Published online Nov 27, 2025. doi: 10.4240/wjgs.v17.i11.111148
Revised: July 11, 2025
Accepted: September 10, 2025
Published online: November 27, 2025
Processing time: 152 Days and 19.8 Hours
Esophageal lymphangioma is a rare benign tumor, and its clinical characteristics and treatment methods warrant attention. In this report, we describe a case of esophageal lymphangioma.
The 48-year-old male patient came to our hospital for a health examination one month ago. An endoscopic examination revealed a protruding lesion in the esophagus, which was completely resected via endoscopic submucosal dissection. Pathological examination of the resected specimen confirmed the diagnosis of a lymphangioma. We have also summarized and compiled previously reported cases of esophageal lymphangioma.
Esophageal lymphangioma is a rare benign tumor, and endoscopic minimally invasive treatment represents a safe and effective therapeutic approach.
Core Tip: Esophageal lymphangioma is an exceedingly rare benign tumor that has been infrequently reported for nearly a century. Given the rarity of this condition, it is imperative for clinicians to possess a comprehensive understanding of its clinical manifestations, pathogenesis, and the findings from endoscopic and imaging studies. Furthermore, summarizing previous treatment methods, their efficacy, and associated complications is crucial. All these will enhance clinicians' diagnostic capabilities and aid in the formulation of appropriate treatment strategies for this disease.
- Citation: Zheng XL, Yu XX. Esophageal lymphangioma: A case report and review of literature. World J Gastrointest Surg 2025; 17(11): 111148
- URL: https://www.wjgnet.com/1948-9366/full/v17/i11/111148.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i11.111148
Lymphangioma is a tumor characterized by the proliferation or dilation of lymphatic endothelial cells within lymphatic vessels. This type of tumor can manifest in any anatomical region containing lymphatic vessels, although it is most commonly found in areas such as the head and neck, axilla, and mediastinum[1]. Lymphangiomas are generally considered benign lesions. Although lymphangiomas are infrequently observed in the gastrointestinal tract, reports of such cases in the esophagus are even rarer[2]. Due to their rarity, there are few international reports available. Therefore, this article presents a case of successful complete resection of an esophageal lymphangioma via endoscopy. We also summarize and compile previously reported cases of esophageal lymphangioma[3-28].
The 48-year-old male patient came to our hospital for a health examination one month ago. An endoscopic examination revealed a protruding lesion in the esophagus.
The patient was healthy and without any uncomfortable symptoms.
The patient had a history of gastrointestinal polyps and a history of endoscopic treatment.
The patient had no history of smoking and alcohol consumption, and his family history was unremarkable.
His vital signs were stable, and a physical examination showed no notable findings.
Laboratory tests indicated hyperlipidemia, with a cholesterol level of 5.38 mmol/L and a triglyceride level of 2.20 mmol/L. All other results were within normal limits.
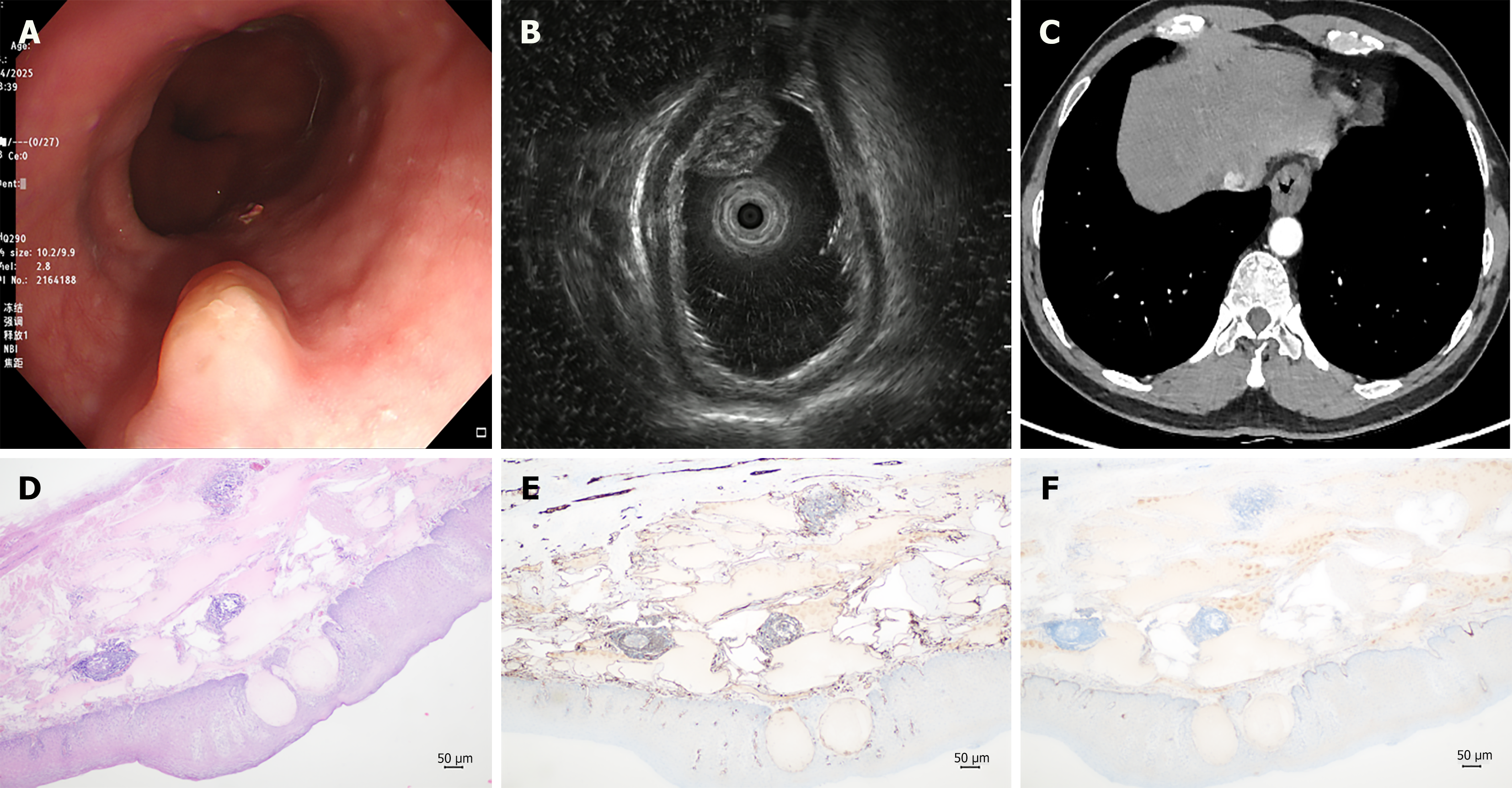
During esophagogastroduodenoscopy, a protruding lesion was identified in the lower segment of the esophagus, which measured approximately 1.5 cm × 0.8 cm. The surface mucosa appeared smooth, and its color was consistent with the surrounding mucosa (Figure 1A). Endoscopic ultrasound (EUS) examination suggested that the esophageal lesion was situated in the submucosal layer, appearing as a mixed hypoechoic mass characterized by internal inhomogeneity and visible minute septal-like changes, with no significant blood flow signals detected (Figure 1B). Chest computed tomography (CT) revealed localized wall thickening in the lower segment of the esophagus (Figure 1C).
Submucosal mass of esophagus of an uncertain nature.
The auxiliary examination results indicated that the esophageal mass was a localized lesion, showing no evidence of distant metastasis or involvement of surrounding organs. The size of the lesion was appropriate for endoscopic minimally invasive resection. Given the uncertainty regarding the nature of the mass and the patient’s request for complete removal, a decision was made to perform endoscopic submucosal dissection (ESD) after thorough com
The lesion was completely resected by ESD. The tumor had a broad-based elevated structure (0-Is), measuring 1.5 cm × 0.8 cm, with both horizontal and vertical margins free of malignancy. Histopathological analysis revealed numerous dilated luminal structures within the lamina propria (Figure 1D), while immunohistochemical analysis demonstrated cluster of differentiation (CD) 31 positivity (Figure 1E) and partial positivity for D2-40 (Figure 1F). The pathological examination confirmed a diagnosis of esophageal lymphangioma. The patient experienced no postoperative complications and was discharged after three days of hospitalization. During follow-up one month later, the patient reported no significant discomfort.
Lymphangioma is a benign tumor that primarily occurs in regions such as the head and neck, axilla, and mediastinum. It can manifest as a solitary lesion or as multiple lesions[1]. According to Wegener’s classification, lymphangiomas can be categorized into simple, spongy, or cystic types[11]. Lymphangiomas have a low incidence in the gastrointestinal tract, with esophageal lymphangiomas being particularly rare[2]. Since the initial case reported by Watson-Williams in 1934, only 44 cases have been documented in the literature to date, as illustrated in Table 1[3-28]. All patients were adults, with an average age of approximately 52 years (range 30-77 years). Of these patients, 28 were male and 17 were female, with lesions primarily located in the middle and lower segments of the esophagus. These lesions predominantly presented as solitary lesions, most of which had a diameter less than 2 cm. The clinical manifestations of patients with esophageal lymphangiomas are non-specific and may correlate with the size and location of the mass. Symptoms can include dysphagia[7,10,12,20], upper abdominal discomfort[28], heartburn[9], nausea[18], vomiting[3,6], and chest pain[3,8,14]; however, some patients may exhibit no obvious clinical symptoms[21].
| Case | Year | Ref. | Country | Gender | Age (years) | Site | Size (cm) | Chief complaints | Treatment |
| 1 | 1934 | Watson-Williams[3] | United Kingdom | Male | 61 | L | NA | Chest pain, vomiting | Observation |
| 2 | 1973 | Brady and Milligan[4] | United States | Female | 62 | U | 5 | Epigastric pain | Observation |
| 3 | 1979 | Armengol-Miro et al[5] | Spain | Male | 64 | L | 1 | Epigastric pain | Snare polypectomy |
| 4 | 1980 | Tamada et al[6] | Japan | Male | 46 | L | NA | Dysphagia and vomiting | Open surgery |
| 5 | 1983 | Liebert[7] | United States | Male | 58 | L | 1.5 | Dysphagia | Snare polypectomy |
| 6 | 1990 | Castellanos et al[8] | Spain | Female | 66 | M | 2 × 1.5 | Chest pain | Open surgery |
| 7 | 1994 | Yoshida et al[9] | Japan | Male | 55 | M | 4 | Heartburn | Open surgery |
| 8 | 1996 | Suwa et al[10] | Japan | Female | 52 | L | 2.2 × 2 | Dysphagia | Snare polypectomy |
| 9 | 1998 | Scarpis et al[11] | Italy | Male | 64 | L | 1.5 | Epigastric pain | Snare polypectomy |
| 10 | 2002 | Lee et al[12] | Korea | Male | 37 | M, L | NA | Dysphagia | INF α2a and partial polypectomy |
| 11 | 2004 | Yoon et al[13] | Korea | Male | 72 | L | 5.1 × 2.3 | Vomiting | Open surgery |
| 12 | 2005 | Saers et al[14] | Germany | Female | 52 | L | 0.7 | Dysphagia, abdominal discomfort, chest pain | EMR |
| 13 | 2007 | Sushil et al[15] | United States | Male | 68 | L | 1.5 | Heartburn | Snare electrocautery |
| 14 | 2008 | Best et al[16] | United States | Male | 64 | U | 3.5 × 2.2; 2.0 × 1.4 | Vertigo and neck pain | CO2 laser resection |
| 15 | 2008 | Seybt et al[17] | United States | Male | 53 | L | 4 | Dysphagia, regurgitation | Open surgery |
| 16 | 2010 | Arashiro et al[18] | Japan | Female | 33 | L | 1.9 × 1.5 | Nausea and heartburn | ESD |
| 17 | 2011 | Lee et al[19] | Korea | Male | 55 | M | 0.7 | None | Endoscopic resection with band ligation |
| 18 | 2012 | Xue et al[20] | China | Male | 58 | M, L | 10 × 2.5 × 1; 6 × 5 × 4 | Dysphagia | Open surgery |
| 19 | 2013 | Zhao et al[21] | China | 2 females + 4 males | 35-77 | 1 U + 4 M + 3 L | 0.4-1.2 | Asymptomatic | Dual-channel endoscopic; resection |
| 25 | 2015 | Barbosa et al[22] | Portugal | Male | 54 | L | 1.2 | None | Observation |
| 26 | 2017 | Luo et al[23] | China | Male | 41 | L | 6 × 1 | Dysphagia | Endoscopic piecemeal mucosal resection |
| 27 | 2017 | Zhao et al[24] | China | Male | 59 | M | NA | Choking | EMR |
| 28 | 2018 | Hu et al[25] | China | Male | 46 | M, L | 16 × 6 × 4 | Dysphagia | ESD |
