Published online Nov 27, 2025. doi: 10.4240/wjgs.v17.i11.110973
Revised: August 18, 2025
Accepted: October 11, 2025
Published online: November 27, 2025
Processing time: 133 Days and 2.2 Hours
Older patients with liver cancer often experience impaired pulmonary function post-surgery, increasing complications and recovery challenges.
To investigate the effects of evidence-based stratified management and stepwise training in the perioperative pulmonary rehabilitation of older patients with liver cancer, providing a basis for clinical application.
In total, 120 older patients with liver cancer who underwent surgery at our hospital between February 2023 and February 2025 were selected and randomly divided into study and control groups, with 60 patients in each group. All the patients underwent radical hepatectomy. Postoperatively, the control group received routine nursing management and rehabilitation training, while the study group received evidence-based stratified management combined with stepwise training for a continuous intervention period of one week. Time to first ambu
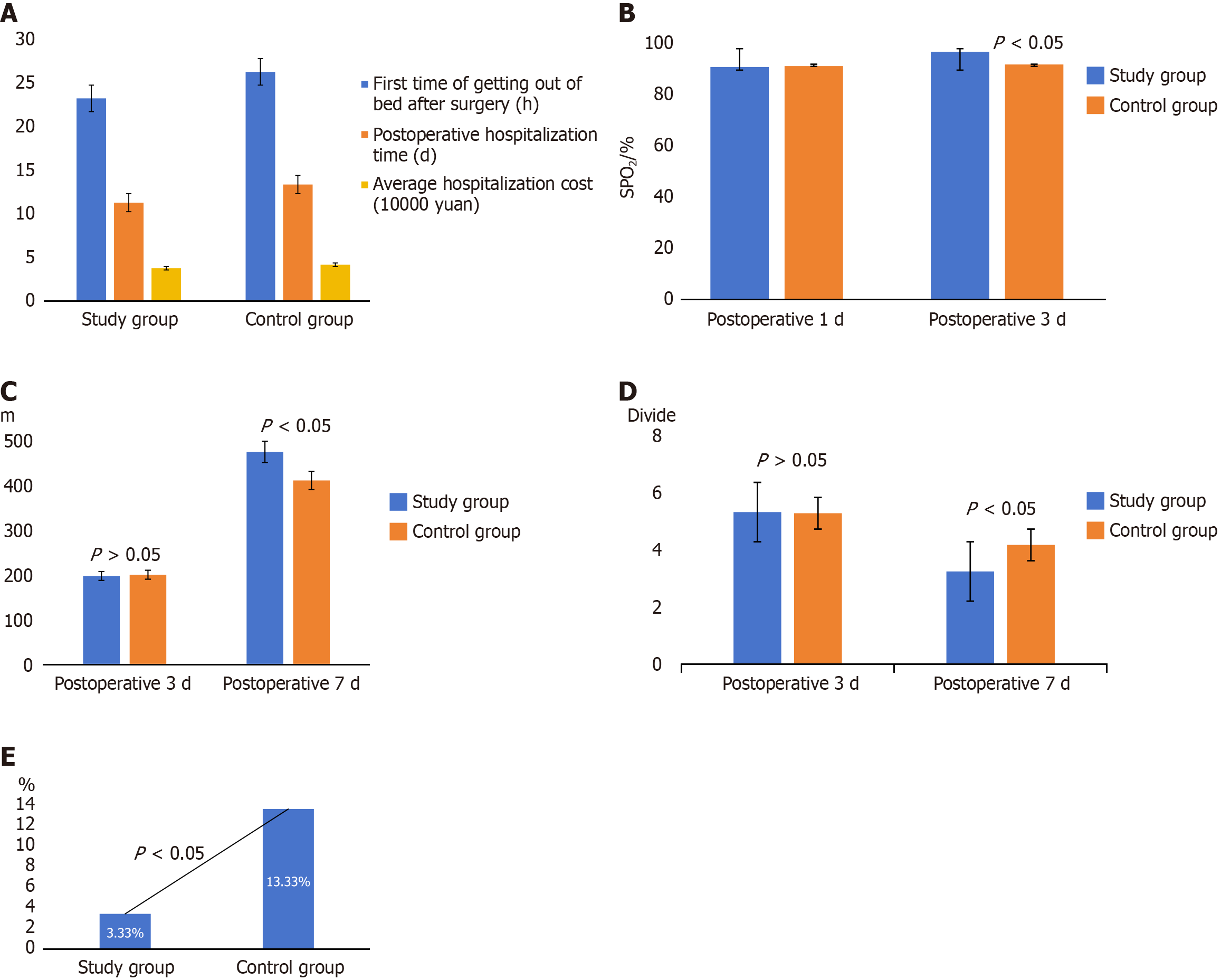
The study group had a significantly shorter time to first ambulation, shorter hospital stays, and lower average hospitalization costs than the control group (P < 0.05). On postoperative day 1, there was no significant difference in SPO2 between the groups (P > 0.05); however, on postoperative day 3, the study group had significantly higher SPO2 (P < 0.05). On postoperative day 7, the study group showed a significantly longer 6-minute walk distance and lower Borg scores than the control group (P < 0.05). The incidence of postoperative complications in the study group was 3.33%, which was significantly lower than that in the control group (13.33%; P < 0.05).
Implementing evidence-based stratified management combined with stepwise training in the perioperative pulmonary rehabilitation of older patients with liver cancer is improves lung function, reduces complications, and promotes effective recovery, demonstrating significant clinical value.
Core Tip: This study evaluated a novel rehabilitation strategy that combined evidence-based stratified management and stepwise training in older patients with liver cancer. The findings indicated that this approach enhanced postoperative recovery, improved pulmonary function, shortened hospital stay, and reduced complication rates, thereby supporting its clinical application in perioperative pulmonary rehabilitation.
- Citation: Zhang Q, Liu CD, Lu XX, Zhang SS, Gong JH, Ding J. Effect of stratified management and stepwise training on pulmonary rehabilitation in older patients with liver cancer. World J Gastrointest Surg 2025; 17(11): 110973
- URL: https://www.wjgnet.com/1948-9366/full/v17/i11/110973.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i11.110973
Liver cancer, one of the most common malignant tumors of the digestive system, is characterized by high morbidity and mortality rates and poses a serious threat to human health and life expectancy worldwide. Surgical resection is the primary curative treatment for hepatocellular carcinoma[1]. However, older patients generally have poorer baseline pulmonary function than young individuals, and are often burdened with chronic comorbidities. Consequently, older patients undergoing radical liver cancer surgery under general anesthesia are at a higher risk of postoperative pulmonary complications, such as pneumonia and atelectasis, with reported incidence rates ranging from 13% to 53%[1]. These complications not only prolong hospitalization and increase healthcare costs but also adversely affect recovery, quality of life, and long-term prognosis. Therefore, optimizing perioperative pulmonary rehabilitation strategies for older patients with liver cancer is clinically important.
In recent years, evidence-based stratified management has emerged as a refined nursing approach that integrates the best available clinical evidence, patient characteristics, and healthcare resources to guide individualized perioperative care[2]. Unlike traditional uniform rehabilitation protocols, this method employs a systematic risk assessment, covering surgical, physiological, and psychosocial dimensions, to classify patients into different risk tiers, thereby enabling targeted interventions for each subgroup. Studies on populations undergoing cardiothoracic and abdominal surgery have demonstrated that such stratification can improve functional recovery, reduce complication rates, and enhance resource efficiency[3].
Whereas, stepwise rehabilitation training, a progressive patient-centered approach, has been increasingly applied to pulmonary and cardiac rehabilitation. This method tailors exercise type, intensity, and duration to the patient’s tolerance, gradually increasing the load to stimulate cardiopulmonary adaptation while avoiding overtraining[4]. Evidence suggests that stepwise programs enhance respiratory muscle strength, improve exercise endurance, and support psychological wellbeing, particularly in older or frail patients recovering from major surgeries. In oncological rehabilitation, phased training interventions have been beneficial in improving quality of life, physical performance, and adherence to recovery plans[5].
However, despite the documented benefits of evidence-based stratified management and stepwise rehabilitation in other clinical settings, their combined application in perioperative pulmonary rehabilitation of older patients with liver cancer remains underexplored. Integrating these two strategies may not only allow for precise, individualized rehabilitation planning but also ensure safe and effective progression of functional recovery. Therefore, this study aimed to evaluate the clinical effectiveness of evidence-based stratified management combined with stepwise rehabilitation training in the perioperative pulmonary rehabilitation of older patients with liver cancer, with the goal of providing a novel and practical approach for improving postoperative outcomes in this vulnerable population.
This clinical study included 120 older patients with liver cancer, who underwent surgery at our hospital between February 2023 and February 2025. The study was approved by the hospital ethics committee, and consent was obtained. The inclusion criteria were as follows: (1) Patients diagnosed with primary liver cancer through pathological and laboratory tests, meeting diagnostic criteria[5]; (2) Normal consciousness and comprehension; (3) Aged ≥ 65 years; (4) Cardiac function graded New York Heart Association classification I-III; (5) Eligible for laparoscopic liver resection; (6) Stable vital signs before surgery; and (7) Informed consent obtained from patients and families. The exclusion criteria were as follows: (1) Patients with preoperative American Society of Anesthesiologists grade > 3; (2) Severe postoperative complications; (3) Combined dysfunction of the heart, lungs, and kidneys; and (4) Systemic infections.
Patients were randomly divided into two groups using a random number table, with 60 patients in each group. The control group comprised 33 men and 27 women aged 66-73 years, with a mean age of 68.67 ± 3.41 years; the surgical types consisted of 21 cases of irregular hepatic segmentectomy and 39 cases of regular hepatic resection. The study group comprised 36 men and 24 women aged 65-74 years, with a mean age of 68.83 ± 3.55 years; the surgical types consisted of 19 cases of irregular hepatic segmentectomy and 41 cases of regular hepatic resection. The basic clinical characteristics of the two groups were similar (P > 0.05), indicating comparability.
All patients underwent liver resection and perioperative interventions, such as antibiotics and expectorants, along with the necessary examinations. Postoperatively, the patient received pain management, nutritional support, and antibiotic treatments.
The control group received routine nursing care and rehabilitation training.
Preoperative preparation: Proactive doctor-patient communication, systematic explanation of the surgical plan, and precautions to ensure full understanding and cooperation from patients and families.
Postoperative care: (1) Monitoring of vital signs: Real-time monitoring of heart rate, blood pressure, oxygen saturation, and prompt emergency response to abnormalities; (2) Infection control: Standardized catheter and drainage bag replacement, reinforced contact isolation protocols, and patient guidance on proper coughing and sputum expectoration techniques; (3) Psychological intervention: On postoperative day 3, the psychological status of the patients were assessed, causes of negative emotions were identified, and targeted counseling and supportive interventions were implemented to alleviate emotional distress; (4) Nutritional support: Customized high-protein, high-vitamin diet plans to promote wound healing and recovery of physical functions; and (5) Rehabilitation training: Patients were guided for early bedside activities, adaptive upper and lower limb physical training, and progressive strengthening of respiratory muscles and limb motor functions.
The study group received evidence-based stratified management combined with stepwise training as follows: (1) Evidence-based stratification: A stratified management team consisting of a medical team leader, head nurse, rehabilitation physician, attending doctors, and nurses was formed. The medical team leader and head nurse acted as team leaders to coordinate the team activities. They organized evidence-based stratified management training for the perioperative rehabilitation of older patients with liver cancer and conducted systematic training and assessments for team members. After passing the assessments, the team performed ward rounds and consultations and developed rehabilitation plans. The rehabilitation physician was responsible for defining the rehabilitation plan, guiding the techniques, and formulating stratified management measures; (2) Level-based assessment: Responsible doctors and nurses conducted systematic assessments of patients, including basic (age, comorbidities, thoracic surgery history, etc.), specialized (type of surgery, anesthesia method, preoperative nutritional status, etc.), and risk evaluations (frailty index, cough score, muscle strength, etc.). The rehabilitation physician then stratified the patients based on their assessment results, as shown in Table 1; and (3) Clinical nursing: Based on evidence-based clinical stratification, perioperative stratified management and rehabilitation training were implemented, specifically stratified management.
| Grade | Postoperative complication risk | Frailty index | Liver function grade | Cough score | Activity level | Surgical method |
| I | High risk | > 2 | Grade A | 0-2 points | Bedridden | Open surgery |
| II | Medium risk | 1-2 | Grade B | 3-4 points | Lying/standing | Laparoscopic surgery |
| III | Low risk | 0 | Grade C | 4-5 points | Walking | Laparoscopic surgery |
Preoperative: Surgical risks were strictly assessed, response plans were formulated, preoperative education was provided to patients and their families, and the surgical plan was clearly explained.
Intraoperative: The least traumatic and effective surgical method was selected, hemodynamics was strictly monitored, and body temperature and coagulation were strictly managed.
Postoperative: These were based on enhanced recovery after surgery (ERAS) principles[6], ERAS is a multidisciplinary, evidence-based perioperative care concept aimed at reducing the physiological and psychological stress of surgery through a series of optimized measures. If ERAS employs effective and reasonable modifications to conventional treatment procedures, it can alleviate surgical stress responses, reduce the occurrence of surgical complications, and lower surgical risks, thereby accelerating postoperative recovery. Continuous monitoring of vital signs, liver and kidney functions, coagulation, infection indicators, and neurological status provides early enteral nutrition support, gradually resumes oral intake, actively prevents and manages complications, dynamically assesses prognosis, and generally requires long-term rehabilitation or nursing support after discharge.
Preoperative: Prehabilitation was strengthened, dynamic nutritional assessments were conducted to ensure good nutritional status; enteral or parenteral nutrition support was provided if necessary; patients were guided on appropriate aerobic balance training; cognitive interventions were conducted; families were informed regarding delirium risks and prevention.
Intraoperative: Enhanced monitoring, implemented active temperature management, and used multimodal analgesia.
Postoperative: Vital signs, liver and kidney function, coagulation, electrolytes, and other physiological indicators were closely monitored; early nutritional support was provided with protein intake of 1.2-2.0 g/kg/day; venous thromboembolis was strictly avoided, and pharmacological prevention was combined with enhanced rehabilitation and activity.
Preoperative: Systematic examination and assessment were conducted, a balanced diet was maintained, appropriate aerobic exercises were encouraged, and psychological support was strengthened.
Intraoperative: Fluid management and active warming was strictly maintained; analgesia tailored to the patient was provided.
Postoperative: On postoperative day 1, bedside activities were conducted according to the patient’s condition; oral intake was initiated as early as possible; drainage and urinary catheters were removed early depending on the postoperative status; and vital signs, liver function, and fluid balance were closely monitored. Active prevention of complications including venous thromboembolis, infection, and liver dysfunction was ensured.
The responsible nurse implemented all interventions and conducted the corresponding stepwise rehabilitation training based on evidence-based stratification.
Level 1: (1) Respiratory training: Patients were guided on resistive breathing exercises, pursed-lip breathing, and maintaining positive airway pressure, such as balloon blowing exercises to strengthen respiratory muscles by overcoming resistance. Additionally, the patients were guided on abdominal pressure breathing using weights like sandbags or water bottles, starting at 0.5 kg and increasing to 1.5 kg, 20 minutes per session, twice daily; (2) Resistance training: The patients were guided to perform moderate aerobic exercises such as standing breathing exercises for 10-15 minutes per session, twice daily; and used resistance bands or balls for chest expansion, shoulder abduction, and seated rowing exercises, 5-8 sets daily; (3) Endurance training: Seven-step bedside exercise method was used, transitioning from independent bed activities to bedside activities until standing and walking independently, later attempting climbing stairs, which was adjusted according to patient endurance to ensure safety; (4) Whole-body muscle strength training: After postoperative ambulation was allowed, sitting and standing training and moderate walking were performed; and (5) Sputum clearance training: The patients were instructed on effective sputum clearance techniques; whereas, family members were instructed on percussion techniques and nebulization inhalation as required.
Level 2: (1) Respiratory training: The patients were guided on diaphragmatic breathing to improve diaphragm movement and ventilation rate, pursed-lip breathing and diaphragmatic breathing training, controlling respiratory rate and exhalation time, 10 minutes per session, twice daily; (2) Resistance training: Similar to level 1 but with reduced intensity, 10-15 minutes per session, once daily; and (3) Muscle strength and endurance training: Arm lifting was appropriately performed in bed, crossing both hands above the head, 20 sets per session, twice daily; straight leg raises were progressively performed, lifting legs to 30° from bed and holding for 10 seconds, 10 sets per session, twice daily; stretching sitting-up exercises were performed, grasping bed rails and using upper limb strength to sit up, 10 repetitions per session, twice daily; “air cycling” exercise were performed to strengthen lower limb muscles (rectus femoris, vastus lateralis) and abdominal muscles by lifting legs and simulating cycling motions, 5-10 minutes per session, twice daily.
Level 3: (1) Respiratory training: Breathing patterns were adjusted according to patient condition, changing shallow rapid breathing to deep slow breathing, training respiratory muscles and reducing accessory muscle use; the patients were guided on deep breathing, pursed-lip breathing, and diaphragmatic breathing, 5-10 minutes per session, three times daily, starting postoperatively; and (2) Resistance training: Early postoperative passive training of upper and lower limb joints assisted by nursing staff, including flexion, extension, adduction, abduction, internal rotation, and external rotation, 20 repetitions per movement, twice daily; progressively, passive cycling training performed for 5-20 minutes per session, twice daily.
Surgical conditions: The first postoperative ambulation time, length of hospital stay, and average hospitalization costs for both groups were recorded.
Oxygen saturation (SPO2): SPO2 refers to the percentage of oxygenated hemoglobin (HbO2) in the total hemoglobin of the arterial blood, which reflects the efficiency of oxygen transport in the body and is an important indicator of respiratory and circulatory function. Measurements were performed using a calibrated portable pulse oximeter (Mindray PM-60; Shenzhen, China). Patients were placed in a resting, semi-recumbent position in a quiet ward environment with ambient temperature maintained at 22-24 °C. The probe was attached to the index finger of the non-dominant hand, ensuring good peripheral perfusion and avoiding nail polish or artificial nails that could interfere with the readings. Measurements were obtained after the patient had rested for at least 5 minutes, and three consecutive readings were obtained within a 1-minute interval; The mean value was recorded. SPO2 levels were assessed on postoperative day 1 and day 3 in both groups.
The 6-minute walk distance: 6-minute-walk distance test was conducted on postoperative day 3 and day 7 to assess exercise endurance. The test was performed indoors in an unobstructed flat corridor with an effective turnaround length of > 30 m, marking the start and end points 30 m apart. Patients walked as fast as possible between these points, rested briefly if fatigued, reminded every minute, stopped at 6 minutes, and the distance walked was recorded[7].
Borg scale: The degree of dyspnea after exercise on postoperative day 3 and day 7 was assessed using the Borg scale, and were scored from 0 to 10, with higher scores indicating greater respiratory difficulty[6].
Postoperative complications: The occurrence of postoperative complications such as atelectasis, pleural effusion, and abdominal infection was observed and recorded.
Statistical analysis was performed using SPSS version 25.0 software. Count data are expressed as n (%), and intergroup comparisons were conducted using the χ2 test; normally distributed measurement data are expressed as mean ± SD, with intergroup comparisons analyzed using the t-test. Statistical significance was set at P < 0.05.
The postoperative first time out of bed, postoperative hospitalization time, and average hospitalization cost of the study group were significantly lower than those of the control group (P < 0.05), as shown in Figure 1A and Table 2.
| Group | Cases | Time to first postoperative mobilization (hours) | Postoperative hospital stays (days) | Average hospitalization cost (10000 yuan) |
| Study group | 60 | 23.19 ± 2.44 | 11.23 ± 1.09 | 3.71 ± 0.44 |
| Control group | 60 | 26.23 ± 2.18 | 13.31 ± 1.24 | 4.10 ± 0.58 |
| t | 7.197 | 19.062 | 7.857 | |
| P value | 0.000 | 0.001 | 0.000 |
There was no significant difference in SPO2 levels between the two groups of patients at postoperative day 1 (P > 0.05). However. the SPO2 levels of the study group at postoperative day 3 was significantly higher than that of the control group (P < 0.05; Figure 1B; Table 3).
| Group | Cases | Postoperative day 1 | Postoperative day 3 | t | P value |
| Study group | 60 | 90.45 ± 2.20 | 96.34 ± 2.15 | 55.211 | 0.001 |
| Control group | 60 | 90.80 ± 2.30 | 91.41 ± 2.72 | 41.476 | 0.000 |
| t | 0.665 | 9.987 | |||
| P value | 0.507 | 0.001 |
There was no significant difference in 6-minute walk distance levels between the two groups at postoperative day 3 (P > 0.05), and both study groups had significantly higher 6-minute walk distance levels than the control group at postoperative day 7 (P < 0.05), as shown in Figure 1C and Table 4.
| Group | Cases | Postoperative day 3 | Postoperative day 7 | t | P value |
| Study group | 60 | 198.32 ± 23.17 | 476.71 ± 34.18 | 52.221 | 0.001 |
| Control group | 60 | 201.08 ± 22.25 | 412.45 ± 36.27 | 38.478 | 0.000 |
| t | 0.665 | 9.987 | |||
| P value | 0.507 | 0.001 |
There was no significant difference in Borg score between the groups on postoperative day 2 (P > 0.05) and postoperative day 3 (P > 0.05). However, on postoperative day 7, the Borg scores in the study group were significantly lower than those in the control group (P < 0.05), as shown in Figure 1D and Table 5.
| Group | Cases | Postoperative day 3 | Postoperative day 7 | t | P value |
| Study group | 60 | 5.32 ± 1.14 | 3.24 ± 1.05 | 10.395 | 0.000 |
| Control group | 60 | 5.28 ± 1.21 | 4.17 ± 1.31 | 4.821 | 0.000 |
| t | 0.186 | 4.291 | |||
| P value | 0.853 | 0.001 |
The postoperative complication rate in the intervention group was 3.33%, which was significantly lower than that in the control group (13.33%; P < 0.05), as shown in Figure 1E and Table 6.
| Group | Number of cases | Atelectasis | Pleural effusion | Abdominal infection | Total occurrences |
| Study group | 60 | 0 (0) | 2 (3.33) | 0 (0) | 2 (3.33) |
| Control group | 60 | 4 (6.67) | 3 (5.0) | 1 (1.67) | 8 (13.33) |
| t | 3.927 | ||||
| χ2 | 0.04 |
Diverse surgical techniques are important for the treatment of liver cancer. Compared with ordinary abdominal surgeries, the complexity of surgeries is significantly increased. This leads to a higher risk of postoperative complications in patients[8]. Recent clinical studies have confirmed that systematic postoperative rehabilitation training plays an important role in promoting physical function in patients with lung cancer, especially in pulmonary function recovery[9]. However, there remains a lack of foundational research on systematic and scientific perioperative rehabilitation training for patients with liver cancer, with insufficient strong clinical evidence and authoritative conclusions, which limits the promotion of this therapy to some extent[10]. Older patients with liver cancer face multiple challenges during the perioperative period, with pulmonary complications being particularly prominent and a key factor hindering postoperative recovery. Conventional perioperative management has limitations in preventing postoperative complications and promoting pulmonary function recovery[11]. Evidence-based graded intervention strategies combined with progressive training programs provide an innovative approach for improving perioperative pulmonary rehabilitation in older patients with liver cancer, and have significant clinical research value.
This study developed stratified management measures based on clinical evidence from older patients with liver cancer, thereby attempting to understand the key points of pulmonary rehabilitation for patients at different levels and laying a solid foundation for personalized rehabilitation programs. Stratified management breaks the traditional universal model and achieves precise allocation of medical resources. Perioperative interventions are stratified according to preoperative assessment to improve the overall perioperative pulmonary rehabilitation efficiency[12,13]. During implementation, medical staff apply differentiated monitoring and intervention measures for different patient groups according to the stratification results. For example, high-risk patients undergo frequent pulmonary function and vital sign monitoring to promptly detect changes in their condition, whereas low-risk patients focus on routine monitoring and rehabilitation guidance to ensure precise and effective nursing care[14,15].
Although traditional rehabilitation methods can promote pulmonary function recovery to some extent, the precise regulation of training intensity and frequency is difficult, which may cause overtraining or insufficient training, adversely affecting postoperative recovery. This study implemented evidence-based stratified management and stepwise rehabilitation training during the perioperative period in older patients with liver cancer[16]. Stepwise rehabilitation training follows the principle of gradual progression and dynamically adjusts the program based on the patient’s recovery progress and tolerance, accommodating the specific needs of different rehabilitation stages. This model effectively avoids training injuries while stimulating the proprioceptive system, enhancing sensory perception, and improving muscle endurance[17,18]. It deeply activates the core small muscle groups, promoting their full participation in synergistic contraction, providing external support for damaged tissue repair, strengthening neuromuscular coupling and interaction, ensuring rehabilitation training effectiveness, and accelerating postoperative recovery[19]. Clinical studies have confirmed that stepwise rehabilitation training combined with music intervention can effectively improve negative psychological states and promote recovery of physical function[20,21].
This study showed that the study group receiving evidence-based stratified management and stepwise rehabilitation had a shorter postoperative first ambulation time and hospital stay and lower hospitalization costs than the control group receiving conventional management and rehabilitation training. This indicates that perioperative stratified management combined with stepwise rehabilitation training helps improve the physical and mental status of patients, promotes functional recovery, and significantly shortens the time to first postoperative ambulation and hospital stay, thereby reducing treatment costs and alleviating the financial burden of patients[22]. Furthermore, the study results showed that the SPO2 on postoperative day 3 in the study group was significantly improved and better than that in the control group, whereas no obvious difference was found on postoperative day 1, which is consistent with previous reports[19]. This finding suggests that evidence-based stratified management combined with stepwise training contributes to recovery of postoperative pulmonary function. Furthermore, measurements showed that the 6-minute walk distance in the study group on postoperative day 7 was higher than that in the control group, whereas the Borg scores were lower than those in the control group (P < 0.05). Additionally, the incidence of postoperative complications in the study group was lower than that in the control group. This demonstrates that stepwise rehabilitation helps improve pulmonary function, daily activity capacity, and exercise tolerance in older patients, and improves their psychological status[23]. The core principle of stepwise rehabilitation nursing is active patient participation with intensity-matched interventions applied according to the characteristics of each rehabilitation stage. This model motivates patients and their families to engage deeply in the rehabilitation process, effectively improving rehabilitation adherence, ensuring good rehabilitation outcomes, enhancing motor function, and reducing postoperative complications.
In summary, implementing a combined program of evidence-based stratified management and stepwise training during perioperative pulmonary rehabilitation in older patients with liver cancer can effectively promote pulmonary function recovery, reduce complication rates, and achieve ideal rehabilitation outcomes, which are of great significance in clinical practice.
| 1. | Guo C, Ding Y, Zhou X, Lv X. Multimodal pulmonary rehabilitation in the perioperative period for patients with hepatocellular carcinoma. Asian J Surg. 2022;45:2127-2128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Cavanaugh D, Holt SK, Dwyer E, Petersen E, Gore JL, Schade GR, Grivas P, Hsieh AC, Lee JK, Montgomery B, Schweizer MT, Yezefski T, Yu EY, Chen JJ, Liao JJ, Weg E, Zeng J, Jannat S, Berry DL, Master VA, Garcia JM, Reed MJ, Bentov I, Wright JL, Psutka SP. Prospective evaluation of comprehensive geriatric assessments in multidisciplinary bladder cancer care and implications for personalized vulnerability phenotyping. Urol Oncol. 2025;43:468.e7-468.e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Batalik L, Pepera G, Papathanasiou J, Rutkowski S, Líška D, Batalikova K, Hartman M, Felšőci M, Dosbaba F. Is the Training Intensity in Phase Two Cardiovascular Rehabilitation Different in Telehealth versus Outpatient Rehabilitation? J Clin Med. 2021;10:4069. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Zhang XL, Ma HY. Comprehensive influence of individualized nutrition support and nursing strategy on rehabilitation of patients with liver cancer after operation. World J Gastrointest Surg. 2025;17:101297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5593] [Cited by in RCA: 6391] [Article Influence: 798.9] [Reference Citation Analysis (9)] |
| 6. | Sökeland G, Brönnimann MP, Vassella E, Stirnimann G, Montani M, Friemel J. Clinically Uncertain Liver Masses: A Guide to Distinguishing Poorly Differentiated Primary Liver Cancer. Biomedicines. 2025;13:1063. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Perrone J, Rabilloud M, Mely L. Change in the 6-min walk test among 71 patients with cystic fibrosis treated with elexacaftor/tezacaftor/ivacaftor. Respir Med. 2025;244:108178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Sirakaya F, Calik Kutukcu E, Onur MR, Dikmen E, Kumbasar U, Uysal S, Dogan R. Re: The Effects of Various Approaches to Lobectomies on Respiratory Muscle Strength, Diaphragm Thickness, and Exercise Capacity in Lung Cancer Re: Enhancing Respiration Function Evaluation and Recovery in Lung Cancer: The Interdisciplinary Approach to Postoperative Management. Ann Surg Oncol. 2025;32:2712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | 9 Alzahrani M, Mehta R, Kadiri S, Algaeed S, Osman A, Alsanad M, Duda J, Gao F, Naidu B. Effect of pulmonary rehabilitation on lung cancer surgery outcomes: a matched-case analysis. Perioper Med (Lond). 2025;14: 35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Kuai J, Liu Y, Ding W, Wang Y. Study on the application of perioperative nutrition management in accelerated rehabilitation surgery in patients with laparoscopic primary liver cancer resection. Minerva Surg. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Milot MH, Léonard G, Corriveau H, Desrosiers J. Using the Borg rating of perceived exertion scale to grade the intensity of a functional training program of the affected upper limb after a stroke: a feasibility study. Clin Interv Aging. 2019;14:9-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Zhao S, Zhu Y, Zhu J, Wang B, Wang E, Zhu J, Wen L, Zhao Y, Yang M, Zuo L, Fan J, Jia J, Wu W, Ren W, Chen X, Li J, Qi X, Du X, Liu L. Liver resection versus interventional treatments for hepatocellular carcinoma patients with hypohepatia: a multicenter study. Surg Endosc. 2025;39:4205-4216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Kawish M, Siddiqui NN, Jahan H, Elhissi A, Zahid H, Khatoon B, Raza Shah M. Targeted pH-responsive delivery of rosmarinic acid via phenylboronic acid functionalized mesoporous silica nanoparticles for liver and lung cancer therapy. Pharm Dev Technol. 2024;29:541-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 14. | Orange ST, Hallsworth K, Brown MC, Reeves HL. The feasibility and acceptability of a home-based, virtual exercise intervention for older patients with hepatocellular carcinoma: protocol for a non-randomised feasibility study (TELEX-Liver Cancer). Pilot Feasibility Stud. 2022;8:113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Li F, Zheng T, Gu X. Prognostic risk factor analysis and nomogram construction for primary liver cancer in elderly patients based on SEER database. BMJ Open. 2022;12:e051946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 16. | Shi L, Wang R, Zhao J, Zhang J, Kuang Z. Detection of Rehabilitation Training Effect of Upper Limb Movement Disorder Based on MPL-CNN. Sensors (Basel). 2024;24:1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Amiss E, Cottrell M. Evaluation of a Novel Step Training Mobile App Intervention in Cardiopulmonary Rehabilitation: A Single-Arm Prospective Cohort Study. Games Health J. 2022;11:330-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Dossett LA, Mott NM, Bredbeck BC, Wang T, Jobin CT, Hughes TM, Hawley ST, Zikmund-Fisher BJ. Using Tailored Messages to Target Overuse of Low-Value Breast Cancer Care in Older Women. J Surg Res. 2022;270:503-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Montroni I, Saur NM. Modern, multidisciplinary colorectal cancer care in older patients: Striking a balance between cancer treatment and patient-centered care. Eur J Surg Oncol. 2020;46:299-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Li T, Li B, Tan L, Lv B. Reminiscence Therapy as a Potential Method to Improve Psychological Health and Quality of Life in Elderly Hepatocellular Carcinoma Patients: A Randomized, Controlled Trial. Front Surg. 2022;9:873843. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 21. | Zhu J, Carr F, Sun M, Tian P, McLeod M, De Coutere S. A Pilot Study to Evaluate a New Hep-GRP Care Pathway to Improve Outcomes Among Canadian Older Adults with Liver Cirrhosis. Can Geriatr J. 2024;27:1-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 22. | Ma Y, Yuan Y, Lu Y, Li S. A pilot clinical trial of exercise program for elderly patients with cirrhosis and frailty: comprehensive exercise rehabilitation intervention. Eur J Gastroenterol Hepatol. 2025;37:313-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Wang B, Huang X, Liu G, Zheng T, Lin H, Qiao Y, Sun W. The sensitivity outcome index system for home care of elderly liver transplant patients was developed based on the Omaha problem classification system. BMC Med Inform Decis Mak. 2024;24:207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |