©The Author(s) 2025.
World J Gastrointest Surg. Dec 27, 2025; 17(12): 112887
Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.112887
Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.112887
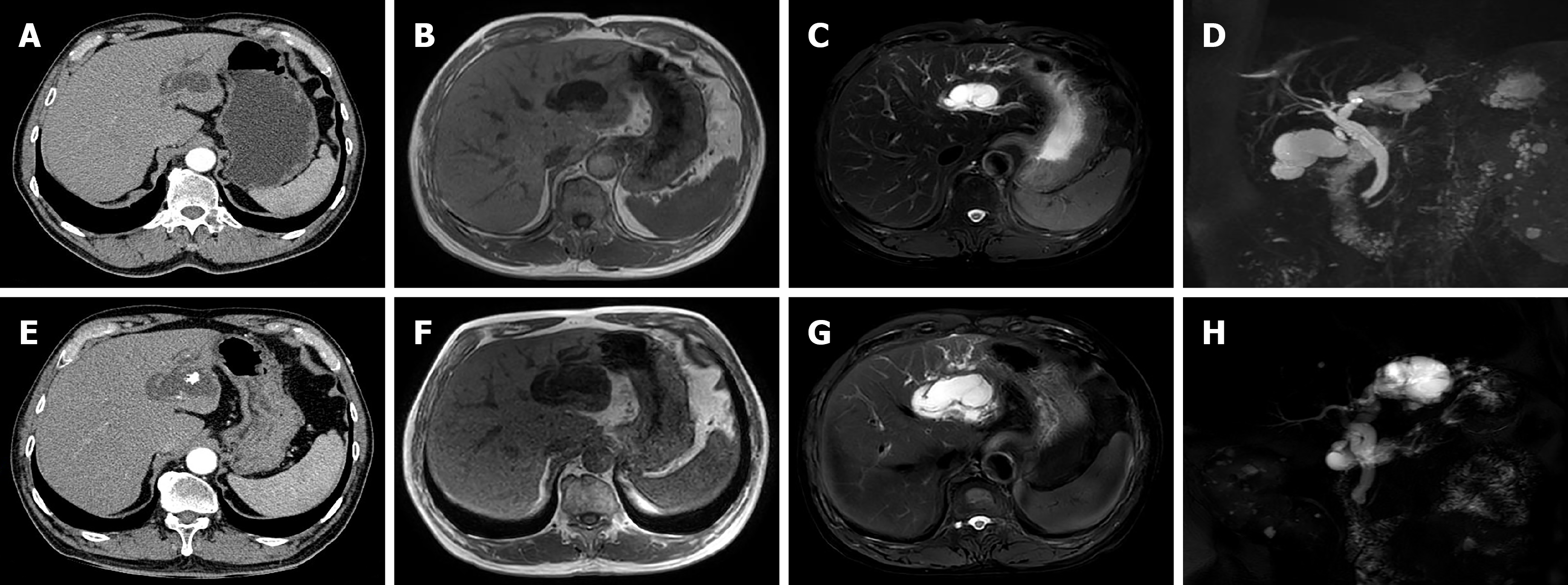
Figure 1 Imaging findings.
A and E: Arterial-phase computed tomography: A 41-mm left intrahepatic bile duct cystic tumour without enhancement 4 years ago (A) and a 63-mm left intrahepatic bile duct cystic tumour and papillary proliferation with slight hyperenhancement at this visit (E); B and F: Magnetic resonance imaging (MRI) on the T1-weighted image: A cystic tumour with low intensity 4 years ago (B) and the growing cystic tumour with low intensity at this visit (F); C and G: MRI on the T2-weighted image: A cystic tumour with high intensity 4 years ago (C) and the growing cystic tumour with high intensity at this visit (G); D and H: Magnetic resonance cholangiopancreatography: A cystic tumour and dilatation of the left hepatic duct and common bile duct 4 years ago (D) and the growing cystic tumour and more severe dilatation of the left hepatic duct and common bile duct at this visit (H).
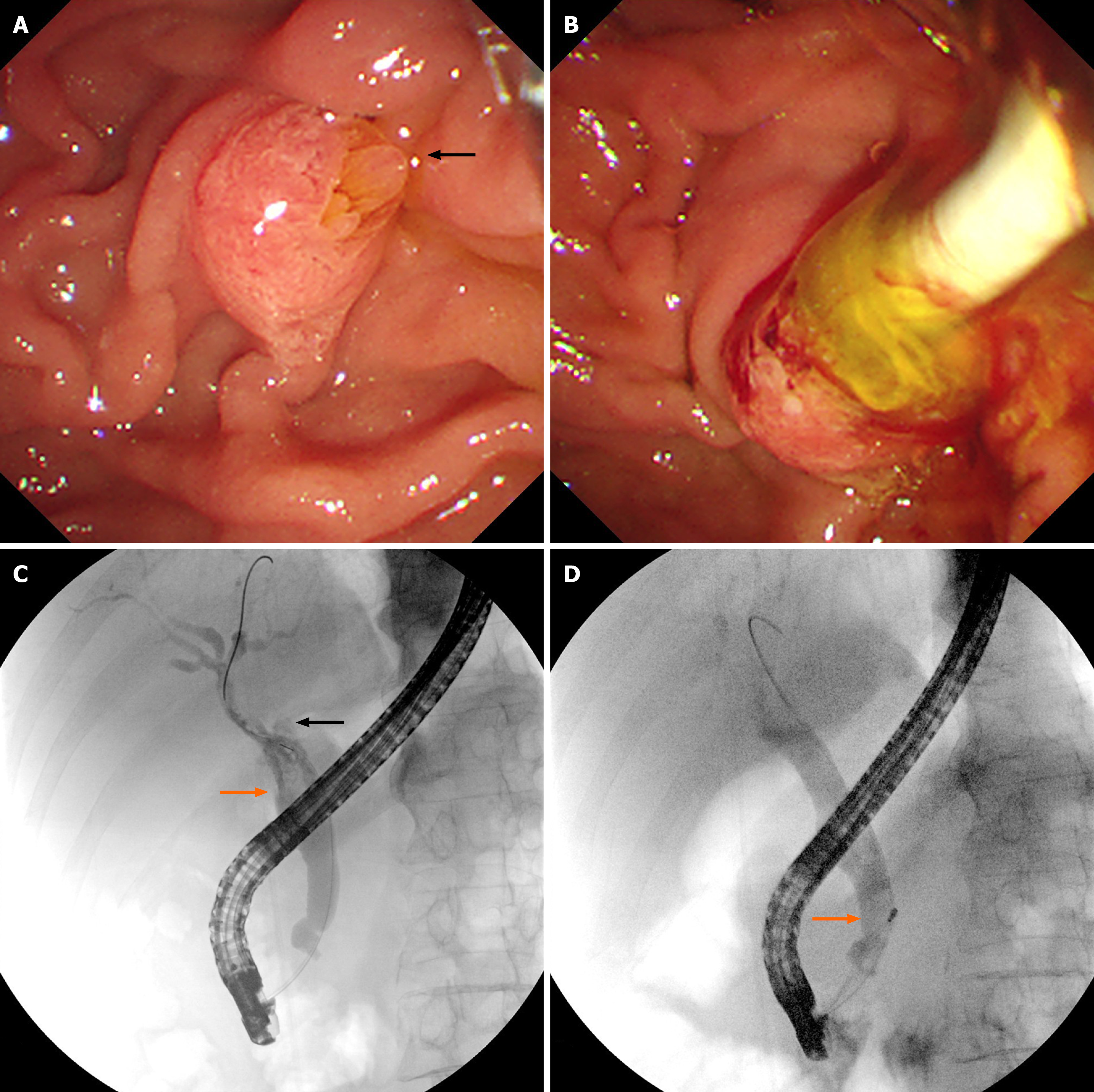
Figure 2 Endoscopic retrograde cholangiopancreatography findings.
A: Duodenoscopy revealed an enlarged duodenal papilla, a dilated papillary orifice with a fish-mouth-like appearance and translucent jelly mucus (black arrow); B: Duodenoscopy revealed a large amount of translucent jelly-like mucus containing bile flowing out during bile duct clearance; C: Endoscopic retrograde cholangiography showed multiple cloudy, irregular filling defects in the dilated extrahepatic bile duct (orange arrow), non-visualized dilated left hepatic duct and an intrahepatic cystic lesion caused by mucin obstruction (black arrow); D: Endoscopic retrograde cholangiography showed the morphology and location of the filling defect in the bile duct were altered during clearing of the bile duct (orange arrow).
Figure 3 The surgical specimen measured 50 mm in maximum diameter, with macroscopically visible mucin secretion, stones (black arrow) and papillary tumour tissue (white arrow).
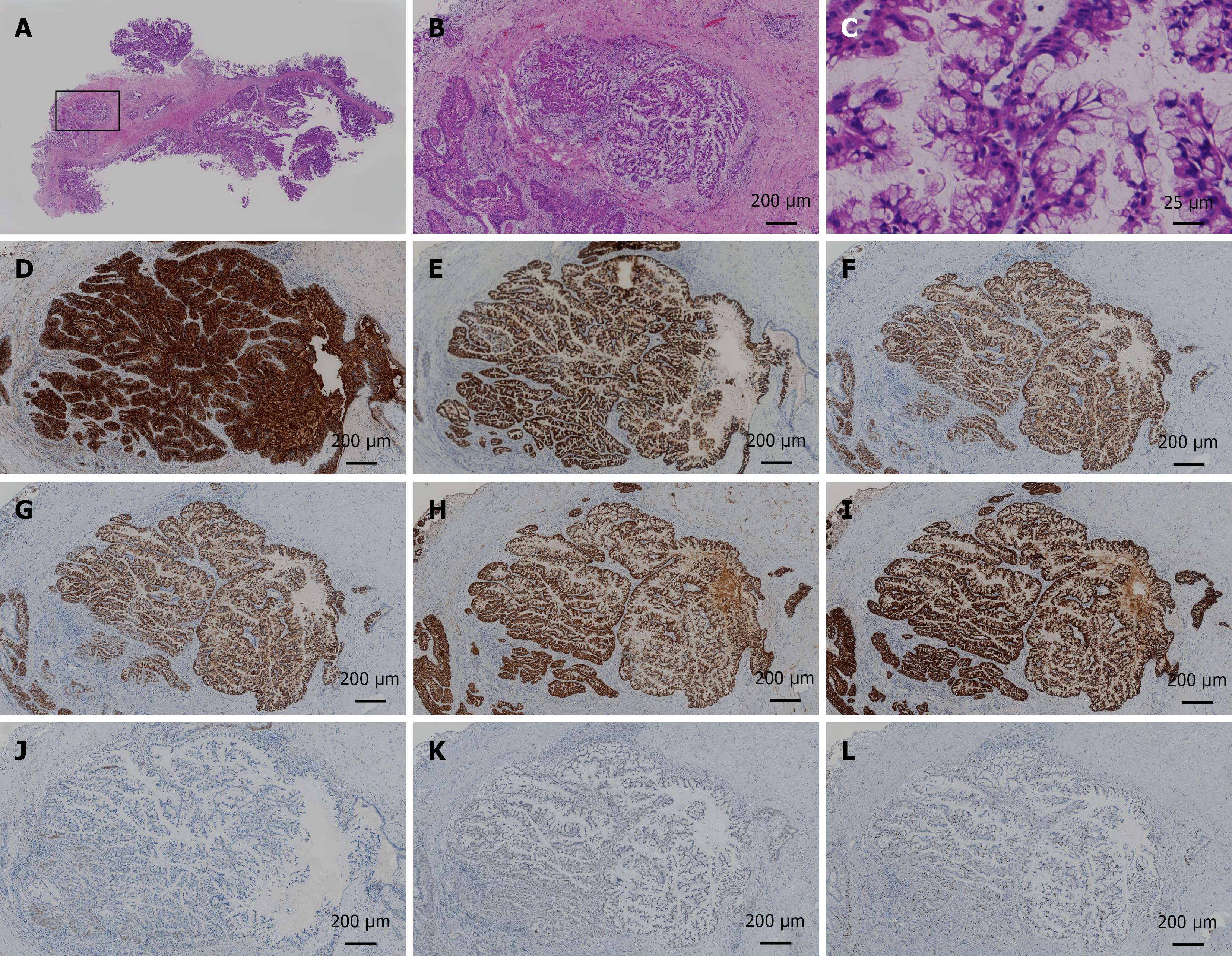
Figure 4 Histopathologic features of the surgical specimen.
A-C: Haematoxylin and eosin staining of the papillary tumour: Macrography (A); × 40 (B); × 400 (C); D-K: Immunohistochemical findings of the papillary tumour: MUC1 positivity (× 40; D); MUC2 positivity (× 40; E); MUC5AC positivity (× 40; F); MUC6 positivity (× 40; G); CK7 positivity (× 40; H); CK19 positivity (× 40; I); CK20 negativity (× 40; J); P53 wild-type (× 40; K); L: Ki-67 expression in approximately 20% of the cells, indicating moderate proliferative activity (× 40).
- Citation: Gu TY, Wang SH, Yang SY, Zhao SQ, Chen MJ, Li XP, Song ZW, Gu XX, Chen F. Intraductal papillary neoplasm of the biliary tract with typical clinicopathological, endoscopic features: A case report. World J Gastrointest Surg 2025; 17(12): 112887
- URL: https://www.wjgnet.com/1948-9366/full/v17/i12/112887.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i12.112887