. Endoscopic and laparoscopic treatment of ileocecal laterally spreading tumor with concomitant appendiceal adenoma: A case report and review of literature. World J Gastrointest Surg 2025; 17(9): 109952
- URL: https://www.wjgnet.com/1948-9366/full/v17/i9/109952.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i9.109952
Laterally spreading tumors (LSTs) are critical lesions in colorectal cancer, with a prevalence of 0.8% in the general population undergoing colonoscopy[1]. Appendiceal tumors are rare[2]. Collins reported that among 280000 appendectomies performed in the United States, the incidence of appendiceal tumors ranged between 0.9% and 1.4%[3], with noncancerous appendiceal tumors accounting for 0.02%-0.08%[4]. Benign appendiceal tumors are often asymptomatic and incidentally detected during clinical examinations, surgery, or pathological evaluation after appendectomy, whereas malignant tumors may cause symptoms related to regional involvement, peritoneal dissemination, or metastatic disease, with acute appendicitis being the most common initial presentation[5]. We report a case of ileocecal LST complicated by an appendiceal tubular adenoma detected during a routine physical examination and managed with endoscopic sub
A 63-year-old female presented to The Affiliated Hospital of Qingdao University with a chief complaint of “changes in bowel habits for six months”.
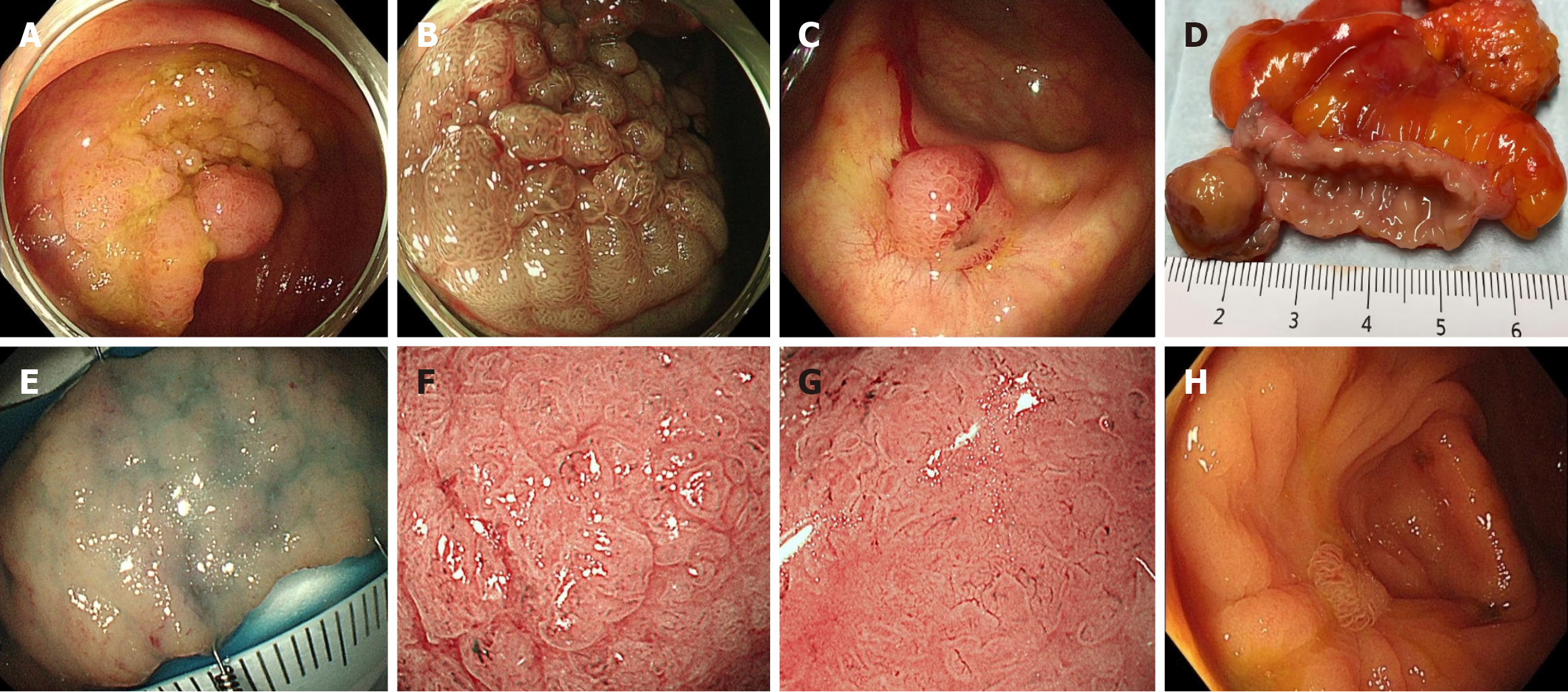
Colonoscopy revealed a 5 cm × 6 cm nodular-mixed type LST in the ileocecal region (Figure 1), with the largest nodule measuring approximately 1 cm in diameter. The appendiceal orifice was not visualized during colonoscopy, suggesting it was covered by the lesion. Pathological biopsy of the lesion revealed a tubulovillous adenoma with high-grade intraepithelial neoplasia in some areas. Given the large size of the lesion and the potential risk of invasive colon cancer, surgical resection, which typically requires right hemicolectomy, was considered. However, to avoid complications such as abdominal pain and diarrhoea associated with right hemicolectomy and maximize the preservation of colonic and ileocecal valve function, ESD of the ileocecal LST was initially performed. The pocket-creation method is used during the dissection, and we did not used any traction devices or methods to facilitate the dissection.
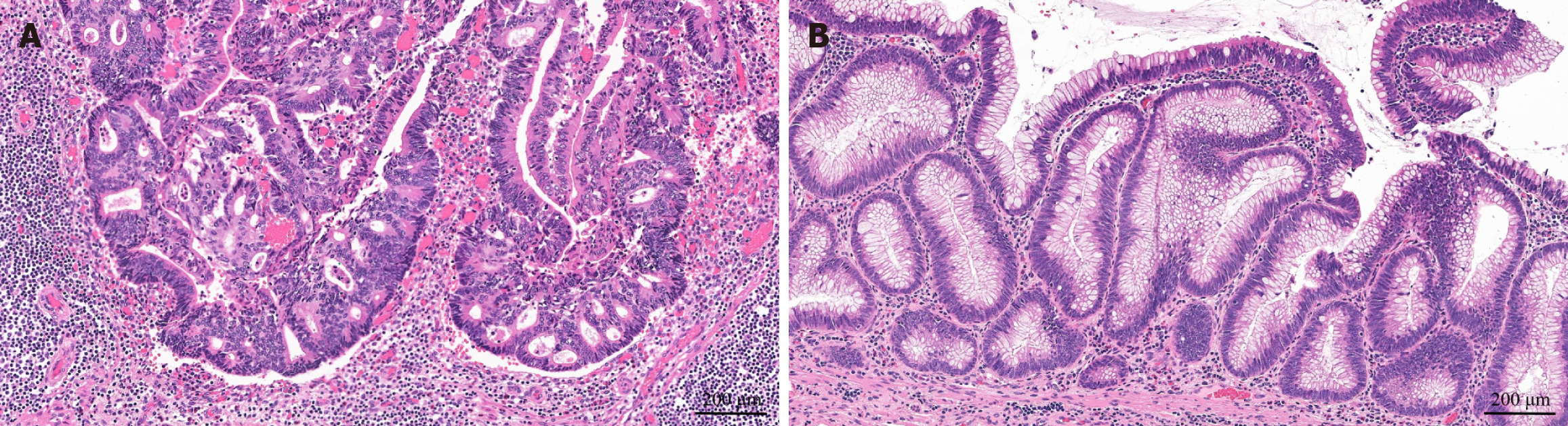
During ESD, the lesion was found to extend into the appendiceal orifice. The mucosal tissue invading the appendix was transected endoscopically, and biopsies were taken from the residual tissue at the appendiceal orifice. The final pathology of the ESD specimen revealed a tubulovillous adenoma with high-grade dysplasia and focal carcinoma, and the histologic grade is moderate differentiated (Figure 2). Surgical margins (lateral and basal) were negative. Biopsies of the appendiceal orifice mucosa revealed chronic inflammation with focal adenomatous hyperplasia. The lesion was diagnosed as early colon cancer, obviating the need for radical colectomy. Although adenomatous tissue was suspected to remain within the appendix, appendiceal ultrasound and abdominal computed tomography (CT) did not detect mucosal thickening of the appendix. After discussion with the patient, LA was planned after wound healing.
Five months later, follow-up colonoscopy revealed good healing at the surgical site. An 8 mm × 8 mm mucosal elevation was noted at the appendiceal orifice, which was clearly visualized (Figure 1). Biopsy confirmed the presence of a tubular adenoma at the appendiceal opening. LA with partial cecectomy was performed. No lymph node dissection was performed, as neither preoperative contrast-enhanced CT nor intraoperative findings showed abnormal lymph nodes. Gross examination of the resected specimen revealed the appendix with a small amount of adjacent ileocecal mucosa. Upon longitudinal sectioning of the appendix (Figure 1) and magnifying observation with narrow-band imaging, adenomatous structures were found in approximately 50% of the appendiceal lumen near the orifice (consistent with endoscopic classification; Figure 1). Final pathology confirmed a tubular adenoma with negative resection margins (Figure 2). The patient was discharged on postoperative day 3. A one-year follow-up CT scan revealed no enlarged abdominal lymph nodes, and colonoscopy confirmed well-healed mucosa (Figure 1). The timeline of diagnosis and treatment is listed in Figure 3.
The patient did have past illness.
The patient did have personal and family history.
Inspection: The abdomen is symmetric in shape, without distension or depression. Abdominal respiration is present. There is no varicose vein on the abdominal wall, and no rash, scar, gastrointestinal pattern, or peristaltic wave is observed. Palpation: The abdominal wall is soft without muscular tension. No tenderness, rebound tenderness, or abnormal mass is detected throughout the abdomen. The liver and spleen are not palpable below the costal margin. The Murphy’s sign is negative, and there is no percussion pain in the renal area. Percussion: The hepatic dullness boundary is present, located from the 5th-6th intercostal space at the right midclavicular line to the lower edge of the right costal arch. Shifting dullness is negative. Auscultation: Bowel sounds are normal, with a frequency of about 4-5 times per minute. No vascular murmur or friction sound is heard.
No obvious abnormalities were found in the patient’s laboratory examinations.
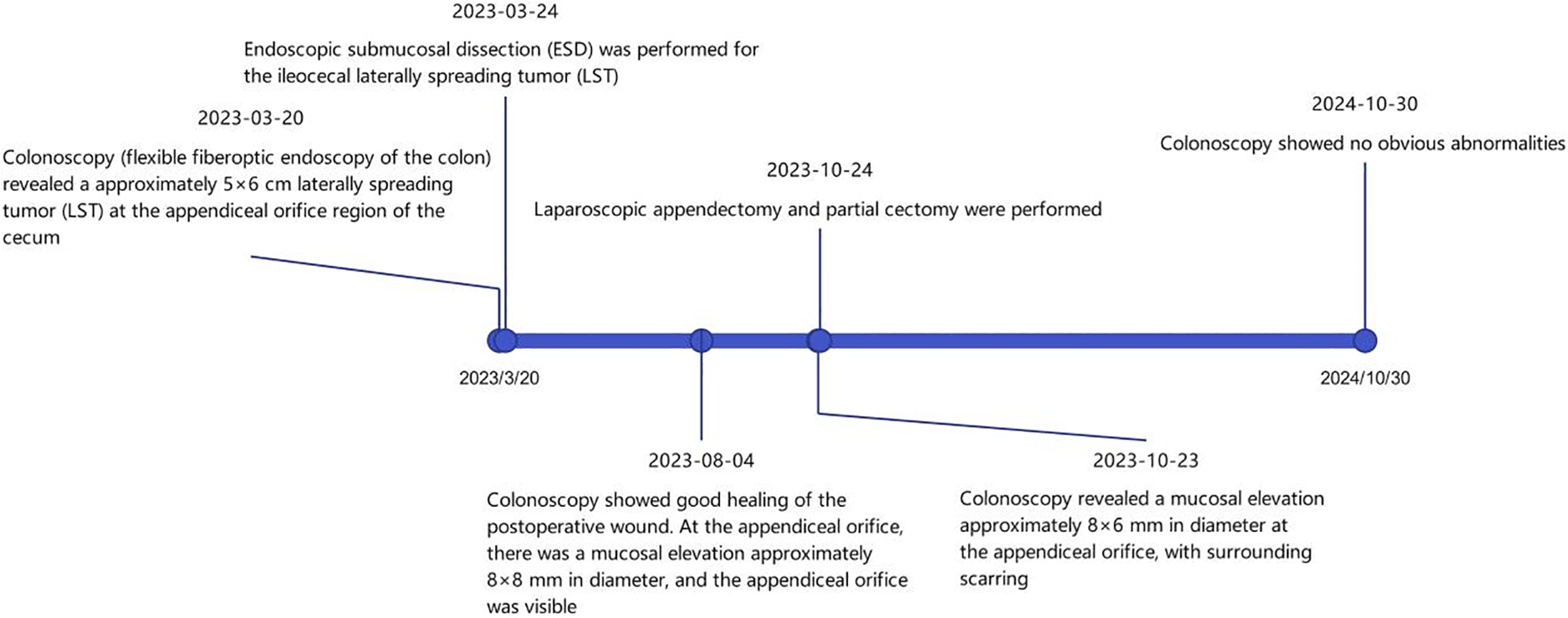
March 20, 2023: Colonoscopy (flexible fiberoptic endoscopy of the colon) revealed an approximately 5 cm × 6 cm LST at the appendiceal orifice region of the cecum. August 4, 2023: Colonoscopy showed good healing of the postoperative wound. At the appendiceal orifice, there was a mucosal elevation approximately 8 mm × 8 mm in diameter, and the appendiceal orifice was visible. October 23, 2023: Colonoscopy revealed a mucosal elevation approximately 8 mm × 6 mm in diameter at the appendiceal orifice, with surrounding scarring. October 23, 2023: Dynamic enhanced CT scan of the lower abdomen: The proximal part of the appendix shows uneven thickening with mild dilation of the appendiceal cavity. Slightly enlarged lymph node shadows are seen medially in the ileocecal region. A tumor in the appendiceal area is suspected. Please make a comprehensive diagnosis combined with clinical history and colonoscopy. October 30, 2024: Colonoscopy showed no obvious abnormalities.
Ileocecal LST with concomitant appendiceal adenoma.
March 24, 2023: ESD was performed for the ileocecal LST. October 24, 2023: LA and partial cecectomy were performed.
The appendiceal adenoma was completely resected. And one-year follow-up after surgery showed no obvious abnormalities on colonoscopy.
This case highlights a rare presentation of an ileocecal LST complicated by an appendiceal tubular adenoma. While ileocecal LSTs are not uncommon, their extension into the appendix is rare. Appendiceal epithelial tumors are observed in 0.2%-0.3% of appendectomy samples, most frequently in individuals aged 50-70 years[6], as in our case. Additionally, tubular adenoma is a rare histological type of nonmucinous epithelial tumor, accounting for only 30% of all appendiceal epithelial tumors[7].
Appendiceal tumors are often difficult to diagnose. Indeed, in most cases, these lesions are asymptomatic and incidentally detected during surgery or pathological examination of surgical samples. A review of appendiceal adenomas indicated that over 93% of these benign lesions are diagnosed postappendectomy or at autopsy[8], with occasional incidental diagnosis during radiological or endoscopic evaluation for other abdominal conditions[9]. In radiological imaging, ultrasound is a valuable modality for detecting appendiceal tumors but is highly operator-dependent and limited in its ability to assess tumor staging. Abdominal CT with or without intravenous and oral contrast is the most accurate method for detecting appendiceal tumors, with a sensitivity of up to 95%[10]. Endoscopic diagnosis is more feasible when a tumor involves the appendiceal orifice and extends to the caecal mucosa. In our case, the patient’s ileocecal LST with appendiceal extension was identified during endoscopy for changes in bowel habits.
After the diagnosis of an appendiceal adenoma, treatment is critical to avoid potential complications such as metastasis, appendicitis, or vomiting. Surgery is widely considered as the gold standard for managing appendiceal tumors[11-13]. However, surgical resection is limited by the challenge of ensuring negative margins without com
With advancements in endoscopic technology, is being applied to regions once considered too complex for endoscopic management. ESD is widely used in many specialized centers for treating superficial colonic neoplasia owing to its lower incidence of postoperative adverse events than that of traditional surgery[15]. Lesions near the appendiceal orifice (L-PAO) were initially deemed unresectable by endoscopy because of the high risks of incomplete resection, perforation, and acute appendicitis[16,17]. However, with increasing experience, endoscopic treatment of L-PAO has been demonstrated to be safe and effective[18,19].
Endoscopic mucosal resection (EMR) has been described for managing lesions involving the appendiceal orifice. Tate et al[20] reported favorable outcomes with EMR; however, for most lesions in their series, endoscopic management was not attempted because of deep extension into the appendiceal lumen or involvement of > 50% of the orifice circumference. Traction techniques may aid in exposing lesion margins[21,22], but visualization remains challenging if the lesion extends deeply into the appendiceal lumen, even with such techniques. Some researchers have proposed underwater EMR for adenomas involving the appendiceal orifice, but its efficacy remains suboptimal in patients with deep luminal extension[22-24].
Historically, for lesions extending deeply into the appendiceal orifice (as in this case), full-thickness resection with a disc-shaped snare has been considered an ideal endoluminal approach, as retracting the lesion into a cap allows resection to deeper portions of the orifice. For lesions > 2 cm in diameter, endoscopic full-thickness resection can also be combined with prior EMR via a “hybrid” technique to ensure complete lateral excision[25]. However, the risk of appendicitis associated with full-thickness resection with a disc-shaped snare cannot be ignored: Two studies by Schmidbaur et al[26] and Ichkhanian et al[27] reported that 15%-17% of patients develop appendicitis, with 50% of patients requiring urgent appendectomy. Recent reports also suggest that this approach may lead to peritoneal seeding of adenomatous tissue in cases of incomplete resection[28].
The most recent study by Jacob et al[29] demonstrated that ESD for L-PAO achieved an overall en bloc resection rate of 94.7%, with both perforation and postoperative bleeding rates at 1.3%. Thus, ESD for L-PAO offers safety and efficacy comparable to those of ESD in extra-appendiceal orifice regions. This study included three lesions extending deep into the appendiceal orifice, all of which were resected en bloc; however, all three patients had a history of prior ap
An alternative approach is to recommend combined endoscopic and laparoscopic surgery, which addresses challenges in identifying lesion margins, ensures en bloc resection, and improves R0 resection rates. Multiple studies[31-33] have confirmed that combined endoscopic and laparoscopic surgery is a safe procedure with favorable clinical outcomes and low recurrence rates. However, its application in nonbenign lesions is limited because of the challenge of ensuring negative margins while minimizing the resection scope.
In the present case, the physician innovatively performed ESD for the ileocecal region and appendiceal orifice first, followed by LA with preservation of the ileocecal valve for a type 3 Lesion. Preoperative endoscopic treatment of the ileocecal mass ensured negative margins and provided high-quality specimens for pathologists to accurately stage the resected lesion, guiding further management (postoperative follow-up vs surgical resection). Multiple endoscopic biopsies and ESD prior to LA confirmed adenoma at the appendiceal orifice, successfully preserving the ileocecal valve, reducing postoperative complications, and improving quality of life.
This case demonstrates that laparoscopic surgery following endoscopic ESD for appendiceal adenoma is safe and effective in achieving curative outcomes. However, a thorough histopathological examination is mandatory postoperatively. If appendectomy pathology reveals cancer, curative resection and lymph node dissection following colorectal cancer guidelines are needed. Additionally, patients should be counselled on the risks of cancer-related complications or the need for further resection after appendectomy.
An ileocecal LST with an appendiceal tubular adenoma is a clinically rare condition that is often incidentally detected during surgery. The preoperative diagnosis is limited by the frequent absence of symptoms and nonspecific diagnostic signs. With the advancement of endoscopic techniques and their lower postoperative complication rates, colorectal tumor lesions invading the appendiceal orifice should no longer be considered contraindications for endoscopic resection. Lesions should be classified according to the degree of invasion into the appendiceal orifice to guide the selection of different resection strategies.
| 1. | Bogie RMM, Veldman MHJ, Snijders LARS, Winkens B, Kaltenbach T, Masclee AAM, Matsuda T, Rondagh EJA, Soetikno R, Tanaka S, Chiu HM, Sanduleanu-Dascalescu S. Endoscopic subtypes of colorectal laterally spreading tumors (LSTs) and the risk of submucosal invasion: a meta-analysis. Endoscopy. 2018;50:263-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (2)] |
| 2. | Leonards LM, Pahwa A, Patel MK, Petersen J, Nguyen MJ, Jude CM. Neoplasms of the Appendix: Pictorial Review with Clinical and Pathologic Correlation. Radiographics. 2017;37:1059-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 90] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 3. | Collins DC. 71,000 Human Appendix Specimens. A Final Report, Summarizing Forty Years' Study. Am J Proctol. 1963;14:265-281. [PubMed] |
| 4. | Shinya H, Wolff WI. Morphology, anatomic distribution and cancer potential of colonic polyps. Ann Surg. 1979;190:679-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 356] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 5. | Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum. 1998;41:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 402] [Cited by in RCA: 418] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 6. | Turaga KK, Pappas SG, Gamblin T. Importance of histologic subtype in the staging of appendiceal tumors. Ann Surg Oncol. 2012;19:1379-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 164] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 7. | Carr NJ, Cecil TD, Mohamed F, Sobin LH, Sugarbaker PH, González-Moreno S, Taflampas P, Chapman S, Moran BJ; Peritoneal Surface Oncology Group International. A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia: The Results of the Peritoneal Surface Oncology Group International (PSOGI) Modified Delphi Process. Am J Surg Pathol. 2016;40:14-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 547] [Article Influence: 54.7] [Reference Citation Analysis (0)] |
| 8. | Graham RP, Williams NP, West KA. Primary epithelial tumours of the appendix in a black population: a review of cases. World J Gastroenterol. 2009;15:1472-1474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (7)] |
| 9. | B B SK, Jasuja P. Appendiceal mucocele-A rare case report. Int J Surg Case Rep. 2019;58:21-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Pickhardt PJ, Levy AD, Rohrmann CA Jr, Kende AI. Primary neoplasms of the appendix manifesting as acute appendicitis: CT findings with pathologic comparison. Radiology. 2002;224:775-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 93] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Chang P, Attiyeh FF. Adenocarcinoma of the appendix. Dis Colon Rectum. 1981;24:176-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Cortina R, McCormick J, Kolm P, Perry RR. Management and prognosis of adenocarcinoma of the appendix. Dis Colon Rectum. 1995;38:848-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 76] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Ito H, Osteen RT, Bleday R, Zinner MJ, Ashley SW, Whang EE. Appendiceal adenocarcinoma: long-term outcomes after surgical therapy. Dis Colon Rectum. 2004;47:474-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 68] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Kulaylat AS, Boltz MM, Moyer M, Mathew A, McKenna K, Messaris E. Management of Large Cecal Polyps: When Can the Ileocecal Valve Be Spared? Dis Colon Rectum. 2018;61:1089-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Saito Y, Uraoka T, Yamaguchi Y, Hotta K, Sakamoto N, Ikematsu H, Fukuzawa M, Kobayashi N, Nasu J, Michida T, Yoshida S, Ikehara H, Otake Y, Nakajima T, Matsuda T, Saito D. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc. 2010;72:1217-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 591] [Cited by in RCA: 609] [Article Influence: 38.1] [Reference Citation Analysis (5)] |
| 16. | Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Yamamichi N, Tateishi A, Oka M, Ogura K, Kawabe T, Ichinose M, Omata M. Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol. 2007;5:678-683; quiz 645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 281] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 17. | Horimatsu T, Fu KI, Sano Y, Yano T, Saito Y, Matsuda T, Fujimori T, Yoshida S. Acute appendicitis as a rare complication after endoscopic mucosal resection. Dig Dis Sci. 2007;52:1741-1744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Boda K, Oka S, Tanaka S, Tanaka H, Matsumoto K, Yamashita K, Sumimoto K, Hirano D, Tamaru Y, Ninomiya Y, Hayashi N, Chayama K. Short-term outcomes of endoscopic submucosal dissection for superficial cecal tumors: a comparison between extension and nonextension into the appendiceal orifice. Therap Adv Gastroenterol. 2018;11:1756284818772794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Song EM, Yang HJ, Lee HJ, Lee HS, Cha JM, Kim HG, Jung Y, Moon CM, Kim BC, Byeon JS. Endoscopic Resection of Cecal Polyps Involving the Appendiceal Orifice: A KASID Multicenter Study. Dig Dis Sci. 2017;62:3138-3148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Tate DJ, Desomer L, Awadie H, Goodrick K, Hourigan L, Singh R, Williams SJ, Bourke MJ. EMR of laterally spreading lesions around or involving the appendiceal orifice: technique, risk factors for failure, and outcomes of a tertiary referral cohort (with video). Gastrointest Endosc. 2018;87:1279-1288.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (1)] |
| 21. | Lambin T, Albouys J, Yzet C, Brun S, Rostain F, Rivory J, Pioche M. Endoscopic submucosal dissection of a lateral spreading tumor involving the appendiceal orifice using a multi-traction device. Endoscopy. 2022;54:E425-E426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | De Cristofaro E, Masgnaux LJ, Lupu A, Wallenhorst T, Jacques J, Rivory J, Pioche M. Treatment of a sessile serrated adenoma/polyp deeply invading the appendiceal orifice enabled by combined adaptive traction and underwater endoscopic submucosal dissection. Endoscopy. 2024;56:E215-E216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 23. | Iwasaki M, Okimoto K, Akizue N, Ota Y, Taida T, Matsumura T, Kato J, Kato N. Underwater modified strip biopsy for colorectal polyp invading into the appendiceal orifice. VideoGIE. 2024;9:344-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Binmoeller KF, Hamerski CM, Shah JN, Bhat YM, Kane SD. Underwater EMR of adenomas of the appendiceal orifice (with video). Gastrointest Endosc. 2016;83:638-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 25. | Mahadev S, Vareedayah AA, Yuen S, Yuen W, Koller KA, Haber GB. Outcomes of a hybrid technique using EMR and endoscopic full-thickness resection for polyps not amenable to standard techniques (with video). Gastrointest Endosc. 2021;94:358-367.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 26. | Schmidbaur S, Wannhoff A, Walter B, Meier B, Schäfer C, Meining A, Caca K. Risk of appendicitis after endoscopic full-thickness resection of lesions involving the appendiceal orifice: a retrospective analysis. Endoscopy. 2021;53:424-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Ichkhanian Y, Barawi M, Seoud T, Thakkar S, Kothari TH, Halabi ME, Ullah A, Edris W, Aepli P, Kowalski T, Shinn B, Shariaha RZ, Mahadev S, Mosko JD, Andrisani G, Di Matteo FM, Albrecht H, Giap AQ, Tang SJ, Naga YM, van Geenen E, Friedland S, Tharian B, Irani S, Ross AS, Jamil LH, Lew D, Nett AS, Farha J, Runge TM, Jovani M, Khashab MA. Endoscopic full-thickness resection of polyps involving the appendiceal orifice: a multicenter international experience. Endoscopy. 2022;54:16-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 28. | Dumoulin FL, Gorris DG, Berger S, Hildenbrand R, Sido B. Full-thickness resection with an over-the-scope device: possible translocation of adenoma tissue in a case of an incomplete resection at the appendix. Endosc Int Open. 2018;6:E622-E624. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Jacob H, Toyonaga T, Ohara Y, Tsubouchi E, Takihara H, Baba S, Yoshizaki T, Kawara F, Tanaka S, Ishida T, Hoshi N, Morita Y, Umegaki E, Azuma T. Endoscopic submucosal dissection of cecal lesions in proximity to the appendiceal orifice. Endoscopy. 2016;48:829-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 30. | Oung B, Rivory J, Chabrun E, Legros R, Faller J, Léger-Nguyen F, Rostain F, Ber CE, Hervieu V, Saurin JC, Ponchon T, Jacques J, Pioche M. ESD with double clips and rubber band traction of neoplastic lesions developed in the appendiceal orifice is effective and safe. Endosc Int Open. 2020;8:E388-E395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 31. | Jiang X, Wang M, Fu M, Wang Y, Zhao L, Fan Z. Breaking boundaries: laparoscopic and endoscopic collaboration in appendectomy. Rev Esp Enferm Dig. 2024;116:727-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Crawford AB, Yang I, Wu RC, Moloo H, Boushey RP. Dynamic article: combined endoscopic-laparoscopic surgery for complex colonic polyps: postoperative outcomes and video demonstration of 3 key operative techniques. Dis Colon Rectum. 2015;58:363-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 33. | Zhang YY, Lu JY, Wang Q, Yang AM. Resection of polyps involving the appendiceal orifice by combined endo-laparoscopic surgery: Two case reports. World J Gastrointest Surg. 2024;16:1948-1952. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/