| 29 | 2018 | Min and Liu[26] | China | Female | 44 | M | 7 | Dysphagia | Snare electrocautery |
| 30 | 2018 | Cheng et al[27] | China | Female | 48 | U | 1.5 × 1.2 × 1 | Dysphagia | ESD |
| 31 | 2022 | Shi et al[28] | China | 8 females + 6 males | 30-71 | Unknown | 0.22-4 | Bloating, abdominal pain, regurgitation, foreign body sensation | 13 EMR + 1 ESD |
| 45 | 2025 | Our case | China | Male | 48 | L | 1.5 × 0.8 | Asymptomatic | ESD |
Endoscopic examination is a crucial method for diagnosing esophageal lymphangiomas. Previous reports have documented cases exclusively in adults, suggesting that esophageal lymphangiomas may be more readily identified after adulthood. On white light endoscopy, esophageal lymphangiomas typically appear as sessile, hemispherical lesions with a smooth surface that matches the color of adjacent mucosa. This presentation can be challenging to differentiate from conditions such as esophageal leiomyomas, stromal tumors, and cysts. EUS can determine the nature of lesions by displaying their ultrasound characteristics, including the origin layer, size, boundaries, echogenicity, and the presence of echoes, which aids in evaluating the subsequent steps for choosing between endoscopic surgery and surgical resection[29]. Previous cases of esophageal lymphangiomas were typically found in the submucosal layer. In the present case, the EUS examination indicated that the lesion was located in the submucosal layer, presenting as a mixed hypoechoic mass with internal heterogeneity, displaying a honeycomb-like change, and without significant blood flow signals. Chest CT can reflect the relationship between esophageal masses and adjacent organs, as well as the presence of metastasis. For submucosal esophageal tumors, a comprehensive analysis of their location, size, EUS findings, CT results, and the patient’s treatment preferences is necessary to develop an appropriate, safe, and effective treatment plan for the patient.
The treatment methods for esophageal lymphangioma depend on factors such as the size and location of the lesion, as well as the patient’s symptoms. In addition, treatment techniques are continually being updated and iterated with advancements in technology. Previous literature indicates that lesions smaller than 2.5 cm are predominantly removed via endoscopic resection, whereas those larger than 2.5 cm are more frequently addressed through open surgery[22]. Previous literature has documented various endoscopic treatment methods. Among these, endoscopic mucosal resection is primarily utilized for lesions smaller than 1 cm[14,24,28], while snare polypectomy[7,10,11,15], and ESD[18,27] are more commonly applied to lesions measuring between 1 cm and 2 cm. Additionally, some less common endoscopic techniques have been reported; for instance, Korean endoscopists have successfully excised two cases of esophageal lymphangioma using endoscopic resection with band ligation and interferon α2a in conjunction with partial polypectomy[12,19]. Furthermore, a case of endoscopic submucosal resection employing CO2 laser resection was described by Best et al[16]. With the continuous maturation and advancement of gastrointestinal endoscopy technology, we are entering a new era of super minimally invasive surgery, where endoscopic minimally invasive resection is poised to become the predominant surgical approach for esophageal lymphangiomas. Notably, Chinese scholars Luo et al[23] and Hu et al[25] have reported successful resection of giant esophageal lymphangiomas utilizing ESD. Zhao et al[21] reported that dual-channel endoscopic resection is also a new technique capable of effectively removing esophageal lymphangiomas. Regardless of the treatment method used, ensuring patient safety and minimizing complications remains crucial.
Pathological diagnosis serves as the primary basis for identifying esophageal lymphangioma, which is characterized by the irregular dilation of lymphatic vessels and the proliferation of endothelial cells[22]. The lumens of these vessels are filled with lymphatic fluid, and lymphocyte aggregation is observed in the surrounding areas. Furthermore, the positive expression of CD31 and D2-40 is significantly valuable for a definitive diagnosis[25]. In this case, the patient’s tissue type exhibited numerous dilated, lumen-like structures in the lamina propria, and immunohistochemistry revealed CD31 positivity and partial positivity for D2-40, with pathological results confirming the diagnosis of esophageal lym
Esophageal lymphangioma is a rare benign tumor of the esophagus, characterized by nonspecific clinical manifestations in patients. EUS effectively demonstrates the tumor’s size, origin layer, and depth. Imaging examinations reveal its relationship with surrounding organs, providing crucial evidence for determining the surgical approach. The positivity of CD31 and D2-40 serves as significant pathological diagnostic criteria. With the increasing number of case reports, it is anticipated that clinical practitioners will develop a deeper understanding of this disease.
| 1. | Richetta L, Cirillo S, Isolato G, Cesarani F, Avataneo T. [The magnetic resonance aspects of cystic lymphangiomatosis. Apropos a case]. Radiol Med. 1993;85:135-138. [PubMed] |
| 2. | Hizawa K, Aoyagi K, Kurahara K, Suekane H, Kuwano Y, Nakamura S, Fujishima M. Gastrointestinal lymphangioma: endosonographic demonstration and endoscopic removal. Gastrointest Endosc. 1996;43:620-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Watson-Williams E. Specimen: Lymphangeioma of the Oesophagus. Proc R Soc Med. 1934;27:1288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 4. | Brady PG, Milligan FD. Lymphangioma of the esophagus--diagnosis by endoscopic biopsy. Am J Dig Dis. 1973;18:423-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Armengol-Miro JR, Ramentol F, Salord J, Costa MP, Palacin A, Vidal MT. Lymphangioma of the oesophagus. Diagnosis and treatment by endoscopic polypectomy. Endoscopy. 1979;11:185-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Tamada R, Sugimachi K, Yaita A, Inokuchi K, Watanabe H. Lymphangioma of the esophagus presenting symptoms of achalasia--a case report. Jpn J Surg. 1980;10:59-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Liebert CW Jr. Symptomatic lymphangioma of the esophagus with endoscopic resection. Gastrointest Endosc. 1983;29:225-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Castellanos D, Sebastián JJ, Larrad A, Menchen P, Senent C, Núñez JM, Lopez de la Riva M. Esophageal lymphangioma: case report and review of the literature. Surgery. 1990;108:593-594. [PubMed] |
| 9. | Yoshida Y, Okamura T, Ezaki T, Yano K, Kodate M, Murata I, Kaido M. Lymphangioma of the oesophagus: a case report and review of the literature. Thorax. 1994;49:1267-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Suwa T, Ozawa S, Ando N, Shinozaki H, Tsujitsuka K, Miki H, Makuuchi H, Kitajima M. Case report: lymphangioma of the oesophagus endoscopically resected. J Gastroenterol Hepatol. 1996;11:786-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Scarpis M, De Monti M, Pezzotta MG, Sonnino D, Mosca D, Milani M. Endoscopic resection of esophageal lymphangioma incidentally discovered. Diagn Ther Endosc. 1998;4:141-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Lee BI, Kim BW, Kim KM, Song HJ, Cho SH, Choi H, Choi MG, Choi KY, Chung IS, Cha SB, Sun HS, Park DH. Esophageal lymphangiomatosis: a case report. Gastrointest Endosc. 2002;56:589-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Yoon YH, Kim KH, Baek WK, Kim JT, Son KH, Han JY, Lee JI. Lymphangioma of the esophagus: surgical treatment. Ann Thorac Surg. 2004;78:e51-e53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Saers T, Parusel M, Brockmann M, Krakamp B. Lymphangioma of the esophagus. Gastrointest Endosc. 2005;62:181-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Sushil A, Aline PC, Metin O, Nadim H. Lymphangioma of the esophagus treated with endoscopic submucosal resection. J Gastroenterol Hepatol. 2007;22:284-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Best SR, Coelho DH, Ahrens WA, Atez G, Sasaki CT. Laser excision of multiple esophageal lymphangiomas: a case report and review of the literature. Auris Nasus Larynx. 2008;35:300-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Seybt MW, Postma GN. Giant esophageal lymphangioma. Ear Nose Throat J. 2008;87:500. [PubMed] |
| 18. | Arashiro M, Satoh K, Osawa H, Yoshizawa M, Nakano H, Ajibe H, Miura Y, Yoshida T, Hirasawa T, Yamamoto H, Sugano K. Endoscopic submucosal dissection of esophageal lymphangioma: a case report with a review of the literature. Clin J Gastroenterol. 2010;3:140-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Lee DG, Kim GH, Park DY, Jeong JH, Moon JY, Lee BE, Hosuk I, Song GA. Endoscopic submucosal resection of esophageal subepithelial lesions using band ligation. Endoscopy. 2011;43:822-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Xue L, Guo WG, Hou J, Ge D, Chen XJ. Huge lymphangiomatosis of the esophagus. Ann Thorac Surg. 2012;93:2048-2051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Zhao ZF, Kuang L, Zhang N, Ma SR, Yang Z, Han X, Zhao YF, Gao F, Gong ZJ, Yang L. Endoscopic diagnosis and treatment of esophageal cavernous lymphangioma. Surg Laparosc Endosc Percutan Tech. 2013;23:299-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Barbosa M, Ribeiro PM, Cotter J. Oesophageal lymphangioma: an exceedingly rare tumour. BMJ Case Rep. 2015;2015:bcr2015209605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Luo D, Ye L, Wu W, Zheng H, Mao X. Huge Lymphangioma of the Esophagus Resected by Endoscopic Piecemeal Mucosal Resection. Case Rep Med. 2017;2017:5747560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Zhao H, Xu W, Wang Z. Multiple Submucosal Masses in the Esophagus: Esophageal Lymphangiomatosis. Am J Gastroenterol. 2017;112:1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Hu L, Fu KI, Tuo B, Di L, Liu X, Zhao K, Wu H. Endoscopic submucosal dissection of a giant esophageal lymphangioma. Endoscopy. 2018;50:E181-E183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Min M, Liu Y. Lymphangioma of the Esophagus. Am J Gastroenterol. 2018;113:936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Cheng Y, Zhou X, Xu K, Huang Q. Esophageal lymphangioma: a case report and review of literature. BMC Gastroenterol. 2019;19:107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Shi Z, Huang X, Li K, Tu Q, Liu D, Zhao L, Yang H, Li D, Zhao Y, Zhang J, Li M, Liu B. Endoscopic resection of upper gastrointestinal lymphangioma: A single-center experience. Front Oncol. 2022;12:1030039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Martínez-Ares D, Lorenzo MJ, Souto-Ruzo J, Pérez JC, López JY, Belando RA, Vilas JD, Colell JM, Iglesias JL. Endoscopic resection of gastrointestinal submucosal tumors assisted by endoscopic ultrasonography. Surg Endosc. 2005;19:854-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |