Published online May 15, 2024. doi: 10.4239/wjd.v15.i5.810
Peer-review started: November 29, 2023
First decision: January 25, 2024
Revised: February 1, 2024
Accepted: March 8, 2024
Article in press: March 8, 2024
Published online: May 15, 2024
Processing time: 163 Days and 8.7 Hours
In this editorial, we comment on an article by Liao et al published in the current issue of the World Journal of Diabetes. We focus on the clinical significance of tibial transverse transport (TTT) as an effective treatment for patients with diabetic foot ulcers (DFU). TTT has been associated with tissue regeneration, improved blood circulation, reduced amputation rates, and increased expression of early angiogenic factors. Mechanistically, TTT can influence macrophage polarization and growth factor upregulation. Despite this potential, the limitations and conflicting results of existing studies justify the need for further research into its optimal application and development. These clinical implications highlight the efficacy of TTT in recalcitrant DFU and provide lasting stimuli for tissue re-generation, and blood vessel and bone marrow improvement. Immunomodulation via systemic responses contributes to its therapeutic potential. Future studies should investigate the underlying molecular mechanisms to enhance our understanding and the efficacy of TTT. This manuscript emphasizes the potential of TTT in limb preservation and diabetic wound healing and suggests avenues for preventive measures against limb amputation in diabetes and peripheral artery disease. Here, we highlight the clinical significance of the TTT and its importance in healing DFU to promote the use of this technique in tissue regeneration.
Core Tip: Tibial transverse transport (TTT) operation is an effective modern-day technique of treating diabetic foot ulcers (DFU) with a high rate of healing and limb savage compared to conventional surgery. TTT significantly improves blood circulation, release of angiogenic factors and reduces recurrence rate of DFU.
- Citation: Mukherjee S, Im SS. Impact of tibial transverse transport in tissue regeneration and wound healing with perspective on diabetic foot ulcers. World J Diabetes 2024; 15(5): 810-813
- URL: https://www.wjgnet.com/1948-9358/full/v15/i5/810.htm
- DOI: https://dx.doi.org/10.4239/wjd.v15.i5.810
Diabetes mellitus (DM) is a progressive, debilitating disorder with an increasing incidence rate worldwide. Diabetic foot ulcers (DFU) are highly morbid complications with a 19%–34% rate of occurrence in patients with chronic DM[1]. The mechanism of DFU formation is complex and is associated with concomitant peripheral arterial disease, triggering neuropathy, localized infection, and foot ischemia, leading to deformities that influence weight distribution and skin damage to the feet, typically causing deep tissue destruction[2,3]. In certain cases, this leads to the development of foot osteomyelitis and healing failure, requiring lower limb amputation[2,4]. The rising prevalence of DM is creating a global burden, with escalating DFU resulting in high mortality rates. Although auxiliary therapies are available, surgical debridement and antibiotic treatment are the most common treatments[5]. Recent investigations, mainly by Chinese surgeons, have focused on a relatively new technique, tibial transverse transport (TTT), for the treatment of diabetic foot; this method was originally based on Ilizarov’s “tension-stress rule” and “natural rebuilding regeneration theory”[6]. This procedure involves tissue regeneration via the proliferation of vascular endothelial cells and recanalization of microcirculatory blood vessels encouraged by a ceaseless and slow transfer to generate a stimulation for local tension using an external fixator[7]. Previous studies have used traditional treatments such as the use of antibiotics, cleaning wounds with adequate flushing, and removal of damaged tissues to treat infected wounds of diabetic feet. However, these interventions have proven to be inadequate, failing to provide efficient treatment for preventing the infection. The use of TTT for the healing of diabetic foot wounds has been shown to improve blood circulation in the affected limb by accelerating the expression of the angiogenic factors in the serum which significantly diminishes the limb amputation ratio[8]. One study proposed that TTT could be a more effective treatment in comparison to conventional surgery of the ulcers in the infected area at the lower extremity[9]. In accordance with the retrospective study by Liao et al[10], another interesting study by Reardon et al[11], in 2020 highlighted that TTT could significantly foster healing of diabetic foot wound by stimulating regeneration of the blood vessels and improve circulation of blood in the leg and foot areas of the patients[10,11]. In addition, the authors categorized diabetic feet into arterial and non-arterial stenosis groups based on the hemodynamic characteristics observed during wound healing (Liao et al[10]), which is an important aspect of the treatment process[10]. Nonetheless, the study has certain limitations, including being a single-center observational study with a non-randomized patient group and having an insufficient sample size without any proper revelation of the in-depth biological mechanisms of TTT. Elucidating the mechanisms underlying the impact of TTT is essential for understanding how TTT could promote wound healing in DFU and for determining its efficacy. TTT has also been reported to successfully treat primary lymphedema of the lower extremities[2]; however, there are controversial reports on the complications associated with this technique. In conclusion, more relevant evidence is required to guide the application and development of TTT.
Through the beginning of the 18th century, traction osteogenesis experiments were conducted on dog legs by Ilizarov[12] and demonstrated regeneration of the microvascular network prior to osteogenesis in the gap between the traction area of the injured bone[12,13]. Further research by Chinese scholars and physicians has applied this theory of tissue regeneration and developed many modified TTT techniques for the treatment of DFU[14]. With respect to basic research, the underlying mechanisms of TTT are complex and involve many factors[7]. Previous studies have reported that TTT aids in lowering the inflammatory responses henceforth facilitating activation of local stem cell by promoting the polarization of M1 macrophage inflammatory responses in distant wounds, whereas M2 macrophages are devoted to anti-inflammatory responses and establishing tissue regeneration[15,16]. A study by Chen et al[17] showed wound healing with improved skin stem cell regeneration when comparing tissue sections of patients before and after TTT; sections showed a significant decrease in the M1/M2 ratio, thereby improving the polarization balance of macrophages[17]. Interestingly, a different group showed significant increases in levels of expression for various growth factors, including vascular endothelial growth factor, basic fibroblast growth factor, epidermal growth factor, and platelet-derived growth factor as a repair mechanism in ulcer tissue after TTT in one study[18]. In a follow up study, the same group reported the possible activation of the stromal cell-derived factor-1/CXC chemokine receptor 4 signaling pathway during skin wound healing in DFU after TTT in a diabetic rat model [19].
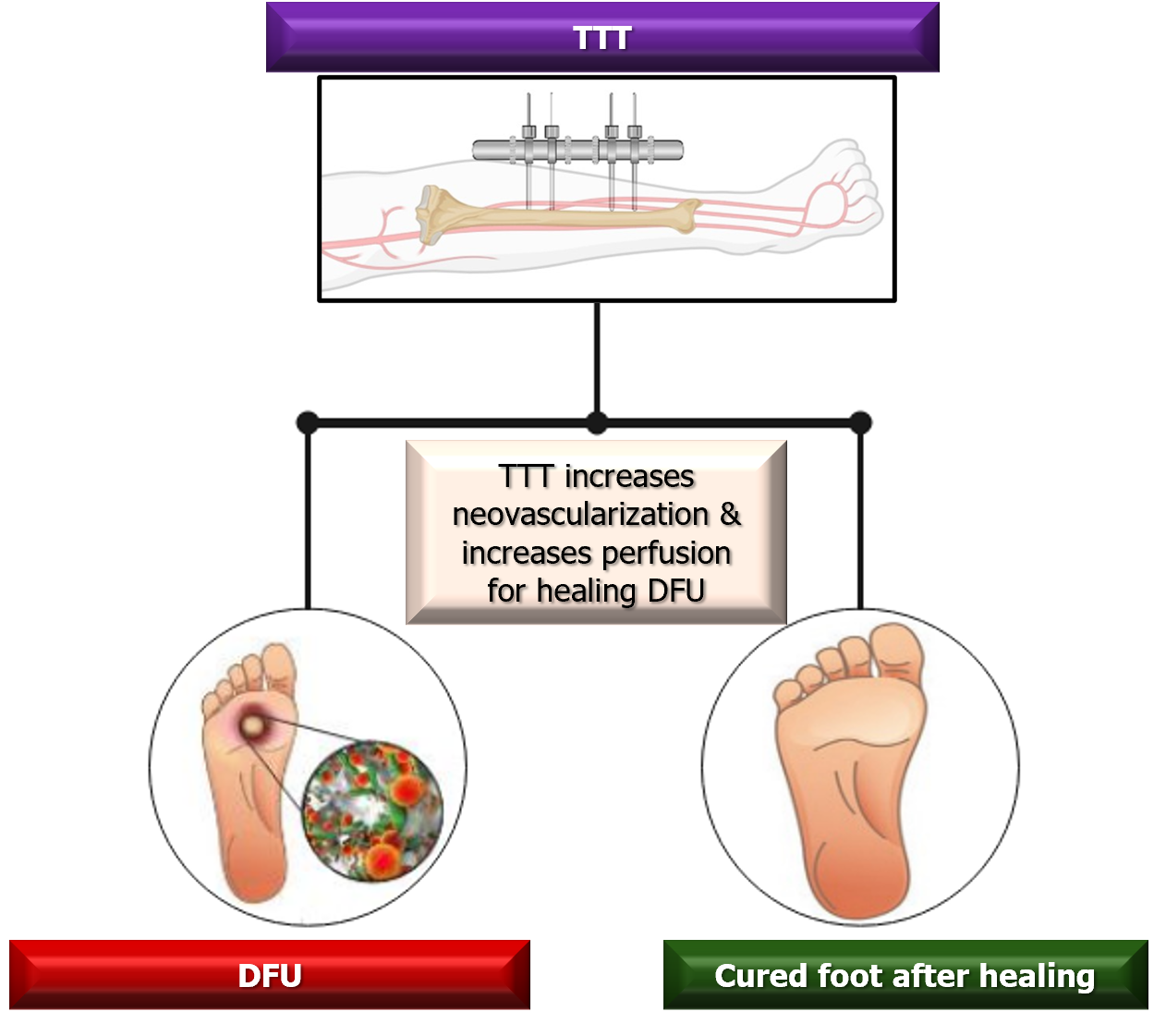
DFU is a medically challenging concern. There are several approaches for treating DFU, including debridement, oxygen therapy, off-loading, and skin substitutes[8]; however, these methods would require simultaneous evaluation of their efficacy, safety, and cost-effectiveness. Compared with other therapeutic methods, the TTT technique can be used as an effective treatment in patients with recalcitrant DFU by providing a stable activity to the bone tissue, muscles, and nerves (Figure 1). This process is achieved via mechanical tensile to promote bone marrow as well as blood vessel regeneration and improve the circulatory system[4,20] and immunomodulation[21,22], ultimately restoring limb perception. Moreover, the TTT procedure may also induce systemic responses[23], including the mobilization of bone marrow-derived mesenchymal stem cells and changes of circulating cytokines, triggered by mechanotransduction[19]. Future studies adopting molecular mechanisms to understand the pathogenesis and management of diabetic foot treatment are required to improve tissue regeneration and healing of diabetic ulcers. In the current issue by Liao et al[10] in 2023, the authors unravel the progress of smooth healing of DFU and the effects of TTT in the early stages of treatment, finally reporting improved microcirculation perfusion, blood flow volume, and velocity in patients with arterial stenosis[10]. However, as in many other studies, this work failed to record the impact of the TTT at the later stages of treatment; future investigations should consider this.
In conclusion, the use of tibial transport for limb preservation and diabetic wound healing offers new treatment options for patients with diabetes and peripheral artery disease. Further innovative treatments and interdisciplinary research could prevent limb amputations in current and future generations.
| 1. | Hu XX, Xiu ZZ, Li GC, Zhang JY, Shu LJ, Chen Z, Li H, Zou QF, Zhou Q. Effectiveness of transverse tibial bone transport in treatment of diabetic foot ulcer: A systematic review and meta-analysis. Front Endocrinol (Lausanne). 2022;13:1095361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Zhang X, Dong T, Yao S, Lu S, Li W. Application of transverse tibial bone transport and microcirculation reconstruction in the treatment of diabetic foot ulcer: a case report. Ann Palliat Med. 2021;10:8358-8364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 3. | Bari MM, Bari AMSR. Management of Diabetic Foot Ulcer (DFU) using Tibial Transverse Technique (TTT), Bone lengthening; Bangladesh Experience. Int J Allied Health Sci. 2021;5:2279-2279. |
| 4. | Chen Y, Ding X, Zhu Y, Jia Z, Qi Y, Chen M, Lu J, Kuang X, Zhou J, Su Y, Zhao Y, Lu W, Zhao J, Hua Q. Effect of tibial cortex transverse transport in patients with recalcitrant diabetic foot ulcers: A prospective multicenter cohort study. J Orthop Translat. 2022;36:194-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 5. | Ding X, Yuan Y, Lu H, Wang Y, Ji K, Lv H, Xu H, Zhou J. Analysis of the Effect of Antibiotic Bone Cement in the Treatment of Diabetic Foot Ulcer through Tibia Transverse Transport. Orthop Surg. 2022;14:2141-2149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 6. | Geraghty T, LaPorta G. Current health and economic burden of chronic diabetic osteomyelitis. Expert Rev Pharmacoecon Outcomes Res. 2019;19:279-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 7. | Guo J, Bao H, Hu H, Lideer, Ni X, Zhao Y, Sun G. Effect of tibial transverse transport on chronic lower extremity angiopathy: a protocol for a systematic review and meta-analysis. BMJ Open. 2022;12:e060249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Ou S, Xu C, Yang Y, Chen Y, Li W, Lu H, Li G, Sun H, Qi Y. Transverse Tibial Bone Transport Enhances Distraction Osteogenesis and Vascularization in the Treatment of Diabetic Foot. Orthop Surg. 2022;14:2170-2179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 31] [Reference Citation Analysis (0)] |
| 9. | Nie X, Kuang X, Liu G, Zhong Z, Ding Y, Yu J, Liu J, Li S, He L, Su H, Qin W, Zhao J, Hua Q, Chen Y. Tibial cortex transverse transport facilitating healing in patients with recalcitrant non-diabetic leg ulcers. J Orthop Translat. 2021;27:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (1)] |
| 10. | Liao MM, Chen S, Cao JR, Wang MW, Jin ZH, Ye J, Ren YJ, Guo RQ. Early hemodynamics after tibial transverse transport in patients with nonarterial stenosis and arterial stenosis diabetic foot. World J Diabetes. 2023;14:1784-1792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 11. | Reardon R, Simring D, Kim B, Mortensen J, Williams D, Leslie A. The diabetic foot ulcer. Aust J Gen Pract. 2020;49:250-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 110] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 12. | Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;249-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1510] [Cited by in RCA: 1355] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 13. | Ilizarov GA. The principles of the Ilizarov method. Bull Hosp Jt Dis Orthop Inst. 1988;48:1-11. [PubMed] |
| 14. | Yuan Y, Ding X, Jing Z, Lu H, Yang K, Wang Y, Xu H. Modified tibial transverse transport technique for the treatment of ischemic diabetic foot ulcer in patients with type 2 diabetes. J Orthop Translat. 2021;29:100-105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 15. | Guilliams M, Ginhoux F, Jakubzick C, Naik SH, Onai N, Schraml BU, Segura E, Tussiwand R, Yona S. Dendritic cells, monocytes and macrophages: a unified nomenclature based on ontogeny. Nat Rev Immunol. 2014;14:571-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1141] [Cited by in RCA: 1437] [Article Influence: 119.8] [Reference Citation Analysis (0)] |
| 16. | Wynn TA, Chawla A, Pollard JW. Macrophage biology in development, homeostasis and disease. Nature. 2013;496:445-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2633] [Cited by in RCA: 3649] [Article Influence: 280.7] [Reference Citation Analysis (0)] |
| 17. | Chen Y, Kuang X, Zhou J, Zhen P, Zeng Z, Lin Z, Gao W, He L, Ding Y, Liu G, Qiu S, Qin A, Lu W, Lao S, Zhao J, Hua Q. Proximal Tibial Cortex Transverse Distraction Facilitating Healing and Limb Salvage in Severe and Recalcitrant Diabetic Foot Ulcers. Clin Orthop Relat Res. 2020;478:836-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 18. | Ou S, Xu C, Li G, Sun H, Yang Y, Lu H, Li W, Qi Y. [Effect of transverse tibial bone transport on expression of serum angiogenesis-related growth factors]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34:98-101. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Ou S, Wu X, Yang Y, Xia C, Zhang W, Qu Y, Li J, Chen B, Zhu L, Xu C, Qi Y. Tibial cortex transverse transport potentiates diabetic wound healing via activation of SDF-1/CXCR4 signaling. PeerJ. 2023;11:e15894. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 20. | Zuo Q, Gao F, Song H, Zhou J. Application of Ilizarov transverse tibial bone transport and microcirculation reconstruction in the treatment of chronic ischemic diseases in lower limbs. Exp Ther Med. 2018;16:1355-1359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 21. | Yang C, Zeisberg M, Mosterman B, Sudhakar A, Yerramalla U, Holthaus K, Xu L, Eng F, Afdhal N, Kalluri R. Liver fibrosis: insights into migration of hepatic stellate cells in response to extracellular matrix and growth factors. Gastroenterology. 2003;124:147-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 231] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 22. | Yang Y, Li Y, Pan Q, Bai S, Wang H, Pan XH, Ling KK, Li G. Tibial cortex transverse transport accelerates wound healing via enhanced angiogenesis and immunomodulation. Bone Joint Res. 2022;11:189-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 23. | Li G, Ling SKK, Li HA, Zhang Y, Hu J. How to perform minimally invasive tibial cortex transverse transport surgery. J Orthop Transl. 2020;25:28-32. [DOI] [Full Text] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Republic of Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fu L, China; Yoshida S, Japan S-Editor: Li L L-Editor: A P-Editor: Chen YX