Published online Jan 16, 2026. doi: 10.4253/wjge.v18.i1.112759
Revised: October 22, 2025
Accepted: November 17, 2025
Published online: January 16, 2026
Processing time: 162 Days and 23 Hours
Snare polypectomy and endoscopic mucosal resection (EMR) are effective and widely utilized for treating duodenal adenomas. However, circumferential, re
To develop a safe and effective treatment for these challenging lesions.
Between 2022 and 2024, a retrospective review was performed for all patients treated with cryoballoon for duodenal adenomas at two institutions. Cryoballoon focal ablation was performed using nitrous oxide, in which a 1-second “pre-puff” of nitrous oxide was performed, followed by delivery for 10 seconds to 14 seco
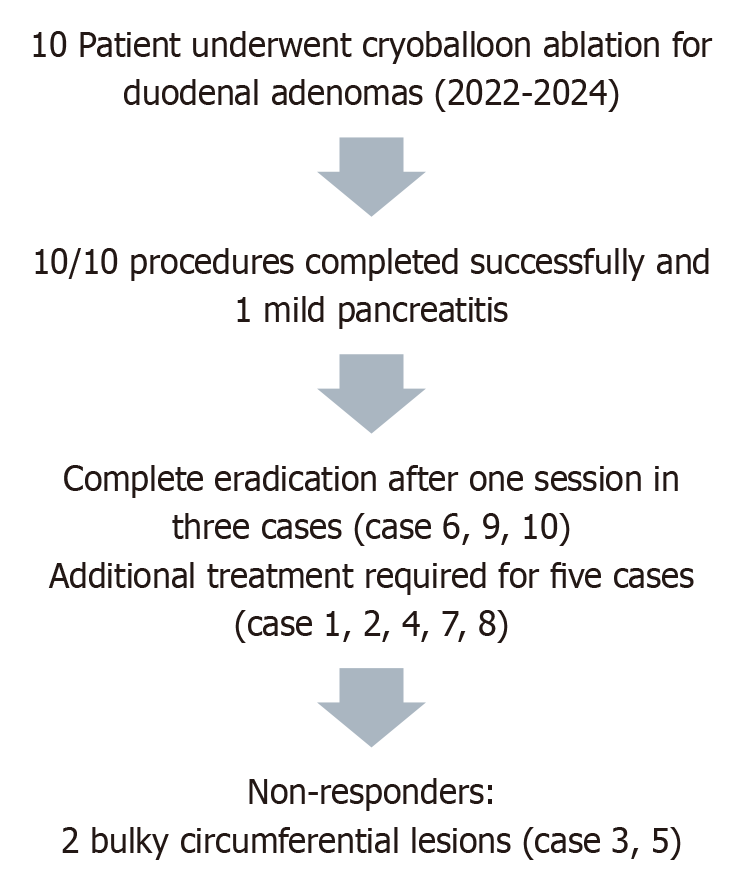
A total of ten individuals were treated, including six patients with recurrent adenomas following previous incomplete endoscopic resections, one patient with an extensive flat adenoma surrounding an ampullary polyp that could not be resected with a snare, and two patients with circumferential sessile duodenal adenomas longer than 5 cm that were considered unresectable by EMR. Follow-up endoscopy demonstrated no efficacy (< 20% improvement) in the two patients with circumferential sessile adenomas. Of the eight patients with non-circumferential adenomas, three had no residual adenoma. Five had significant improvement with < 40% of the adenoma remaining and were treated again with cryoballoon (3) or cold snare (2). Three of the five patients had no recurrence following the second treatment. The remainder are awaiting repeat endoscopy. Seven patients were treated as outpatients and had no adverse events. Two patients undergoing concomitant snare ampullectomy were hospitalized for observation; one developed mild pancreatitis and was discharged following a 48-hour admission, and the second patient was asymptomatic.
Cryoballoon treatment may be effective for non-circumferential flat duodenal adenomas that are not amenable to snare polypectomy or EMR, such as those with severe fibrosis from prior treatment. More than one treatment may be required. However, the treatments are safe and well-tolerated. Limited experience in two patients suggests that cryotherapy is not an effective treatment for bulky circumferential adenomas.
Core Tip: Conventional procedures for treating fibrotic, recurring, or widespread duodenal adenomas, such as snare poly
- Citation: Modirian N, Wei MT, Friedland S. Cryoballoon treatment of endoscopically unresectable duodenal adenomas. World J Gastrointest Endosc 2026; 18(1): 112759
- URL: https://www.wjgnet.com/1948-5190/full/v18/i1/112759.htm
- DOI: https://dx.doi.org/10.4253/wjge.v18.i1.112759
Duodenal adenomas are identified in 0.1% to 0.4% of endoscopies[1]. Duodenal adenomas are precancerous lesions with potential for progression to duodenal adenocarcinoma. Risk of malignant transformation rises with larger lesion size, high-grade dysplasia, and villous histology[2]. As a result, early detection and removal are critical to preventing cancer development. Endoscopic mucosal resection (EMR) is presently the standard therapy for superficial duodenal adenomas[3]. However, given the thin wall and abundant vascular supply of the duodenum, EMR poses a significant risk. Delayed bleeding occurs in 15%-20% of patients, and perforation occurs in 4%-5%, making the surgery technically difficult and sometimes dangerous[4]. Furthermore, up to 25% of patients can have recurrence following EMR, particularly after piecemeal resections[5].
Another therapy for duodenal adenomas is endoscopic submucosal dissection (ESD). ESD has emerged as a promising technique for achieving en bloc resection with histologically clear margins. While ESD is well-established for gastric and esophageal lesions, its application in the duodenum remains limited due to technical challenges and a higher com
Nitrous oxide CBA is a novel endoscopic technique that applies localized cryotherapy to ablate gastrointestinal muc
All patients who underwent duodenal CBA at Stanford University (Stanford, CA, United States) and the Veterans Affairs Palo Alto Health Care System (Palo Alto, CA, United States) between 2022 and 2024 were retrospectively reviewed. All procedures were performed by one endoscopist (Friedland S). This retrospective study was approved by the Ethics Committee of Stanford University Administrative Panel on Human Subjects in Medical Research. Duodenal adenomas that were deemed endoscopically unresectable due to fibrosis from prior incomplete treatment or extensive (> 3 cm) circumferential extent were included. Lesions with suspected invasive malignancy were excluded. Exclusion criteria included endoscopic features such as deep ulceration, non-lifting sign after submucosal injection, irregular or depressed morphology, or friability with spontaneous bleeding.
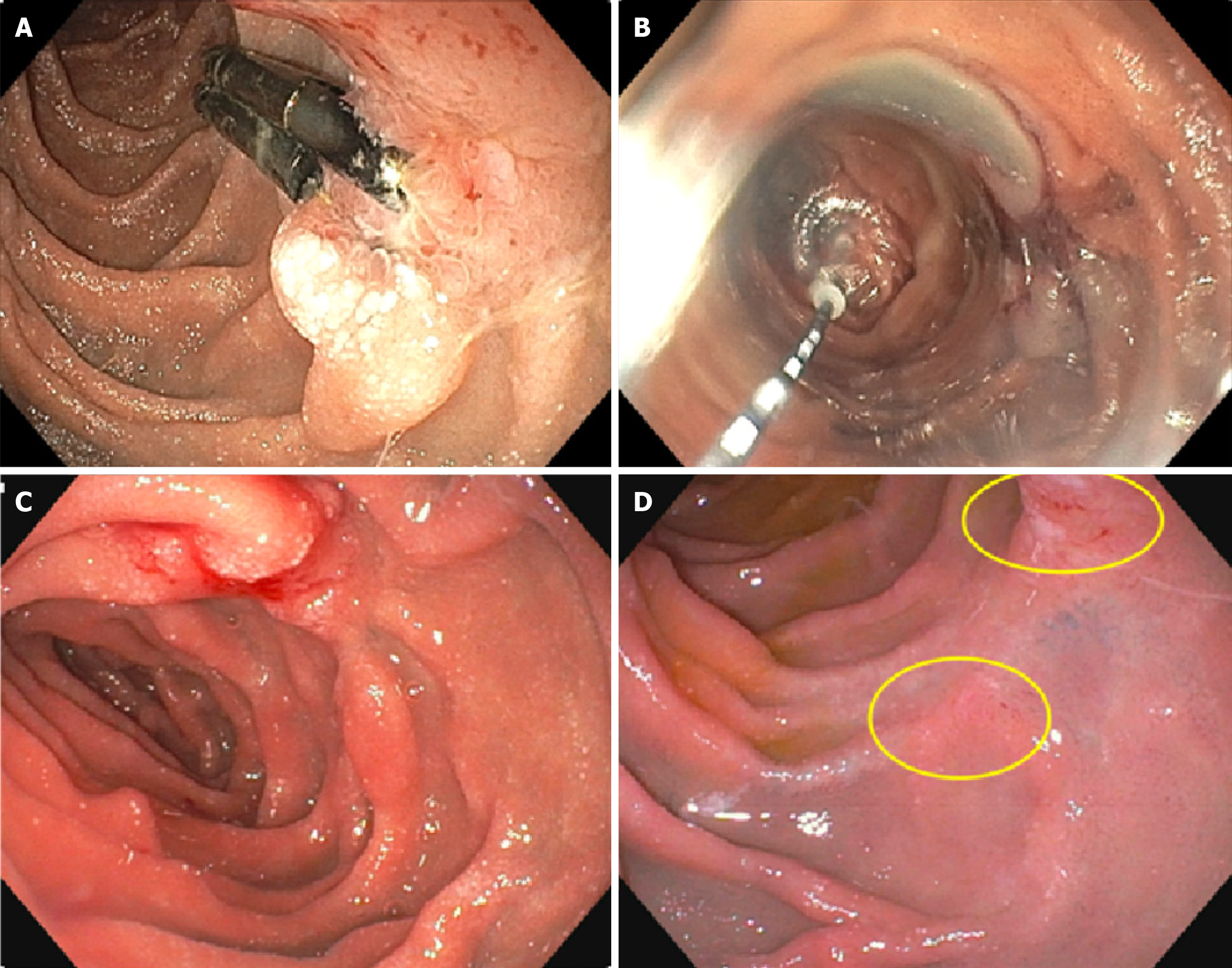
The CryoBalloon Focal Ablation System (CbFAS, Pentax Medical, GA, United States) was used in all procedures. Under monitored anesthesia care, the cryoballoon catheter was introduced via a high-definition therapeutic upper endoscope[10,12]. A 1-second “prepuff” of nitrous oxide was used to inflate the balloon and orient the diffuser against the lesion, followed by cryogen delivery for 10-14 seconds until an ice patch entirely covered the lesion. Applications were applied as needed until post-treatment erythema was observed over the entire lesion (Figure 1)[11,13]. Technical success was defined as accurate catheter positioning and the execution of at least one cryotherapy application. Surveillance endoscopy with biopsy was performed at 3 months to 12 months post-ablation to assess efficacy (≥ 50% lesion reduction and no recurrence) and to identify potential adverse events, such as perforation, bleeding, or stricture formation[11].
For all analyses, all tests were 2-tailed. A P-value < 0.05 was considered statistically significant. Continuous variables were expressed as mean ± SD.
Between 2022 and 2024, ten patients underwent CBA of duodenal adenomas (Table 1; Figure 2). The study comprised of six patients with recurrent lesions after prior endoscopic resection and four individuals with previously untreated, unresectable lesions due to morphology or anatomical restrictions. The mean age of the patients was 66.7 years (standard deviation 12.1 years), and 60% were male. The lesions primarily involved D2, which affected 70% (7 of 10) of patients, while 30% (3 of 10) involved duodenal bulb, and 30% (3 out of 10) had involvement in horizontal duodenum; 3 of the lesions involved more than one segment. Average lesion size was 34.5 mm (standard deviation 26.9 mm). CBA was completed successfully in all patients, with no intra-procedural complications.
| Case | Age | Sex | Comorbidities | Location | Prior treatment | Size at first cryogenic (mm) | Morphology | Fibrosis | Pathology | Cryogenic performed | Adverse event | Follow-up outcome |
| 1 | 73 | Male | Cardiomyopathy, metastatic cancer | D3 | Tattoo and biopsy | 20 mm | Flat | Severe | Adenomas | 12 seconds × 2 sites | None | Minimal residual adenoma at 4 months (5 mm, biopsied and repeat cryoballoon), no further surveillance due to severe comorbidities |
| 2 | 55 | Male | D2 | Incomplete EMR | 15 mm | Flat | Severe | Adenomas | 10 seconds × 2 sites | None | Two 8 mm residual adenomas were ablated at 3 months, 3 mm residual adenomas at 8 months were ablated, and no residual adenomas were found at biopsy at 15 months | |
| 3 | 77 | Male | FAP | D1, D3 (including periampullary) | Biopsy | 100 mm | Circumferential sessile | None | Adenomas | 12 seconds × 9 sites | None | < 20% improvement at 4 months, cryogenic repeated (12 seconds × 6 sites), no improvement at 9 months. Adenoma on biopsy |
| 4 | 72 | Male | D2 | Incomplete EMR and Ovesco for bleeding | 20 mm | Flat and Ovesco are attached | Severe | Adenomas | 12 seconds × 3 sites | None | Ovesco was still attached at 6 months, removed by traction. 1/3 of adenoma remained, removed by cold snare. Awaiting repeat endoscopy | |
| 5 | 71 | Male | D2, D3 (starting 1 cm distal to ampulla) | Biopsy | 50 mm | Circumferential sessile | None | Adenomas | 12 seconds × 12 sites | None | < 20% improvement at 2 months. Repeat biopsy of adenoma. Had surgical resection (adenoma) | |
| 6 | 70 | Female | Cirrhosis with varices | D1 | EMR/band | 10 mm | Flat | Severe | HGD | 10 seconds × 1 sites | None | No recurrence at 1 year (biopsy normal) |
| 7 | 78 | Female | Prior XRT for lymphoma | D2 | PEMR with clip | 15 mm | Flat with clip attached | Severe | HGD | 10 seconds × 1 sites | None | 2/3 gone at 3 months, repeat ablation 10 seconds × 3 sites, no recurrence on biopsy at 6 months or 18 months |
| 8 | 78 | Female | D2 (including ampulla) | None | 50 mm | Flat, unable to grasp the snare | Mild | HGD | 10 seconds × 5 sites | None | 90% gone at 6 months, treated with cold snare. Recurrence at the ampulla treated with snare at 12 months. No recurrence on 18-month follow-up | |
| 9 | 41 | Female | FAP | D1, D2 (including near the ampulla) | PEMR | 20 mm | Flat | Severe | Adenomas | 10 seconds × 4 sites | Admitted 48 hours for mild pancreatitis | No recurrence at 6 months |
| 10 | 52 | Male | D2 | PEMR/tattoo | 20 mm | Flat (IIa + IIc) | Severe | Foveolar metaplasia but only small piece so unclear | 14 seconds × 3 sites | None | No recurrence at 6 months |
Eight patients were treated on an outpatient basis and experienced no adverse events. Two patients underwent concurrent snare ampullectomy and were admitted for observation. One patient developed mild post-procedural pancreatitis, which resolved with supportive care during a 48-hour hospital stay. The second patient remained asymptomatic and was discharged without incident.
Treatment response varied by lesion morphology during follow-up endoscopy. Two patients with large circumferential sessile duodenal adenomas > 5 cm experienced a < 20% reduction in lesion size and were classified as non-responders. One of the patients subsequently received surgical resection. In contrast, among the eight patients with non-circumferential adenomas, three achieved complete eradication of the adenoma on the first follow-up endoscopy. Five patients experienced a significant improvement, with a reduction of ≥ 60% in adenoma burden. Of these, three underwent repeat CBA, while two were managed with cold snare resection. One patient achieved complete resolution after a second cryoablation session, and another remained recurrence-free following a third treatment. Another patient received two rounds of snare resection, with no recurrence at the third follow-up (18 months after the index treatment). The remaining two patients are pending repeat endoscopic assessment or were unable to do so due to severe comorbidities.
Current endoscopic management strategies for duodenal adenomas have primarily been limited to EMR and ESD. EMR is widely considered the preferred first-line therapy for non-ampullary duodenal adenomas; however, its efficacy diminishes in cases of fibrosis or lesion recurrence. In a multicenter, prospective study, EMR for duodenal adenomas ≥ 10 mm was associated with an overall adverse event rate of 22.2%, including 18.5% delayed bleeding and 4.2% perforation, with lesion recurrence observed in 23% of patients at follow-up[4]. ESD offers higher en bloc and R0 resection rates but carries a significantly greater risk of complications. Honda et al[6] reported a perforation rate of 35% in their experience with duodenal ESD, while Jung et al[7] observed delayed perforation and bleeding despite successful en bloc resection.
CBA has rapidly evolved from an experimental therapy to a practical option for duodenal adenomas, driven by three key reports that collectively define its scope and safety. In the multicenter series by Dbouk, flat (Paris 0-IIa) duodenal adenomas in over 30 patients were treated with cryoballoon therapy, achieving 100% technical success. Notably, 76.5% of lesions shrank by at least half after a median of two sessions. No serious adverse events were observed, underscoring the safety of CBA[11]. Raphael presented a single patient “rescue” case: After repeated EMR attempts failed to clear a 1.2 cm flat adenoma, a single nitrous oxide cryoballoon application resulted in complete endoscopic and histologic eradication, with no immediate or delayed complications[12]. Similarly, in our experience, cryoablation treatment demonstrated a high technical success rate, with all ten cases (100%) achieving successful deployment and delivery of cryogen to the intended location. Out of the 6 cases of non-circumferential adenomas with completed follow-up, all six were able to achieve complete eradication, though several repeat therapies were required in some instances. On the other hand, circumferential sessile adenomas were unsuccessfully treated by cryoballoon, with < 20% improvement. This suggests that cryoballoon may not be a feasible strategy for managing bulky circumferential lesions, but more data are needed at this time, given the limited number of cases.
Strengths of this study include its focus on real-world cases of duodenal adenomas considered unresectable by conventional methods, a uniform treatment approach, and detailed follow-up with both clinical and technical outcomes. All procedures being performed by a single expert operator increased procedural consistency. Limitations include retro
While EMR and ESD are accepted therapies for duodenal adenomas, in our case series, we find that cryotherapy can also be an accepted approach for challenging lesions. While more than one therapy session may be required, the high safety profile of this procedure makes cryoballoon treatment an attractive approach. In our study, we find that cryoballoon treatment is effective in noncircumferential duodenal adenomas that cannot be treated with snare polypectomy or EMR due to significant fibrosis from previous treatments. However, cryoballoon therapy may be less effective for bulky circumferential adenomas. Further studies are needed to evaluate the application of cryotherapy in the management of duodenal lesions.
| 1. | Jepsen JM, Persson M, Jakobsen NO, Christiansen T, Skoubo-Kristensen E, Funch-Jensen P, Kruse A, Thommesen P. Prospective study of prevalence and endoscopic and histopathologic characteristics of duodenal polyps in patients submitted to upper endoscopy. Scand J Gastroenterol. 1994;29:483-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 147] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Yadav A, Nundy S. Case series of non-ampullary duodenal adenomas. Ann Med Surg (Lond). 2021;69:102730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 3. | Klein A, Nayyar D, Bahin FF, Qi Z, Lee E, Williams SJ, Byth K, Bourke MJ. Endoscopic mucosal resection of large and giant lateral spreading lesions of the duodenum: success, adverse events, and long-term outcomes. Gastrointest Endosc. 2016;84:688-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 4. | Probst A, Freund S, Neuhaus L, Ebigbo A, Braun G, Goelder S, Weber T, Märkl B, Anthuber M, Messmann H. Complication risk despite preventive endoscopic measures in patients undergoing endoscopic mucosal resection of large duodenal adenomas. Endoscopy. 2020;52:847-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Navaneethan U, Hasan MK, Lourdusamy V, Zhu X, Hawes RH, Varadarajulu S. Efficacy and safety of endoscopic mucosal resection of non-ampullary duodenal polyps: a systematic review. Endosc Int Open. 2016;4:E699-E708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Honda T, Yamamoto H, Osawa H, Yoshizawa M, Nakano H, Sunada K, Hanatsuka K, Sugano K. Endoscopic submucosal dissection for superficial duodenal neoplasms. Dig Endosc. 2009;21:270-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 120] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 7. | Jung JH, Choi KD, Ahn JY, Lee JH, Jung HY, Choi KS, Lee GH, Song HJ, Kim DH, Kim MY, Bae SE, Kim JH. Endoscopic submucosal dissection for sessile, nonampullary duodenal adenomas. Endoscopy. 2013;45:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 107] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 8. | Kim DH, Park SY, You HS, Jung YW, Joo YE, Myung DS, Kim HS, Kim NI, Kim SJ, Ju JK. Modified underwater endoscopic mucosal resection for intermediate-sized sessile colorectal polyps. Front Med (Lausanne). 2023;10:1200145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Schmidt A, Beyna T, Schumacher B, Meining A, Richter-Schrag HJ, Messmann H, Neuhaus H, Albers D, Birk M, Thimme R, Probst A, Faehndrich M, Frieling T, Goetz M, Riecken B, Caca K. Colonoscopic full-thickness resection using an over-the-scope device: a prospective multicentre study in various indications. Gut. 2018;67:1280-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 218] [Article Influence: 27.3] [Reference Citation Analysis (2)] |
| 10. | Canto MI, Shaheen NJ, Almario JA, Voltaggio L, Montgomery E, Lightdale CJ. Multifocal nitrous oxide cryoballoon ablation with or without EMR for treatment of neoplastic Barrett's esophagus (with video). Gastrointest Endosc. 2018;88:438-446.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Dbouk M, Brewer Guiterrez O, Trindade AJ, Diehl DL, Kwon RS, Thosani NC, Khara HS, Benias PC, Kerdsirichairat T, Canto MI. Initial multicenter experience with nitrous oxide cryoballoon for treatment of flat duodenal adenomas (with video). Gastrointest Endosc. 2021;93:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Raphael KL, Benias PC, Trindade AJ. Salvage CryoBalloon cryotherapy ablation for a duodenal adenoma. Endoscopy. 2020;52:E189-E190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Thaker AM, Muthusamy VR. Cryoballoon ablation for duodenal adenomas: Time to warm up to a cool new approach? Gastrointest Endosc. 2021;93:247-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/