Published online Mar 15, 2020. doi: 10.4239/wjd.v11.i3.78
Peer-review started: August 21, 2019
First decision: October 13, 2019
Revised: November 21, 2019
Accepted: January 8, 2020
Article in press: January 8, 2020
Published online: March 15, 2020
Processing time: 191 Days and 4.9 Hours
Diabetic foot ulceration (DFU) is the prime health concern globally. It accounts for the major burden related to disease mortality and morbidity and economic cost. The timely and early recognition of the DFU can help present its occurrence and improve clinical outcomes.
To evaluate interrelationships between foot ulcers, risk factors, and antibiotic resistance among diabetic patients having ulcers in their foot.
The databases such as PubMed, ERIC, Medline, and Google Scholar were extensively used for the extraction of studies. The selected studies were published within the time-period of 2014-2018. Ten studies were selected, which were found to be completely relevant to the current study.
The prevalence of diabetic foot ulcers among the population was evaluated, and the associated risk factors with its prevalence. Moreover, few studies also reported on the bacteria that are found to be most prevailing among diabetic patients. A narrative discussion was drawn through this analysis, which was used to highlight the specific area of research through selected studies, extraction of the significant information that matched with the topic of research, and analysis of problem through the findings of the selected articles. The results helped in assessing significant knowledge regarding the risk factors of diabetic foot ulcers and the role of antimicrobial resistant in its treatment.
The gram-negative bacteria were found to be the most common reason for diabetic foot ulcers. The study only included 10 studies that are not sufficient to produce generalized results, and no information was reported on the tests required to analyze antimicrobial susceptibility that can guide clinicians to propose better and sound treatment plans. It is evident that most study results depicted that the most common risk factors were found to be hypertension and neuropathy.
Core tip: The study has investigated relationship between foot ulcer, risk factors and antibiotic resistance among diabetic patients having ulcers in their foot. The results demonstrated that gram-negative bacteria are more responsible for the occurrence of diabetic foot ulcers. Antimicrobial sensitivity needs to be controlled by prescribing effective treatment plans to patients. Whereas, the overuse of antibiotics can negatively influence the health of patients.
- Citation: Zubair M. Prevalence and interrelationships of foot ulcer, risk-factors and antibiotic resistance in foot ulcers in diabetic populations: A systematic review and meta-analysis. World J Diabetes 2020; 11(3): 78-89
- URL: https://www.wjgnet.com/1948-9358/full/v11/i3/78.htm
- DOI: https://dx.doi.org/10.4239/wjd.v11.i3.78
With the prevalence of diabetes, a number of new complications related to the health of patients have been witnessed in the recent decades. On top of it, diabetic foot infection is a severe complication being faced by a large number of diabetic patients consisting of lesions in the deep tissues[1,2]. Foot complications are the major cause of mortality and morbidity among diabetic patients leading to increased health care cost[3,4]. Moreover, foot wounds are the most common diabetes-related complication often leading to hospitalization. Around 15% of diabetic patients experience foot ulcer once in their lifetime[5,6].
The pathophysiology of the diabetic foot is complex; however, the infection is generally caused by the disturbance in the host such as; neuropathy, immunopathy and arteriopathy and other factors related to pathogen[7]. The development of ulcer on the foot is related to the trauma that disrupts the protective skin envelope on the foot, leading to the bacterial colonization of the underlying subcutaneous tissues[8]. However, infection is caused by the overgrowth of microorganisms in these areas leading to the destruction of tissues. Therefore, a foot ulcer might result in the amputation of the lower limb due to healing failure[5].
The most common type of risks that leads to foot ulcers are diabetic neuropathy and peripheral vascular disorders. The most common type of neuropathy is diabetic neuropathy, developing in around 50% of Type 1 and Type 2 diabetic patients[9,10]. The risk factors of diabetic foot ulcer include age[10], duration of diabetes[10,11], male gender[11,12], poor glycemic control[13], peripheral vascular disease[12,14], diabetic retinopathy[11,12], and nephropathy[7,15].
Adding to the challenges faced by the clinicians in treating diabetic foot ulcers is the antibiotic resistance, which restricts the choice of antibiotics for the treatment process. In this regard, a study conducted by Xie et al[16] explained the bacterial profile and antibiotic resistance in patients with diabetic foot ulcers. The main focus of the study was on the differences among different Wagner’s Grades, ulcer types and Infectious Diseases Society of America/International Working Group on the Diabetic Foot Grades. To support this, McArdle et al[17] also conducted a study to evaluate the antibiotic resistance in foot ulceration. A cohort of literature has been dedicated to evaluate the antibiotic resistance in patients with diabetic foot ulcers. The studies have also suggested various recommendations including; clinicians must pay significant attention to the antibiotic resistance patterns of common pathogens in their areas[18], reconsidering antibiotic choice[19,20] and curtailing the prevention of the development of drug resistant strains[21,22]. Based on the literature present on the topic of research, the current meta-analysis is aimed at discussing the prevalence of foot diseases, risk factors and antibiotic resistance among patients with diabetic foot ulcers. Moreover, the current study will help in providing recommendations to address the issues related to antibiotic resistance among patients with diabetic foot ulcers.
The present review aims to discuss the prevalence and the interrelationship between the risk factors, foot diseases and antibiotic resistance among patients with diabetic foot ulcer. The following meta-analysis highlights the recommendations and methods discussed in the previous studies to cure diabetic foot ulcer. Moreover, the current study also analyzes the prevalence of risk factors leading to diabetic foot ulcer. The research questions for this study are as follows: (1) Is diabetic foot ulcer more prevalent among the population below the poverty line and those living in developing countries? (2) What are the risk factors which contribute to the development of foot ulcer among diabetic patients? (3) Is antibiotic resistance a major factor causing increase in diabetic foot ulcer? and (4) What are the possible recommendations to address the prevalence of diabetic foot ulcer and antibiotic resistance?
To retrieve the qualitative and most authentic studies, the databases such as: PubMed, ERIC, Medline, and Google Scholar were extensively used for the extraction of studies. The inclusion and exclusion criteria were strictly applied to all the selected studies. The inclusion criteria were based on the complete relevance of the selected studies to the topic of research, time-period of the selected studies (2014-2018) and the limitation that selected studies must be a review article. Some common keywords used for the literature survey included; prevalence of diabetic foot ulcer, risk factors of diabetic foot ulcer, antibiotic resistance of diabetic foot ulcer, nephropathy and diabetic foot ulcer, and diabetic foot ulcer. The studies which did not meet the inclusion criteria were excluded from the study. Moreover, essays, reports, and blogs were also excluded due to reduced reliability and authenticity.
Meta-analysis was conducted to review the studies that were found relevant with the topic of research. A narrative discussion was drawn through this analysis, which was used to highlight the specific area of research through selected studies, extraction of the significant information that matched with the topic of research and analysis of problem through the findings of the selected articles.
Based on the keywords, the aforementioned platforms were extensively researched, and 2150 abstracts were extracted for the study. A two-stage investigation of the selected abstracts was carried out with the help of a professional and an investigator. With regards to this, the older version of the studies was excluded due to reduced reliability and authenticity and cross-sectional, prospective and retrospective studies were included in the study. The abstracts chosen for the study discussed the prevalence, risk factors and antibiotic resistance in foot ulcers among diabetic patients.
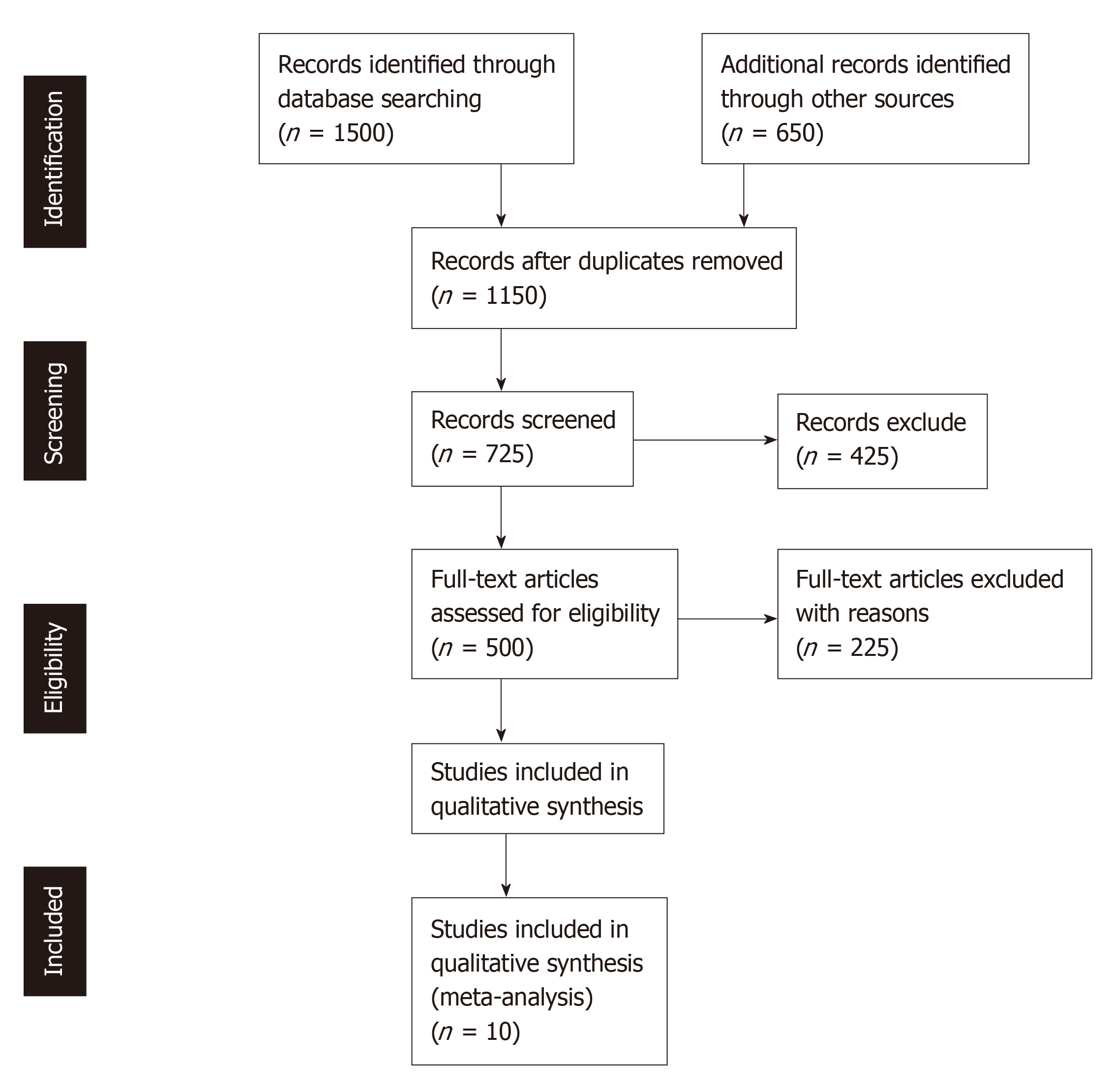
After the first application of inclusion criteria, the number of abstracts reduced to 725 with the elimination of 1425 abstracts. The inclusion criteria were again applied which reduced the number of articles to 125 after the exclusion of 1300 abstracts that were found irrelevant with the topic of study. The remaining 125 articles were again passed through a phase of strict scrutiny and were evaluated on the basis of conceptual framework to assure the direction and significance of the study. In the next step, only 10 studies were selected which were found to be completely relevant with the current study. Pictorial depiction of literature survey has been demonstrated in Figure 1.
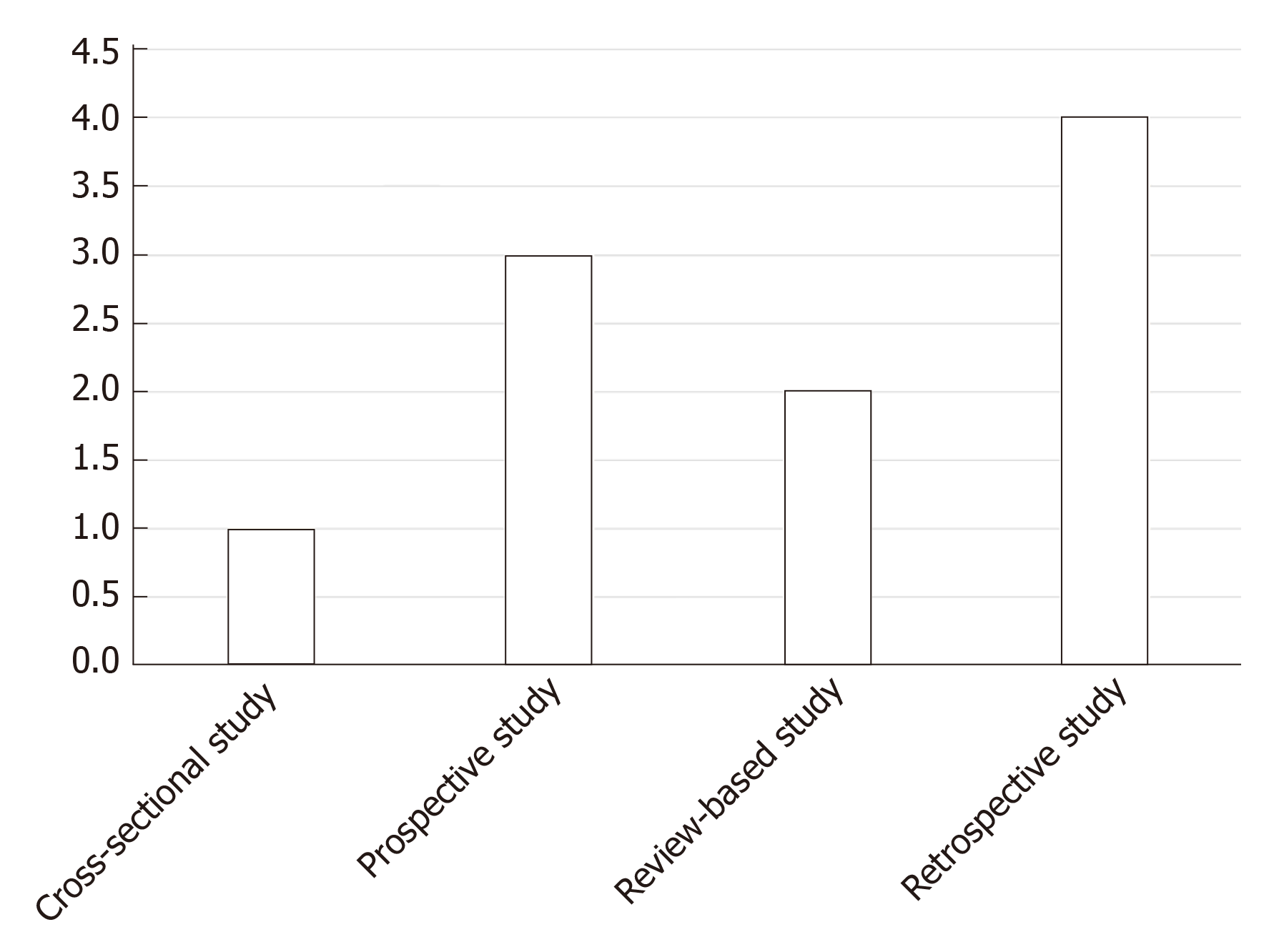
A total of 10 studies were selected for the systematic literature survey which included information regarding the topic of research. The prevalence of diabetic foot ulcers among the population was evaluated and the associated risk factors with its prevalence. Moreover, few studies also reported on the bacteria that are found to be most prevailing among diabetic patients. Furthermore, data regarding the antimicrobial resistance offered by these bacteria was also mentioned in the study. Different types of approaches used in the selected studies were summarized in the graphical form (Figure 2); whereas, Table 1 has illustrated the characteristics of included studies that include; study type, mean age, male and female ratio, diabetes duration, Hemoglobin A1c percentage, ulcer description, and follow-up months. In Hemoglobin A1c, A1c percentage measures the quantity of the sugar present in the blood’s hemoglobin protein. It measures how well the sugar in the blood is controlled. Table 2 has summarized the study objective, methodology used, and study outcomes of the included studies. Whereas, Table 3 has provided description of the included studies related to the causative agents from diabetic foot ulceration (DFU).
| Ref. | Study type | Male: Female ratio | Type 2 diabetes mellitus/Type 1 diabetes | Duration of Diabetes | HbA1c% | Ulcer description | Follow-up months |
| Quilici et al[21] | Cross-sectional study | 68 males and 32 females | T2DM | 22% had for less than five yr; 24% had from 5-10 yr; 17% had from 10-15 yr; 16% had from 15-20 yr; 21% had for >20 yr | - | 75% patients had Grade 4 ulcers; 20% had Grade 3 ulcers; 5% had Grade 2 ulcers | - |
| Commons et al[26] | Prospective study | 60% male and 40% females | All patients had T1DM, except of 7 patients | - | Median value was 8.8% | Diabetic patients with ulcers or foot infections were referred | 14 mo |
| Barwell et al[28] | Combination of literature review | - | T1DM and T2DM | - | - | Standardized using validated classifications schemes such as the University of Texas rating, SINBAD or IWGDF PEDIS | - |
| Roth-Albin et al[24] | Retrospective cohort study | 67.9% were males | - | - | - | Ulcer sizes > 1 cm2 | 52 wk |
| Fitzgerald et al[30] | Retrospective study | 4:4 | - | Average disease duration 22 yr | - | Active foot-ulcer with a wound swab taken | 15 mo |
| Kathirvel et al[22] | Retrospective study | 74.6% males and 25.33% females | T2DM | < 5 yr - 40%; 5-10 yr - 34%; 10-15 yr - 17%; 15-20 yr - 7.3%; > 20 yr - 1.3% | 6%-7% | Categorized into necrotic/non-necrotic; ulcers based on signs of infection | - |
| Xie et al[16] | Hospital-based retrospect study | 230 males and 158 females | T2DM | - | - | Severity of ulcer was assessed by Wagner-Meggit classification system | - |
| Dwedar et al[41] | Observational prospective study | 48 males (57%) and 32 females (43%) | - | 5-32 yr | - | Graded according to Wagner’s grade | - |
| Abbas et al[45] | Literature review | - | T2DM | - | - | Classified on the basis of wound debridement, pressure off-loading, glycemic control, surgical interventions, and occasionally other adjunctive measures | - |
| Oliveira et al[46] | Epidemiological, retrospective and descriptive study | 27 males and 30 females | - | - | - | Infected ulceration was associated with germs present in the community | - |
| Ref. | Methodology/Approach | Findings | Outcome |
| Quilici et al[21] | Cross-sectional study | Prevalence of amputation was 42% due to the previous use of antimicrobials. Risk of amputation was 26% for patients who had less compliant with the diabetes treatment | Highlight factors for the management patients with diabetic foot infection |
| Commons et al[26] | Prospective study was conducted among patients with diabetic foot infections, enrolled in Royal Darwin Hospital, were selected. The relation with Pseudomonas aeruginosa and methicillin resistant Staphylococcus aureus was also determined | P. aeruginosa and Methicillin resistant S. aureus infections were cured by long-term courses of antibiotics and increased hospital stay | Prevalence of diabetic foot ulcer is directly and significantly related to the best bed days |
| Barwell et al[28] | A literature review was conducted | Antibiotic and antimicrobial resistance of Gram positive organisms occurred as a main challenge in the treatment of diabetic foot infection | Provides guideline as empirical evidence to support clinicians |
| Roth-Albin et al[24] | Retrospective cohort study | 35 out of 40 patients were healed in 52 weeks. 7.1% underwent amputation and 8.9% died before receiving any kind of treatment | Healing rates significantly improved by proper and continued care |
| Fitzgerald et al[30] | Retrospective exploratory study | Diabetes and Cardiovascular disease/peripheral-vascular disease was identified in 2 and 6 patients, respectively. 28 patients had foot ulcers and RA. Inflicted patients were treated with antirheumatic drugs and steroids | Inaccurate diagnosis of ulcer infection leads to failure of microbiological analysis |
| Kathirvel et al[22] | 150 patients’ clinical examination, clinical history and microbiological profile were prospectively examined | 99 patients were isolated from MDRO. MDRO risk factors include; previous antibiotic usage, retinopathy, polymicrobial culture, presence of ulcer, antibiotic usage, ulcer size, history of amputation, peripheral vascular disease, neuropathy, and necrotic ulcer | MDRO prevalence was high among diabetic patients with foot ulcers |
| Xie et al[16] | Retrospective study was conducted using 207 bacteria from diabetic foot infections. Microbial and clinical information was also collected | Gram negative bacteria were found to be more as compared to gram positive bacteria with, Staphylococcus and Enterobacteriaceae to be the most dominant | The antibiotic sensitivity and bacterial profile of diabetic foot ulcers varied with their types and grades |
| Dwedar et al[41] | 80 patients with diabetic foot infections were prospectively studied | Gram negative bacteria were more common. Vancomycin was found to be the best against gram-positive bacteria; whereas, colistin, imipenem and amikacin were effective against gram-negative bacteria | Knowledge regarding antibiotic sensitivity is required for future treatment of diabetic foot ulcers |
| Abbas et al[45] | Non-systematic research | Antibiotic therapy is necessary for several clinically infected wounds | Antibiotic therapies should be used for treatment |
| Oliveira et al[46] | Descriptive, retrospective and epidemiological study was used | 65% of cases suffered amputations. Staphylococci was the most common bacteria type. Three patients were found to be enterobacteria and second was, Staphylococci | Clindamycin and cephalexin were most resistant to bacteria |
| Ref. | Total no of enrolled patients | Number of patients with isolated strains/ with multiple strains n(%) | Number of microorganisms, n (%) | ||||||||||||
| Gram positive | Gram negative | Fungus | |||||||||||||
| Aerobes | Ananerobes | Aerobes | Ananerobes | ||||||||||||
| Methicillin-sensitive Staphylococcus aureus (MSSA) | Methicillin-resistant Staphylococcus aureus. (MRSA) | Other Staphyloccus sp (Staphylococcus species) | Streptocccus sp | Enterococcus sp | Other Gram positive | Enterobacteriaceac members | Pseudomonas sp | Acinetobacter sp | Other gram negative sp | ||||||
| Quilici et al[21] | 100 | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Commons et al[26] | 177 | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Barwell et al[28] | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Roth-Albin et al[24] | 40 | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Fitzgerald et al[30] | 28 | - | +++ | - | - | - | - | - | ++ | - | - | - | - | - | - |
| Kathirvel et al[22] | 150 | - | - | - | - | - | - | 17.9% | - | - | - | - | 69.89% | - | - |
| Xie et al[16] | 405 | 95.8% | 43.2%, 41/95 | - | 65.2%, 62/95 | - | 20.0%, 19/95 | 45.9%, 95/207 | - | 73.2%, 82/112 | - | - | 54.1%, 112/207 | - | 10.7% |
| Dwedar et al[41] | 80 | 77 | 11.4% | (10.1% | 46.8% | - | 27.7% | - | - | 10.8% | - | 56.08% | 8.1% | - | |
| Abbas et al[45] | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Oliveira et al[46] | 66 | - | 22.7% | - | 4.5% | - | - | - | - | - | - | - | - | - | - |
Quilici et al[21] measure the risk factors that are involved in the amputation process for diabetic patients hospitalized due to foot infections. One hundred patients were selected who were suffering complications related to diabetes infections in their lower limbs. Multiple Cox regression analysis was used to analyze the data collected from the patients. The prevalence of several factors was evaluated, among which, hypertension and neuropathy were found to be the prevalent risk factors. The results conducted from Morisky test showed that 42% of patients were on the risk of progression to amputation due to the previous use of microbials. Also, the results suggested that those patients who did not comply with diabetes treatment were on 26% more risk of amputation. Such that, it can be concluded that these risk factors can significantly increase the risk of amputation among patients. The knowledge of these risk factors will help practitioners to develop treatment plans that can effectively reduce the risk of amputation among diabetic patients. Another study conducted by Pickwell et al[23] reported a 28% ratio of patients that underwent amputation.
Roth-Albin et al[24] assess the advanced wound care for diabetic foot ulcers. A retrospective cohort design was followed which included adult patients suffering from diabetic foot ulcers. The delayed risks of diabetic foot ulcers were evaluated in the study. The results showed that, only 35 out of 40 patients were able to heal through all diabetic foot ulcers in the period of 52 wk. The factors influencing the healing process of diabetic foot ulcers include peripheral vascular disease, chronic ulcers, multiple ulcers, and ulcer sizes. Furthermore, the results showed that the rate of unadjusted healing rate of recurrent ulcers was more than other factors. Such that, the study concluded that continued self-care, advanced wound care and outpatient has significant influence on the healing of diabetic foot infections. Jeffcoate et al[25] also emphasized on improving self-care among patients to enhance the outcomes of diabetic health infections.
Commons et al[26] appraise the high burden of diabetic foot infections in Australia. The study highlighted that the ratio of diabetic patients is increasing all over the world leading to amputations in worst cases. Foot infections were reported as the common cause of amputation among patients with foot ulcers. All the patients with diabetic foot infections enrolled in Royal Darwin Hospital were included in the study. The results showed that indigenous patients were found to be more subjected to amputations as compared to non-indigenous patients. Furthermore, the study highlighted P. aeruginosa or Methicillin resistant S. aureus as one of the leading infections that required longer hospital stay and antibiotic courses. Another study conducted by O’Rourke et al[27] also reported that 52% of patients in Far North Queensland were indigenous who went through amputation. Such that, results concluded from these studies emphasize on increasing self-care and management of foot care, which can lead to reduction in major amputation.
Barwell et al[28] reported on diabetic foot infections and recommendation related to good practice and antibiotic therapy. The study reported that diabetic foot infections can cause mortality, morbidity and a burden of economic cause on patients. According to the study, tissue sampling at the very beginning can help in overcoming the increased cost of treatment and long use of antibiotics. Long use of certain antibiotic can make the resistant toward it, thus, making the infection more complicated to treatment. A literature review was carried out to evaluate these aspects, and expert discussion was also considered. The results reported that gram positive organisms are the most common pathogens that induce foot infections. The study also reported that there are several challenges present regarding antibiotic availability and antibiotic resistance. The study concluded that the use of alternative oral agents and outpatient antibiotics can help in increasing diabetic foot care. Kang et al[29] also reported that long-term use of antibiotics makes the patients with diabetic foot ulcers resistant to the antibiotics.
Fitzgerald et al[30] conducted a study to evaluate the prevalence and microbiological characteristics of clinically infected foot-ulcers in patients with rheumatoid arthritis (RA). A retrospective cohort design was followed to collect data from the patients with arthritis. The patients attending a clinic aimed for the treatment of rheumatology and wound swab data was collected from the patients suffering from clinical infection. The results showed that only 28 patients were identified who were suffering from both foot infection and RA. Among these patients, only 8 had wound swabs taken and clinical infection. The study concluded that microbiological analysis has failed to isolate the pathogens. The rationale behind this failure might be due to inappropriate diagnosis or issue with tissue sampling. The study highlighted on the importance of conducting more research for infection diagnosis, processing and wound sampling. On the other hand, Grigoropoulou et al[31] defined the importance of microbiological culture for the treatment of foot infections. The study emphasized that proper knowledge of the severity of infection can lead to the development of adequate treatment strategies.
Kathirvel et al[22] discussed risk factors for diabetic foot infections with multidrug-resistant microorganisms. The study included a total of 150 patients who were diagnosed with foot ulcers. A detailed and thorough examination of the clinical history and examination of the patients with foot ulcer was carried out. Microbiological analysis of all the patients was studied. The results showed that multidrug-resistant organisms were isolated from 99 out of 150 patients. Multidrug-resistant organisms were found to be isolated organisms. On the other hand, the risk factors of diabetic foot ulcers were examined to be peripheral vascular disease, retinopathy, polymicrobial culture, and neuropathy. Moreover, the study predicted that the rate of multidrug-resistant organisms was reaching an alarming rate. Therefore, the practitioners are advised to develop proper treatment plans that reduce the rate of multidrug-resistant organisms. Other studies also emphasized on the interventions for the management of foot infection among diabetic patients[32-35].
Xie et al[16] also evaluated bacterial profile and antibiotic resistance in patients with diabetic foot ulcer. The study included a sample of 207 bacteria from a total of 117 diabetic foot infections. The result stated that gram-negative bacteria were found to be in higher proportion as compared to gram-positive bacteria. Moreover, Staphylococcus and Enterobacteriaceae were found to be the most prevalent microorganisms among sample. Thus, the study recommended clinicians to examine the antibiotic resistance pattern of common pathogens. Furthermore, Perim et al[36] also confirmed the high prevalence of multidrug-resistant pathogens in DFUs. Moreover, other studies focused on evaluating the antibiotic susceptibility patterns of isolates to develop effective treatment plans[37-40].
Dwedar et al[41] also measure the microbiological causes of diabetic foot infections and their associated antibiotic resistance patterns. A total of 80 patients suffering from diabetic foot infections were selected as the sample of the study. The sterile swabs from the sample were collected along with thorough examination of the antimicrobial susceptibility through several susceptibility tests. The results concluded that gram-negative bacteria were more isolated as compared to gram-positive bacteria. The most common isolates were found to be Staphylococcus aureus, Escherichia coli, Proteus mirabilis, Pseudomonas spp, and Methicillin resistant Staphylococcus aureus. The study concluded that gram-negative bacteria are highly responsible for causing diabetic foot ulcers. Moreover, the information on the antibiotic sensitivity help clinicians to prescribe drugs that are efficient for the treatment of diabetic ulcers. Other studies also emphasized on attaining the knowledge of antibiotic sensitivity among patients with diabetic ulcers[42-44].
Abbas et al[45] evaluate the role of antibiotics in treating infection among diabetic foot ulcers, not to heal wounds. The study stated that antibiotic therapy is used for clinically infected wounds and not for uninfected ulcers. However, the study described that often clinicians fail to prescribe drugs related to such conditions. Such mistakes by clinicians can impose negative impact on the overall health of the patient. Overuse of antibiotics can make the patient more prone to the specific drug; thus, reducing its effectiveness. To this end, the study concluded that clinicians should thoroughly examine the condition of patients and should limit prescribing antibiotics for uninfected foot wounds. On the other hand, other studies also emphasized on studying the antimicrobial resistance profiles of patients[46-49].
In conclusion, The ratio of diabetic foot infections among patients is increasing all over the world; thus, resulting in increased amputation rates. The study was aimed to evaluate the prevalence and interrelationships of foot diseases, associated risk factors and antibiotic resistance in patients with diabetic foot ulcers. The systematic review helped in assessing significant knowledge regarding the risk factors of diabetic foot ulcers and the role of antimicrobial resistant in its treatment. Thus, it can be concluded that gram-negative bacteria are more responsible for the occurrence of diabetic foot ulcers. Moreover, the risk factors were identified to be hypertension, neuropathy, etc. On the other hand, the study also reported that antimicrobial sensitivity needs to be controlled by prescribing effective treatment plans to patients. Overuse of antibiotics can negatively influence the health of patients. Therefore, clinicians are addressed to study the antimicrobial pattern among patients before prescribing any treatment plan.
Despite of the cohort of information provided in the following study, it has few limitations. The study only included 10 studies which are not sufficient to produce generalized results; therefore, the researchers should include a large number of studies in the future work. Moreover, no information was reported on the tests required to analyze antimicrobial susceptibility that can guide clinicians to propose better and sound treatment plans. To this end, the researchers were advised to include these aspects in future studies to address the issues related to the diagnosis of patients.
Globally, the occurrence of diabetic foot ulceration (DFU) reported as a significant health concern which calls for early prevention and diagnosis.
This study would assist in setting out relevant guidelines for reducing the incidence of DFU and overcome the resistance among patients for its treatment.
The main objectives were to examine the interrelationships between foot ulcers, risk factors, and antibiotic resistance among diabetic patients having ulcers in their foot.
A systematic and meta-analysis method is adopted for providing comprehensive insights on the DFU prevalence, risk factors as well as its resistance.
The research findings showed an increased prevalence of gram-negative bacteria among the DFU cases.
The review concludes hypertension and neuropathy as the major risk factors among DFU patients.
The review highlights that antimicrobial susceptibility can be considered for attaining better treatment outcomes.
The author is very thankful to all the associated personnel in any reference that contributed in/for the purpose of this research.
Manuscript source: Unsolicited manuscript
Specialty type: Endocrinology and metabolism
Country of origin: Saudi Arabia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mrzljak A S-Editor: Dou Y L-Editor: A E-Editor: Ma YJ
| 1. | Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med. 2017;49:106-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 666] [Cited by in RCA: 1060] [Article Influence: 117.8] [Reference Citation Analysis (6)] |
| 2. | Datta P, Chander J, Gupta V, Mohi GK, Attri AK. Evaluation of various risk factors associated with multidrug-resistant organisms isolated from diabetic foot ulcer patients. J Lab Physicians. 2019;11:58-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Diabetes Canada Clinical Practice Guidelines Expert Committee. Embil JM, Albalawi Z, Bowering K, Trepman E. Foot Care. Can J Diabetes. 2018;42 Suppl 1:S222-S227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Bowling FL, Boulton AJ. Diabetic Foot. In: Bonora E., DeFronzo R. Diabetes Complications, Comorbidities and Related Disorders. Endocrinology. Springer, Cham. 2018;355-376. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Yazdanpanah L, Nasiri M, Adarvishi S. Literature review on the management of diabetic foot ulcer. World J Diabetes. 2015;6:37-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 291] [Cited by in RCA: 343] [Article Influence: 31.2] [Reference Citation Analysis (18)] |
| 6. | Tchero H, Kangambega P, Noubou L, Becsangele B, Fluieraru S, Teot L. Antibiotic therapy of diabetic foot infections: A systematic review of randomized controlled trials. Wound Repair Regen. 2018;26:381-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Spichler A, Hurwitz BL, Armstrong DG, Lipsky BA. Microbiology of diabetic foot infections: from Louis Pasteur to ‘crime scene investigation. BMC Medicine. 2015;13:2. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 92] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 8. | Padros C, Cantadori E, Fuste E, Vinuesa T, Vinas M. Diabetic foot infection in spain. Acta Medica Mediterr. 2018;3:651-656. [DOI] [Full Text] |
| 9. | Shahbazian H, Yazdanpanah L, Latifi SM. Risk assessment of patients with diabetes for foot ulcers according to risk classification consensus of International Working Group on Diabetic Foot (IWGDF). Pak J Med Sci. 2013;29:730. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (5)] |
| 10. | Al-Rubeaan K, Al Derwish M, Ouizi S, Youssef AM, Subhani SN, Ibrahim HM, Alamri BN. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015;10:e0124446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 234] [Cited by in RCA: 229] [Article Influence: 20.8] [Reference Citation Analysis (1)] |
| 11. | Almobarak AO, Awadalla H, Osman M, Ahmed MH. Prevalence of diabetic foot ulceration and associated risk factors: an old and still major public health problem in Khartoum, Sudan? Ann Transl Med. 2017;5:340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 12. | Jupiter DC, Thorud JC, Buckley CJ, Shibuya N. The impact of foot ulceration and amputation on mortality in diabetic patients. I: From ulceration to death, a systematic review. Int Wound J. 2016;13:892-903. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 248] [Cited by in RCA: 225] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 13. | Porselvi A, Shankar MS, Lakshmi KS, Sankar V. A retrospective qualitative study on current diabetic foot ulcer management and discussion on extended role of clinical pharmacist. Marmara J Pharm. 2017;21:412-418. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Smith-Strøm H, Iversen MM, Igland J, Østbye T, Graue M, Skeie S, Wu B, Rokne B. Severity and duration of diabetic foot ulcer (DFU) before seeking care as predictors of healing time: A retrospective cohort study. PLoS One. 2017;12:e0177176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 15. | Meloni M, Giurato L, Izzo V, Stefanini M, Gandini R, Uccioli L. Risk of contrast induced nephropathy in diabetic patients affected by critical limb ischemia and diabetic foot ulcers treated by percutaneous transluminal angioplasty of lower limbs. Diabetes Metab Res Rev. 2017;33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Xie X, Bao Y, Ni L, Liu D, Niu S, Lin H, Li H, Duan C, Yan L, Huang S, Luo Z. Bacterial Profile and Antibiotic Resistance in Patients with Diabetic Foot Ulcer in Guangzhou, Southern China: Focus on the Differences among Different Wagner's Grades, IDSA/IWGDF Grades, and Ulcer Types. Int J Endocrinol. 2017;2017:8694903. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 17. | McArdle CD, Lagan KM, McDowell DA. Effects of pH on the Antibiotic Resistance of Bacteria Recovered from Diabetic Foot Ulcer Fluid An In Vitro Study. J Am Podiatr Med Assoc. 2018;108:6-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Hassan MA, Tamer TM, Rageh AA, Abou-Zeid AM, Abd El-Zaher EHF, Kenawy ER. Insight into multidrug-resistant microorganisms from microbial infected diabetic foot ulcers. Diabetes Metab Syndr. 2019;13:1261-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 19. | Nur AHH, Intan NS, Syafinaz AN, Zalinah A, Lailatul MA, Devnani AS. Clinical presentation and micro-organisms sensitivity profile for diabetic foot ulcers: a pilot study. Med J Malaysia. 2015;70:182-187. |
| 20. | Kurup R, Ansari AA, Singh J. A review on diabetic foot challenges in Guyanese perspective. Diabetes Metab Syndr. 2019;13:905-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Quilici MT, Del Fiol Fde S, Vieira AE, Toledo MI. Risk Factors for Foot Amputation in Patients Hospitalized for Diabetic Foot Infection. J Diabetes Res. 2016;2016:8931508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Kathirvel M, Jayarajan J, Sivakumar A, Govindan V. Risk factors for the diabetic foot infection with multidrug-resistant microorganisms in South India. Int J Surg. 2018;5:675-682. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Pickwell K, Siersma V, Kars M, Apelqvist J, Bakker K, Edmonds M, Holstein P, Jirkovská A, Jude E, Mauricio D, Piaggesi A, Ragnarson Tennvall G, Reike H, Spraul M, Uccioli L, Urbancic V, van Acker K, van Baal J, Schaper N. Predictors of lower-extremity amputation in patients with an infected diabetic foot ulcer. Diabetes Care. 2015;38:852-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 136] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 24. | Roth-Albin I, Mai SHC, Ahmed Z, Cheng J, Choong K, Mayer PV. Outcomes Following Advanced Wound Care for Diabetic Foot Ulcers: A Canadian Study. Can J Diabetes. 2017;41:26-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Jeffcoate WJ, Vileikyte L, Boyko EJ, Armstrong DG, Boulton AJM. Current Challenges and Opportunities in the Prevention and Management of Diabetic Foot Ulcers. Diabetes Care. 2018;41:645-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 296] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 26. | Commons RJ, Robinson CH, Gawler D, Davis JS, Price RN. High burden of diabetic foot infections in the top end of Australia: An emerging health crisis (DEFINE study). Diabetes Res Clin Pract. 2015;110:147-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 27. | O'Rourke S, Steffen C, Raulli A, Tulip F. Diabetic major amputation in Far North Queensland 1998-2008: what is the Gap for Indigenous patients? Aust J Rural Health. 2013;21:268-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Barwell ND, Devers MC, Kennon B, Hopkinson HE, McDougall C, Young MJ, Robertson HMA, Stang D, Dancer SJ, Seaton A, Leese GP; Scottish Diabetes Foot Action Group. Diabetic foot infection: Antibiotic therapy and good practice recommendations. Int J Clin Pract. 2017;71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 29. | Kang WJ, Shi L, Shi Y, Cheng L, Ai HW, Zhao WJ. Analysis on distribution, drug resistance and risk factors of multi drug resistant bacteria in diabetic foot infection. Biomed Res. 2018;28:10186-10190. |
| 30. | Fitzgerald P, Siddle HJ, Backhouse MR, Nelson EA. Prevalence and microbiological characteristics of clinically infected foot-ulcers in patients with rheumatoid arthritis: a retrospective exploratory study. J Foot Ankle Res. 2015;8:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Grigoropoulou P, Eleftheriadou I, Jude EB, Tentolouris N. Diabetic Foot Infections: an Update in Diagnosis and Management. Curr Diab Rep. 2017;17:3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 32. | Peters EJ, Lipsky BA, Aragón-Sánchez J, Boyko EJ, Diggle M, Embil JM, Kono S, Lavery LA, Senneville E, Urbančič-Rovan V, Van Asten SA, Jeffcoate WJ; International Working Group on the Diabetic Foot. Interventions in the management of infection in the foot in diabetes: a systematic review. Diabetes Metab Res Rev. 2016;32 Suppl 1:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 33. | Edmonds M, Lázaro-Martínez JL, Alfayate-García JM, Martini J, Petit JM, Rayman G, Lobmann R, Uccioli L, Sauvadet A, Bohbot S, Kerihuel JC, Piaggesi A. Sucrose octasulfate dressing versus control dressing in patients with neuroischaemic diabetic foot ulcers (Explorer): an international, multicentre, double-blind, randomised, controlled trial. Lancet Diabetes Endocrinol. 2018;6:186-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 148] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 34. | Gariani K, Lebowitz D, von Dach E, Kressmann B, Lipsky BA, Uçkay I. Remission in diabetic foot infections: Duration of antibiotic therapy and other possible associated factors. Diabetes Obes Metab. 2019;21:244-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 35. | Wang C, Guo M, Zhang N, Wang G. Effectiveness of honey dressing in the treatment of diabetic foot ulcers: A systematic review and meta-analysis. Complement Ther Clin Pract. 2019;34:123-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 36. | Perim MC, Borges Jda C, Celeste SR, Orsolin Ede F, Mendes RR, Mendes GO, Ferreira RL, Carreiro SC, Pranchevicius MC. Aerobic bacterial profile and antibiotic resistance in patients with diabetic foot infections. Rev Soc Bras Med Trop. 2015;48:546-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 37. | Sekhar M S, M K U, Rodrigues GS, Vyas N, Mukhopadhyay C. Antimicrobial susceptibility pattern of aerobes in diabetic foot ulcers in a South-Indian tertiary care hospital. Foot (Edinb). 2018;37:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 38. | Kaimkhani GM, Siddiqui AA, Rasheed N, Rajput MI, Kumar J, Khan MH, Nisar S, Mustafa S, Yaqoob U. Pattern of Infecting Microorganisms and Their Susceptibility to Antimicrobial Drugs in Patients with Diabetic Foot Infections in a Tertiary Care Hospital in Karachi, Pakistan. Cureus. 2018;10:e2872. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Bello OO, Oyekanmi EO, Kelly BA, Mebude OO, Bello TK. Antibiotic Susceptibility Profiles of Bacteria from Diabetic Foot Infections in Selected Teaching Hospitals in Southwestern Nigeria. Int Ann Sci. 2018;4:1-3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Babu S. Antibiotic Susceptibility Pattern of Pseudomonas aeruginosa Isolates from Wound Infections in a Tertiary Care Centre in South Kerala, India. J Crit Care Med. 2018;3:30. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 41. | Dwedar R, Ismail, DK, Abdulbaky A. Diabetic foot Infection: Microbiological Causes with Special Reference to their Antibiotic Resistance Pattern. Egypt J Med Microbiol. 2015;38:1-8. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Mehta VJ, Kikani KM, Mehta SJ. Microbiological profile of diabetic foot ulcers and its antibiotic susceptibility pattern in a teaching hospital, Gujarat. International Journal of Basic. Clin Pharm. 2017;3:92-95. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 43. | Lakshmi BV, Bindhu H, Sudhakar M, Apoorva G, Uhasri J, Pradeep M, Sahaja D. Diabetic Foot Ulcers And Biofilm Formation. World J Pharm Res. 2019;8:640-650. [DOI] [Full Text] |
| 44. | Sari R, Apridamayanti P, Puspita ID. Sensitivity of Escherichia coli Bacteria Towards Antibiotics in Patient with Diabetic Foot Ulcer. Pharm Sci Res. 2018;5:19-24. |
| 45. | Abbas M, Uçkay I, Lipsky BA. In diabetic foot infections antibiotics are to treat infection, not to heal wounds. Expert Opin Pharmacother. 2015;16:821-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 101] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 46. | Oliveira AFD, Oliveira Filho HD. Microbiological species and antimicrobial resistance profile in patients with diabetic foot infections. J Vasc Bras. 2014;13:289-293. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 47. | Kwon KT, Armstrong DG. Microbiology and Antimicrobial Therapy for Diabetic Foot Infections. Infect Chemother. 2018;50:11-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 73] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 48. | Yarbrough ML, Lainhart W, Burnham CA. Epidemiology, Clinical Characteristics, and Antimicrobial Susceptibility Profiles of Human Clinical Isolates of Staphylococcus intermedius Group. J Clin Microbiol. 2018;56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 49. | Yasin M, Zafar S, Rahman H, Khan TA, Nazir S, Shah S, Dawood M, Ahmad S, Basit A, Khan SN, Saleha S. Baseline characteristics of infected foot ulcers in patients with diabetes at a tertiary care hospital in Pakistan. J Wound Care. 2018;27:S26-S32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |