Published online Nov 15, 2025. doi: 10.4251/wjgo.v17.i11.110828
Revised: July 15, 2025
Accepted: October 15, 2025
Published online: November 15, 2025
Processing time: 148 Days and 21.9 Hours
Esophageal cancer is a clinically common malignant tumor of the digestive sys
We report the case of a 61-year-old man who underwent repeated esophageal di
The establishment of a multidisciplinary case management team, combined with the implementation of a self-help balloon dilation technique, early identification and management of nursing issues and complications, and personalized extended care, can significantly enhance patient satisfaction during hospitalization, improve quality of life, and extend the interval between readmissions. These strategies can provide valuable practical guidance for the clinical treatment and nursing of patients with recurrent esophageal stenosis.
Core Tip: By meticulously documenting the patient’s stenosis recurrence patterns, procedural details (such as balloon dilation), and treatment efficacy, this case report provides clinicians with standardized procedural protocols and evidence-based decision-making references for clinical practice. By demonstrating multidisciplinary collaboration across gastroenterology, head and neck surgery, nutrition, and pain management specialties, this case study proposes a replicable collaborative model that optimizes clinical outcomes through coordinated care pathways for complex patient management. This case report addresses the literature gap in managing refractory stenosis following endoscopic submucosal dissection and offers clinical evidence to inform guideline updates through systematic documentation of therapeutic interventions.
- Citation: Yang SH, Ren HF, Chen X, Wang R, Zhang MG. Refractory esophageal stenosis after endoscopic submucosal dissection for esophageal cancer managed with multiple dilations: A case report. World J Gastrointest Oncol 2025; 17(11): 110828
- URL: https://www.wjgnet.com/1948-5204/full/v17/i11/110828.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i11.110828
Esophageal cancer is a common malignant tumor of the digestive system. According to statistics, in 2022, esophageal cancer ranked eleventh in incidence and sixth in cancer-related mortality worldwide[1], while in China, it ranked seventh in incidence and fifth in mortality[2]. The mortality rate from esophageal cancer remains among the highest of all cancer-related deaths. Owing to tumor invasion, the main clinical manifestation of esophageal cancer is dysphagia[3]. Current conventional treatment options include surgery, chemotherapy, radiotherapy, and molecular-targeted therapy[4]. In the early stages, esophageal cancer often presents with nonspecific symptoms, and most patients are diagnosed at an ad
This case involved a patient with refractory esophageal stenosis who required seven esophageal dilations within one year following endoscopic submucosal dissection (ESD)[6]. Repeated hospitalizations caused significant physical and psychological suffering, imposed a substantial economic burden on the patient and family, and demanded considerable time and energy. Therefore, our department established a multidisciplinary case management team to identify nursing issues and complications at an early stage through collaborative efforts. We also pioneered the application of a self-help balloon dilation technique in patients with esophageal stenosis to explore its scientific basis and effectiveness. The details of this case are presented below.
Persistent hoarseness for more than 1 year.
A 61-year-old man presented with a post-ESD stricture following esophageal squamous cell carcinoma. Over a year ago, the patient had experienced dysphagia without any obvious cause, accompanied by a dry throat, a foreign body sensation in the throat, and hoarseness. On May 31, 2023, he visited our hospital’s Outpatient Department and underwent a neck computed tomography (CT) scan, which suggested a nodule in the right pyriform sinus, raising suspicion of a tumor. Laryngoscopy revealed a mass in the right pyriform sinus and leukoplakia of the vocal cord. A biopsy of the mass in the right pyriform sinus indicated high-grade squamous intraepithelial neoplasia with areas of invasive squamous cell carcinoma. On June 13, 2023, painless gastroscopy showed Helicobacter pylori infection and large areas of rough esopha
| Time | Interventions | Results |
| June 15, 2023 | Pyriform sinus cancer resection + vertical hemilaryngectomy and laryngeal function reconstruction + right neck lymph node dissection + tracheotomy | Discharge |
| August 4, 2023 | Painless endoscopic ultrasound + painless gastroscopy + endoscopic submucosal dissection | Discharge |
| September 6, 2023 | Esophageal dilation via endoscopy + nutritional tube placement | Discharge |
| December 1, 2023 | Painless gastroscopy + esophageal dilation + nutritional tube placement | Discharge |
| January 26, 2024 | Painless gastroscopy + esophageal dilation + nutritional tube placement | Discharge |
| March 22, 2024 | Painless gastroscopy + esophageal dilation + nutritional tube placement | Discharge |
| April 30, 2024 | Painless gastroscopy + esophageal dilation + nutritional tube placement | Discharge |
| June 5, 2024 | Painless gastroscopy + esophageal dilation + nutritional tube placement | Discharge |
| July 22, 2024 | Esophageal dilation via endoscopy + gastric tube placement | Discharge |
| August 29, 2024 | Esophageal dilation via endoscopy + three-lumen double-cystic tube placement | Discharge |
| October 23, 2024 | Esophageal dilation via endoscopy + gastric tube placement | Discharge |
The patient had a 5-year history of hypertension, for which he had been taking felodipine sustained-release tablets (5 mg once daily) and metoprolol succinate extended-release tablets (23.75 mg once daily). His blood pressure had previously been well-controlled, but he had discontinued antihypertensive medications for over 8 months before presentation.
The patient reported no significant family history.
The patient was a 61-year-old man, measuring 160 cm in height and weighing 49 kg. Physical examination revealed a tracheostomy in the neck; no skin rash or subcutaneous hemorrhage was observed, and no superficial lymphadenopathy was palpable. The head was normocephalic without deformities, with bilaterally anicteric sclerae. The neck was supple without rigidity, with normal carotid pulses and jugular venous pressure; the thyroid gland was non-enlarged, non-tender, and without audible bruits. The thorax was symmetrical without deformities, with symmetrical bilateral respiratory movements and breasts without abnormalities; tactile fremitus was symmetrical and normal bilaterally, with no pleural friction rubs palpable; percussion notes were resonant bilaterally, and breath sounds were clear without crackles, wheezes, or rhonchi on auscultation. Cardiac examination showed normal heart borders with a regular rhythm and no murmurs auscultated over any valve area. The abdomen exhibited a normal contour, was soft, non-tender, and without rebound tenderness; no masses were palpable, with the liver and spleen non-palpable below the costal margins and kidneys non-ballotable. Extremities showed no peripheral edema, joints had no apparent abnormalities, and patho
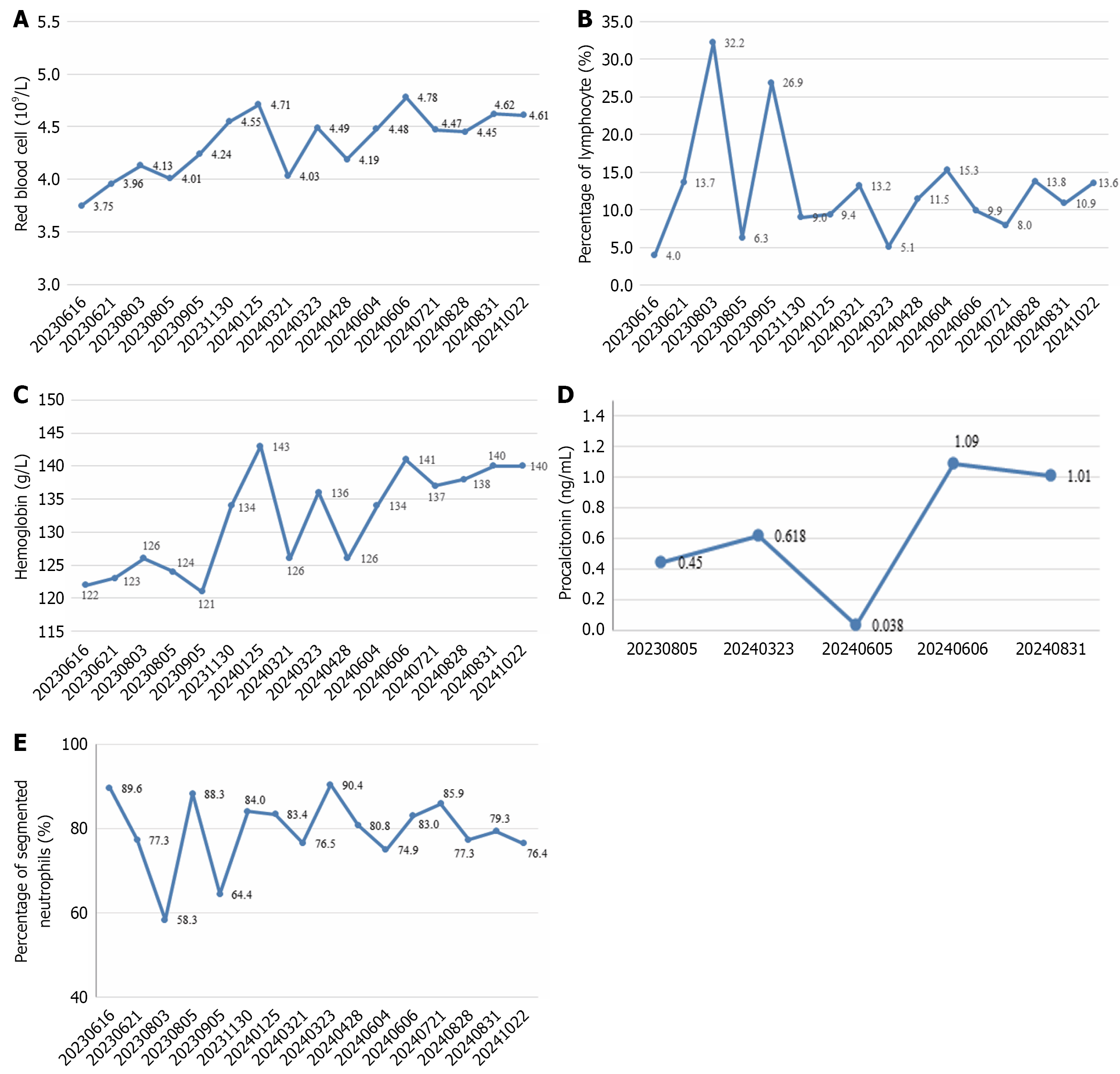
Laboratory investigations showed Serratia marcescens growth with a small number of colonies (++) in the sputum culture. Blood tests showed reduced red blood cell (× 1012/L) count, lymphocyte percentage (%), and hemoglobin (g/L) level compared to normal values (Figures 1A–1C). Platelet (× 109/L) counts consistently remained within the normal reference range [(100–300) × 109/L] throughout the testing period. The white blood cell (× 109/L) count was slightly reduced at 3.34 × 109/L on September 5, 2023, marginally below the normal range of 3.5–9.5 × 109/L, while maintaining normal levels at other time points. In addition, partial elevations were observed in procalcitonin (ng/mL) and segmented neutrophil percentage (%) compared to normal values (Figures 1D and 1E).
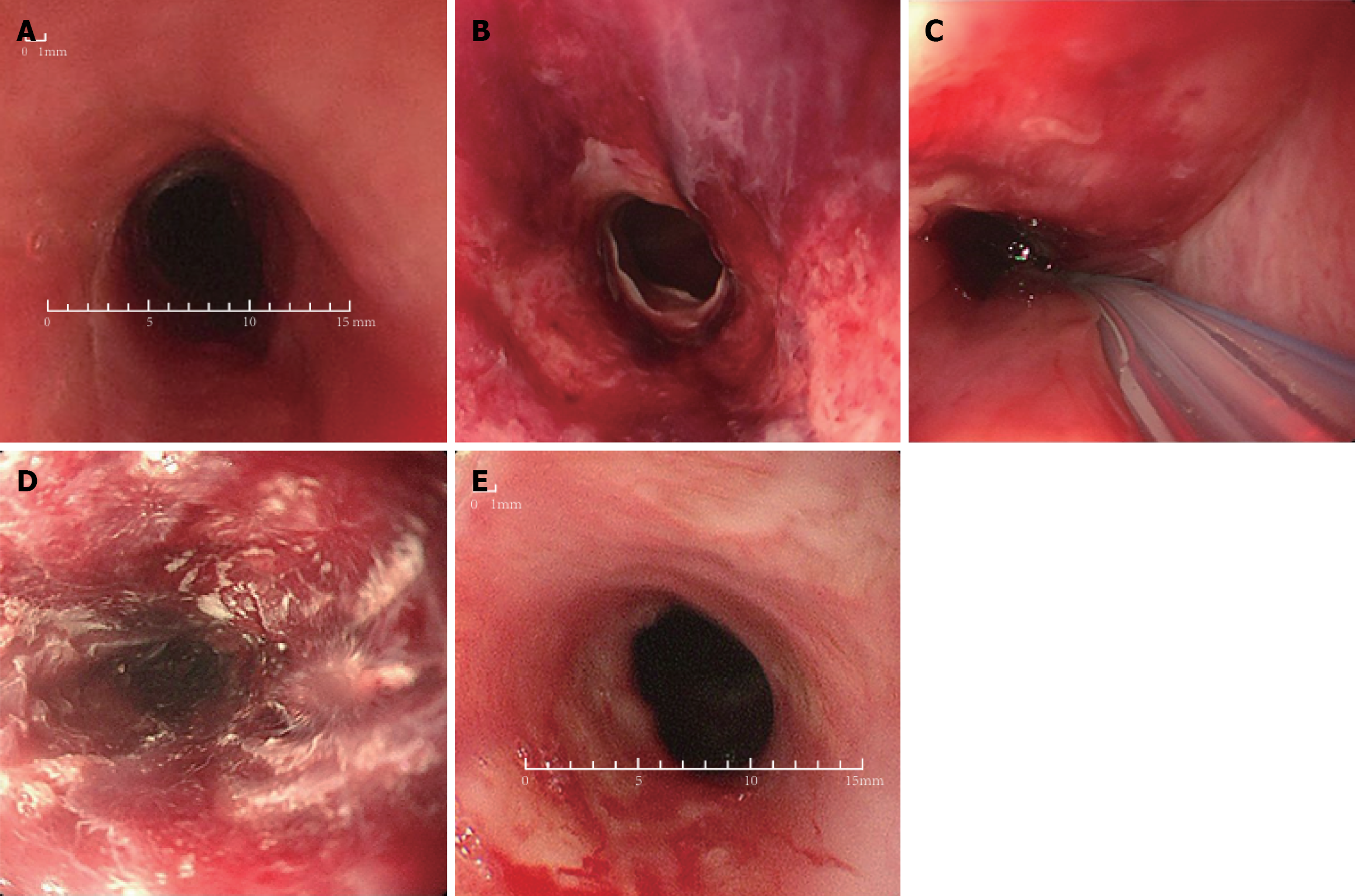
The neck CT demonstrated circumferential wall thickening and edema in the mid-to-upper esophageal segment, accompanied by focal luminal stenosis. The chest CT revealed a few small nodules in both lungs, which were mostly due to inflammatory reactions, and a few fibrous streaks in both lungs. Endoscopic examination revealed severe stenosis of the esophageal lumen with a diameter of 5 mm (Figure 2A).
Esophageal squamous cell carcinoma (M3, circumferential) with post-ESD stricture, post-endoscopic dilation for esophageal stenosis (seventh procedure).
On the day of admission, the attending physician conducted a physical examination, a specialist examination, and ancillary tests for the patient. The responsible nurse performed an admission assessment, which included a general condition assessment and pain assessment, and guided the patient to complete the standard questionnaire for the Core Quality of Life Questionnaire (QLQ-C30)[8] and the esophageal cancer-specific supplementary questionnaire, the Quality of Life–Oesophageal cancer 18 (QLQ-OES18)[9]. The “Sunshine Angel” team administered the West China Mental Health Index questionnaire for psychological assessment. The assessment revealed that the patient had issues such as dysphagia, nutritional imbalance, pain, ineffective airway clearance, pulmonary infection, and reduced endurance for activities.
A multidisciplinary case management team was established, comprising healthcare professionals from gastroenterology, head and neck surgery, respiratory medicine, nutrition, infectious diseases, pain management, and psychology depart
After ESD, the patient developed recurrent esophageal stenosis, resulting in dysphagia and necessitating multiple hospitalizations for esophageal dilation procedures. Therefore, the primary treatment focus was to prevent or slow down recurrent esophageal stenosis. During the patient’s eighth admission, the case management team reviewed domestic and international literature[10-13] to develop a self-help balloon dilation protocol, which was further optimized through external training. On August 29, 2024, the patient underwent esophageal dilation via endoscopy along with placement of a three-lumen double-cystic tube (Figures 2B and 2C). Postoperatively, the patient was instructed on the self-help balloon dilation technique to facilitate home-based dilation, aiming to reduce the frequency of hospital readmissions for dilation procedures.
Operational steps: (1) Set an alarm to remind the patient to perform self-dilation at fixed times daily; (2) The esophageal balloon valve is a one-way valve. Before each operation, use a 50-mL syringe to evacuate the gas inside the balloon and confirm that it is empty; (3) Use a 50-mL syringe to draw the predetermined volume of air (as instructed by the physician) and inject it into the esophageal balloon; do not change the volume arbitrarily. Perform dilation four times a day, with each session lasting 20 minutes. Record the completion and any discomfort in the “Esophageal Stenosis Self-help Balloon Dilation Record”; (4) After dilation, evacuate the gas from the balloon and confirm that it is empty; and (5) After the pro
Precautions: (1) Throat discomfort or even pain may occur 3–5 days after the placement of the dilation balloon. If it is unbearable, the patient can take ibuprofen sustained-release capsules orally or via the feeding tube. The capsules must be opened before administration, with a dosage of one capsule per day; (2) During non-dilation periods, the patient can consume liquid diets orally. If there is a sensation of obstruction during eating, food can be pureed and administered through the feeding tube; (3) Gastroscopy should be reviewed every 3 weeks to assess the epithelialization of the esophageal stenosis site and to determine whether to replace or remove the dilation balloon. The balloon is expected to be worn for 2 months, but the duration may vary based on follow-up assessments; and (4) If any severe discomfort occurs, healthcare providers should be contacted immediately.
Management of esophageal restenosis: The pathology report indicated that the patient’s esophageal stenosis was caused by inflammatory granulation tissue hyperplasia. To prevent or slow down further hyperplasia, the medical staff in the endoscopy center used a mixture of triamcinolone acetonide (1 mL) and normal saline (4 mL) for extensive multi-point injection into the submucosal or mucosal layer at the site of the tear during the procedure (Figure 2D). Postoperatively, the patient was prescribed prednisone orally or administered via a feeding tube[14].
Nutritional management: The patient experienced a weight loss from 52 kg to 49 kg after falling ill, resulting in a body mass index of 19.14 kg/m2. Ensuring adequate nutritional intake was therefore of vital importance. On the day of sur
Pain management: On the day of admission, the day of surgery, the first postoperative day, and during pain flare-ups, the responsible nurse assessed the patient’s pain score, pain location, intensity, nature, and its impact on daily life, and promptly notified the physician for intervention. During the esophageal dilation via endoscopy, a Savary dilator was used to gradually expand the stenotic esophagus from 6 mm to 11–12 mm. After dilation, visible tearing of the esophageal mucosa and the local muscular layer was observed, without perforation. After the nutritional tube was placed, the patient experienced minor bleeding from the nostrils and complained of unbearable pain in the neck and nasal area during the early hours after surgery. The assigned nurse assessed the pain score at 6, indicating moderate pain. Following the physician’s order, a dezocine injection (5 mg) was administered intramuscularly, and the pain was significantly relieved within half an hour, with the pain score reduced to 2 (mild pain). During the hospital stay, the patient received the following treatments daily: (1) Intravenous infusion of 4 mL of phenytoin injection + 100 mL of 0.9% normal saline; (2) Midazolam 1 mg via feeding tube to aid sleep, once per night; and (3) Topical application of 0.4 g of lidocaine hydrochlo
Anti-infective therapy: Chest CT revealed a few small nodules in both lungs, mostly due to inflammatory reactions, and a few fibrous streaks in both lungs. Sputum culture results showed Serratia marcescens with a small number of colonies (++). During the hospitalization period, blood tests indicated elevated levels of procalcitonin and the percentage of segmented neutrophils, with the majority of measurements exceeding normal values. Elevated levels of procalcitonin and segmented neutrophils are associated with infection[16,17]. The patient had a pulmonary infection, which was related to the disruption of the respiratory mucosal immune barrier after tracheostomy, weakened cough reflex, and reduced mucociliary movement, making it easier for pathogens to enter the bronchi and lung tissue[18]. During hospitalization, the attending physician administered intravenous cephalosporin antibiotics twice daily for anti-infective therapy.
Airway management: The patient had a large amount of thick sputum. During hospitalization, nebulized inhalation with 5 mL of 0.9% sodium chloride injection was administered three times a day to dilute the sputum, and suctioning was performed as needed. The excessive sputum was related to the pulmonary infection, while the viscosity of the sputum was associated with the loss of the humidifying function of the nasal cavity after tracheostomy, which led to increased sputum viscosity[19].
Psychological nursing: Since the diagnosis of a malignant tumor in August 2023, the patient had been hospitalized multiple times for esophageal dilation to relieve dysphagia. During each admission, the “Sunshine Angel” team in our department would assess the patient’s psychological condition using the West China Mental Health Index questionnaire, which consists of nine items. The results indicated that the patient had no or only very mild negative emotions (such as depression and/or anxiety) and no significant mental health issues. If the patient experienced emotional fluctuations during hospitalization, the Sunshine Angel team would reassess the patient’s psychological condition and provide psychological nursing interventions. The patient did not experience any psychological issues during hospitalization.
The case management team developed individualized discharge instructions based on the patient’s condition. Before discharge, a WeChat group was established for the patient and their family, and the patient was instructed to follow a WeChat mini-program for regular health education updates. The discharge instructions were as follows: (1) Dietary management: Consume or tube-feed protein-rich liquid or semi-liquid diets; (2) Tube care: Ensure the patency of the gastric tube and esophageal balloon cavity. Flush the gastric tube before and after feeding, thoroughly grind food or medication, and administer in small, multiple doses to avoid overly viscous substances[20]; (3) Tracheostomy care: Regularly clean the inner cannula, suction as needed, and use nebulized inhalation to humidify the airway and prevent blockage; (4) Medications for discharge: Take or tube-feed enteral nutrition powder (ensure) for nutritional supplementation. Take or tube-feed omeprazole before meals to treat duodenal ulcers and gastroesophageal reflux disease. Take or tube-feed prednisone, gradually tapering the dose, to reduce and treat pulmonary inflammatory reactions and prevent or slow down the recurrence of esophageal stenosis due to inflammatory granulation tissue hyperplasia; (5) Regular follow-up in gastroenterology clinic: Undergo gastroscopy. If there is a blockage in the gastric tube or issues with the tracheal balloon inflation or deflation, seek medical attention promptly; (6) Monitoring symptoms: Pay attention to chest pain, sore throat, respiratory status, and stool color. If there is a significant worsening, visit the Emergency Department immediately; and (7) Postoperative surveillance for hypopharyngeal squamous cell carcinoma: Follow up in the oto
The patient was discharged on September 4, 2024, in improved condition. He was originally scheduled to return to the hospital for a gastroscopy review in the third week after surgery (September 19, 2024) to assess the degree of esophageal dilation and determine whether to replace or remove the self-help balloon. After the placement of the three-lumen double-cystic tube, the patient performed daily esophageal dilation as prescribed (Table 2). However, he experienced significant discomfort and pain in the nasal ala and pharynx, making it difficult to tolerate. After administration of analgesics via the feeding tube, the gastric tube became blocked, and the patient experienced difficulty breathing during balloon inflation. Therefore, he returned to the hospital for evaluation on September 13, 2024. The physician assessed the situation and removed the three-lumen double-cystic tube and reinserted the gastric tube. The patient was subsequently readmitted on October 23, 2024, for another esophageal dilation procedure. On the day of discharge, the responsible nurse assessed the patient’s satisfaction during the hospital stay using the Public Hospital Medical Service Quality Patient Satisfaction Survey[21]. The patient’s satisfaction score was 5.81 out of a maximum of 6, indicating a high level of sa
| Date/dilation time | 8:00 | 13:00 | 18:00 | Before sleep | Recommended gas volume (mL) | Discomfort |
| September 4, 2024 | Completed | Completed | Completed | Completed | 35 | Discomfort and pain in the throat and pharynx |
| September 5, 2024 | Completed | Completed | Completed | Completed | 35 | Discomfort and pain in the throat and pharynx |
| September 6, 2024 | Completed | Completed | Completed | Completed | 35 | Discomfort and pain in the nasal ala and pharynx |
| September 7, 2024 | Completed | Completed | Completed | Completed | 35 | Discomfort and pain in the nasal ala and pharynx |
| September 8, 2024 | Completed | Completed | Completed | Incomplete | 35 | Discomfort and pain in the nasal ala and pharynx |
| September 9, 2024 | Completed | Completed | Completed | Completed | 35 | Discomfort and pain in the nasal ala and pharynx |
| September 10, 2024 | Completed | Completed | Completed | Completed | 35 | Discomfort and pain in the nasal ala and pharynx |
| September 11, 2024 | Completed | Completed | Completed | Incomplete | 35 | Discomfort and pain in the nasal ala and pharynx |
| September 12, 2024 | Completed | Completed | Completed | Incomplete | 35 | Discomfort and pain in the nasal ala and pharynx |
The extended care nurse followed up with the patient for 6 months, using the QLQ-C30[8] and the supplementary questionnaire for patients with esophageal cancer, QLQ-OES18[9], to assess his quality of life, as well as the interval between readmissions and the diameter of the esophageal stenosis. The QLQ-C30 comprises 20 items divided into three parts, namely functional dimension, symptom dimension, and overall health status. The QLQ-OES18 includes 18 items divided into functional and symptom dimensions. The scores for each dimension are averaged and linearly transformed to obtain a standard score ranging from 0 to 100. Higher scores in the functional dimension and overall health status indicate better patient conditions, while higher scores in the symptom dimension indicate more severe problems. After 6 months, the patient’s scores in the functional dimension and overall health status of the QLQ-C30 were higher than those before the intervention, while the symptom dimension score was lower. Similarly, the functional dimension score of the QLQ-OES18 was higher, and the symptom dimension score was lower, indicating an improvement in the patient’s quality of life. However, the overall level of the patient’s quality of life remained relatively low. The specific scores are shown in Table 3. The patient’s weight increased from 49 kg to 50 kg, and the interval between readmissions for eso
| Time | QLQ-C30 | QLQ-OES18 | |||
| Functional dimension | Symptom dimension | Overall health status | Functional dimension | Symptom dimension | |
| Before intervention | 33.3 | 33.33 | 50 | 22.33 | 48.90 |
| 6 months after follow-up | 50 | 23 | 66.67 | 33.33 | 42.23 |
Multiple hospital admissions for esophageal dilation and the short intervals between procedures imposed significant physical, psychological, and economic burdens on the patient, negatively affecting his quality of life. In response, our department established a multidisciplinary case management team to provide the patient with higher-quality and more diverse treatment options and nursing measures. The primary concern for this patient was to prevent or slow down the recurrence of esophageal stenosis. To this end, the case management team administered corticosteroids intraoperatively and postoperatively to prevent the regrowth of inflammatory granulation tissue at the site of stenosis and instructed the patient on how to perform self-dilation at home using a self-help balloon technique[14].
At the 6-month follow-up, the patient’s weight had increased from 49 kg to 50 kg. Notably, since disease onset, involuntary weight loss exceeding 5% (from 55 kg to 49 kg) occurred during gastric tube feeding and liquid diet intake, accompanied by a body mass index decline from 21.5 kg/m2 to 19.1 kg/m2, fulfilling the diagnostic criteria for cancer-related cachexia[22]. Although this patient exhibited only a 1-kg gain in weight post-treatment, weight stabilization constitutes a clinically significant outcome in cancer cachexia management, demonstrating the efficacy of multidiscip
The self-help balloon technique was first introduced in the 1970s. Compared to conventional esophageal dilation methods such as endoscopic stent placement, balloon dilation, and bougie dilation, the self-help balloon technique is primarily operated by the patients themselves. During hospitalization, healthcare providers instruct the patient on how to perform self-dilation at home. After discharge, medical staff monitor the patient’s daily self-dilation activities, promptly address any discomfort reported by the patient, and guide them on regular follow-up visits. The dilation device can be removed when the mucosa at the tear site is almost healed, and a standard endoscope can pass through without resis
Studies have shown that the self-help balloon technique can reduce the risk of repeated endoscopic procedures, maintain or improve the severity of dysphagia, and enhance patients’ quality of life[11,13,24]. However, during self-dilation at home, patients may experience adverse reactions such as perforation, bleeding, throat pain, and nasal ala pain, which can affect their adherence to the treatment[12]. Although the self-help balloon technique has been in practice since the 1970s, there is limited literature on this therapy. Recently, it has gradually been applied to patients with simple esophageal stenosis, primarily in international settings. The Gastroenterology Department in our hospital first applied this technique to a patient with esophageal stenosis. After 2 weeks of using the three-lumen double-cystic tube, the patient returned to the hospital, reporting severe pain in the nasal ala and throat, which persisted despite the use of analgesics. Owing to the patient’s inability to continue with the self-dilation technique, the attending physicians assessed the situation and removed the three-lumen double-cystic tube, replacing it with a gastric tube.
This pioneering case report evaluated self-help balloon dilation in a patient with refractory esophageal stricture, representing an early application of this approach in China’s clinical practice. The primary objectives were to prolong recurrence-free intervals and reduce endoscopic dilation frequency. However, the patient discontinued self-dilation after 2 weeks. The possible reasons for the short duration of self-dilation using the three-lumen double-cystic tube in this case are as follows: (1) The patient had a tracheostomy in the neck, which lowered his pain tolerance compared to patients with simple esophageal stenosis, resulting in poor adherence and difficulty in continuing the treatment; (2) The presence of a tracheostomy cannula may induce extrinsic esophageal compression, compromising the technical feasibility of self-help dilation procedures; (3) The presence of a tracheostomy in the neck meant that inflating the balloon could compress the tracheal cannula, causing difficulty in breathing and making the procedure intolerable; and (4) The self-help balloon device used in this case was a traditional three-lumen double-cystic tube, which has a relatively large diameter and low comfort level. Moreover, the relatively narrow lumen of the gastrostomy tube leads to frequent tube occlusion during enteral feeding. Therefore, in the future, our department could start with patients who have simple esophageal stenosis, gradually improve the self-help balloon technique, and develop more refined and comfortable devices. This would allow us to apply the technique to a broader range of patients with esophageal stenosis.
The establishment of a multidisciplinary case management team, combined with the implementation of the self-help balloon dilation technique, early identification and management of nursing issues and complications, and personalized extended care, can significantly enhance patient satisfaction during hospitalization, improve quality of life, extend the interval between readmissions for surgery, and effectively alleviate esophageal stenosis. Despite its potential benefits, the self-help balloon dilation technique is currently underutilized. Future efforts should focus on protocol refinement through systematic documentation of clinical experience, technical optimization, and rigorous validation in large-scale randomized controlled trials with extended follow-up periods to establish robust evidence for clinical implementation.
| 1. | Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5690] [Cited by in RCA: 12184] [Article Influence: 6092.0] [Reference Citation Analysis (6)] |
| 2. | Han B, Zheng R, Zeng H, Wang S, Sun K, Chen R, Li L, Wei W, He J. Cancer incidence and mortality in China, 2022. J Natl Cancer Cent. 2024;4:47-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 1167] [Article Influence: 583.5] [Reference Citation Analysis (0)] |
| 3. | Wang Y, Xie Z, Liu Y, Wang J, Liu Z, Li S. Symptom clusters and impact on quality of life in esophageal cancer patients. Health Qual Life Outcomes. 2022;20:168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 4. | Wang Y, Mukkamalla SKR, Singh R, Lyons S. Esophageal Cancer. 2024 Aug 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. [PubMed] |
| 5. | Spechler SJ. American gastroenterological association medical position statement on treatment of patients with dysphagia caused by benign disorders of the distal esophagus. Gastroenterology. 1999;117:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 60] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Chinese Society of Digestive Endoscopy; Endoscopic Physician Branch of Chinese Medical Doctor Association; Beijing Society of Digestive Endoscopy; Beijing Medical Association. [Consensus of Chinese experts on the endoscopic prevention and treatment of esophageal benign and malignant stricture (2020, Beijing)]. Zhonghua Weichang Neijing Dianzi Zazhi. 2020;7:165-175. [DOI] [Full Text] |
| 7. | Ueno H, Murphy J, Jass JR, Mochizuki H, Talbot IC. Tumour 'budding' as an index to estimate the potential of aggressiveness in rectal cancer. Histopathology. 2002;40:127-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 499] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 8. | Wang JP, Chen ZG, Lin WJ, Cui JN. [Assessment of quality of life in cancer patients: EORTC QLQ-C30 for use in China]. Xinli Xuebao. 2000;32:438-442. |
| 9. | Li HX, Yang H, Lang WJ, Lin YT, Zhang L, Cao N, Han D. [Validation of EORTC QLQ-OES18 scale in Chinese patients with esophageal cancer]. Chongqing Yixue. 2016;45:2969-2972. [DOI] [Full Text] |
| 10. | van Halsema EE, 't Hoen CA, de Koning PS, Rosmolen WD, van Hooft JE, Bergman JJ. Self-dilation for therapy-resistant benign esophageal strictures: towards a systematic approach. Surg Endosc. 2018;32:3200-3207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Halland M, Prichard DO, Kahn A, Lavey CJ, Katzka DA, Alexander JA. Esophageal Self-Dilation in Benign Refractory Esophageal Strictures: Outcomes from a Randomized Controlled Trial and a Prospective Observational Study. Dig Dis Sci. 2024;69:2883-2889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Li LS. [A novel self-help inflatable balloon to prevent and treat esophageal stricture after endoscopic submucosal dissection]. MSc Thesis, Chinese People’s Liberation Army Medical School. 2019. Available from: https://cdmd.cnki.com.cn/Article/CDMD-90115-1019247598.htm. |
| 13. | Qin Y, Sunjaya DB, Myburgh S, Sawas T, Katzka DA, Alexander JA, Halland M. Outcomes of oesophageal self-dilation for patients with refractory benign oesophageal strictures. Aliment Pharmacol Ther. 2018;48:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Yang J, Wang X, Li Y, Lu G, Lu X, Guo D, Wang W, Liu C, Xiao Y, Han N, He S. Efficacy and safety of steroid in the prevention of esophageal stricture after endoscopic submucosal dissection: A network meta-analysis. J Gastroenterol Hepatol. 2019;34:985-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Arends J, Bodoky G, Bozzetti F, Fearon K, Muscaritoli M, Selga G, van Bokhorst-de van der Schueren MA, von Meyenfeldt M; DGEM (German Society for Nutritional Medicine), Zürcher G, Fietkau R, Aulbert E, Frick B, Holm M, Kneba M, Mestrom HJ, Zander A; ESPEN (European Society for Parenteral and Enteral Nutrition). ESPEN Guidelines on Enteral Nutrition: Non-surgical oncology. Clin Nutr. 2006;25:245-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 423] [Cited by in RCA: 403] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 16. | Schuetz P, Albrich W, Mueller B. Procalcitonin for diagnosis of infection and guide to antibiotic decisions: past, present and future. BMC Med. 2011;9:107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 295] [Cited by in RCA: 339] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 17. | Naumenko V, Turk M, Jenne CN, Kim SJ. Neutrophils in viral infection. Cell Tissue Res. 2018;371:505-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 18. | Wang SM, Zhang AR, Wang XD, Yuan B, Wang XY, Yang L. [Risk factors of respiratory tract infection in tracheotomy patients in intensive care unit]. Zhonghua Yiyuan Ganranxue Zazhi. 2019;29:1000-1002+1023. [DOI] [Full Text] |
| 19. | He XY, Cai YY. [Research progress in the molecular biology of mucus regulators]. Guoji Neikexue Zazhi. 2006;33:29-31. |
| 20. | Liao X, Yang J, Jiang LL, Liu YW, Li K. [Research progress on the application of nursing risk management strategy in the management of nasogastric tube complications]. Huli Yanjiu. 2024;38:2868-2872. [DOI] [Full Text] |
| 21. | Du TY, Fan GR, Wang T, Yu J, Zou DD, Chen SW, Xue D. [Study on the Scales to Measure Patient Satisfaction of Public Hospitals]. Zhongguo Yiyuan Guanli. 2015;35:10-12. |
| 22. | Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, Jatoi A, Loprinzi C, MacDonald N, Mantovani G, Davis M, Muscaritoli M, Ottery F, Radbruch L, Ravasco P, Walsh D, Wilcock A, Kaasa S, Baracos VE. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12:489-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4623] [Cited by in RCA: 4051] [Article Influence: 270.1] [Reference Citation Analysis (0)] |
| 23. | Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, Fearon K, Hütterer E, Isenring E, Kaasa S, Krznaric Z, Laird B, Larsson M, Laviano A, Mühlebach S, Muscaritoli M, Oldervoll L, Ravasco P, Solheim T, Strasser F, de van der Schueren M, Preiser JC. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36:11-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1318] [Cited by in RCA: 1926] [Article Influence: 192.6] [Reference Citation Analysis (1)] |
| 24. | Gambardella C, Allaria A, Siciliano G, Mauriello C, Patrone R, Avenia N, Polistena A, Sanguinetti A, Napolitano S, Conzo G. Recurrent esophageal stricture from previous caustic ingestion treated with 40-year self-dilation: case report and review of literature. BMC Gastroenterol. 2018;18:68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |