Published online Nov 27, 2025. doi: 10.4240/wjgs.v17.i11.112025
Revised: July 28, 2025
Accepted: September 26, 2025
Published online: November 27, 2025
Processing time: 132 Days and 18.4 Hours
Surgery and percutaneous radiological methods [puncture, aspiration, injection, re-aspiration (PAIR)] are the current invasive treatment strategies for patients with hepatic hydatid cyst (HHC). Biliary leak is a common complication in patients who underwent these treatments of HHC. Bile leak should be treated effectively as uncontrolled biliary fistula may lead to life-treating conditions such as severe cholangitis, intraabdominal abscesses and septicemia. Endoscopic retrograde cholangiopancreatography (ERCP) has become the main treatment of post-interventional biliary fistula.
To evaluate the efficacy and safety of ERCP in the management of biliary fistula following HHC-related surgery or PAIR.
We evaluated data of patients who developed bile leakage following HHC-related interventions from endemic area during the period of March 2017 and February 2025. We included 88 patients (50 female, 57%) with a median age of 33 years (range: 8-83 years) at the time of ERCP. Bile leak occurred following surgery in 72 (82%) patients and after PAIR in 16 (18%) patients. Low-grade leakage (< 400 mL/day) was identified in 46 (52%) patients.
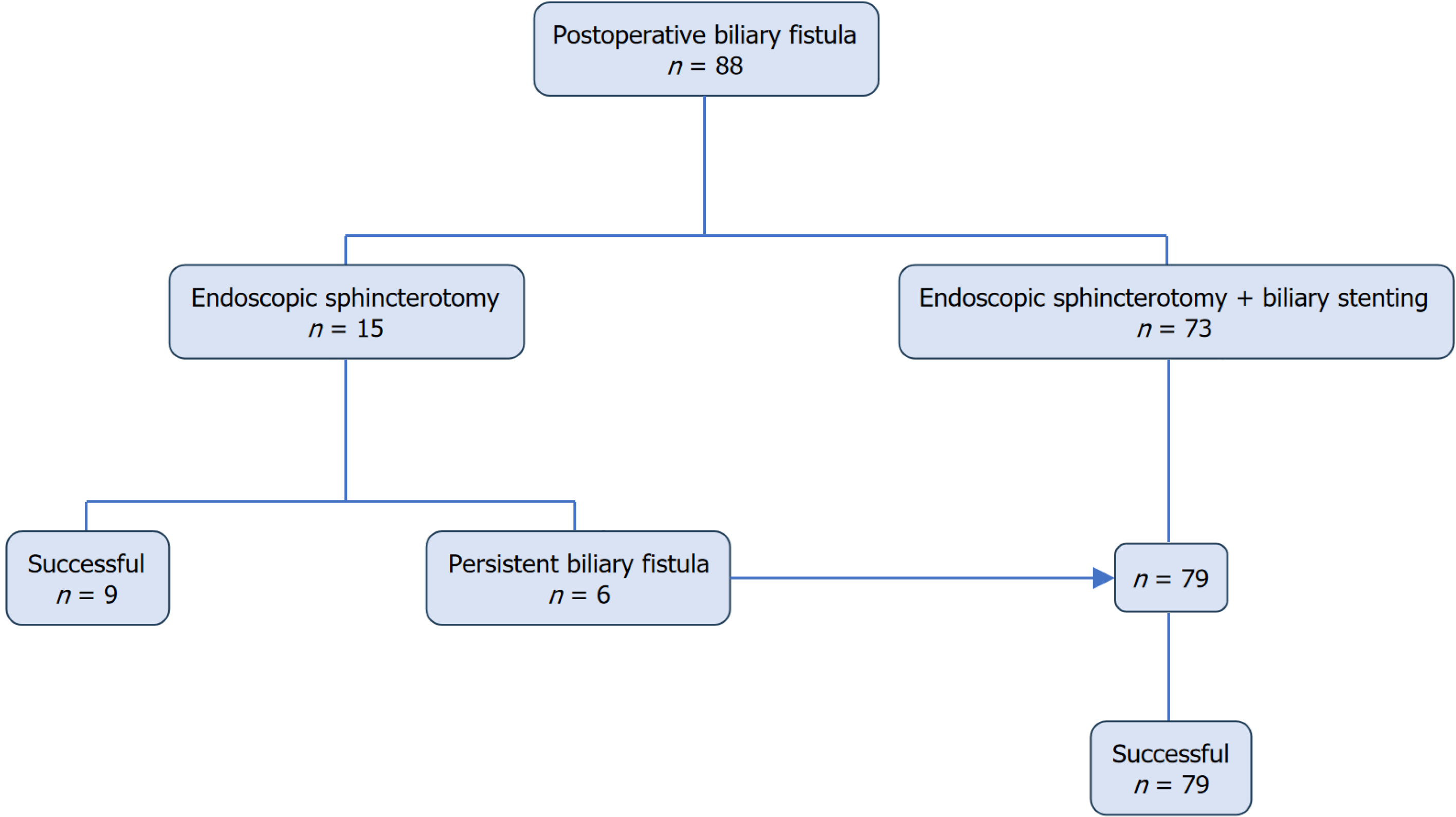
Initial mode of ERCP was endoscopic sphincterotomy (ES) with biliary drainage (plastic stent or nasobiliary drain) in 73 (83%) patients and ES alone in remaining 15 (17%) patients. Six patients who initially treated by ES alone had persistent fistula and underwent repeat ERCP with stent placement. ERCP type (ES + biliary stenting) and fistula flow rate (< 400 mL/day) were significantly associated with 20-days complete closure of the fistula [P = 0.020; odds ratio (OR) = 5.27, 95% confidence interval (95%CI): 1.30-21.37] and (P = 0.008; OR = 3.43, 95%CI: 1.37-8.55), respectively. ERCP-related complications were mild pancreatitis in 5 (5.9%) patients and minor bleeding in 4 (4.7%) patients and mild-moderate cholangitis in 4 (4.7%) patients.
This case based-study from endemic area demonstrates that ERCP is highly effective and safe for managing bile leakage following both surgery and PAIR. ES + biliary stenting seems better mode of ERCP procedure.
Core Tip: Liver is the most commonly affected organ of hydatid cyst involvement. Majority of patients with hepatic hydatid cysts (HHCs) are diagnosed incidentally or when HHCs-related complications occur. Rupture into intrahepatic bile ducts is the common and serious complication in individuals with HHCs. Surgery and percutaneous radiological methods [puncture, aspiration, injection, re-aspiration (PAIR)] are the current standard treatment strategies for patients with HHC. Biliary leak is a common complication in patients who underwent surgery or PAIR. We investigated efficacy and safety of ERCP in the management of biliary fistula following HHC-related surgery and PAIR.
- Citation: Polat M, Batıbay E, Erkmen F, Yüksekyayla O, Emin Boleken M, Kırhan I, Celik B, Sürmeli S, Akkoyun Z, Atlas I, Atlas A, Dere O, Kaya V, Dumanlı S, Moral K, Kekilli M, Şimşek C, Efe C. Endoscopic retrograde cholangiopancreatography for the management of biliary fistula following liver hydatid cyst related surgery or radiological interventions. World J Gastrointest Surg 2025; 17(11): 112025
- URL: https://www.wjgnet.com/1948-9366/full/v17/i11/112025.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i11.112025
Hydatid disease which is caused by the larval form of Echinococcus granulosus, is a significant zoonotic disease that leads to mortality and morbidity in Mediterranean countries, the Middle East, Australia, and South America. The increasing population movements have led to a rise in the incidence of hydatid disease in non-endemic regions, such as the United States and Europe[1].
Liver is the most commonly affected organ in hydatid cyst involvement, accounting for 70% of cases. Most of people living with hepatic hydatid cyst (HHC) are diagnosed incidentally or when complications related to the cyst occur[2,3]. Rupture into intrahepatic bile ducts is a common and serious complication in individuals with HHC[4,5].
Surgery is the current standard treatment strategy for HHC. However, percutaneous radiological methods, such as puncture, aspiration, injection, re-aspiration (PAIR), are also effective treatment options for a select group of patients with HHC[6,7]. Biliary leak is a common complication that is reported in 50%-63% of patients who underwent these treatments of HHC[5]. Bile leak should be treated effectively, as uncontrolled biliary fistula can lead to life-threatening conditions such as severe cholangitis, intraabdominal abscesses, and septicemia[5,7]. Endoscopic retrograde cholangiopancreatography (ERCP) is the standard initial therapeutic option for individuals who developed biliary fistula following HHC-related interventions as surgical management of biliary fistula is associated with mortality and morbidity[5]. In these patients, endoscopic sphincterotomy (ES) alone or ES with biliary drainage (plastic or nasobiliary stent) is the re
In this two-center cohort study, we evaluated the efficacy and safety of ERCP in HHC patients who developed bile leakage following PAIR or surgery. We also tried to identify factors associated with complete closure time of biliary fistula in these patients.
This multicenter retrospective cohort study was conducted at two tertiary referral centers in Türkiye, Harran University Hospital and Gazi University Hospital. The study protocol was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Harran University Faculty of Medicine (HRU/21.08.22).
We included consecutive patients who developed bile leakage following surgery or radiological intervention for HHC between March 2017 and February 2025. Bile leakage was defined as the presence of bile in percutaneous drains and/or radiological evidence of biliary extravasation. ERCP was considered for patients with continuous bile discharge (daily output > 100 mL) after 10 days of HHC-related intervention[5].
Data were extracted from electronic health records using a standardized data collection form. Baseline demographic characteristics included age, sex, comorbidities, and previous management history. Laboratory parameters included a complete blood count, liver biochemical tests, renal function tests, a coagulation profile (prothrombin time, partial thromboplastin time, international normalized ratio), and inflammatory markers (C-reactive protein, erythrocyte sedimentation rate). Cyst-specific data included size, location, number, and Gharbi classification[10]. Surgical details documented the type of intervention, timing, and immediate post-operative course.
All patients underwent comprehensive pre-procedural imaging, including abdominal ultrasonography, computed tomography, or magnetic resonance cholangiopancreatography. Prophylactic antibiotics were administered according to institutional protocols. Rectal indomethacin (100 mg) was administered to patients for post-ERCP pancreatitis pro
Patients were monitored for immediate post-procedural complications, including bleeding, pancreatitis, and perforation. Adverse events were classified according to the lexicon proposed by Cotton et al[12].
Data analysis was conducted using SPSS version 27.0 (IBM Corp., Armonk, NY, United States). The Shapiro-Wilk test was used to assess the normality of the distribution. Continuous variables were presented as mean ± SD or median (in
We analyzed data from 88 patients (57% female) who developed bile leak following HHC-related interventions and underwent ERCP. The general characteristics of the study population are presented in Table 1. The median age of the patients was 33 years (range: 8-83 years) at the time of ERCP. The median cyst size was 9.5 cm (range: 3-23 cm). Sixty-five patients had single cysts, while 23 patients had multiple cysts. The most common location of HHC was segment VII of the liver (n = 29). According to the Gharbi classification, the distribution of HHC was stage I in 10 (11%) patients, stage II in 36 (41%), stage III in 31 (35%), and stage IV in 11 (13%) patients. Initially, surgery was the preferred management for HHC in 72 (82%) patients, while PAIR was chosen in 16 (18%) patients. Bile leakage originated from the right intrahepatic bile ducts in 62 (70%) patients and from the left intrahepatic bile ducts in 26 (30%) patients. A total of 42 (48%) patients presented with high-grade leakage.
| Total patients | n = 88 |
| Gender (female), n (%) | 50 (57) |
| Median age (range; years) | 33 (8-83) |
| Comorbidities, n (%) | |
| Diabetes mellitus | 6 (6.8) |
| Arterial hypertension | 4 (4.5) |
| Coronary artery disease | 1 (1.1) |
| Celiac disease | 1 (1.1) |
| Thalassemia major | 1 (1.1) |
| Gordon syndrome | 1 (1.1) |
| Polycystic kidney disease | 1 (1.1) |
| Median cyst size (cm) | 9.5 (4-23) |
| Gharbi classification, n (%) | |
| Type 1 | 10 (11) |
| Type 2 | 36 (41) |
| Type 3 | 31 (35) |
| Type 4 | 11 (13) |
| Cyst characteristics, n (%) | |
| Single cyst | 65 (74) |
| Right lobe | 70 (62) |
| Intervention type (surgery) | 72 (82) |
| Daily fistula output (> 400 mL) | 42 (48) |
| ERCP time (< 10 days), n (%) | 38 (43) |
| Mode of ERCP, n (%) | |
| ES + biliary stenting | 73 (83) |
| ES alone | 15 (17) |
| Number of ERCP procedures, n (%) | |
| 1 | 66 (75) |
| 2 | 17(19) |
| 3 | 4 (5) |
| 4 | 1 (1) |
| All complications, n (%) | |
| Pancreatitis (mild) | 5 (6) |
| Bleeding (mild) | 4 (5) |
| Infection/cholangitis (non-severe) | 4 (5) |
| Discharge (days), n (%) | |
| 1 | 56 (64) |
| 2 | 18 (20) |
| > 3 | 14 (16) |
| Median fistula closure time (range; days) | 17 (8-93) |
Initial treatment options included ES with biliary drainage (using a plastic stent, n = 70, or a nasobiliary catheter, n = 3) in 73 (83%) patients, and ES alone in 15 (17%) patients. Six patients treated with ES alone had persistent fistula and were managed by repeat ERCP with stent placement. We performed a total of 116 ERCP procedures (excluding stent removals) in this study. Single-session treatment was successful in 66 (75%) patients, while 22 (25%) patients required multiple ERCP procedures. Of these, 17 patients underwent two procedures, four patients had three procedures, and one patient required four ERCP procedures. The common bile duct was successfully cannulated in 87 (98.8%) patients during the first ERCP session. In only one (1.2%) patient, cannulation of the common bile duct was achieved in the second ERCP procedure. The difficult cannulation rate was 17% (n = 15) in the study population. Concurrently, common bile duct stones were detected in three patients, all of whom were successfully removed during the same session using by balloon or basket techniques.
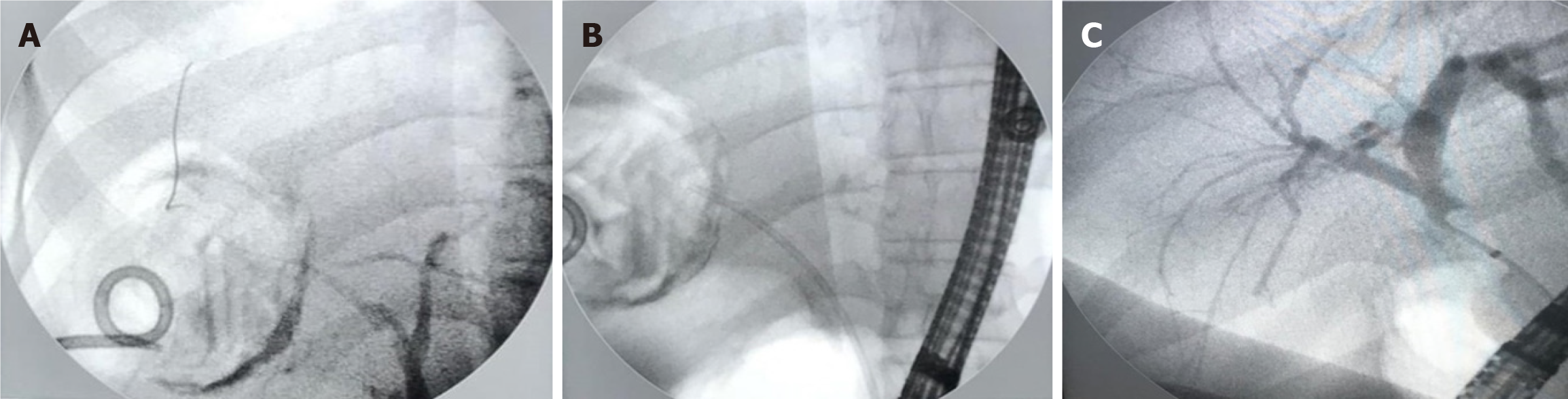
Figure 1 shows the mode of ERCP procedure and clinical outcomes of patients with HHC-related biliary fistula. Complete bile leakage closure was achieved in all patients median 20 days (range: 8-93 days) after the initial ERCP procedure. In the ES + biliary stenting group, bile drainage ceased in all patients median 18 days (range: 8-93 days) after first ERCP procedure. In the ES alone group, bile drainage resolved in nine patients median 17 days (range: 12-19 days) after the ERCP procedure while remaining six patients required repeated ERCP with stenting due to persistent bile leaks (> 20 days) with daily output exceeding 200 mL. These patients achieved bile leak closure median 15.5 days (range: 10-25 days) after repeated ERCP. Figure 2 presents the management of patient with post-interventional HCC-related biliary fistula.
Predictors of complete fistula closure within 20 days are presented in Table 2. Multivariate regression analysis revealed that ERCP intervention type (ES + biliary drainage) and fistula flow rate (< 400 mL/day) were significantly associated with 20-day complete closure of the fistula (P = 0.020; OR = 5.27, 95%CI: 1.30-21.37) and (P = 0.008; OR = 3.43, 95%CI: 1.37-8.55), respectively.
| Variable | Univariate analysis | Multivariate analysis | ||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Gender | ||||
| Male | 1 | |||
| Female | 1.23 (0.53-2.87) | 0.625 | ||
| Size (cm) | ||||
| > 9.4 | 1 | |||
| < 9.4 | 1.19 (0.51-2.75) | 0.683 | ||
| Number of cyst | ||||
| Single | 1 | |||
| Multiple | 1.00 (0.38-2.60) | 0.991 | ||
| Garbi classification | ||||
| 1 | 1 | |||
| 2 | 1.40 (0.34-5.70) | 0.639 | ||
| 3 | 0.63 (0.160-2.65) | 0.530 | ||
| 4 | 0.571 (0.100-3.27) | 0.530 | ||
| ERCP intervention type | ||||
| EST | 1 | 1 | ||
| EST + BD | 4.58 (1.19-17.63) | 0.027 | 5.27 (1.30-21.37) | 0.020 |
| Fistula flow rate | ||||
| High | 1 | 1 | ||
| Low | 3.11 (1.29-7.44) | 0.011 | 3.43 (1.37-8.55) | 0.008 |
| ERCP complication | ||||
| Present | 1 | |||
| Absent | 1.108 (0.297-4.125) | 0.879 | ||
| Intervention type | ||||
| PAIR | 1 | |||
| Surgery | 1.11 (0.378-3.30) | 0.841 | ||
| Localization of leakage | ||||
| Right intrahepatic | 1 | |||
| Left intrahepatic | 1.13 (0.443-2.89) | 0.794 | ||
| Postoperative hospital stays (day) | ||||
| > 5 | 1 | |||
| < 5 | 1.0 (0.433-2.30) | 1.000 | ||
| ERCP time (day) | ||||
| > 10 | 1 | |||
| < 10 | 1.026 (0.441-2.38) | 0.953 | ||
ERCP-associated complications were observed in 13 (15.3%) patients. Post-ERCP pancreatitis developed in five (5.9%) patients, bleeding occurred in four (4.7%) patients, and four (4.7%) patients were complicated by cholangitis. All these complications were minor and managed with conservative measures. No ERCP-related perforation or procedure-related mortality was observed. Three (3.4%) patients developed liver abscesses, which were successfully managed by placing ultrasound-guided percutaneous drainage catheters.
Bile leakage following HHC related interventions is a challenging complication that significantly impacts patient outcomes and healthcare resource utilization. ERCP has emerged as the contemporary standard of care for post-operative bile leakage management, supported by extensive clinical evidence and consensus guidelines[5,13-19]. We presented a large cohort of patients who developed bile leaks following HHC-related surgery or PAIR from HHC endemic area. Our study results confirmed that ERCP is safe and effective in managing patients with bile leaks that developed after HHC-related interventions.
HHC-related fistula with daily output > 100 mL is rarely resolve spontaneously. Previous studies suggested that ES alone or ES with biliary stent placement for management of HHC-related fistula. Biliary stenting offers several mechanical and physiological advantages beyond simple leak occlusion. The placement of a stent reduces common bile duct pressure and upstream pressure gradients[5]. This mechanism facilitates healing of leak site as well preventing secondary biliary stenosis and associated complications. Further, biliary stenting enables endoscopic clearance of residual cyst materials from the biliary system[16,19]. Our results showed that ES with biliary stenting was associated with higher probability of 20-days closure of bile leak. Also, some of patients with persistent bile leak following ES alone were successfully managed by biliary stenting. Two large case-based studies reported that closure time of the HHC-related bile leak was shorter in patients who had ES combined with stenting than those managed by ES alone[19,20]. These results suggest that ES with biliary stenting may be better management strategy for bile leak that develops following HHC-related interventions.
We found that daily output (< 400 mL) was significantly associated with 20-days fistula closure. In one study, daily biliary drainage volume < 102 mL was predictor of spontaneous fistula closure[21]. We performed ERCP in only patients who had continuously (> 10 days after HHC related intervention) higher than 100 mL daily output fistula. Other studies did not find any correlation between daily output and fistula closure duration[17,19,20]. Importantly, we performed more robust statistical analysis and we believe that our findings can help physicians in the management of this group of patients.
A previous study reported that a 10 F diameter plastic stent was more effective in treating post-interventional HHC-related biliary fistula[19]. However, we did not observe correlation between the duration of fistula closure and the number or size of biliary stents. In another study[1], the authors recommended using nasobiliary drains instead of plastic stent for patients with HHC-related biliary fistula. Nasobiliary drainage demonstrated favorable clinical outcomes in our three patients, but all patients reported significant discomfort during follow-up. Therefore, we preferred plastic stent as the primary management strategy for most patients with post-interventional HHC-related biliary fistula. Several other factors such as post-operative timing of ERCP, number of HHC, HHC localization or size were not associated with 20-days bile leakage closure in our study population.
Previous studies reported 81%-100% technical and clinical success rates of ERCP in patients with HHC-related biliary fistula[5]. In our study, clinical and technical success rate was 100%. The difficult cannulation rate was 4.7% (n = 4) in the study population. These results strongly suggest that ERCP is the standard care method for post-interventional HHC-related biliary fistula.
Post-ERCP pancreatitis occurred in 5 (5.9%) and bleeding in 4 (4.7%) patients. All these complications were minor and successfully managed by conservatively. Four (4.7%) patients developed cholangitis. No mortality was observed in our study population. Previous study also reported acceptable adverse outcome rates in patients with HHC-related biliary fistula who underwent ERCP. Three patients developed liver abscess and required percutaneous intervention. This adverse outcome seems to be related to surgery or PAIR rather than ERCP procedure.
The retrospective design is the main limitation of our study. We also could not provide long-term outcome of patients who underwent ERCP for the management of post-interventional HHC-related biliary fistula. Importantly, this specific information is not aim of our study as long-term complications are mainly related to PAIR or surgical intervention. Due to lack of a uniform treatment protocol, our results may also be influenced by patient selection bias for each type of ERCP procedure. To overcome this limitation, we carefully collect data of all included patients and all procedures were performed by experienced two gastroenterologists who work in high volume ERCP centers. Future, prospective studies with long-term follow-up would address these limitations and reveal better therapeutic management strategies for patients with post-interventional HHC-related biliary fistula.
Our study results suggest that ERCP is effective and safe for the management of post-surgery or PAIR related biliary fistula in patients with HHC. ERCP type and low-output fistula (< 400 mL/day) were predictor of 20-days fistula closure. Therefore, we recommended that standard care of ERCP should include ES with biliary stenting for patients with post-interventional HHC-biliary fistula.
We thank to Dilek Yapar for reviewing statistical methods and techniques that used in our study.
| 1. | Cicek B, Parlak E, Disibeyaz S, Oguz D, Cengiz C, Sahin B. Endoscopic therapy of hepatic hydatid cyst disease in preoperative and postoperative settings. Dig Dis Sci. 2007;52:931-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Greco S, Cannella R, Giambelluca D, Pecoraro G, Battaglia E, Midiri M, Brancatelli G, Vernuccio F. Complications of hepatic echinococcosis: multimodality imaging approach. Insights Imaging. 2019;10:113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Belli S, Akbulut S, Erbay G, Koçer NE. Spontaneous giant splenic hydatid cyst rupture causing fatal anaphylactic shock: a case report and brief literature review. Turk J Gastroenterol. 2014;25:88-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | İskurt Y, Yabaci Tak A, Destek S, Akcakaya A, Bulbuloglu E, Deger KC. Management of complicated hepatic hydatid cysts: Our single-center experience. Ulus Travma Acil Cerrahi Derg. 2025;31:531-539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Dolay K, Akbulut S. Role of endoscopic retrograde cholangiopancreatography in the management of hepatic hydatid disease. World J Gastroenterol. 2014;20:15253-15261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 49] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 6. | Men S, Hekimoğlu B, Yücesoy C, Arda IS, Baran I. Percutaneous treatment of hepatic hydatid cysts: an alternative to surgery. AJR Am J Roentgenol. 1999;172:83-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 75] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Pavlidis ET, Galanis IN, Pavlidis TE. Current considerations for the management of liver echinococcosis. World J Gastroenterol. 2025;31:103973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Carr-Locke AD. 'Biliary stenting alone versus biliary stenting plus sphincterotomy for the treatment of post-laparoscopic cholecystectomy bile leaks'. Eur J Gastroenterol Hepatol. 2006;18:1053-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Tzias V, Psatha P, Stergiopoulos S, Lagoudakis M. Left hepatic duct cutaneous fistula after right hepatic lobe hydatid cyst operation treated with nasobiliary tube. Gastrointest Endosc. 1999;50:710-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic liver. Radiology. 1981;139:459-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 528] [Cited by in RCA: 493] [Article Influence: 11.0] [Reference Citation Analysis (1)] |
| 11. | Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M, Gyokeres T, Hafner M, Halttunen J, Hassan C, Lopes L, Papanikolaou IS, Tham TC, Tringali A, van Hooft J, Williams EJ. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:657-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 429] [Article Influence: 42.9] [Reference Citation Analysis (1)] |
| 12. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2082] [Article Influence: 59.5] [Reference Citation Analysis (1)] |
| 13. | Kayaalp C, Bzeizi K, Demirbag AE, Akoglu M. Biliary complications after hydatid liver surgery: incidence and risk factors. J Gastrointest Surg. 2002;6:706-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Ramia JM, Figueras J, De la Plaza R, García-Parreño J. Cysto-biliary communication in liver hydatidosis. Langenbecks Arch Surg. 2012;397:881-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Batıbay E, Yüksekyayla O, Polat M, Bayhan İ, Sevinç M, Dağ A, Barutçu S, Kocaman OH, Boleken ME, Şimşek C, Erkmen F, Efe C. Endoscopic Retrograde Cholangiopancreatography in Pediatric Population: A Decade-Long Experience from 2 Tertiary Centers. Turk J Gastroenterol. 2025;36:321-327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Ozaslan E, Bayraktar Y. Endoscopic therapy in the management of hepatobiliary hydatid disease. J Clin Gastroenterol. 2002;35:160-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Dolay K, Akçakaya A, Soybir G, Cabioğlu N, Müslümanoğlu M, Iğci A, Topuzlu C. Endoscopic sphincterotomy in the management of postoperative biliary fistula A complication of hepatic hydatid disease. Surg Endosc. 2002;16:985-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Giouleme O, Nikolaidis N, Zezos P, Budas K, Katsinelos P, Vasiliadis T, Eugenidis N. Treatment of complications of hepatic hydatid disease by ERCP. Gastrointest Endosc. 2001;54:508-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Adas G, Arikan S, Gurbuz E, Karahan S, Eryasar B, Karatepe O, Tekant Y. Comparison of endoscopic therapeutic modalities for postoperative biliary fistula of liver hydatid cyst: a retrospective multicentric study. Surg Laparosc Endosc Percutan Tech. 2010;20:223-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 20. | Akcakaya A, Sahin M, Karakelleoglu A, Okan I. Endoscopic stenting for selected cases of biliary fistula after hepatic hydatid surgery. Surg Endosc. 2006;20:1415-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Zeybek N, Dede H, Balci D, Coskun AK, Ozerhan IH, Peker S, Peker Y. Biliary fistula after treatment for hydatid disease of the liver: when to intervene. World J Gastroenterol. 2013;19:355-361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |