Published online Nov 27, 2025. doi: 10.4240/wjgs.v17.i11.110884
Revised: August 20, 2025
Accepted: October 11, 2025
Published online: November 27, 2025
Processing time: 126 Days and 3.1 Hours
Peripherally inserted central catheter (PICC) is the preferred intravenous route for chemotherapy in patients with cancer, but its complications, especially deep vein thrombosis (DVT), are becoming increasingly prevalent. Medical staff proficient in intubation and maintenance techniques can reduce complications. The multivariate integration teaching model applies the integration of “teaching learning application” to medical training, which helps shift the prevention of complications from “passive management of complications” to “active con
To investigate the efficacy of the multivariate integration teaching model in patients with gastric cancer and concurrent DVT after PICC intubation and analyze its effect on patients’ quality of life index (QLI) and satisfaction.
A retrospective analysis of medical records of 100 patients with gastric cancer and PICC treated at Zhejiang Provincial People’s Hospital from May 2019 to November 2020 was conducted. According to the different treatment methods and teaching modes received by medical staff, they were divided into a control group and an experimental group, with 50 cases in each group. The routine clinical teaching model and the multivariate integration teaching model were administered to the medical staff for the control group and the experimental group, respectively, to compare the incidence rates of DVT and other adverse reactions, QLI scores, Karnofsky Performance Scale scores, Mental Status Scale in Non-Psychiatric Settings scores, patient satisfaction, medical staff’s test marks, and satisfaction evaluation of the teaching model.
Compared with the control group, the experimental group exhibited significantly lower incidence rates of DVT and other adverse reactions and MSSNS scores but significantly higher QLI scores, KPS scores, patient satisfaction, medical staff’s test marks, and their satisfaction evaluations of the teaching model (P < 0.05).
In a single-center practice, performing the multivariate integration teaching model for medical staff may effectively improve the patients’ QLI and satisfaction and may have certain application value in preventing DVT in patients with gastric cancer and PICC.
Core Tip: The aim of this study is to explore the preventive effect of using a multiple integral teaching model on deep vein thrombosis in cancer patients after peripherally inserted central catheter catheterization, and analyze its impact on patients’ quality of life and satisfaction. Compared with the control group using conventional clinical teaching mode, the experimental group using multivariate integration teaching model training for medical staff can effectively improve patients’ quality of life index and satisfaction, and has certain application value in preventing deep vein thrombosis in cancer peripherally inserted central catheter patients.
- Citation: Zhao XY, Lu YY, Hong X, Wu XY, Ruan MF. Preventive of deep vein thrombosis in cancer patients after peripherally inserted central catheter catheterization using a diversified comprehensive teaching model. World J Gastrointest Surg 2025; 17(11): 110884
- URL: https://www.wjgnet.com/1948-9366/full/v17/i11/110884.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i11.110884
The multivariate integration teaching model refers to the teaching model that integrates teaching, learning, and doing, and it has been widely implemented in schools due to the continuous development of the educational sector, which has remarkably transformed pedagogical approaches[1-3]. Medical students must not only acquire theoretical knowledge in the classroom but also use it in practice, facilitating the enhancement of their professional knowledge and skills. Therefore, the advantages and characteristics of the multivariate integration teaching model can be effectively utilized for the comprehensive development of medical students. In addition, the teaching model has been widely advocated and implemented in educational institutions and healthcare facilities, improving the practical skills of medical staff and enhancing patient treatment and recovery[4-6]. The insertion of a peripherally inserted central catheter (PICC) is necessary for administering chemotherapy in oncology patients, as it effectively mitigates the irritation caused by chemotherapy agents, reduces the risk of catheter damage from standard steel or indwelling needles, and decreases the frequency of punctures required. However, patients frequently experience deep vein thrombosis (DVT) after PICC intubation, which largely affects their health and daily activities; thus, DVT prophylaxis is a critical aspect of their care[7-9]. After selecting patients with gastric cancer and PICC as the research object, this study explored the influence of a multivariate integration teaching model for medical staff on DVT incidence, quality of life index (QLI), and patient satisfaction, with detailed findings presented below.
A retrospective analysis of medical records of 100 patients with gastric cancer and PICC treated at Zhejiang Provincial People’s Hospital from May 2019 to November 2020 was conducted. On the basis of the different treatment methods and instruction modes received by medical staff, they were divided into a control group and an experimental group, with 50 cases in each group. The age ranges of patients and medical staff in the experimental group were 29-73 years old and 19-48 years old, respectively, whereas those in the control group were 30-75 years old and 19-50 years old, respectively. The demographic data of patients and medical staff, including gender and age, were not statistically different (P > 0.05; Table 1).
| Group | Experimental group | Control group | χ2/t | P value |
| Gender (male/female) | 25/25 | 26/24 | 0.04 | 0.84 |
| Patients’ age (years old) | 36.91 ± 4.35 | 36.30 ± 4.50 | 0.69 | 0.49 |
| Height (cm) | 169.22 ± 7.46 | 168.76 ± 7.55 | 0.30 | 0.76 |
| Weight (kg) | 72.59 ± 5.02 | 72.00 ± 5.18 | 0.58 | 0.56 |
| Duration of disease (months) | 3.55 ± 0.54 | 3.72 ± 0.53 | 1.59 | 0.12 |
| Smoking history | 19 | 17 | 0.17 | 0.68 |
| Drinking history | 28 | 30 | 0.16 | 0.69 |
| Hypertension | 3 | 5 | 0.83 | 0.36 |
| Diabetes | 1 | 2 | 0.39 | 0.53 |
| Hyperlipidemia | 4 | 2 | 0.95 | 0.33 |
| Age of medical care personnel (years old) | 31.00 ± 4.38 | 30.56 ± 4.41 | 0.50 | 0.62 |
| Qualification of medical staff (years) | 5.16 ± 1.30 | 5.11 ± 1.32 | 0.19 | 0.85 |
Inclusion criteria: (1) The patients were diagnosed with gastric cancer and underwent PICC intubation; (2) The patients were at least 18 years old; (3) Medical staff who have worked for at least 3 years and hold the title of “primary nurse practitioner” or above; (4) The patients had no history of drug allergies, substance abuse, or severe addiction; (5) The patients had no other organic disease; and (6) The study was approved by the Ethics Committee of Zhejiang Provincial People’s Hospital, which agreed to waive informed consent.
Exclusion criteria: (1) The patients had altered consciousness and were unable to participate in the study; (2) The patients presented with other organic diseases; and (3) The patients failed to meet the criteria for PICC intubation.
The routine clinical teaching model was implemented for the medical staff responsible for the patients in the control group. In particular, the medical staff underwent routine training and instruction, performed routine treatment and nursing protocols, monitored the basic condition of patients with PICC, maintained and sanitized the PICC catheter, and advised patients on precautions such as wearing loose and comfortable clothes to prevent compression and friction on the catheter.
The medical staff in the experimental group received the multivariate integration teaching model. A nurse with a PICC specialist nurse certificate or above, a bachelor’s degree, at least 5 years of work experience, expertise in catheterization techniques, extensive clinical knowledge, rich clinical experience, and certain research abilities will serve as the teaching instructor. By combining teaching, learning, and doing into medical training, medical staff could not only learn and reinforce relevant theoretical knowledge but also foster collaboration between medical treatment and nursing, enabling a close link between the two disciplines. Compared with traditional classroom education, this hospital teaching model was more intuitive and prompter, enabling students to promptly identify and correct their deficiencies while gaining a clear understanding of their medical and nursing responsibilities in relation to their practical experience. First, it involved an understanding of the PICC catheterization process, delivery of theoretical and practical instruction on PICC catheterization via a Microsoft PowerPoint presentation, and use of case analysis to elucidate the PICC catheterization process. Second, PICC maintenance and replacement of PICC dressings under the guidance of the instructor were practiced. The instructor is always ready to provide assistance and instruction in the event of any problems. During the process, rigorous aseptic techniques should be observed, and each nurse should provide operational guidance once and gradually transition to clinical exams. Finally, the evaluation criteria encompassed specialized theoretical examinations, operational assessments, medical staff’s test scores, and satisfaction evaluations of teaching modes.
With the knowledge learned, the medical staff could deliver enhanced professional treatment and nursing to patients with gastric cancer and PICC, such as performing Allen’s test prior to puncture, assessing the feasibility of radial artery catheterization based on the test result, and reducing puncture-related discomfort. The medical personnel carefully disinfected and cleaned the anterior section of the catheter to avoid infection from microorganism entry and the incidence of intraductal thrombosis. They strictly adhered to the catheter maintenance protocol, promptly identified thrombus warning signals, strengthened workplace communication, and developed detailed treatment and nursing plans for the patients.
During catheterization, patients were observed for DVT. A questionnaire on their QLI scores, Karnofsky Performance Scale (KPS) scores, and satisfaction was administered, and the professional grades and recognition of the medical staff’s teaching model were documented and analyzed. The patients’ conditions were consistently monitored and assessed during home observation. Telephone follow-ups were performed in a timely manner, and if necessary, home visits were conducted. The nursing plan was adjusted in a timely manner based on the follow-up results.
All patients were treated with dual lumen 5Fr catheters (Bard Corporation, United States), operated by specialized nurses with PICC puncture qualifications in our department. Ultrasound-guided modified Sedinger technique was used for upper arm vein catheterization. The placement of catheters in the left and right upper limbs was determined according to the patient’s wishes and vascular condition. In the absence of exceptional circumstances, the right upper limb was preferred. The Guiyao vein was the first choice for vascular puncture, followed by the brachial vein and cephalic vein. The patients were notified of precautions and possible complications before catheterization, and auxiliary examinations were completed.
Before PICC catheterization, the patient must be positioned supine with the arm on the puncture side extended at a 90-degree angle, fully exposing the puncture area. The puncture site was disinfected in a spiral pattern, centering on the puncture point. A sterile cloth was placed to cover the patient’s entire body and operating area. The LOGIQ Book (General Electric Company, MA, United States) ultrasound guidance system was used to evaluate the patient’s venous condition and measure the target vein diameter, vessel depth, and arm circumference. Under ultrasound guidance, the puncture needle was inserted into the vein, and a guide wire was inserted after the blood returned. The puncture needle was withdrawn, and a skin expander was employed along the guide wire to enlarge the puncture site on the skin. The tear able sheath was inserted over the guidewire, the guidewire and dilator were withdrawn, and the sheath was maintained in the vein. The PICC catheter was slowly inserted into the vein through the sheath until it reached the predetermined length. The sheath was detached and ruptured while maintaining the catheter’s position in the vein. Ultrasound was employed throughout catheterization to explore the internal jugular vein and subclavian vein, ensuring the catheter’s direction was devoid of abnormalities. The right atrial electrocardiogram detection catheterization technique was utilized to verify that the catheter tip was located at the intersection of the superior vena cava and the right atrium or at the lower segment of the superior vena cava. Follow up chest X-ray was conducted after surgery to determine the position of the catheter tip. Any abnormalities were addressed immediately, and the patient was provided with health education.
The incidence rates of DVT and other adverse reactions, QLI scores, KPS scores, Mental Status Scale in Non-Psychiatric Settings (MSSNS) scores, patient satisfaction, and medical staff’s test marks and satisfaction evaluation of the teaching model were compared between the two groups. The Mindray color Doppler ultrasound diagnostic instrument (model: Nuewa R9, Shenzhen Mindray Medical Co., Ltd., China) was used for DVT examination. A high-frequency linear probe was used with a frequency adjusted to 12-14 MHz, and the patient was kept in a supine position to examine the lower limb veins. Guiding the patient’s movements enhanced the observation of venous valve function in each segment.
The maximum KPS score was 100 points, with high scores indicating superior physical condition and high tolerance to side effects[10]. The scoring criteria for the QLI included daily activities, work and life, and interpersonal relationships. The maximum score for each criterion was 10 points, with high scores indicating improved QLI, and vice versa. The MSSNS score established 60 points as the threshold. Scores below 60 points indicated normal mental status, scores between 60 and 70 points suggested mild abnormal mental status, and scores over 70 points reflected abnormal mental status[11].
Patient satisfaction referred to the satisfaction of patients regarding the accepted treatment and nursing care, which was classified as fully satisfied (completely recognized the treatment and nursing mode), satisfied (generally recognized the treatment and nursing mode), and dissatisfied (quite disagreed with the treatment and nursing mode and sought relevant modifications). The test for medical staff comprised 10 items, including theoretical knowledge assessment, practical skills assessment, and daily work assessment. The total score of each item was 10 points, with higher scores indicating superior quality. The medical staff’s satisfaction with the teaching model was classified as very satisfied, satisfied, and dissatisfied. “Very satisfied” indicated that they could learn the expected knowledge and skills under the teaching model and considered it highly worthy of promotion. “Satisfied” indicated that they learned most of the expected knowledge and addressed key problems. “Dissatisfied” suggested that the model hindered rather than enhanced work efficiency.
This study used SPSS version 20.0 for data processing and GraphPad Prism 7 for graphical representation. The items included comprised enumeration and measurement data, which were expressed by n (%) and mean ± SD and analyzed using the χ2 test and t-test, respectively. Differences were considered statistically significant at P < 0.05.
The incidence rates of DVT and other adverse reactions of the experimental group were significantly lower than those of the control group (P < 0.05; Table 2).
| Group | DVT | Infection | Phlebitis | Catheter shedding | Other adverse reactions |
| Experimental group | 1 (2) | 3 | 1 | 0 | 8% |
| Control group | 7 (14) | 5 | 3 | 4 | 24% |
| χ2 | 4.89 | 4.76 | |||
| P value | 0.03 | 0.03 |
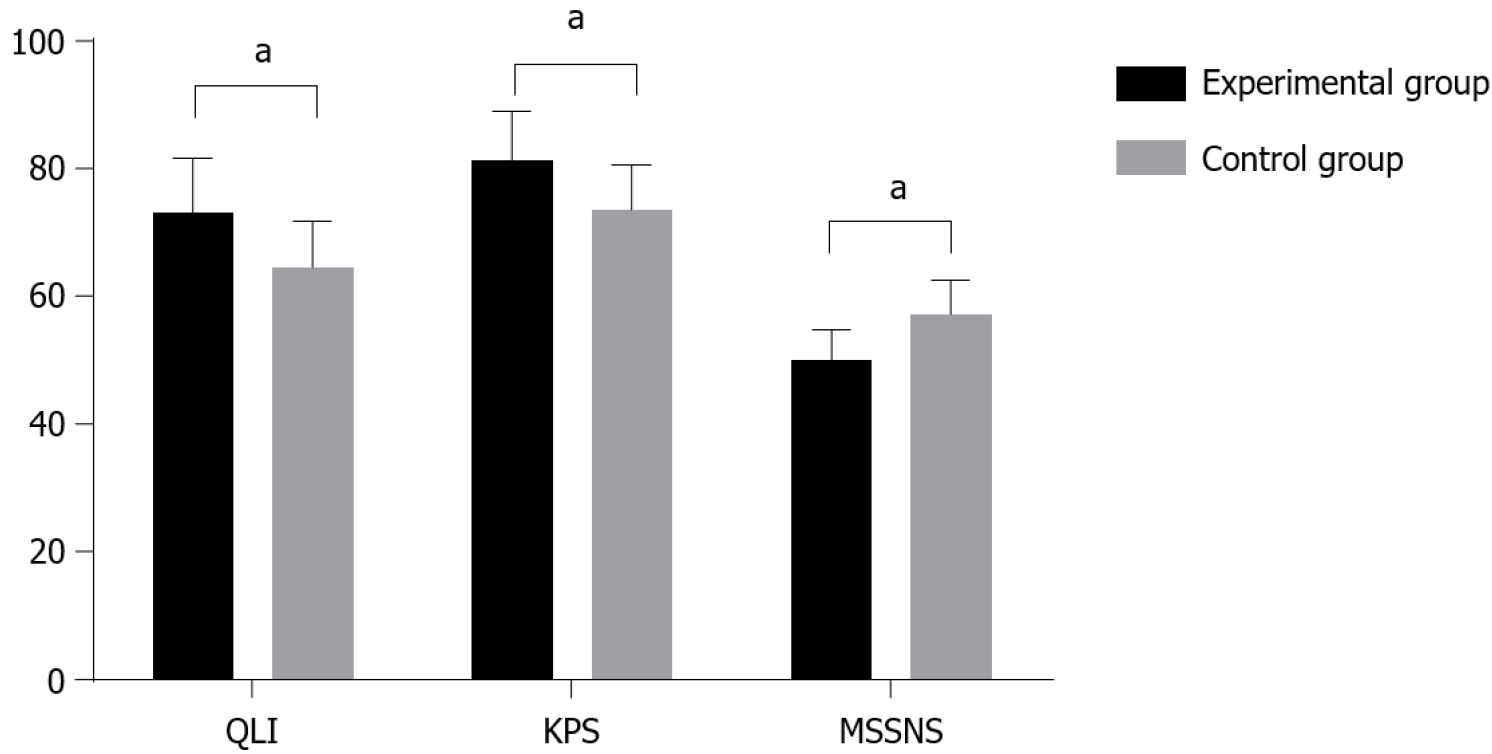
The experimental group had significantly higher QLI and KPS scores and lower MSSNS scores than the control group (P < 0.05; Figure 1). The QLI scores of the experimental group and the control group were 73.05 ± 8.46 and 64.49 ± 7.22, respectively, and an indicated that the results were statistically significant (t = 5.44, P < 0.001). The KPS scores of the experimental group and the control group were 81.24 ± 7.71 and 73.35 ± 7.28, respectively, and ‘b’ indicated that the results were statistically significant (t = 5.26, P < 0.001). The MSSNS scores of the experimental group and the control group were 50.03 ± 4.86 and 57.12 ± 5.33, respectively, and ‘c’ indicated that the results were statistically significant (t = 6.95, P < 0.001).
The experimental group presented significantly higher patient satisfaction than the control group (P < 0.05; Table 3).
| Group | Fully satisfied | Satisfied | Dissatisfied | Total satisfaction |
| Experimental group | 26 | 18 | 6 | 88% |
| Control group | 19 | 15 | 16 | 68% |
| χ2 | 5.83 | |||
| P value | 0.02 |
The medical staff of the experimental group had significantly higher test marks in treating and nursing patients than the control group (P < 0.05; Table 4).
| Group | Theoretical knowledge | Practical ability | Daily work | Total marks |
| Experimental group | 8.59 ± 0.88 | 9.00 ± 0.74 | 8.12 ± 1.01 | 86.32 ± 7.71 |
| Control group | 7.10 ± 0.62 | 7.58 ± 0.66 | 7.33 ± 0.59 | 78.87 ± 7.02 |
| t | 9.79 | 10.13 | 4.78 | 5.05 |
| P value | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
The satisfaction of medical staff with the teaching model in the experimental group was significantly higher than that in the control group (P < 0.05; Table 5).
| Group | Fully satisfied | Satisfied | Dissatisfied | Total satisfaction |
| Experimental group | 35 | 15 | 0 | 100% |
| Control group | 27 | 14 | 9 | 82% |
| χ2 | 9.89 | |||
| P value | 0.002 |
The multivariate integration teaching model aims to combine teaching, learning, and doing into an innovative theory-practice pedagogical framework, allowing students to acquire basic knowledge and theoretical understanding, implement theory in practice, and achieve comprehensive development. As medical technology continually evolves, some medical staff require ongoing education and training after graduating to work in hospitals[12-14]. By implementing the multivariate integration teaching model into their learning, they can swiftly adapt to advancements in the hospital settings and enhance the treatment environment for patients[15-17]. Patients with gastric cancer are susceptible to DVT after PICC intubation, which can seriously affect their medical prognosis; thus, prioritizing treatment and nursing care for such patients is essential to prevent DVT[15,18,19]. To explore the clinical effect of the multivariate integration teaching model in preventing DVT for patients with gastric cancer and PICC and determine its influence on the patients’ QLI and satisfaction, we selected 100 patients as the research object to receive treatment and care from various medical staff trained under different teaching models.
According to the study results, after medical staff trained using the multivariate integration teaching model provided treatment and nursing to patients in the experimental group, the patients’ QLI, DVT incidence, and satisfaction remarkably improved, indicating an obviously better application effect than the routine teaching model. The occurrence of DVT was not due to a single factor, but it was related to the patient’s own condition, changes in blood flow after intubation, and location of the penetrating vessel. Therefore, factors such as puncture location, puncture method, and nursing content were associated with the prevention of DVT[20-22]. The implementation of the multivariate integration teaching model, which facilitated the combination of teaching, learning, and doing, and the close interaction between health and care enabled medical staff to gain a deep understanding of patients’ basic conditions. This awareness fostered increased vigilance toward patients, thereby mitigating the incidence of DVT. Consequently, DVT incidence was effectively controlled, leading to an improvement in patients’ QLI and satisfaction levels. From the perspective of medical staff, learning at work and applying knowledge into practice resulted in a significant improvement in their test scores. Zhang and Wang[23] concluded that integrated health care reform can enhance the emotional well-being of patients with PICC and reduce complications such as catheter dislodgment. This conclusion was similar to the results of the study, demonstrating that this research was scientific and reliable.
Implementing the multivariate integration teaching model for medical staff may effectively improve the patients’ QLI and satisfaction, and it has certain application value in preventing DVT in patients with gastric cancer and PICC.
| 1. | Gozzo C, Farina R, Coppolino P, Cancemi G, Foti PV, Palmucci S, Venturini M, Basile A. Double May-Thurner syndrome causing chronic deep vein thrombosis and natural venous femoro-femoral bypass: a description of rare case. Radiol Case Rep. 2021;16:1608-1612. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Fares Y, Sinzogan-Eyoum YC, Billoir P, Bogaert A, Armengol G, Alexandre K, Lammens J, Grall M, Levesque H, Benhamou Y, Miranda S. Systematic screening for a proximal DVT in COVID-19 hospitalized patients: Results of a comparative study. J Med Vasc. 2021;46:163-170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Rana S, Brutsaert E. Deep Venous Thrombosis in a Patient With Cushing’s Syndrome. J Endocr Soc. 2021;5:A581-A581. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Oguz SH, Buyukasik Y, Yildiz BO. Management of Recurrent Deep Vein Thrombosis in a Transgender Woman. J Endocr Soc. 2021;5:A792-A792. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Li Y, Sutedjo J, Chen YC, Gu JP. Efficacy of modified pressure cuff for thrombolytic treatment on lower extremity deep venous thrombosis. Medicine (Baltimore). 2021;100:e25664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Liu W, He L, Zeng W, Yue L, Wei J, Zeng S, Wang X, Gong Z. Peripherally inserted central venous catheter in upper extremities leads to an increase in D-dimer and deep vein thrombosis in lower extremities. Thromb J. 2021;19:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Guo HN, Cao Y, Lian SF, Zhang WB. [Application effect of nursing intervention based on FMEA in preventing deep venous thrombosis caused by PICC catheter chemotherapy for malignant tumors]. Guoji Yiyao Weisheng Daobao. 2022;28:3153-3157. [DOI] [Full Text] |
| 8. | Sun TY, Fang JX, Qian HY. [The application value of nursing mode guided by deep vein thrombosis risk score in PICC patients with malignant tumors]. Guoji Hulixue Zazhi. 2023;42:3601-3604. [DOI] [Full Text] |
| 9. | Pi LY. [The preventive effect of nursing intervention based on feedforward control theory on deep vein thrombosis in leukemia PICC patients]. Guoji Hulixue Zazhi. 2022;41:2249-2252. [DOI] [Full Text] |
| 10. | Joga S, Bansal A, Talwar V, Bothra SJ, Dash P, Goel V, Koyyala VPB. Spontaneous pulmonary arterial embolization: A rare complication of the silicon-based peripherally inserted central venous catheter (PICC). J Vasc Access. 2022;23:471-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Bozzi M, Raffaghelli JE, Zani M. Peer Learning as a Key Component of an Integrated Teaching Method: Overcoming the Complexities of Physics Teaching in Large Size Classes. Educ Sci. 2021;11:67. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Souza BICC, Silva MMD. Occlusions in peripherally inserted central venous catheters in pediatric patients in antineoplastic chemotherapy. Rev Gaucha Enferm. 2021;42:e20190495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Patel S, Vazquez JA, Chase A, Ebong E. 89. A Collaborative & Novel Antimicrobial Stewardship Initiative– Mandatory Approval of Peripherally Inserted Central Venous Catheters. Open Forum Infect Dis. 2020;7:S60-S61. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Hueppchen N, Dalrymple JL, Hammoud MM, Abbott JF, Casey PM, Chuang AW, Cullimore A, Davis KR, Dugoff L, Espey EL, Kaczmarczyk JM, Nuthalapaty FS, Peskin E, Pradhan A, Katz NT; Association of Professors of Gynecology and Obstetrics Undergraduate Medical Education Committee. To the point: medical education reviews-ongoing call for faculty development. Am J Obstet Gynecol. 2011;205:171-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Inoue M, Miyazaki N, Suematsu H, Yamagishi Y, Mikamo H. Necrotizing fasciitis on a peripherally inserted central venous catheter site. Pediatr Int. 2020;62:1303-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Pu YL, Li ZS, Zhi XX, Shi YA, Meng AF, Cheng F, Ali A, Li C, Fang H, Wang C. Complications and Costs of Peripherally Inserted Central Venous Catheters Compared With Implantable Port Catheters for Cancer Patients: A Meta-analysis. Cancer Nurs. 2020;43:455-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 17. | Silva JT, Lagares-Velasco A, Fernández-Ruiz M, González-Monterrubio G, Pérez-Cárdenas MD, Aguado JM, López-Medrano F. Peripherally inserted central venous catheter placed and maintained by a dedicated nursing team for the administration of antimicrobial therapy vs. another type of catheter: a retrospective case-control study. Enferm Infecc Microbiol Clin (Engl Ed). 2020;38:425-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Van Mechelen K, Mahieu L. A new technique for difficult removal of a peripherally inserted central venous catheter (PICC) in a neonate. Eur J Pediatr. 2021;180:973-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Kubiak A, Jazmati T, Sare A, Kumar A, Shukla PA. Overutilization of Peripherally Inserted Central Venous Catheters in the Hospital Setting. J Radiol Nurs. 2020;39:302-304. [DOI] [Full Text] |
| 20. | Yintian L, Qiuying L, Jinai H, Na L. Study on the Effects of IC-ECG Method in Neonatal PICC Catheterization. Am J Pediatr. 2020;6:178-182. [DOI] [Full Text] |
| 21. | Benvenuti S, Parolini F, Ceresoli R, Orizio P, Alberti D. Technique for replacement of Groshong® peripherally inserted central venous catheters (PICCs) in children. Minerva Pediatr (Torino). 2022;74:403-407. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Suzuki D, Kobayashi R, Sano H, Yanagi M, Hori D, Matsushima S, Nakano T, Kobayashi K. Peripherally Inserted Central Venous Catheter for Pediatric and Young Adult Patients With Hematologic and Malignant Diseases. J Pediatr Hematol Oncol. 2020;42:429-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Zhang L, Wang Y. [The effect of group cognitive behavioral intervention combined with medical care integration positive suggestion on mood state and catheter maintenance compliance of PICC patients with hematopathy]. Linchuang Xinshenjibing Zazhi. 2021;27:72-76. [DOI] [Full Text] |