©The Author(s) 2026.
World J Diabetes. Feb 15, 2026; 17(2): 113149
Published online Feb 15, 2026. doi: 10.4239/wjd.v17.i2.113149
Published online Feb 15, 2026. doi: 10.4239/wjd.v17.i2.113149
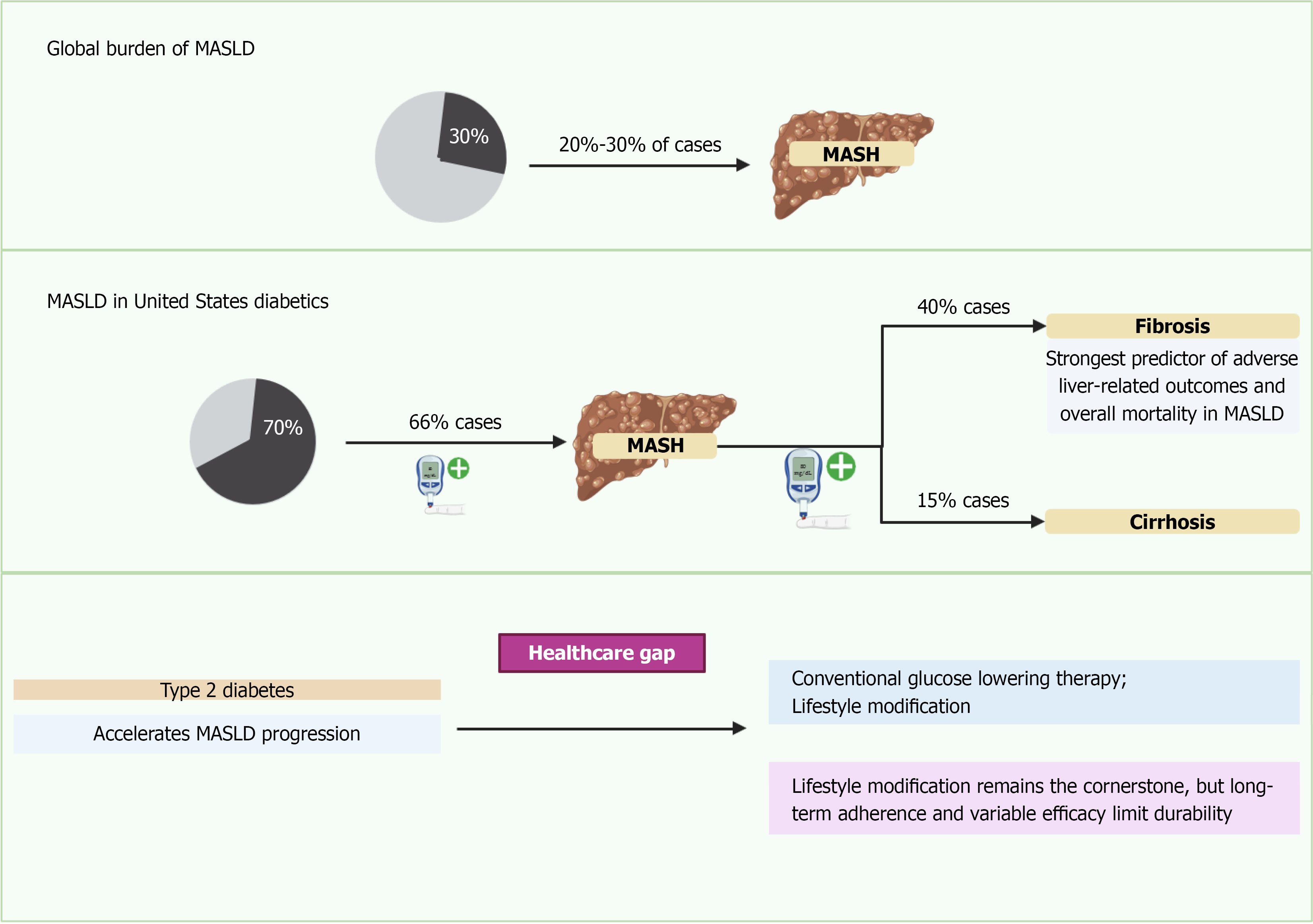
Figure 1 Global prevalence of metabolic dysfunction-associated steatotic liver disease in type 2 diabetes mellitus.
Metabolic dysfunction-associated steatotic liver disease (MASLD) affects more than half of individuals with type 2 diabetes mellitus worldwide, with prevalence ranging between 55% and 70% in recent meta-analyses. Estimates vary by region, diagnostic modality, and population studied. MASLD is consistently associated with increased risk of advanced fibrosis, cirrhosis, hepatocellular carcinoma, and cardiovascular outcomes. MASLD: Metabolic dysfunction-associated steatotic liver disease; MASH: Metabolic dysfunction-associated steatohepatitis.
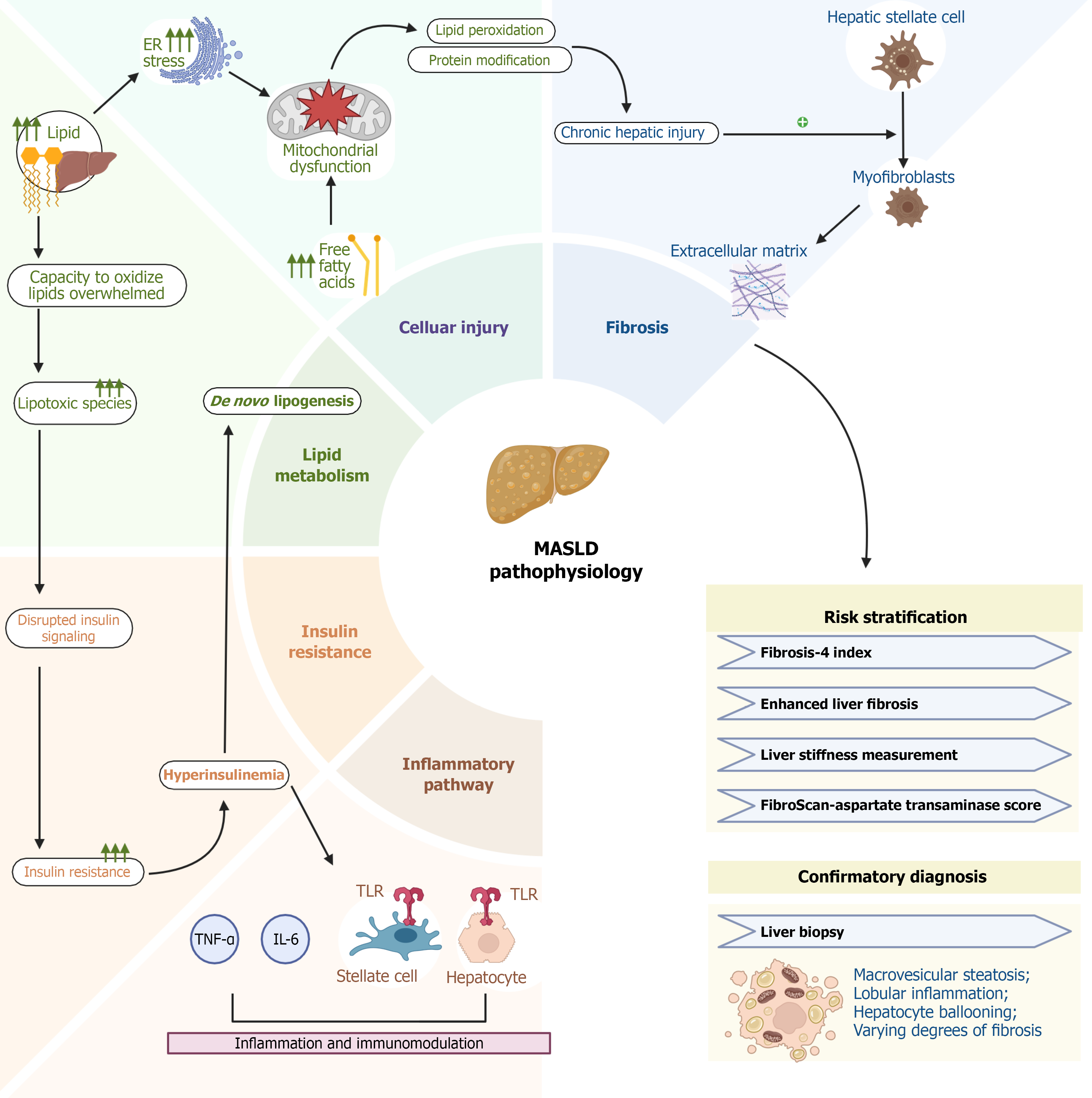
Figure 2 Pathophysiology of metabolic dysfunction-associated steatotic liver disease in type 2 diabetes mellitus.
The pathogenesis of metabolic dysfunction-associated steatotic liver disease is multifactorial and includes insulin resistance, lipotoxicity, oxidative stress, gut-liver axis alterations, and inflammatory signaling. Hepatic fat accumulation promotes oxidative stress and mitochondrial dysfunction, while adipose tissue dysfunction and systemic inflammation exacerbate steatohepatitis and fibrosis. Genetic predisposition (e.g., PNPLA3, TM6SF2) and environmental factors (diet, sedentary lifestyle) modulate disease progression. ER: Endoplasmic reticulum; ROS: Reactive oxygen species; MASLD: Metabolic dysfunction-associated steatotic liver disease; TLR: Toll-like receptor; TNF: Tumor necrosis factor; IL: Interleukin.
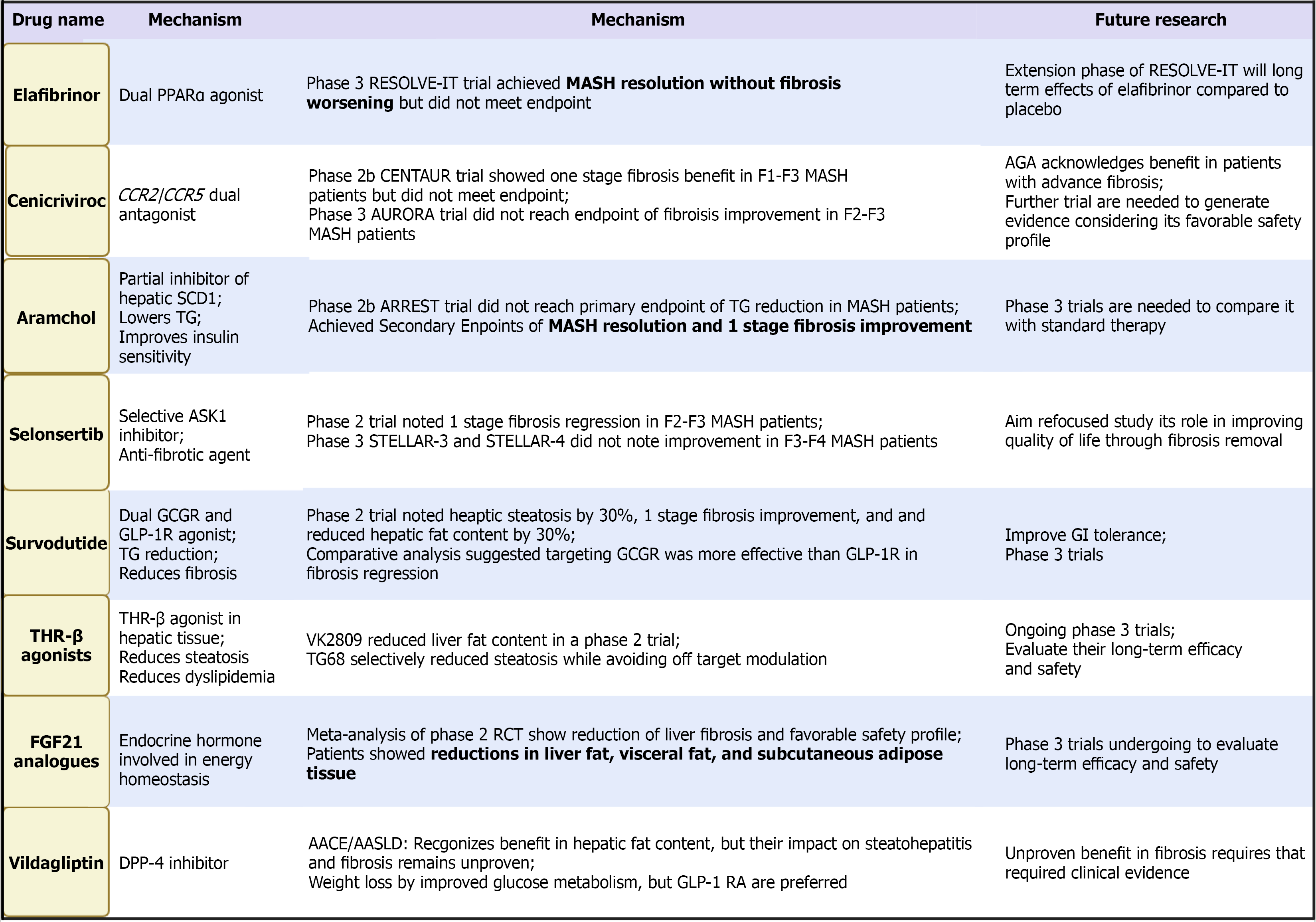
Figure 3 Lifestyle intervention in metabolic dysfunction-associated steatotic liver disease and type 2 diabetes mellitus.
Lifestyle modification remains the cornerstone of metabolic dysfunction-associated steatotic liver disease management. Sustained weight loss of ≥ 7%-10% is associated with steatohepatitis resolution and fibrosis regression. Dietary strategies such as the mediterranean diet and structured exercise programs (aerobic and resistance training) provide durable benefit, although long-term adherence is challenging. THR: Thyroid hormone receptor; FGF: Fibroblast growth factor; PPAR: Peroxisome proliferator-activated receptor; SCD1: Stearoyl-CoA desaturase 1; TG: Triglyceride; ASK1: Apoptosis signal-regulating kinase 1; GCGR: Glucagon receptor; GLP-1R: Glucagon-like peptide-1 receptor; DPP-4: Dipeptidyl peptidase 4; MASH: Metabolic dysfunction-associated steatohepatitis; RCT: Randomized clinical trial; GLP-1 RA: Glucagon-like peptide-1 receptor agonists; AACE: American Association of Clinical Endocrinologists; AASLD: American Association for the Study of Liver Diseases; AGA: American Gastroenterological Association; GI: Gastrointestinal.
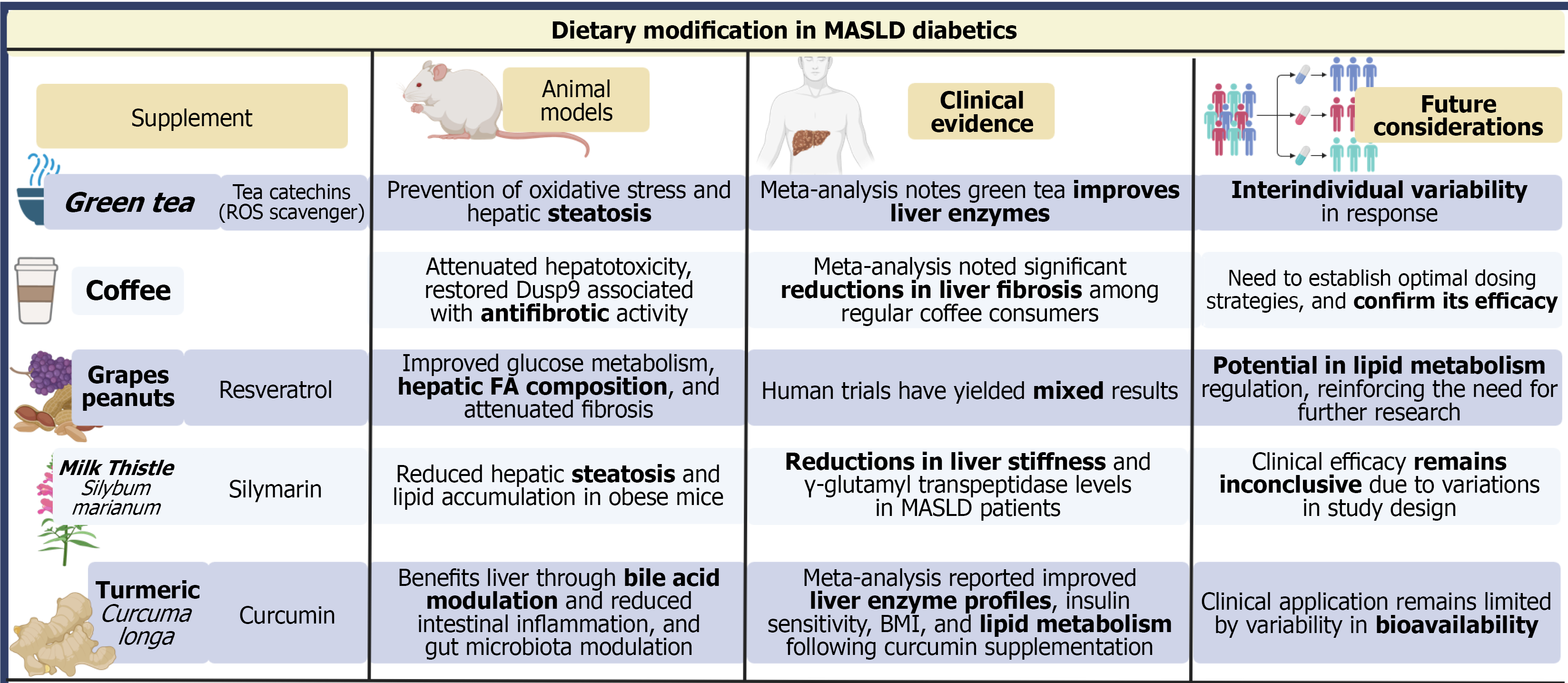
Figure 4 Emerging therapies in metabolic dysfunction-associated steatotic liver disease.
Several investigational drugs target diverse pathways: Dual incretin agonists (tirzepatide), thyroid hormone receptor-β agonists (resmetirom), farnesoid X receptor agonists (obeticholic acid), pan-peroxisome proliferator-activated receptor agonists (lanifibranor), and fibroblast growth factor analogs (efruxifermin, aldafermin). Most agents demonstrate histologic or imaging benefit in phase 2/3 studies, though none are yet approved. Combination approaches are under evaluation. MASLD: Metabolic dysfunction-associated steatotic liver disease; FA: Fatty acid.
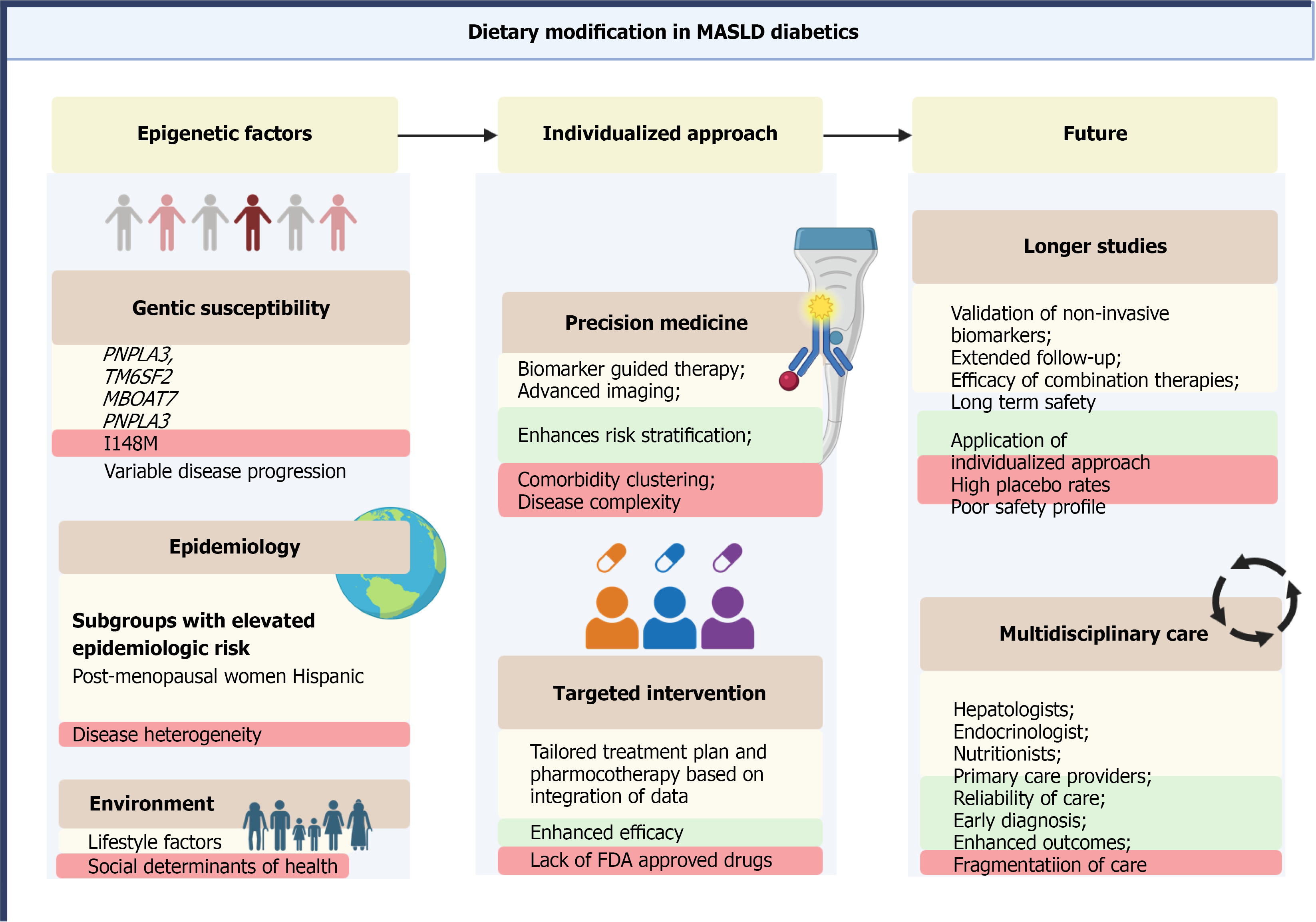
Figure 5 Personalized medicine framework in metabolic dysfunction-associated steatotic liver disease.
Future metabolic dysfunction-associated steatotic liver disease management will integrate genetic risk (e.g., PNPLA3, TM6SF2), metabolic and lifestyle factors, and non-invasive biomarkers with artificial intelligence and electronic health records to enable individualized therapy. Multidisciplinary care involving hepatology, endocrinology, cardiology, and primary care will be essential for optimal outcomes. FDA: Food and Drug Administration.
- Citation: Suresh MG, Mohamed S, Geetha HS, Prabhu S, Trivedi N, Ng ZC, Mehta PD, Brar AS, Sohal A, Goyal MK, Hatwal J, Batta A. Metabolic dysfunction-associated steatotic liver disease and type 2 diabetes: Pathophysiology, diagnosis, and emerging therapeutic strategies. World J Diabetes 2026; 17(2): 113149
- URL: https://www.wjgnet.com/1948-9358/full/v17/i2/113149.htm
- DOI: https://dx.doi.org/10.4239/wjd.v17.i2.113149