Published online Aug 27, 2022. doi: 10.4240/wjgs.v14.i8.849
Peer-review started: January 26, 2022
First decision: March 12, 2022
Revised: March 26, 2022
Accepted: July 22, 2022
Article in press: July 22, 2022
Published online: August 27, 2022
Processing time: 209 Days and 23.1 Hours
Small bowel diverticulosis is an uncommon condition which is usually asym
A 68-year-old male presented with symptoms of small bowel obstruction. Computed tomography (CT) of the abdomen demonstrated small bowel ob
The pathophysiology underlying enterolith formation is unclear, so it is difficult to predict if or when enteroliths may form and cause bowel obstruction. More research could provide advice to prevent recurrent enterolith formation and its sequelae.
Core Tip: Enterolith formation in small bowel diverticula followed by impaction is a rare cause of small bowel obstruction. Small bowel diverticulosis in itself is a rather rare entity. As such, the management of this acute surgical problem can vary widely depending on the situation. Only a few case reports of this pathology have been described, and the management of this condition was variable. Of note, the management of a recurrent episode in the same patient is not previously described. This case report adds to the current knowledge base of the management of this rare pathology.
- Citation: Lee C, Menezes G. Recurrent small bowel obstruction secondary to jejunal diverticular enterolith: A case report. World J Gastrointest Surg 2022; 14(8): 849-854
- URL: https://www.wjgnet.com/1948-9366/full/v14/i8/849.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i8.849
Small bowel diverticulosis is an uncommon condition whose prevalence increases with age[1]. It is thought to arise due to high intraluminal pressure in the bowel that leads to sac-like protrusions of the mucosa and/or submucosa through mural weak points[2]. This condition is usually asymptomatic and is discovered incidentally. It can, however, be complicated by conditions such as diverticulitis, hae
Enteroliths are categorised as primary or secondary enteroliths. Primary enteroliths are those that form within the bowel, be it via precipitation of bowel content or clumping of ingested materials. Secondary enteroliths are stones that form in other viscera, such as gallstones. Primary enteroliths are thought to form due to stasis of intestinal content in the bowel. Such stasis can occur in diverticula, but can also be seen in other conditions such as intestinal strictures and anastomoses with blind pouches.
A few cases of small bowel obstruction from enterolith formation in jejunal diverticula have been described in literature[5-8], but recurrent small bowel obstruction from this aetiology has not been described previously. Here, we report a case of a 68-year-old male who presented with recurrent small bowel obstruction secondary to impaction of an enterolith formed in jejunal diverticula.
A 68-year-old Caucasian male was brought by ambulance to a regional emergency department with a three-day history of epigastric pain, vomiting, and reduced oral intake. He also reported a two-day history of obstipation.
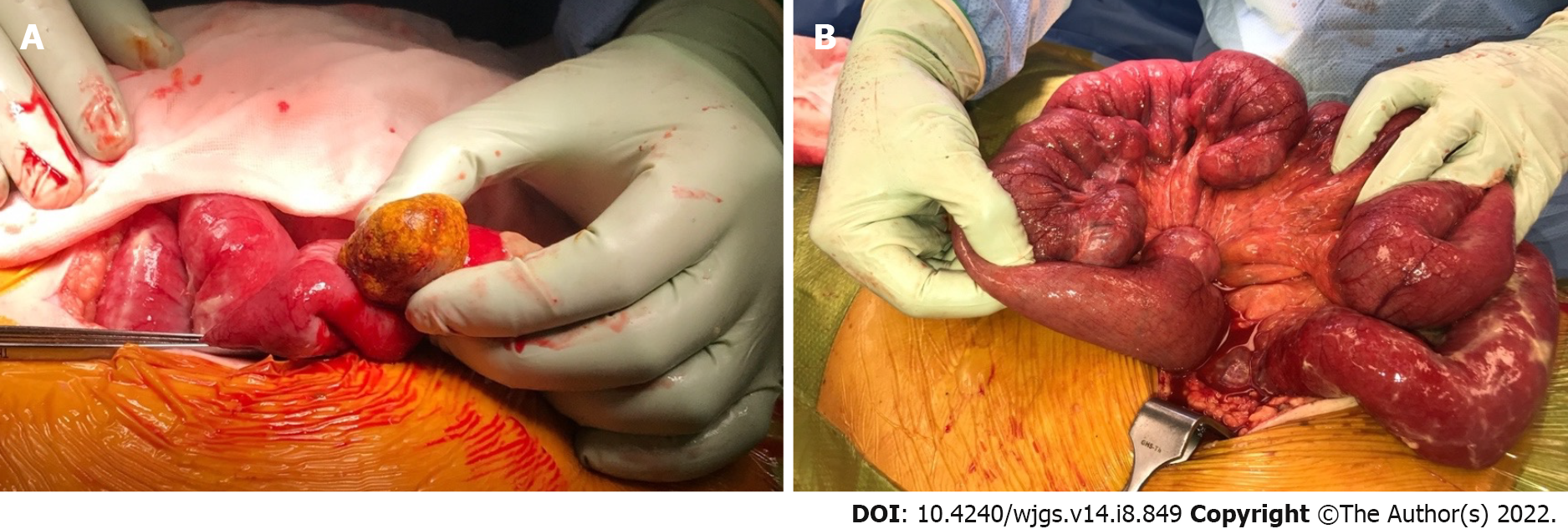
This patient reported that his symptoms were strikingly similar to an episode seven months ago, when he underwent a laparotomy and small bowel resection for small bowel obstruction caused by an enterolith. At that time, enterolith impaction caused small bowel obstruction and ileal perforation, leading to purulent peritonitis. Extensive jejunal diverticulosis was also noted. A longitudinal enterotomy was made proximal to the impacted enterolith, the large enterolith was milked out, and the enterotomy was closed transversely (Figure 1A). The perforated ileal segment was resected separately and anastomosed side-to-side with a cutting linear stapler. The jejunal diverticula were not resectable, given the extensive jejunal involvement (Figure 1B). The final pathology of the enterolith revealed degenerate adipose and vegetable matter intermingled with bacteria, crystalline material, and red blood cells. This was suggestive of a primary enterolith with calcifications.
The patient’s past history included open cholecystectomy, open appendicectomy, type 2 diabetes, hypertension, hypercholesterolaemia, and knee osteoarthritis. His medications were: Rosuvastatin 10 mg nocte, sitagliptin/metformin 50 mg/850 mg twice daily, telmisartan 80 mg mane, and meloxicam 15 mg nocte, with good adherence to his regimen. He did not have any known adverse drug reactions.
The patient is a non-smoker and does not drink alcohol. He was not aware of any relevant family history.
On examination, the patient’s temperature was 36 ˚C, heart rate was 88 bpm, blood pressure was 120/60 mmHg, respiratory rate was 20 breaths per minute, and oxygen saturation was 100% in room air. The abdomen was soft without peritonitis, but distended and moderately tender generally.
Blood analysis showed a normal white cell count of 7.1 × 109/L, a mild rise in serum C-reactive protein level at 50 mg/L, a serum lactate level of 1.2 mmol/L, and pH of 7.39. He had an acute kidney injury with a serum creatinine level of 195 μmol/L.
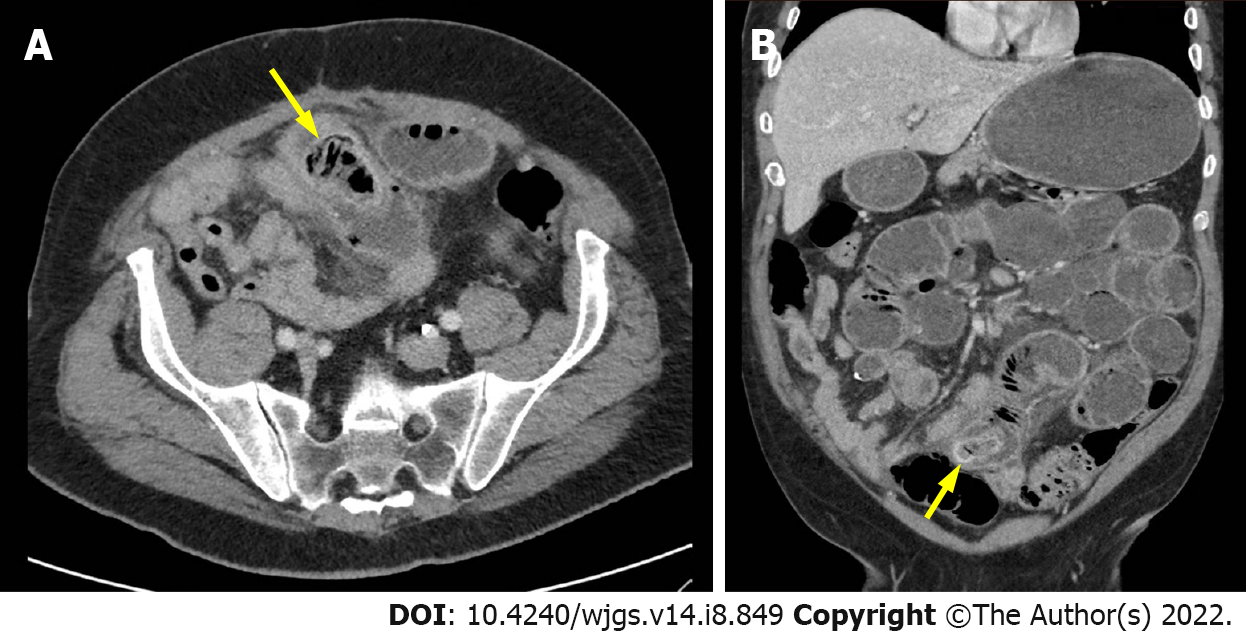
A computed tomography (CT) scan of the abdomen and pelvis suggested small bowel obstruction with a transition point at the previous small bowel anastomosis site. The scan was reviewed again with the radiologist, who was provided with the pertinent recent surgical history from seven months ago. It was at this point that the offending enterolith was evident on the CT scan (Figure 2). The findings were explained to the patient, and he was booked and consented for an exploratory laparotomy.
The final diagnosis of this case is recurrent small bowel obstruction secondary to impacted enterolith related to extensive jejunal diverticulosis.
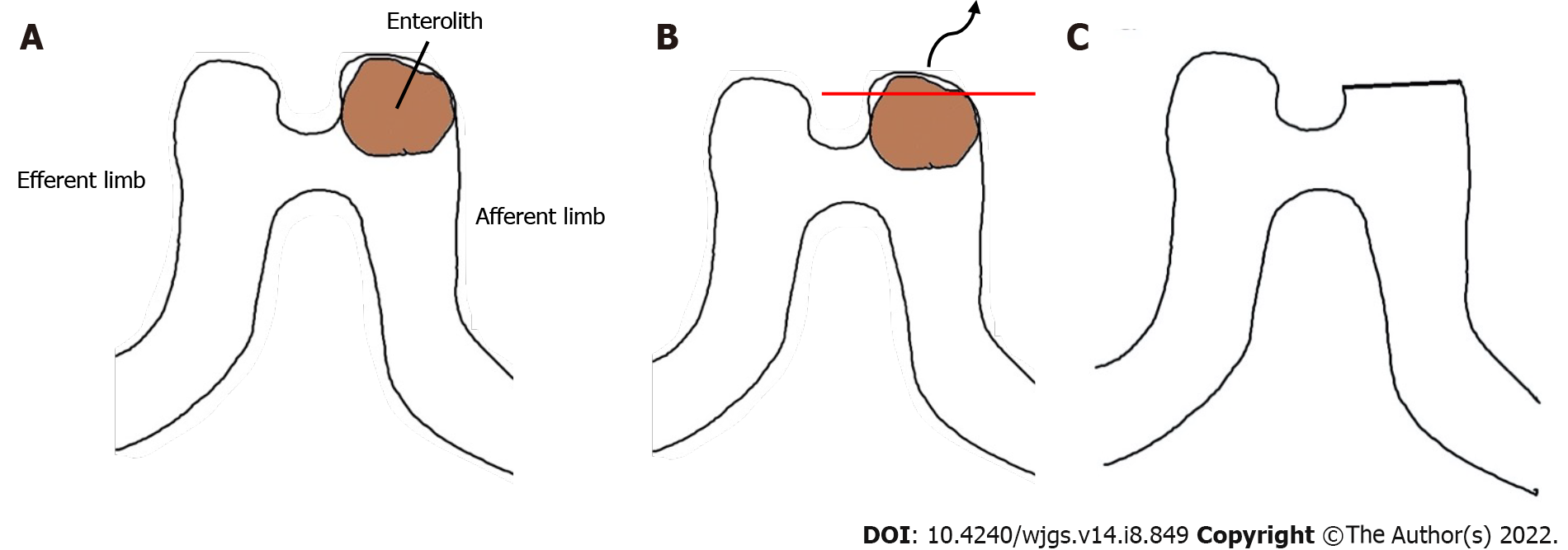
Intraoperatively, extensive adhesions from the previous operation were divided. A bowel run revealed a large obstructive enterolith impacted at the afferent limb of the previous anastomosis (Figure 3A). All examined bowel was viable and extensive jejunal diverticulosis was once again noted. An enterotomy was made at the blind end of the afferent limb, and the enterolith was milked out (Figure 3B). The enterotomy was closed with a cutting linear stapler (Figure 3C). The patient recovered well and was discharged on postoperative day 5.
In the two years following his second laparotomy, there was no recurrence of enterolith-related bowel obstruction. Serum calcium and uric acid levels were measured and found to be within normal limits. The pathological analysis of the enterolith revealed degenerate food particles and vegetable matter, again indicative of a primary enterolith.
About one year following the second laparotomy, this patient was admitted for an episode of small bowel obstruction secondary to postoperative adhesions. This was non-operatively managed with success. Furthermore, he developed incisional hernias related to the laparotomy wound for which he has been wait-listed for elective repair. This patient had a follow up colonoscopy six months following his first laparotomy at which sigmoid diverticulosis was noted. Subjectively, the patient was satisfied with the treatment he received. There were no adverse or unanticipated events in the perioperative periods.
Bowel diverticula are abnormal sac-like mural outpouchings which can involve the small or large bowel. Small bowel diverticulosis is most common in the duodenum at 79% followed by the jejunum or ileum at 18%[9]. Overall, jejunoileal diverticulosis is quite rare, evident in 0.5% to 2.3% of individuals in radiographic studies. It is most commonly reported in 60 to 70-year-old males[7]. The exact pathophysiology is unclear, but intestinal dysmotility, high intraluminal pressures, and weak points in the alimentary tract are thought to be strong contributors to this condition. About 10% of individuals with jejunoileal diverticulosis may develop complications such as bowel obstruction, haemorrhage, and diverticulitis[9-11].
Enterolith impaction causing bowel obstruction should be on the list of differential diagnoses in individuals known to have small bowel diverticulosis. Such cases have been managed operatively with enterotomy and stone removal as in this case. Another method described was to crush the enterolith in the small bowel and milking distally into the colon[12]. Quek and Tanase[13] also recently described a case which was managed non-operatively for the first time with success.
Recurrent enterolith formation is possible in individuals with small bowel diverticulosis. Three episodes of recurrent bowel obstruction from primary enterolith in a three-year time period was described only once previously by Shrestha and Shrestha[14], but there were no small bowel diverticula noted in that patient. It is not possible to resect all affected segments in individuals with extensive diverticular involvement due to the result of unacceptably short small bowel length. Current evidence to prevent recurrent formation of enteroliths in these patients is lacking. Surgically, anatomical alterations that avoid stasis of intestinal content probably should be implemented. More research is required to explore the mechanism by which enteroliths form. Evidence-based dietary advice for these patients with extensive small bowel diverticulosis could decrease the risk of recurrent enterolith formation and its sequelae.
This case report sheds new light on the pathophysiology of bowel obstruction caused by primary enterolith formation in small bowel diverticula. This is the first case in literature of a recurrent small bowel obstruction caused by a primary enterolith associated with jejunal diverticulosis. In particular, this case highlighted the time frame between episodes of enterolith related bowel obstruction: seven months. The current knowledge base of the pathophysiology of enterolith formation supports the practice of avoiding anatomical alterations that promote stasis of intestinal content. More research on dietary modifications may prove to be beneficial for individuals with unresectable extensive small bowel diverticulosis.
| 1. | Noer T. Non-Meckelian diverticula of the small bowel. The incidence in an autopsy material. Acta Chir Scand. 1960;120:175-179. [PubMed] |
| 2. | Gurvits GE, Lan G. Enterolithiasis. World J Gastroenterol. 2014;20:17819-17829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 66] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 3. | Longo WE, Vernava AM 3rd. Clinical implications of jejunoileal diverticular disease. Dis Colon Rectum. 1992;35:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 94] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 4. | Sibille A, Willocx R. Jejunal diverticulitis. Am J Gastroenterol. 1992;87:655-658. [PubMed] |
| 5. | Ishizuka D, Shirai Y, Hatakeyama K. Duodenal obstruction caused by gallstone impaction into an intraluminal duodenal diverticulum. Am J Gastroenterol. 1997;92:182-183. [PubMed] |
| 6. | Eckhauser FE, Zelenock GB, Freier DT. Acute complications of jejuno-ileal pseudodiverticulosis: surgical implications and management. Am J Surg. 1979;138:320-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 7. | Harris LM, Volpe CM, Doerr RJ. Small bowel obstruction secondary to enterolith impaction complicating jejunal diverticulitis. Am J Gastroenterol. 1997;92:1538-1540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Yang HK, Fondacaro PF. Enterolith ileus: a rare complication of duodenal diverticula. Am J Gastroenterol. 1992;87:1846-1848. [PubMed] |
| 9. | Singh MP, Huda T, Singh KV. A Primary Jejunal Enterolith Presenting as Small Bowel Obstruction. Indian J Surg. 2018;80:292-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Afify SJ, George J, Kelty CJ, Shah N. Largest sized enterolith ileus due to a duodenal diverticulum in a virgin abdomen causing small bowel obstruction. BMJ Case Rep. 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Jadib A, Tabakh H, Chahidi El Ouazzani L, Boumlik K, Boutachali R, Siwane A, Touil N, Kacimi O, Chikhaoui N. Primary true enterolithiasis: A rare cause of acute small bowel obstruction. Radiol Case Rep. 2022;17:610-614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM. Small-bowel diverticulosis: perceptions and reality. J Am Coll Surg. 1997;184:383-388. [PubMed] |
| 13. | Quek FF, Tanase A. P53 First Reported Case of Successful Non-Surgical Management for Acute Small Intestinal Obstruction Caused by Enterolith as A Rare Complication of Jejunal Diverticulosis. BJS Open 2021; 5: zrab032. 52;0. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Shrestha AL, Shrestha P. Recurrent Enterolithiasis Small Bowel Obstruction: A Case Seldom Described. Case Rep Gastrointest Med. 2017;2017:4684182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Australia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Awad AK, Egypt; Hu B, China S-Editor: Yan JP L-Editor: A P-Editor: Yan JP