INTRODUCTION
Owing to rapid advancements in endoscopy technology and continuous improvements in endoscopic devices, techniques such as endoscopic submucosal dissection (ESD), endoscopic mucosal resection (EMR), peroral cholangioscopy (POC), endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound have been increasingly adopted for the diagnosis and treatment of digestive diseases. However, numerous challenges have emerged during their application. For example, surgical complications frequently occur due to the limitations of the conventional endoscope[1,2]. Although some researchers have proposed strategies such as floss traction and the use of transparent caps, these approaches have yielded suboptimal outcomes due to variations in patients’ anatomical characteristics. In addition, certain conditions, such as complex bile duct stones and bleeding gastric ulcers located at the high lesser curvature, remain difficult to manage with conventional endoscopic techniques.
The multibending (MB) endoscope was initially developed to address challenges in accessing special sites, such as areas where ESD is deemed unfeasible[3]. Owing to its added bending section, the MB endoscope enables double-clamp operations (Figure 1). Furthermore, owing to its advantages, this technology has been applied in gastroscopy, duodenoscopy, and POC. In gastroscopy, the MB endoscope has been utilized primarily in ESD. Besides, it is integrated with other innovative diagnostic and therapeutic technologies, and supplements new medical approaches in gastroscopy. In duodenoscopy, the MB endoscope has optimized ERCP technology. Furthermore, in POC, the MB ultraslim endoscope has improved the endoscopic management of biliary diseases. This review highlights the advantages and achievements of the MB endoscope across different fields while also exploring potential future directions for its application.
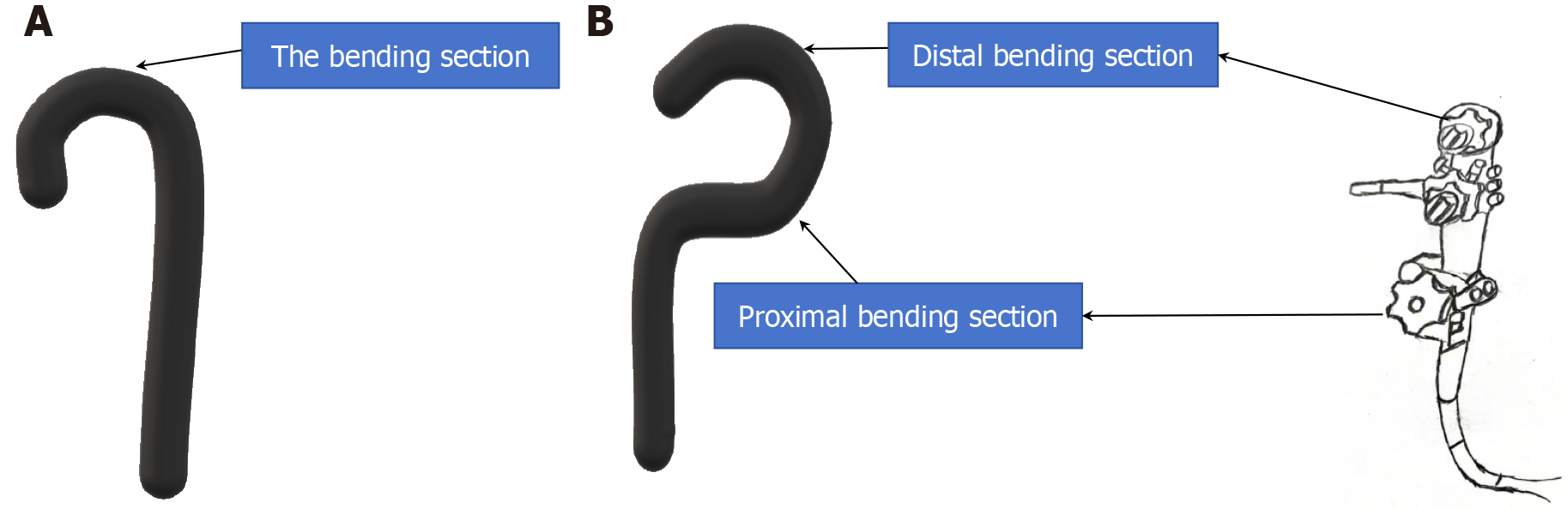
Figure 1 The figure of the comparison of structures between the conventional endoscope and the multibending endoscope.
A: The conventional endoscope constrained by limited curvature with a single bending section; B: The multibending endoscope offers enhanced flexibility, featuring two independently controlled bending sections. The control section includes two dials, each regulating the proximal and distal bending section, enabling precise and adaptable navigation.
THE MB ENDOSCOPE IN ESD
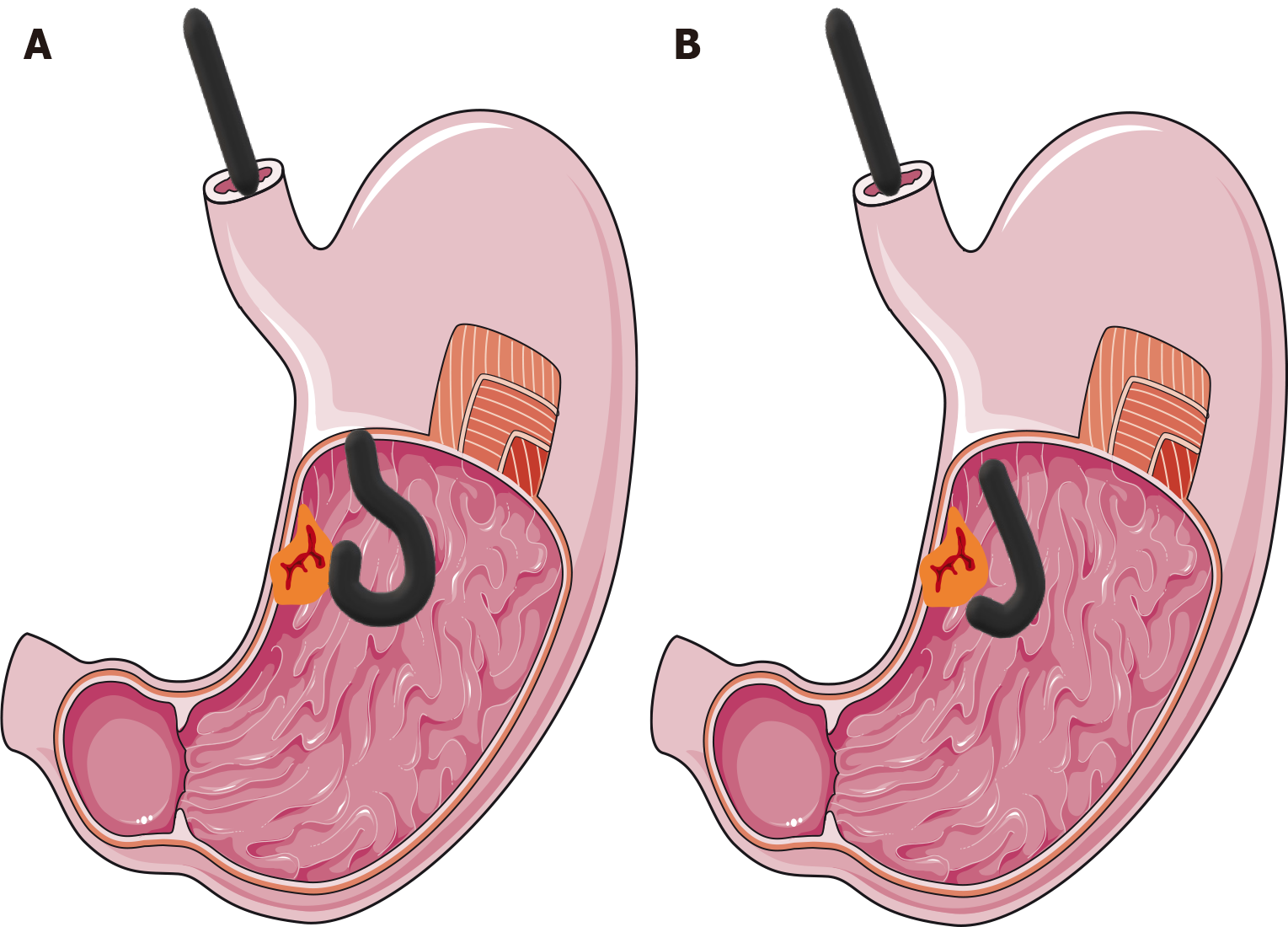
Complications such as bleeding and perforation are commonly observed during gastric ESD. These issues are primarily due to difficulty in accessing certain anatomical sites with a conventional endoscope. As a result, dissection is often performed from a distance, making blood vessels, muscle layer boundaries and the submucosa difficult to distinguish[4,5]. Furthermore, another significant cause of perforation is the inability of a conventional endoscope to approach the submucosa at an angle parallel to the muscle layer[6] (Figure 2).
Figure 2 The figure of the comparison between the conventional endoscope and the multibending endoscope in endoscopic submucosal dissection.
A and B: In the gastric endoscopic submucosal dissection, the multibending endoscope enables precise access to the submucosa at an angle parallel to the muscle layer, thereby minimizing trauma to the gastric muscle layer (A); the conventional endoscope is limited to a nearly perpendicular approach the constrained by a single bending section (B).
Owing to its complex structure, researchers have divided the stomach into upper, middle, and lower regions for study purposes[7-10]. Thus, one study revealed that performing ESD with an MB endoscope significantly reduces damage to the muscle layers and lowers the risk of complications, such as bleeding and perforation, for lesions located in the upper two-thirds of the stomach. However, the improvement is less pronounced for lesions in the lower third of the stomach[10]. Nonetheless, dividing the stomach into just three regions may oversimplify its intricate anatomy and fail to adequately guide decisions on MB endoscope usage. A new classification system based on 12 anatomical sites and histological factors has been proposed and is considered more precise[11]. According to this system, the use of the MB endoscope for ESD is particularly beneficial for lesions in areas such as the lesser curvature of the body, the fornix and the lesser curvature of the antrum, the esophagogastric junction and the gastric fundus[5,12]. Similarly, the conventional endoscope may not be suitable for EMR at certain sites, such as the lesser curvature of the antrum. The MB endoscope, however, enhances EMR efficiency in these areas, with the degree of improvement depending on the size of the lesions[13]. In addition, lesions in the gastric fundus, where the tip of the conventional endoscope is difficult to access, present a significant challenge for ESD. To address this problem, underwater and traction-assisted ESD using an MB endoscope has been proposed[12]. This innovative strategy has the potential to overcome the difficulties associated with ESD for lesions in the gastric fundus.
In addition to improving the success of gastric ESD and reducing complication rates, the MB endoscope has also overcome many other challenges associated with gastroscopy. Owing to the unique histological and anatomical characteristics of the stomach, mucosal defect closure after ESD has long been a difficult issue. For example, the greater curvature is often stretched when the operator pushes a conventional endoscope distally to access the gastric antrum, making closure of the defect challenging[14]. Interestingly, a new scheme, known as the reopenable clip-over-the-line method, allows for smooth defect closure when the MB endoscope is used[14]. Hemostasis for bleeding peptic ulcers located on the upper side of the lesser curvature is widely recognized as challenging with the conventional endoscope. The MB endoscope, however, improves the field of view and allows for better angulation owing to its dual-bending functionality, thereby enabling successful hemostasis in such difficult cases[3].
The MB endoscope can improve diagnosis and treatment when combined with other technologies. A newly developed MB endoscope, the XGIF-Q240ZMY, has the traditional characteristics of the MB endoscope as well as the characteristics of a magnifying endoscope. This combination allows for the efficient removal of lesions in various regions on the basis of the appearance of superficial mucosal capillaries during EMR. Notably, this improvement seems to be influenced by the size of the tumor being removed[15]. In addition, a novel ultrasound gastroscope, created by incorporating a high-frequency catheter probe into the MB endoscope, offers significant advancements. This design enables the high-frequency catheter probe to be more perpendicular to the plane being scanned during gastroscopy, resulting in superior ultrasound images and more accurate evaluations of certain lesions[16].
The advantages of the MB endoscope extend beyond its dual-bending functionality to include its capacity for dual-channel operation. Dual-channel operation enables smooth submucosal injection and mucosal incision during ESD, significantly enhancing surgical efficiency[6]. In addition, the dual channels also allow for the simultaneous use of two alligator forceps, enabling the efficient grasping and removal of large trichobezoars that adhere tightly to the gastric mucosa and are otherwise challenging to separate under endoscope[17].
THE MB ENDOSCOPE IN CHOLECYSTECTOMY
The MB endoscope has significantly contributed to the development and refinement of various innovative endoscopic technologies. Considering the postoperative pain, substantial tissue damage, and poor cosmetic outcomes of traditional cholecystectomy, trans-gastric cholecystectomy has been proposed. This new procedure involves accessing the abdominal cavity via the peroral trans-gastric route, where the endoscope is used to open the stomach and navigate into the abdominal cavity. However, the conventional endoscope cannot reach such areas within the upper abdominal cavity that lie above the level of the stomach[18,19]. Owing to its advanced design, the MB endoscope is expected to overcome these limitations, thereby facilitating the broader application of cholecystectomy[20].
THE MB ENDOSCOPE IN DUODENOSCOPY
The greatest impact of the MB endoscope on duodenoscopy is evident in its application in ERCP. This is reflected not only in the high surgical efficiency associated with the use of the MB endoscope for ERCP in patients with an intact gastrointestinal anatomy[21] but also in the ability to perform the procedure smoothly for patients whose ERCP procedure is likely to be difficult after gastrointestinal surgery. ERCP in patients with a history of Billroth I or Billroth II gastrectomy is likely difficult due to an altered gastrointestinal anatomy[21-24]. Although the conventional forward-viewing endoscope has circumvented some of these difficulties, selective biliary cannulation remains problematic[24,25]. The development of an MB forward-viewing endoscope and a novel second-generation MB backward-oblique viewing duodenoscope offers effective solutions to these challenges[21,24]. Although the first-generation MB backward-oblique-viewing duodenoscope poorly navigated pathological narrow areas, the upgraded second-generation model was stiffer, thereby addressing this limitation[21]. Interestingly, despite variations in the location and configuration of the papilla, the presence of a periampullary diverticulum, or tumor infiltration, the MB endoscope, with its dual-bending capability, can effectively visualize the surface of the papilla and facilitate successful bile duct cannulation[24].
THE MB ENDOSCOPE IN DIRECT POC
The diagnostic and therapeutic techniques of endoscopy in the biliary tract remain underdeveloped. POC can be classified into duodenoscopy-assisted POC systems and direct POC (DPOC), which involves direct insertion of an ultraslim endoscope into the biliary tract. DPOC may be better because of high-quality endoscopic imaging and a larger working channel[26]. However, technological limitations pose significant challenges. The conventional ultraslim endoscope with a single bend has difficulty advancing into the biliary tree, making DPOC highly challenging, thus restricting progress in biliary diagnosis and treatment[26]. Both prototype and clinical studies suggest that even with free-hand insertion and no auxiliary tools, the MB ultraslim endoscope contributes to the success of DPOC[26-28]. However, this conclusion remains controversial, as another study revealed that successful navigation of the endoscope into the biliary tract during DPOC still requires auxiliary devices, such as guidewires and anchoring balloons[29]. Owing to the ease of insertion and its high-quality imaging, the MB ultraslim endoscope is suitable for comprehensive exploration of the biliary system. This is particularly important for early screening for biliary diseases such as cholangiocarcinoma. Interestingly, the application of MB ultraslim endoscope in DPOC has also provided an effective new approach for the treatment of difficult common bile duct stones[30].
The ultraslim endoscope not only improves the efficiency of DPOC but also enables bile duct and gallbladder exploration during POC in certain cases. After ultrasound-guided choledochoduodenostomy, the placement of a lumen-apposing metal stent makes the MB ultraslim endoscope particularly suitable for exploring the hepatic ducts and the distal common bile duct. It also facilitates diagnostic and therapeutic procedures, such as stone or foreign body extraction[31]. Similarly, following endoscopic ultrasound-guided gallbladder drainage, the altered anatomical structure and the presence of a lumen-apposing metal stent allow the MB ultraslim endoscope to be used for gallbladder exploration, biopsy, and stone extraction[32]. However, this is exceedingly difficult to perform with a conventional endoscope.
Although the need for auxiliary tools for inserting the ultraslim endoscope into the biliary tract has been extensively studied, studies have suggested that the MB ultraslim endoscope can be safely used in DPOC only for patients with dilated bile ducts[33]. However, the ultraslim endoscope has significantly optimized DPOC and plays an important role in the evolution of endoscopic techniques for diagnosing and treating biliary diseases.
DISCUSSION
The MB endoscope was initially conceived to facilitate ESD in difficult-to-reach areas of the stomach[3], but its applications have since expanded across multiple endoscopic fields. By incorporating an additional bend and enabling dual-channel operation, it has improved the efficiency of endoscopic procedures. At present, this technology has been applied in gastroscopy, duodenoscopy, DPOC, and ultrasound gastroscopy, but its integration with magnifying gastroscopy for both diagnosis and treatment has also attracted significant attention. The impact of this innovation is reflected in several key areas: (1) Enhanced accessibility and precision - the MB endoscope allows access to anatomical regions that are difficult to reach with the conventional endoscope, improving operating angles in gastric ESD and EMR; (2) Improvements in ERCP - it addresses the challenges of performing ERCP in patients who have undergone Billroth I or Billroth II gastrectomy; (3) Development of DPOC - it contributes to the evolution of DPOC, paving the way for further advancements in endoscopic exploration of the bile duct tree; (4) Gallbladder application - after ultrasound-guided gallbladder drainage surgery, the MB endoscope facilitates gallbladder examination, biopsy and stone extraction; (5) Integration with other technologies - when combined with ultrasound gastroscopy and magnifying gastroscopy, it increases diagnostic and therapeutic outcomes; (6) Innovative treatment approaches - it plays a role in the development of new procedures, such as transgastric cholecystectomy and novel ESD techniques for lesions in the gastric fundus; (7) Solutions to conventional challenges - the MB endoscope has improved the management of difficult conditions, including difficult common bile duct stones, bleeding peptic ulcers in the upper lesser curvature, and closure of mucosal defects in the gastric antrum after ESD; and (8) Dual-channel benefits - the dual-channel design not only improves the efficiency of surgery but also facilitates the removal of foreign bodies that are tightly bound to the gastric mucosa, such as trichobezoars. Despite these breakthroughs, the application of the MB endoscope in colonoscopy and enteroscopy remains largely unexplored.
CONCLUSION
As the technology of MB endoscope continues to evolve, it has the potential to further reduce the invasiveness of medical procedures, enhance diagnostic precision, and expand therapeutic possibilities. However, this potential still needs to be validated through extensive research.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
P-Reviewer: Ghritlaharey RK S-Editor: Wang JJ L-Editor: A P-Editor: Wang WB