Published online Mar 15, 2025. doi: 10.4239/wjd.v16.i3.102526
Revised: December 30, 2024
Accepted: January 8, 2025
Published online: March 15, 2025
Processing time: 92 Days and 18 Hours
Premixed insulin combines two types of insulin in a single injection. This com
Core Tip: Premixed insulin improved patient adherence because of its simplified treatment regimens, fewer injections, and low price. Therefore, premixed insulin is widely used, especially in developed countries. However, patients receiving premixed insulin commonly have less satisfactory blood glucose control. The fixed ratio of premixed insulin usually fails to meet the nuanced demands of individualized glucose-lowering therapy. Moreover, aberrant local absorption and potential systemic autoimmune responses of premixed insulin may further affect glycemic control. New insulin formulations offer improved blood glucose control, weight management, and reduced hypoglycemia. Further studies are needed to guide the optimization of insulin use through individualized treatment approaches or to mitigate the side effects of premixed insulin through novel drug combinations.
- Citation: Xia Y, Hu Y, Ma JH. Premixed insulin: Advantages, disadvantages, and future. World J Diabetes 2025; 16(3): 102526
- URL: https://www.wjgnet.com/1948-9358/full/v16/i3/102526.htm
- DOI: https://dx.doi.org/10.4239/wjd.v16.i3.102526
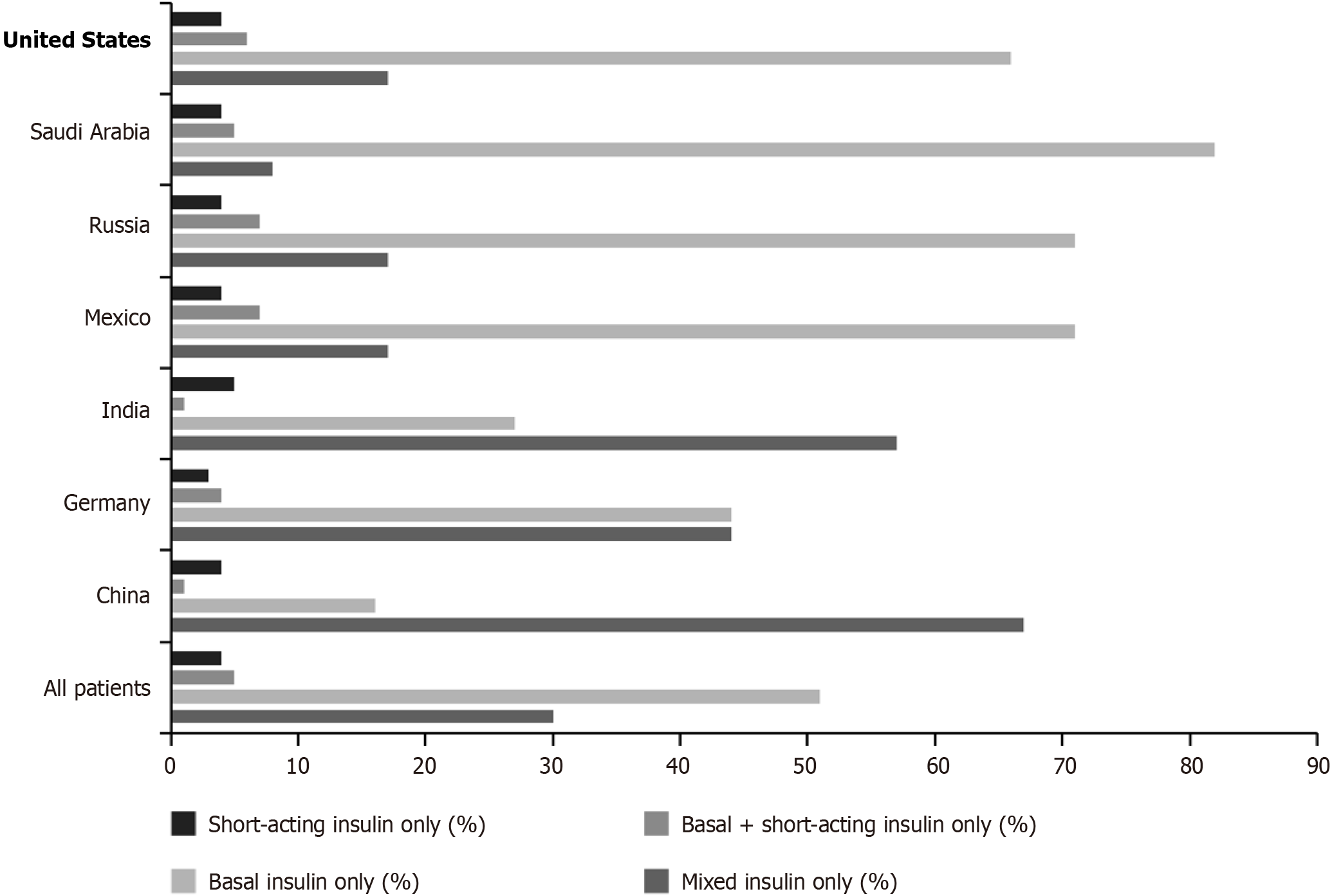
Treatment of diabetes aims to manage the blood glucose levels, prevent complications and improve the quality of life. Lifestyle interventions and oral medications are mainly used in the early stages of type 2 diabetes, and insulin therapy is often required after the progression of the disease. Current insulin therapies include basal insulin to control the fasting blood glucose levels, mealtime insulin to manage the postprandial blood glucose levels, and a simplified regimen of premixed insulin. In China, 67% of patients with type 2 diabetes treated with insulin use premixed insulin, ranking first globally (Figure 1)[1]. Premixed insulin is an insulin formulation that combines short or rapid insulin with intermediate or long-acting insulin in a fixed ratio, aimed at simplifying treatment regimens for diabetes[2]. Common types of pre
An important advantage of premixed insulin is that it simplifies the insulin treatment regimen[6]. By combining two types of insulin with different durations of action into a single injected dose, patients need to be injected only once to achieve short and intermediate-acting insulin effects[7]. This reduces the number of daily injections, typically requiring only two injections per day (morning and evening), making it more convenient and improving patient adherence com
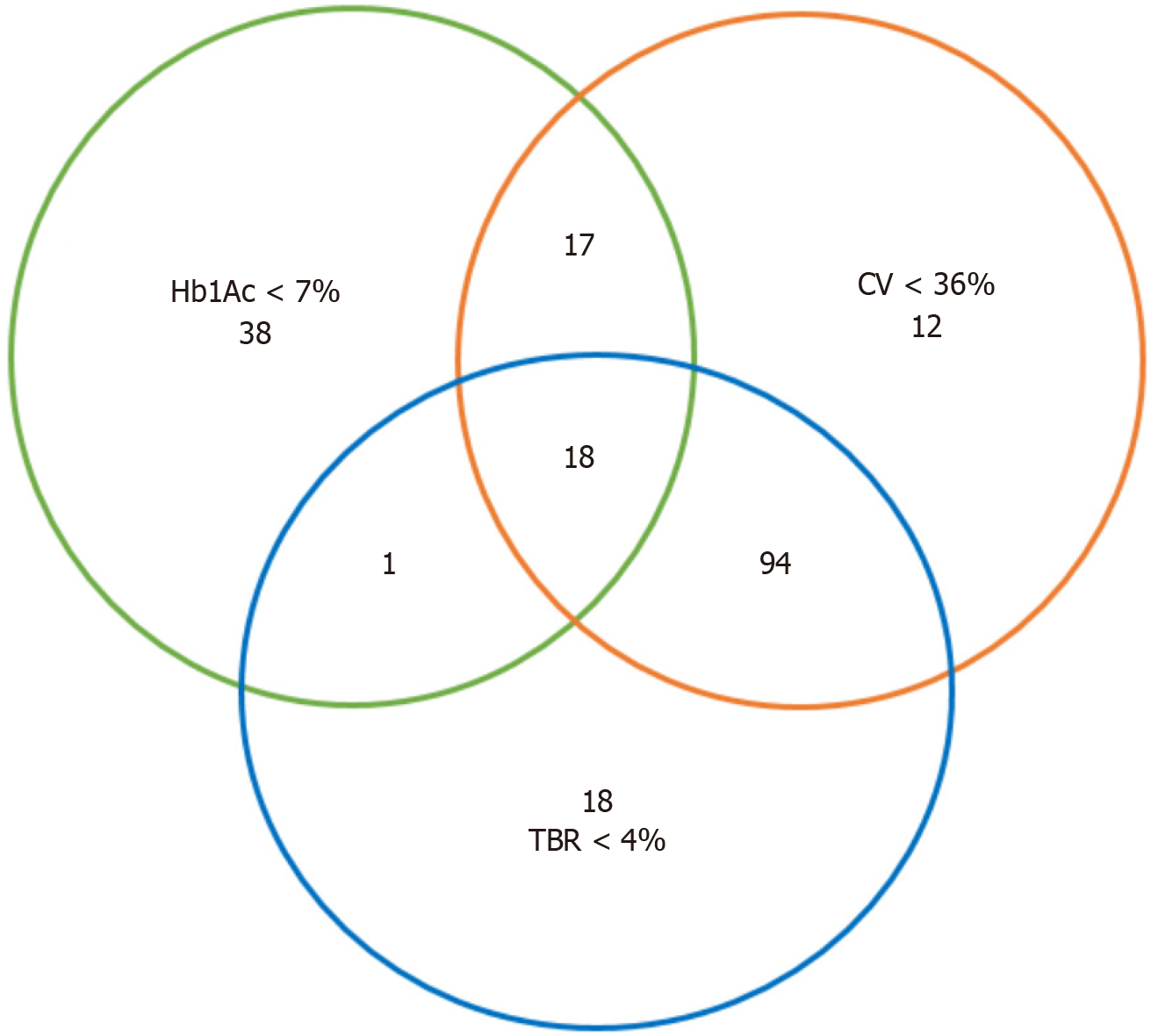
Premixed insulin is a fixed-ratio combination insulin formulation[11]. This means that patients cannot adjust the ratio of short and intermediate-acting insulin based on fluctuation in their blood glucose or due to their lifestyle[12]. A cross-sectional study collected the data of glycaemic control using the FreeStyle Libre Pro™ system from 172 patients using premix insulin, and it showed that only 8.1% of patients achieved the composite goal of glycaemic control including glycosylated haemoglobin (HbA1c) < 7%, glycaemic variability < 36%, and time below range < 4%[13], which indicated the poor blood glucose control in patients being administered premixed insulin therapy (Figure 2). When physical activity and insulin sensitivity increase, it may be necessary to adjust insulin doses to avoid hypoglycaemia; however, the fixed ratio and duration of action of premixed insulin limit the space for such adjustments[12]. The effect of intermediate-acting insulin lasts throughout the night, potentially increasing the risk of nighttime hypoglycaemia, particularly if the dose is not adjusted after the evening meal[14]. Therefore, individualized treatment taking into account these factors is necessary and deserves further study. Short-acting insulin causes fewer persistent hypoglycaemic events due to its rapid clearance, particularly under reasonable dose adjustment and postprandial monitoring[15]. A prospective, randomized, open-label clinical trial in 200 insulin-naive patients with type 2 diabetes showed that in patients with type 2 diabetes, the glargine combined with quick-acting insulin group had better HbA1c, fasting and postprandial blood glucose, and lower incidence of hypoglycemia than that in the premixed insulin group[16]. These findings were also observed in patients with type 1 diabetes and further supported by meta-analysis[17,18]. Therefore, premixed insulin is less recommended than long-acting insulin analogues plus rapid-acting insulin analogues in type 1 diabetes[19]. However, the choice of insulin type is not specified in patients with type 2 diabetes yet[20].
Insulin autoimmune syndrome (IAS) is a rare hypoglycaemic condition characterized by a high serum insulin level and the presence of insulin antibodies. Similar symptoms have been observed in patients with diabetes using exogenous insulin, leading to the term exogenous IAS (EIAS)[21]. Studies have reported that most patients with EIAS use premixed insulin, specifically Novolin 30R, Humulin 70/30, and other similar formulations[22]. Hypoglycaemia in these patients often occurs at night or in the early morning, with many having a serum insulin level > 100 U/mL and a low C-peptide level during hypoglycaemic episodes. When insulin associated with EIAS is discontinued, hypoglycaemic symptoms typically disappear within a few months[22]. Testing for insulin antibodies is the key to diagnosing IAS[23]. Adjusting treatment plans, such as changing the type of insulin or switching to oral medications, can effectively reduce the in
Premixed insulin can cause local lipohypertrophy (fat accumulation), which significantly affects insulin absorption[27]. Lipohypertrophy is often associated with frequent insulin injections to the same site. Insulin can promote fat synthesis by stimulating fat cells to convert and store glucose[28]. The primary characteristic of lipohypertrophy is the thickening of subcutaneous fat tissue at the injection site, which forms fibrotic and poorly vascularized tissue. Studies have shown that insulin absorption in lipohypertrophic tissue is 25%-30% lower than that in normal tissue, which in
In recent years, new insulin or insulin/glucagon-like peptide 1-receptor agonists combinations, such as insulin degludec/insulin aspart (IDegAsp), insulin degludec/liraglutide, and insulin glargine/lixisenatide (IGlarLixi) have emerged, further optimizing the management of diabetes. Compared to traditional premixed insulin, these new formulations offer significant advantages and address the shortcomings of conventional premixed insulin, particularly in terms of immunogenicity, blood glucose control, weight management, and risk of hypoglycaemia[36].
A retrospective analysis showed that in patients with type 2 diabetes, switching from premixed insulin to IDegAsp can decrease HbA1c, fasting and postprandial blood glucose, total daily insulin dose, and injection frequency[37]. A ran
New medications usually come with a higher price tag. From 2011 to 2020, the expenditures of antidiabetic agents increased from 27.15 to 89.17 billion in the United States and insulin had the highest expenditure among antidiabetic agents[39]. The high cost of these new insulins may limit their widespread use. To promote the use of these new drugs, government and health agency may adjust their policies, such as drug price negotiations and financial subsidies, so that these innovative drugs can be provided to more patients with diabetes[40]. Updating clinical treatment guidelines and appropriately training medical staff should also be considered.
In the future, more and more “smart” insulin and insulin delivery devices may improve efficacy and convenience of insulin therapy. Recently, a new insulin “NNC2215” with the glucose-sensitive bioactivity has been introduced[41]. However, further studies are still needed to guide the optimization of premixed insulin use through individualized treatment approaches, or to mitigate the side effects of premixed insulin through novel drug combinations.
Premixed insulin improved patient adherence because of its simplified treatment regimens, fewer injections, and low price. Therefore, premixed insulin is widely used, especially in developed countries. However, the unsatisfactory glycemic control in patients on premixed insulin therapy needs to be evaluated more carefully, not only HbA1c, but also hypoglycemia and blood glucose variability. Lipohypertrophy and autoimmune insulin antibodies may also affect blood glucose control in these patients. Long-acting insulin analogues with or without rapid-acting insulin analogues and new insulin formulations will partially solve these problems.
| 1. | Polinski JM, Kim SC, Jiang D, Hassoun A, Shrank WH, Cos X, Rodríguez-Vigil E, Suzuki S, Matsuba I, Seeger JD, Eddings W, Brill G, Curtis BH. Geographic patterns in patient demographics and insulin use in 18 countries, a global perspective from the multinational observational study assessing insulin use: understanding the challenges associated with progression of therapy (MOSAIc). BMC Endocr Disord. 2015;15:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Gross JL, Rojas A, Shah S, Tinahones FJ, Cleall S, Rodríguez A. Efficacy and safety of a premixed versus a basal-plus insulin regimen as intensification for type 2 diabetes by timing of the main meal. Curr Med Res Opin. 2016;32:1109-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Moon SJ, Choe HJ, Kwak SH, Jung HS, Park KS, Cho YM. Comparison of Prevailing Insulin Regimens at Different Time Periods in Hospitalized Patients: A Real-World Experience from a Tertiary Hospital. Diabetes Metab J. 2022;46:439-450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 4. | Lingvay I, Handelsman Y, Linjawi S, Vilsbøll T, Halladin N, Ranc K, Liebl A. EFFICACY AND SAFETY OF IDEGLIRA IN OLDER PATIENTS WITH TYPE 2 DIABETES. Endocr Pract. 2019;25:144-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Wang W, Agner BFR, Luo B, Liu L, Liu M, Peng Y, Qu S, Stachlewska KA, Wang G, Yuan G, Zhang Q, Ning G. DUAL I China: Improved glycemic control with IDegLira versus its individual components in a randomized trial with Chinese participants with type 2 diabetes uncontrolled on oral antidiabetic drugs. J Diabetes. 2022;14:401-413. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 6. | Jude EB, Ali A, Emral R, Nanda N, Lubwama R, Palmer KD, Shaunik A, Raskin P, Gomez-peralta F, Trescoli C. 1029-P: Effectiveness of Premix Insulin (Premix) in Type 2 Diabetes (T2D): A Retrospective UK Cohort Study. Diabetes. 2020;69. [DOI] [Full Text] |
| 7. | Chen X, Xu Y, Zhang J, Shao S, Duan Y, Liu P, Shen L, Zhang J, Zeng J, Lin M, Zhao S, Ma J, Zhao T, Hu J, Liao Y, Chen X, Hu S, Xue Y, Zeng Z, He W, Liu Z, Li W, Liu L, Yin P, Yu X. Exenatide Twice Daily Plus Glargine Versus Aspart 70/30 Twice Daily in Patients With Type 2 Diabetes With Inadequate Glycemic Control on Premixed Human Insulin and Metformin. Endocr Pract. 2021;27:790-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Maiorino MI, Bellastella G, Esposito K, Giugliano D. Premixed insulin regimens in type 2 diabetes: pros. Endocrine. 2017;55:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Spollett GR. Improved Disposable Insulin Pen Devices Provide an Alternative to Vials and Syringes for Insulin Administration. Diabetes Spectr. 2012;25:117-122. [DOI] [Full Text] |
| 10. | Zhang X, Ma Y, Chen H, Lou Y, Ji L, Chen L. A pragmatic study of mid-mixture insulin and basal insulin treatment in patients with type 2 diabetes uncontrolled with oral antihyperglycaemic medications: A lesson from real-world experience. Diabetes Obes Metab. 2020;22:1436-1442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Wang H, Zhou Y, Wang Y, Cai T, Hu Y, Jing T, Ding B, Su X, Li H, Ma J. Basal Insulin Reduces Glucose Variability and Hypoglycaemia Compared to Premixed Insulin in Type 2 Diabetes Patients: A Study Based on Continuous Glucose Monitoring Systems. Front Endocrinol (Lausanne). 2022;13:791439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 12. | Zhang B, Zhao J, Yang W; Lantus Registry Study Group. Glycemic control and safety in Chinese patients with type 2 diabetes mellitus who switched from premixed insulin to insulin glargine plus oral antidiabetics: a large, prospective, observational study. Diabetes Metab Res Rev. 2017;33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Yan RN, Cai TT, Jiang LL, Jing T, Cai L, Xie XJ, Su XF, Xu L, He K, Cheng L, Cheng C, Liu BL, Hu Y, Ma JH. Real-Time Flash Glucose Monitoring Had Better Effects on Daily Glycemic Control Compared With Retrospective Flash Glucose Monitoring in Patients With Type 2 Diabetes on Premix Insulin Therapy. Front Endocrinol (Lausanne). 2022;13:832102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Bellido V, Suarez L, Rodriguez MG, Sanchez C, Dieguez M, Riestra M, Casal F, Delgado E, Menendez E, Umpierrez GE. Comparison of Basal-Bolus and Premixed Insulin Regimens in Hospitalized Patients With Type 2 Diabetes. Diabetes Care. 2015;38:2211-2216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 15. | Mathiesen ER, Alibegovic AC, Corcoy R, Dunne F, Feig DS, Hod M, Jia T, Kalyanam B, Kar S, Kautzky-Willer A, Marchesini C, Rea RD, Damm P; EXPECT study group. Insulin degludec versus insulin detemir, both in combination with insulin aspart, in the treatment of pregnant women with type 1 diabetes (EXPECT): an openlabel, multinational, randomised, controlled, non-inferiority trial. Lancet Diabetes Endocrinol. 2023;11:86-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 32] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 16. | Raghavan A, Nanditha A, Satheesh K, Susairaj P, Vinitha R, Nair DR, Snehalatha C, Ramachandran A. A prospective, multicentre, randomized, open-label comparison of a long-acting basal insulin analog glargine plus glulisine with premixed insulin in insulin naïve patients with Type 2 diabetes - A study from India. Prim Care Diabetes. 2024;18:210-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 17. | Janež A, Guja C, Mitrakou A, Lalic N, Tankova T, Czupryniak L, Tabák AG, Prazny M, Martinka E, Smircic-Duvnjak L. Insulin Therapy in Adults with Type 1 Diabetes Mellitus: a Narrative Review. Diabetes Ther. 2020;11:387-409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 18. | Giugliano D, Chiodini P, Maiorino MI, Bellastella G, Esposito K. Intensification of insulin therapy with basal-bolus or premixed insulin regimens in type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Endocrine. 2016;51:417-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 19. | Disclosures: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47:S309-S313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 20. | Jia W, Weng J, Zhu D, Ji L, Lu J, Zhou Z, Zou D, Guo L, Ji Q, Chen L, Chen L, Dou J, Guo X, Kuang H, Li L, Li Q, Li X, Liu J, Ran X, Shi L, Song G, Xiao X, Yang L, Zhao Z; Chinese Diabetes Society. Standards of medical care for type 2 diabetes in China 2019. Diabetes Metab Res Rev. 2019;35:e3158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 517] [Article Influence: 73.9] [Reference Citation Analysis (0)] |
| 21. | Shen Y, Song X, Ren Y. Insulin autoimmune syndrome induced by exogenous insulin injection: a four-case series. BMC Endocr Disord. 2019;19:148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Li Z, Yi D, Zheng L, Li S, Fang W, Wang C. Analysis of the clinical characteristics of insulin autoimmune syndrome induced by exogenous insulin in diabetic patients. Diabetol Metab Syndr. 2021;13:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Chen S, Chen H, Jiang Y, Zheng X, Zhang M, Yang T, Gu Y. Association of subclass distribution of insulin antibody with glucose control in insulin-treated type 2 diabetes mellitus: a retrospective observational study. Front Endocrinol (Lausanne). 2023;14:1141414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 24. | Zhang P, Jiang Q, Ding B, Yan RN, Hu Y, Ma JH. Association between glucose-lowering drugs and circulating insulin antibodies induced by insulin therapy in patients with type 2 diabetes. World J Diabetes. 2024;15:1489-1498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 25. | Liu Y, Ping F, Yu J, Lv L, Zhao Y, Qi M, Li W, Xu L, Yu M, Li M, Zhang H, Li Y. Hypoglycemia Caused by Exogenous Insulin Antibody Syndrome: A Large Single-Center Case Series From China. J Clin Endocrinol Metab. 2023;108:713-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 26. | Meng Z, Xu C, Liu H, Gao X, Li X, Lin W, Ma X, Yang C, Hao M, Zhao K, Hu Y, Wang Y, Kuang H. Effects of mulberry twig alkaloids(Sangzhi alkaloids) and metformin on blood glucose fluctuations in combination with premixed insulin-treated patients with type 2 diabetes. Front Endocrinol (Lausanne). 2023;14:1272112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 27. | Barola A, Tiwari P, Bhansali A, Grover S, Dayal D. Insulin-Related Lipohypertrophy: Lipogenic Action or Tissue Trauma? Front Endocrinol (Lausanne). 2018;9:638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 28. | Gentile S, Guarino G, Della Corte T, Marino G, Fusco A, Corigliano G, Colarusso S, Piscopo M, Improta MR, Corigliano M, Martedi E, Oliva D, Russo V, Simonetti R, Satta E, Romano C, Vaia S, Strollo F; AMD-OSDI Study Group on Injection Techniques; Nefrocenter Network and Nyx Start-up Study Group. Lipohypertrophy in Elderly Insulin-Treated Patients With Type 2 Diabetes. Diabetes Ther. 2021;12:107-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 29. | Pozzuoli GM, Laudato M, Barone M, Crisci F, Pozzuoli B. Errors in insulin treatment management and risk of lipohypertrophy. Acta Diabetol. 2018;55:67-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 30. | Mader JK, Fornengo R, Hassoun A, Heinemann L, Kulzer B, Monica M, Nguyen T, Sieber J, Renard E, Reznik Y, Ryś P, Stożek-Tutro A, Wilmot EG. Relationship Between Lipohypertrophy, Glycemic Control, and Insulin Dosing: A Systematic Meta-Analysis. Diabetes Technol Ther. 2024;26:351-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 31. | Chen L, Xing Q, Li J, Zhou J, Yuan Y, Wan Y, Pflug BK, Strauss KW, Hirsch LJ. Injection Technique Education in Patients with Diabetes Injecting Insulin into Areas of Lipohypertrophy: A Randomized Controlled Trial. Diabetes Ther. 2021;12:813-826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 32. | Radermecker RP, Piérard GE, Scheen AJ. Lipodystrophy reactions to insulin: effects of continuous insulin infusion and new insulin analogs. Am J Clin Dermatol. 2007;8:21-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 33. | Gupta S, Ramteke H, Gupta S, Gupta S, Gupta KS. Are People With Type 1 Diabetes Mellitus Appropriately Following Insulin Injection Technique Practices: A Review of Literature. Cureus. 2024;16:e51494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 34. | Bahendeka S, Kaushik R, Swai AB, Otieno F, Bajaj S, Kalra S, Bavuma CM, Karigire C. EADSG Guidelines: Insulin Storage and Optimisation of Injection Technique in Diabetes Management. Diabetes Ther. 2019;10:341-366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 35. | Ucieklak D, Mrozińska S, Wojnarska A, Małecki MT, Klupa T, Matejko B. Type 1 Diabetes Mellitus and Lipohypertrophy - Impact of the Intervention on Glycemic Control via Patient's Examination and Retraining on Change of Infusion Set. Endocr Pract. 2023;29:174-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Mehta R, Chen R, Hirose T, John M, Kok A, Lehmann R, Unnikrishnan AG, Yavuz DG, Fulcher G. Practical use of insulin degludec/insulin aspart in a multinational setting: beyond the guidelines. Diabetes Obes Metab. 2020;22:1961-1975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Wu Y, Zhang J, Li A. Switching from Premixed Insulin to Insulin Degludec/Insulin Aspart for the Management of Type 2 Diabetes Mellitus: Implications of a Real-World Study on Insulin Degludec Dosing. Diabetes Ther. 2024;15:2515-2523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 38. | Liu M, Gu W, Chen L, Li Y, Kuang H, Du J, Alvarez A, Lauand F, Souhami E, Zhang J, Xu W, Du Q, Mu Y; SoliD trial investigators. The efficacy and safety of iGlarLixi versus IDegAsp in Chinese people with type 2 diabetes suboptimally controlled with oral antidiabetic drugs: The Soli-D randomized controlled trial. Diabetes Obes Metab. 2024;26:3791-3800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 39. | Chi W, Song J, Yazdanfard S, Daggolu J, Varisco TJ. Why the increase? Examining the rise in prescription medication expenditures in the United States between 2011 and 2020. Res Social Adm Pharm. 2024;20:432-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 40. | Luo Q, Zhou L, Zhou N, Hu M. Cost-effectiveness of insulin degludec/insulin aspart versus biphasic insulin aspart in Chinese population with type 2 diabetes. Front Public Health. 2022;10:1016937. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 41. | Hoeg-Jensen T, Kruse T, Brand CL, Sturis J, Fledelius C, Nielsen PK, Nishimura E, Madsen AR, Lykke L, Halskov KS, Koščová S, Kotek V, Davis AP, Tromans RA, Tomsett M, Peñuelas-Haro G, Leonard DJ, Orchard MG, Chapman A, Invernizzi G, Johansson E, Granata D, Hansen BF, Pedersen TA, Kildegaard J, Pedersen KM, Refsgaard HHF, Alifrangis L, Fels JJ, Neutzsky-Wulff AV, Sauerberg P, Slaaby R. Glucose-sensitive insulin with attenuation of hypoglycaemia. Nature. 2024;634:944-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/