Published online May 15, 2021. doi: 10.4239/wjd.v12.i5.569
Peer-review started: December 2, 2020
First decision: March 16, 2021
Revised: March 16, 2021
Accepted: March 29, 2021
Article in press: March 29, 2021
Published online: May 15, 2021
Processing time: 154 Days and 20 Hours
Hypoglycemia limits optimal glycemic management of patients with type 1 diabetes mellitus (T1DM). Fear of hypoglycemia (FoH) is a significant psycho
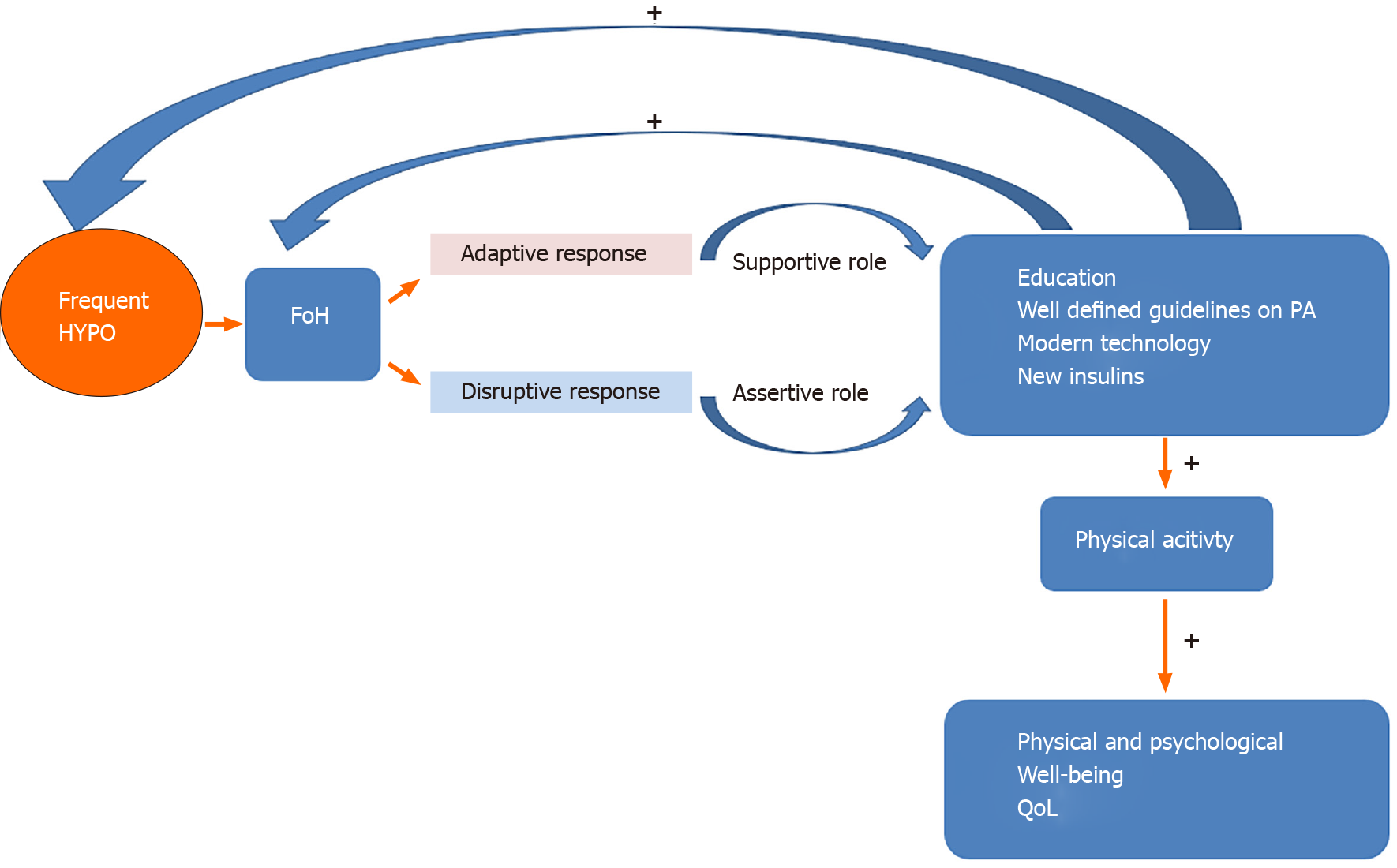
Core Tip: Fear of hypoglycemia (FoH) is a major barrier to achieving recommended childhood and adult levels of physical activity (PA) in type 1 diabetes mellitus patients. The main factor associated with FoH is the frequency of hypoglycemia. The occurrence of hypoglycemia can be mitigated by well-defined recommendations on performing PA and maintaining euglycemia, implementing modern technologies and improved insulin regimens, educational programs, and social media information.
- Citation: Cigrovski Berkovic M, Bilic-Curcic I, La Grasta Sabolic L, Mrzljak A, Cigrovski V. Fear of hypoglycemia, a game changer during physical activity in type 1 diabetes mellitus patients. World J Diabetes 2021; 12(5): 569-577
- URL: https://www.wjgnet.com/1948-9358/full/v12/i5/569.htm
- DOI: https://dx.doi.org/10.4239/wjd.v12.i5.569
Intensified insulin regimens aim to achieve a near-normal glucose level, which is the primary goal of type 1 diabetes mellitus (T1DM) management because it is associated with a decreased risk of long-term chronic micro- and macrovascular complications. On the other hand, intensive treatment increases the risk of acute side effects, such as hypoglycemia, which in itself correlates with increased morbidity and even mortality[1,2]. Hypoglycemia is often the limiting factor in the glycemic management of T1DM patients[3], and it can compromise patients' willingness to maintain a healthy lifestyle, primarily adversely affecting involvement in regular physical activity (PA)[4]. Reducing the risk of hypoglycemia and, at the same time, maintaining or improving glycemic control is imperative. Patient education, empowerment, modern technology, improved insulin regimens, and healthcare workers' support are deemed necessary.
Regular PA beginning in early childhood is important for both physical and psychological development. For individuals with T1DM, PA offers many health benefits, including improved glycemic control and blood lipid profiles, better cardiovascular function, and psychological wellbeing[5,6]. Unfortunately, most people with T1DM do not regularly engage in adequate PA. As a direct or indirect consequence, as many as 60% of patients have hyperlipidemia, 40% have hypertension, and 60% are obese or overweight, thus having an increased cardiovascular risk[7]. On the other hand, the results of an extensive cross-sectional study suggest that regular PA that includes exercising ≥ 2 times weekly can improve cardiometabolic parameters and reduce microvascular complications (e.g., nephropathy-microalbuminuria or retinopathy) of diabetes[8]. Exercise intervention studies have generally failed to show clinically meaningful improvements in hemoglobin A1c (HbA1c) with PA in T1DM[9]. That might be attributable to differences in study design and exercise dosage as well as adjustments of insulin dosing and/or carbohydrate intake while exercising intended to minimize exercise-induced hypoglycemia and ensure safe blood glucose levels[10]. The study by Dube et al[11] found that people with T1DM who were engaged in moderate or intense PA reported increased HbA1c, carbohydrate consumption, and weight gain, which was explained by their tendency to avoid hypoglycemia. Therefore, hypoglycemia and fear of hypoglycemia (FoH), in addition to lack of knowledge of exercise management in T1DM, are significant obstacles in reaching recommended PA targets.
FoH encompasses an anxiety disorder in patients and their families that is caused by hypoglycemia and the associated behavioral changes affecting glycemic management, such as avoiding exercise, maintaining high blood glucose levels, and administering low insulin doses[12]. FoH can have a severe impact not only on regular exercise but also on all aspects of life quality. Anxiety is the most common consequence of hypoglycemia-induced distress leading to two potential scenarios. One could be adaptive, instigating productive behavior regarding glucose management[13,14]. However, that could also be disruptive, triggering behavioral changes leading to poor glycemic control and impaired quality of life[15]. So far, it has been shown that, FoH frequently occurs in parents who report severe hypoglycemia in their children[16,17]. Several studies have confirmed a positive correlation between FoH and HbA1c in young children and adolescents and that high parent and adolescent scores in an FoH survey were associated with increased HbA1c levels[18-20]. Other factors affecting parental FoH were nonmodifiable sociodemographics (e.g., age, education, nationality) and modifiable psychological factors (e.g., mindful parenting)[21]. A study assessing FoH in adult patients identified the frequency of severe hypoglycemia as the most relevant factor associated with FoH[22]. In addition, several predictive factors such as female gender, hypoglycemia unawareness, and glucose variability seem to be associated with hypoglycemia[23]. Moreover, FoH was recently shown not to be time-dependent in most cases, but to be conditioned by change in hypoglycemia frequency, which emphasizes the significance of mitigating hypoglycemic events[24]. Results of the Diabetes MILES study in the Netherlands have shown that FoH in adults with T1DM was associated with a history of hypoglycemia and depressive symptoms[25]. Interestingly, although FoH is a major obstacle to performing regular PA, there are few data on FoH and exercise. However, existing studies identified FoH as a major culprit for inadequate exercise[26-28]. Surprisingly, in the SEARCH for Diabetes in Youth Case-Control Study, 82% of participants with T1DM achieved the recommended PA goals compared to healthy peers[29], in contrast to the 33% of young adults with T2DM who achieved the recommended PA targets[7]. Recently published data showed that increased levels of vigorous PA (VPA) were associated with increased FoH scores in SEARCH patients with T1DM. In addition, there was a decrease in VPA with age and an increase in moderate PA[30]. Therefore, we can assume that FoH does not affect PA or that VPA is considered a better option, given recent recommendations that include the benefits of high intensity interval training (HIIT) to avoid hypoglycemia[31]. In the same study, HbA1c positively correlated with pediatric FoH, resulting in poor glycemic control. On the other hand, lower HbA1c correlated with higher VPA, emphasizing a well-known positive effect of PA on glucose management[32].
Although the recommendations on PA for people with T1DM and those with type 2 diabetes mellitus do not differ, some specifics need to be considered. In general, 150 min of accumulated aerobic PA is recommended weekly, with no more than 2 consecutive days without PA plus resistance training two to three times weekly, but not on consecutive days[33]. For children and adolescents, the recommendation is to be involved in PA at least 60 min daily[34,35].
What makes the difference in managing PA in the case of T1DM are the specific patient goals for exercise (e.g., metabolic control, prevention of complications, fitness, weight loss, or competition and performance), which should be considered before decisions on diabetes management are made. For example, strategies behind exercising for weight loss should focus on reducing insulin doses during and after exercise instead of consuming carbohydrates. On the other hand, if sports results and exercise performance are the primary goals, nutritional guidance specific to the sporting activity is most important, while modifications in insulin dosing are secondary to match the new/additional nutritional requirements. Regardless of the set goals, blood glucose monitoring before, during, and after exercise is essential to avoid hypo and hyperglycemia[36-38]. Despite the perceived benefits, many young people with T1DM do not meet the proposed PA recommendations[39], and it is still unclear what would be the most effective type of exercise for improvement of metabolic control and cardiovascular health in people with T1DM[40,41].
From a practical standpoint, to minimize the risk of hypoglycemia, glycemic levels during, but also before and after exercise should be individually tailored. For the majority of patients with T1DM, the starting glucose range should be somewhere between 7-10 mmol/L when initiating aerobic exercise lasting up to an hour. When engaging in HIIT and anaerobic exercise, training can be initiated at the lower starting glucose concentration range, somewhere between 5-7 mmol/L, as during this kind of exercise, glucose levels either remain stable or even tend to rise[31]. Although it is still unclear whether there is an optimal glycemic range during exercise, available data suggest that concentrations between 6-8 mmol/L should be preferred[42]. Strategies to prevent hypoglycemia rely on previous hypoglycemic episodes, which should be taken into account when planning subsequent PA[43]. An episode of severe hypoglycemia within the previous 24 h presents a contraindication to exercise[44]. As insulin sensitivity increases after exercise (and can remain increased for up to 48 h[45]), strategies to minimize exercise-related hypoglycemia, especially nocturnal occurrence, should be employed, including the avoidance of the exercise during the late afternoon[46-48].
Regular PA is usually recommended as an integral part of diabetes management in children and adults with T1DM[33,35]. However, it is frequently accompanied by unwanted blood glucose changes and requiring a range of potential preventive measures. Even if implemented, precautions are not always sufficient to avoid excessive glucose excursions. Moreover, handling different forms of PA can be particularly challenging for both individuals with T1DM and healthcare providers, whereby the decision-making process is often trial and error based[49]. In younger children, the tricky part about PA is that it is often unplanned and unpredictable.
Among the well-known barriers to regular PA, FoH and loss of glycemic control are shared by adults and youth with T1DM[26,27,31]. Consequently, the need for education on safe PA practices is widely recognized and acknowledged[30,31,50,51]. Recent advances in insulin formulations, delivery methods, continuous glucose monitoring (CGM) systems, applications (apps), and algorithms that integrate novel technologies are expected to improve glycemic control with less hypoglycemia and a better quality of life for people with T1DM.
Insulin therapy has been the cornerstone of diabetes management for almost a century, and despite the current availability of a wide array of insulin preparations, significant unmet needs remain[52]. With rapid-acting insulin analogs (e.g., insulin aspart, lispro, glulisine), a reduction in bolus dose accompanying the meal before exercise is still required. On the other hand, with new long-acting basal insulin analogs (e.g., degludec, glargine U300), dose adjustments for PA are impractical and cannot be performed without overall glycemic control disturbance[31]. A glucose-responsive insulin patch, an innovative and promising treatment option already successfully tested in diabetic animals, is awaiting clinical trials in humans.
In recent years there has been a great expansion of diabetes-specific technology, including CGM systems, insulin pumps, and automated insulin delivery systems. Glycemic management during exercise has been made easier with CGM technology. Most common CGM systems measure glucose in the interstitial fluid, providing real-time sensor glucose data (rtCGM) and triggering alerts for hypo and hyperglycemia. Intermittently scanned CGM systems (isCGM) measure interstitial glucose levels at the time of scanning and lack alarms. A lag time between blood and interstitial fluid glucose value exists and is particularly pronounced when blood glucose levels change rapidly, that occur during exercise. Furthermore, physiological changes during PA, such as alterations in blood flow rate, body temperature, and acidity, can theoretically disturb interstitial glucose-sensing accuracy[53]. General recommendations can be used as an initial guidance tool when using rtCGM/isCGM before exercise, during exercise, after exercise, and the nocturnal post-exercise phase[54]. However, for different groups of people with T1DM, different glycemic ranges around exercise may be required. Finally, all recommendations should be tailored individually, relying on the use of sensor glucose values accompanied by trend arrows while employing safe sensor glucose thresholds[54].
Insulin pumps offer better flexibility in insulin dose adjustments and management of exercise-associated glucose excursions than other insulin delivery methods[55-57]. Basal rate reduction mitigates the risk of hyperglycemia after moderate exercise more effectively than basal insulin suspension and appears to be associated with reduced risk of hypoglycemia both during and after PA[58]. However, the optimal timing and percentage of basal rate reduction have to be individually determined. Besides, for a more effective reduction of circulating insulin levels during PA, the remaining insulin from the bolus applied within the previous 2 h can be considered[59]. For intense exercise, the best option is to temporarily stop the pump, which coincides quite nicely with the preference of patients who wish to remove their pump during activity. To prevent early exercise-related hypoglycemia after the meal, the premeal bolus dose reduction might be more effective than reducing the basal rate[58].
Sensor-augmented pump therapy combines insulin pumps, CGM systems, and therapy management software to automatically suspend insulin delivery for up to two hours when CGM detects a glucose level that has reached a prespecified threshold or to suspend insulin in anticipation of hypoglycemic events. In recent years, those devices have been connected to create a more automated glucose monitoring and insulin dosing combo marketed as a closed-loop system that automatically adjusts basal insulin delivery based on CGM readings[60]. Several studies have shown a reduction in hypoglycemia incidence and severity in patients using closed-loop systems in pediatric and adult patients[61,62]. However, although effective and highly promising, these systems warrant further research for an optimized use around exercise[63].
Digital health technology is developing rapidly, and numerous health-related apps installed on smartphones or other wireless devices are already available to support people with diabetes in lifestyle interventions or insulin adjustments in response to glucose monitoring data[64]. Several apps are primarily intended to support PA in people with T1DM, as they allow users to track activity, count calories, and set goals for exercise and weight management. However, the available evidence on the safety and efficacy of such stand-alone diabetes apps is still limited. Several issues, including inadequate or insufficient information on app accuracy, clinical validity, data security, and lack of user training, need to be resolved to ensure the full potential of such diabetes apps[65].
General guidelines for minimizing exercise-related glucose excursions exist, but their implementation is often burdensome for people with T1DM. As numerous factors influence glycemia during exercise, such as glucose level at the start of PA, the type, intensity, and duration of exercise as well as its' timing concerning meals, all the preventive actions require major individualization and are not always successful in avoiding hypoglycemia. Optimizing glycemic control around exercise is still demanding. Despite many advances in insulin formulations, delivery methods, and CGM systems, a thorough education is still essential. As technology continues to progress, people with T1DM are expected to achieve better glycemic control around exercise with less hypoglycemia and a lighter mental burden. However, many questions regarding availability, affordability, and adherence to expanding diabetes technology remain. Although FoH remains one of the main obstacles in achieving recommended PA levels, according to the latest research in young populations, it could even encourage more vigorous exercise patterns. Possibly, the development of new technologies, educational programs and social media information on the importance of PA, updated recommendations regarding the type and time of exercise, and necessary adjustments allowing euglycemia during and after the exercise have had a significant impact on alleviating FoH. Hopefully, future research embracing all of these FoH related aspects will enable us to minimize or disregard the problem of FoH. Finally, our understanding of exercise physiology and the different effects aerobic, anaerobic, resistance training and HIIT have on glycemic levels can minimize the risk of hypoglycemia and improve T1DM management, especially in the setting of new technology and improved insulin on board (Figure 1).
| 1. | International Hypoglycaemia Study Group. Glucose Concentrations of Less Than 3.0 mmol/L (54 mg/dL) Should Be Reported in Clinical Trials: A Joint Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2017;40:155-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 464] [Article Influence: 51.6] [Reference Citation Analysis (0)] |
| 2. | Li W, Huang E, Gao S. Type 1 Diabetes Mellitus and Cognitive Impairments: A Systematic Review. J Alzheimers Dis. 2017;57:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 122] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 3. | Seaquist ER, Anderson J, Childs B, Cryer P, Dagogo-Jack S, Fish L, Heller SR, Rodriguez H, Rosenzweig J, Vigersky R; American Diabetes Association; Endocrine Society. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. J Clin Endocrinol Metab. 2013;98:1845-1859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 185] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 4. | Gonder-Frederick L, Nyer M, Shepard JA, Vajda K, Clarke W. Assessing fear of hypoglycemia in children with Type 1 diabetes and their parents. Diabetes Manag (Lond). 2011;1:627-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 5. | Tielemans SM, Soedamah-Muthu SS, De Neve M, Toeller M, Chaturvedi N, Fuller JH, Stamatakis E. Association of physical activity with all-cause mortality and incident and prevalent cardiovascular disease among patients with type 1 diabetes: the EURODIAB Prospective Complications Study. Diabetologia. 2013;56:82-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Chimen M, Kennedy A, Nirantharakumar K, Pang TT, Andrews R, Narendran P. What are the health benefits of physical activity in type 1 diabetes mellitus? Diabetologia. 2012;55:542-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 296] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 7. | McCarthy MM, Funk M, Grey M. Cardiovascular health in adults with type 1 diabetes. Prev Med. 2016;91:138-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Bohn B, Herbst A, Pfeifer M, Krakow D, Zimny S, Kopp F, Melmer A, Steinacker JM, Holl RW; DPV Initiative. Impact of Physical Activity on Glycemic Control and Prevalence of Cardiovascular Risk Factors in Adults With Type 1 Diabetes: A Cross-sectional Multicenter Study of 18,028 Patients. Diabetes Care. 2015;38:1536-1543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 232] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 9. | Kennedy A, Nirantharakumar K, Chimen M, Pang TT, Hemming K, Andrews RC, Narendran P. Does exercise improve glycaemic control in type 1 diabetes? PLoS One. 2013;8:e58861. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 109] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 10. | Yardley J, Mollard R, MacIntosh A, MacMillan F, Wicklow B, Berard L, Hurd C, Marks S, McGavock J. Vigorous intensity exercise for glycemic control in patients with type 1 diabetes. Can J Diabetes. 2013;37:427-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Dubé MC, Prud'homme D, Lemieux S, Lavoie C, Weisnagel SJ. Relation between energy intake and glycemic control in physically active young adults with type 1 diabetes. J Sci Med Sport. 2014;17:47-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Barnard K, Thomas S, Royle P, Noyes K, Waugh N. Fear of hypoglycaemia in parents of young children with type 1 diabetes: a systematic review. BMC Pediatr. 2010;10:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 183] [Cited by in RCA: 157] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 13. | Shalitin S, Phillip M. Hypoglycemia in type 1 diabetes: a still unresolved problem in the era of insulin analogs and pump therapy. Diabetes Care. 2008;31 Suppl 2:S121-S124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Seaquist ER, Anderson J, Childs B, Cryer P, Dagogo-Jack S, Fish L, Heller SR, Rodriguez H, Rosenzweig J, Vigersky R. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013;36:1384-1395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 955] [Cited by in RCA: 995] [Article Influence: 76.5] [Reference Citation Analysis (0)] |
| 15. | Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder-Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: Implications for diabetes management and patient education. Patient Educ Couns. 2007;68:10-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 384] [Cited by in RCA: 407] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 16. | Amiri F, Vafa M, Gonder-Frederick L. Glycemic Control, Self-Efficacy and Fear of Hypoglycemia Among Iranian Children with Type 1 Diabetes. Can J Diabetes. 2015;39:302-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Haugstvedt A, Wentzel-Larsen T, Aarflot M, Rokne B, Graue M. Assessing fear of hypoglycemia in a population-based study among parents of children with type 1 diabetes - psychometric properties of the hypoglycemia fear survey - parent version. BMC Endocr Disord. 2015;15:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Johnson SR, Cooper MN, Davis EA, Jones TW. Hypoglycaemia, fear of hypoglycaemia and quality of life in children with Type 1 diabetes and their parents. Diabet Med. 2013;30:1126-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 109] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 19. | Freckleton E, Sharpe L, Mullan B. The relationship between maternal fear of hypoglycaemia and adherence in children with type-1 diabetes. Int J Behav Med. 2014;21:804-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Haugstvedt A, Wentzel-Larsen T, Graue M, Søvik O, Rokne B. Fear of hypoglycaemia in mothers and fathers of children with Type 1 diabetes is associated with poor glycaemic control and parental emotional distress: a population-based study. Diabet Med. 2010;27:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 125] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 21. | Aalders J, Hartman E, Nefs G, Nieuwesteeg A, Hendrieckx C, Aanstoot HJ, Winterdijk P, van Mil E, Speight J, Pouwer F. Mindfulness and fear of hypoglycaemia in parents of children with Type 1 diabetes: results from Diabetes MILES Youth - The Netherlands. Diabet Med. 2018;35:650-657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Anderbro T, Amsberg S, Adamson U, Bolinder J, Lins PE, Wredling R, Moberg E, Lisspers J, Johansson UB. Fear of hypoglycaemia in adults with Type 1 diabetes. Diabet Med. 2010;27:1151-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 23. | Weinstock RS, DuBose SN, Bergenstal RM, Chaytor NS, Peterson C, Olson BA, Munshi MN, Perrin AJ, Miller KM, Beck RW, Liljenquist DR, Aleppo G, Buse JB, Kruger D, Bhargava A, Goland RS, Edelen RC, Pratley RE, Peters AL, Rodriguez H, Ahmann AJ, Lock JP, Garg SK, Rickels MR, Hirsch IB; T1D Exchange Severe Hypoglycemia in Older Adults With Type 1 Diabetes Study Group. Risk Factors Associated With Severe Hypoglycemia in Older Adults With Type 1 Diabetes. Diabetes Care. 2016;39:603-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 136] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 24. | Anderbro TC, Amsberg S, Moberg E, Gonder-Frederick L, Adamson U, Lins PE, Johansson UB. A longitudinal study of fear of hypoglycaemia in adults with type 1 diabetes. Endocrinol Diabetes Metab. 2018;1:e00013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Nefs G, Bevelander S, Hendrieckx C, Bot M, Ruige J, Speight J, Pouwer F. Fear of hypoglycaemia in adults with Type 1 diabetes: results from Diabetes MILES - The Netherlands. Diabet Med. 2015;32:1289-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 26. | Brazeau AS, Rabasa-Lhoret R, Strychar I, Mircescu H. Barriers to physical activity among patients with type 1 diabetes. Diabetes Care. 2008;31:2108-2109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 374] [Cited by in RCA: 424] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 27. | Jabbour G, Henderson M, Mathieu ME. Barriers to Active Lifestyles in Children with Type 1 Diabetes. Can J Diabetes. 2016;40:170-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 28. | Martyn-Nemeth P, Quinn L, Penckofer S, Park C, Hofer V, Burke L. Fear of hypoglycemia: Influence on glycemic variability and self-management behavior in young adults with type 1 diabetes. J Diabetes Complications. 2017;31:735-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 95] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 29. | Lobelo F, Liese AD, Liu J, Mayer-Davis EJ, D'Agostino RB Jr, Pate RR, Hamman RF, Dabelea D. Physical activity and electronic media use in the SEARCH for diabetes in youth case-control study. Pediatrics. 2010;125:e1364-e1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Roberts AJ, Taplin CE, Isom S, Divers J, Saydah S, Jensen ET, Mayer-Davis EJ, Reid LA, Liese AD, Dolan LM, Dabelea D, Lawrence JM, Pihoker C. Association between fear of hypoglycemia and physical activity in youth with type 1 diabetes: The SEARCH for diabetes in youth study. Pediatr Diabetes. 2020;21:1277-1284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 31. | Riddell MC, Gallen IW, Smart CE, Taplin CE, Adolfsson P, Lumb AN, Kowalski A, Rabasa-Lhoret R, McCrimmon RJ, Hume C, Annan F, Fournier PA, Graham C, Bode B, Galassetti P, Jones TW, Millán IS, Heise T, Peters AL, Petz A, Laffel LM. Exercise management in type 1 diabetes: a consensus statement. Lancet Diabetes Endocrinol. 2017;5:377-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 701] [Cited by in RCA: 592] [Article Influence: 65.8] [Reference Citation Analysis (0)] |
| 32. | Quirk H, Blake H, Tennyson R, Randell TL, Glazebrook C. Physical activity interventions in children and young people with Type 1 diabetes mellitus: a systematic review with meta-analysis. Diabet Med. 2014;31:1163-1173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 169] [Cited by in RCA: 158] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 33. | Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, Horton ES, Castorino K, Tate DF. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care. 2016;39:2065-2079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1608] [Cited by in RCA: 1747] [Article Influence: 174.7] [Reference Citation Analysis (1)] |
| 34. | Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev. 2009;67:114-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 213] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 35. | Adolfsson P, Riddell MC, Taplin CE, Davis EA, Fournier PA, Annan F, Scaramuzza AE, Hasnani D, Hofer SE. ISPAD Clinical Practice Consensus Guidelines 2018: Exercise in children and adolescents with diabetes. Pediatr Diabetes. 2018;19 Suppl 27:205-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 125] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 36. | Adolfsson P, Mattsson S, Jendle J. Evaluation of glucose control when a new strategy of increased carbohydrate supply is implemented during prolonged physical exercise in type 1 diabetes. Eur J Appl Physiol. 2015;115:2599-2607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 37. | Campbell MD, Walker M, Trenell MI, Luzio S, Dunseath G, Tuner D, Bracken RM, Bain SC, Russell M, Stevenson EJ, West DJ. Metabolic implications when employing heavy pre- and post-exercise rapid-acting insulin reductions to prevent hypoglycaemia in type 1 diabetes patients: a randomised clinical trial. PLoS One. 2014;9:e97143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Thomas DT, Erdman KA, Burke LM. Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and Athletic Performance. J Acad Nutr Diet. 2016;116:501-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 531] [Cited by in RCA: 720] [Article Influence: 72.0] [Reference Citation Analysis (0)] |
| 39. | Lascar N, Kennedy A, Hancock B, Jenkins D, Andrews RC, Greenfield S, Narendran P. Attitudes and barriers to exercise in adults with type 1 diabetes (T1DM) and how best to address them: a qualitative study. PLoS One. 2014;9:e108019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 126] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 40. | Yardley JE, Hay J, Abou-Setta AM, Marks SD, McGavock J. A systematic review and meta-analysis of exercise interventions in adults with type 1 diabetes. Diabetes Res Clin Pract. 2014;106:393-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 41. | Salem MA, AboElAsrar MA, Elbarbary NS, ElHilaly RA, Refaat YM. Is exercise a therapeutic tool for improvement of cardiovascular risk factors in adolescents with type 1 diabetes mellitus? Diabetol Metab Syndr. 2010;2:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 96] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 42. | Kelly D, Hamilton JK, Riddell MC. Blood glucose levels and performance in a sports cAMP for adolescents with type 1 diabetes mellitus: a field study. Int J Pediatr. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 43. | Galassetti P, Tate D, Neill RA, Richardson A, Leu SY, Davis SN. Effect of differing antecedent hypoglycemia on counterregulatory responses to exercise in type 1 diabetes. Am J Physiol Endocrinol Metab. 2006;290:E1109-E1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 44. | Graveling AJ, Frier BM. Risks of marathon running and hypoglycaemia in Type 1 diabetes. Diabet Med. 2010;27:585-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 45. | Teich T, Riddell MC. The Enhancement of Muscle Insulin Sensitivity After Exercise: A Rac1-Independent Handoff to Some Other Player? Endocrinology. 2016;157:2999-3001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 46. | Frier BM. Hypoglycaemia in diabetes mellitus: epidemiology and clinical implications. Nat Rev Endocrinol. 2014;10:711-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 339] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 47. | Davey RJ, Howe W, Paramalingam N, Ferreira LD, Davis EA, Fournier PA, Jones TW. The effect of midday moderate-intensity exercise on postexercise hypoglycemia risk in individuals with type 1 diabetes. J Clin Endocrinol Metab. 2013;98:2908-2914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 48. | Gomez AM, Gomez C, Aschner P, Veloza A, Muñoz O, Rubio C, Vallejo S. Effects of performing morning vs afternoon exercise on glycemic control and hypoglycemia frequency in type 1 diabetes patients on sensor-augmented insulin pump therapy. J Diabetes Sci Technol. 2015;9:619-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 90] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 49. | Kime NH, Pringle A, Rivett MJ, Robinson PM. Physical activity and exercise in adults with type 1 diabetes: understanding their needs using a person-centered approach. Health Educ Res. 2018;33:375-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 50. | MacMillan F, Kirk A, Mutrie N, Moola F, Robertson K. Building physical activity and sedentary behavior support into care for youth with type 1 diabetes: patient, parent and diabetes professional perceptions. Pediatr Diabetes. 2016;17:140-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 51. | Roberts AJ, Mitrovich C, Yi-Frazier JP, Taplin CE. Feasibility of Routine Assessment of Exercise Knowledge and Safety in Youth With Type 1 Diabetes. Diabetes Educ. 2019;45:469-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 52. | Standl E, Owen DR. New Long-Acting Basal Insulins: Does Benefit Outweigh Cost? Diabetes Care. 2016;39 Suppl 2:S172-S179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 53. | Moser O, Yardley JE, Bracken RM. Interstitial Glucose and Physical Exercise in Type 1 Diabetes: Integrative Physiology, Technology, and the Gap In-Between. Nutrients. 2018;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 54. | Moser O, Riddell MC, Eckstein ML, Adolfsson P, Rabasa-Lhoret R, van den Boom L, Gillard P, Nørgaard K, Oliver NS, Zaharieva DP, Battelino T, de Beaufort C, Bergenstal RM, Buckingham B, Cengiz E, Deeb A, Heise T, Heller S, Kowalski AJ, Leelarathna L, Mathieu C, Stettler C, Tauschmann M, Thabit H, Wilmot EG, Sourij H, Smart CE, Jacobs PG, Bracken RM, Mader JK. Glucose management for exercise using continuous glucose monitoring (CGM) and intermittently scanned CGM (isCGM) systems in type 1 diabetes: position statement of the European Association for the Study of Diabetes (EASD) and of the International Society for Pediatric and Adolescent Diabetes (ISPAD) endorsed by JDRF and supported by the American Diabetes Association (ADA). Diabetologia. 2020;63:2501-2520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 123] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 55. | Chu L, Hamilton J, Riddell MC. Clinical management of the physically active patient with type 1 diabetes. Phys Sportsmed. 2011;39:64-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 56. | Yardley JE, Iscoe KE, Sigal RJ, Kenny GP, Perkins BA, Riddell MC. Insulin pump therapy is associated with less post-exercise hyperglycemia than multiple daily injections: an observational study of physically active type 1 diabetes patients. Diabetes Technol Ther. 2013;15:84-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 57. | Taplin CE, Cobry E, Messer L, McFann K, Chase HP, Fiallo-Scharer R. Preventing post-exercise nocturnal hypoglycemia in children with type 1 diabetes. J Pediatr 2010; 157: 784-8. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 58. | Franc S, Daoudi A, Pochat A, Petit MH, Randazzo C, Petit C, Duclos M, Penfornis A, Pussard E, Not D, Heyman E, Koukoui F, Simon C, Charpentier G. Insulin-based strategies to prevent hypoglycaemia during and after exercise in adult patients with type 1 diabetes on pump therapy: the DIABRASPORT randomized study. Diabetes Obes Metab. 2015;17:1150-1157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 59. | Colberg SR, Laan R, Dassau E, Kerr D. Physical activity and type 1 diabetes: time for a rewire? J Diabetes Sci Technol. 2015;9:609-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 60. | Allen N, Gupta A. Current Diabetes Technology: Striving for the Artificial Pancreas. Diagnostics (Basel). 2019;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 61. | Phillip M, Battelino T, Atlas E, Kordonouri O, Bratina N, Miller S, Biester T, Stefanija MA, Muller I, Nimri R, Danne T. Nocturnal glucose control with an artificial pancreas at a diabetes camp. N Engl J Med. 2013;368:824-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 285] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 62. | Kovatchev BP, Renard E, Cobelli C, Zisser HC, Keith-Hynes P, Anderson SM, Brown SA, Chernavvsky DR, Breton MD, Mize LB, Farret A, Place J, Bruttomesso D, Del Favero S, Boscari F, Galasso S, Avogaro A, Magni L, Di Palma F, Toffanin C, Messori M, Dassau E, Doyle FJ 3rd. Safety of outpatient closed-loop control: first randomized crossover trials of a wearable artificial pancreas. Diabetes Care. 2014;37:1789-1796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 145] [Cited by in RCA: 127] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 63. | Tagougui S, Taleb N, Molvau J, Nguyen É, Raffray M, Rabasa-Lhoret R. Artificial Pancreas Systems and Physical Activity in Patients with Type 1 Diabetes: Challenges, Adopted Approaches, and Future Perspectives. J Diabetes Sci Technol. 2019;13:1077-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 64. | Kordonouri O, Riddell MC. Use of apps for physical activity in type 1 diabetes: current status and requirements for future development. Ther Adv Endocrinol Metab. 2019;10:2042018819839298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 65. | Fleming GA, Petrie JR, Bergenstal RM, Holl RW, Peters AL, Heinemann L. Diabetes Digital App Technology: Benefits, Challenges, and Recommendations. A Consensus Report by the European Association for the Study of Diabetes (EASD) and the American Diabetes Association (ADA) Diabetes Technology Working Group. Diabetes Care. 2020;43:250-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 168] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee CH S-Editor: Fan JR L-Editor: Filipodia P-Editor: Li X