Published online Sep 16, 2024. doi: 10.4253/wjge.v16.i9.519
Revised: August 1, 2024
Accepted: August 12, 2024
Published online: September 16, 2024
Processing time: 72 Days and 23.9 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) is associated with a variety of adverse events (AEs). One of the most important AEs is post-ERCP pancreatitis (PEP), which is most common in cases of difficult biliary cannulation. Although the precut technique has been reported as a PEP risk factor, recent studies indicate that early precut could reduce PEP, and that precut itself is not a risk factor.
To evaluate the safety of the precut technique, especially in terms of PEP.
We conducted a retrospective study, spanning the period from November 2011 through December 2021. It included 1556 patients, aged ≥ 20 years, who under
The PEP incidence rate did not significantly differ between the precut and non-precut groups. However, the PEP incidence was significantly lower in the early precut group than the delayed precut group (3.5% vs 10.5%; P = 0.02). The PEP incidence in the delayed precut group without pancreatic stent insertion (17.3%) was significantly higher compared to other cases (P < 0.01).
Our findings indicate that early precut may reduce PEP incidence. If the precut decision is delayed, a pancreatic stent should be inserted to prevent PEP.
Core Tip: Early needle-knife precut papillotomy (NKPP) may significantly reduce the incidence of post-endoscopic retrograde cholangiopancreatography pancreatitis (PEP) in patients with difficult bile duct cannulation. Our single-center retrospective study found that early NKPP (EP) within 10 min of standard cannulation attempts led to a lower PEP rate compared to delayed NKPP (DP). When EP is not feasible, inserting a pancreatic stent after DP effectively prevents PEP, demonstrating a similar protective effect as EP. These findings suggest adopting EP or pancreatic stenting for delayed procedures to improve patient outcomes.
- Citation: Tanikawa T, Miyake K, Kawada M, Ishii K, Fushimi T, Urata N, Wada N, Nishino K, Suehiro M, Kawanaka M, Shiraha H, Haruma K, Kawamoto H. Can early precut reduce post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with difficult bile duct cannulation? World J Gastrointest Endosc 2024; 16(9): 519-525
- URL: https://www.wjgnet.com/1948-5190/full/v16/i9/519.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i9.519
Biliary cannulation is the first step in therapeutic endoscopic retrograde cholangiopancreatography (ERCP), and is thus crucial for a successful procedure. ERCP has a reported success rate of 67%-99.4%[1,2], and various techniques have been proposed to improve this rate, including wire-guided cannulation, the pancreatic guide-wire technique, and the two-devices-in-one-channel technique[3]. Moreover, the precut technique efficiently increases the biliary cannulation success rate, which is reported as 89.3%-91.5%[4-6]. There are no fixed criteria for selecting a method in cases with challenging biliary cannulation. Each method has advantages and disadvantages, and the endoscopist must choose an appropriate method for each case.
When selecting a procedure to maximize the probability of successful cannulation, the incidence of adverse events (AEs) is an important factor. Post-ERCP pancreatitis (PEP) is one of the most important AEs that is likely to occur in cases with difficult biliary cannulation. Some reports have indicated that the precut technique itself increases the risk of PEP[7,8]. However, recent studies have shown that early precut can reduce PEP, and that precut itself is not a risk factor[9,10]. Cennamo et al[5] reported that the timing of the precut procedure did not influence the risk of complications. These contradictory findings leave unanswered questions regarding the safety of the precut technique.
In this study, we evaluated the safety of the precut technique, especially in terms of PEP.
We performed a retrospective observational analysis. In this study, we adhered to the principles of the 1975 Helsinki Declaration, and received approval from the Institutional Research Ethics Committee (Admission No. 5984-00).
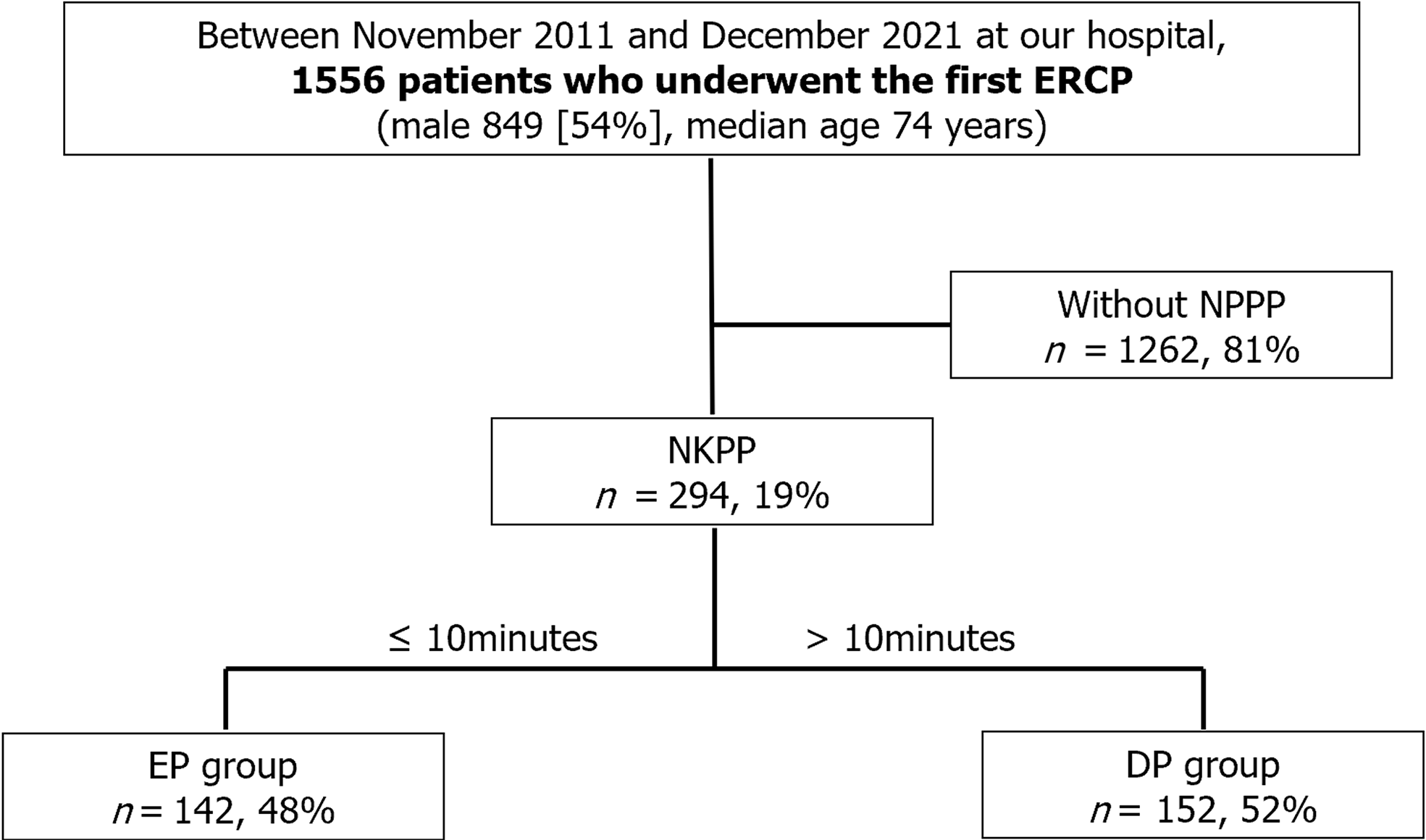
The patient selection process is illustrated in Figure 1. This retrospective study spanned the period from November 2011 through December 2021 at the Kawasaki University General Medical Center. We enrolled 1556 patients with normal gastrointestinal anatomy and naïve papilla, aged ≥ 20 years, who underwent their first ERCP procedure for biliary disease. Exclusion criteria were indication for a pancreatic procedure, pregnancy, and refusal to give informed consent.
In previous studies, early precut has been defined as initiating precut within 5-12 min of standard attempts, or after fewer than 2-4 unintended cannulation episodes into the pancreatic duct[9-11]. However, no specific definition has been established. In the present study, precut was arbitrarily defined as starting within 10 min of standard cannulation, a factor previously associated with PEP risk.
We prioritized needle-knife precut papillotomy (NKPP) over other precut techniques, because NKPP is suitable for a wide range of cases. Patients were categorized into two groups: early NKPP (EP) group (patients who received precut within 10 min) and delayed NKPP (DP) group (patients who received precut after 10 min). We compared outcomes between these groups.
Procedures were performed using a side-viewing endoscope (JF-260V or TJF-260v; Olympus Co. Ltd., Tokyo, Japan). Conventional contrast cannulation was the standard approach. In difficult cases, trainees opted for wire-guided cannulation or the pancreatic guidewire method. If selective biliary deep cannulation was not achieved within 15 min, the trainers took over, continuing with conventional contrast cannulation. For difficult cases, precut was chosen as the primary option, with no specific time limit. Precut methods typically included NKPP, needle-knife fistulotomy, transpancreatic sphincterotomy, or needle-knife sphincterotomy along with a pancreatic stent. NKPP was most commonly employed and was performed with a KD-10Q-1 instrument (Olympus), due to its adaptability and precision in incising the sphincter.
In cases of difficult cannulation or residual contrast media in the pancreatic duct after the procedure, a temporary pancreatic stent was inserted to mitigate PEP. At the end of the procedure, a guidewire was reintroduced into the pancreatic duct, and a 4Fr or 5Fr temporary plastic pancreatic stent was placed.
The primary outcome was the PEP incidence rate, diagnosed according to the Japanese acute pancreatitis guidelines. Secondary outcomes were the biliary cannulation success rate, cannulation time, and effectiveness of pancreatic stents for preventing PEP.
Statistical analyses were conducted using IBM SPSS Statistics version 26 (IBM, Armonk, NY, United States). Continuous variables were compared using the Mann-Whitney U test, and are presented as the median and interquartile range. Categorical variables were assessed using Fisher’s exact test. For all analyses, a significance level of P < 0.05 was applied.
Table 1 presents the patients’ characteristics. Precut procedures were performed in 294 patients (19%). Patients who underwent precut were significantly older than patients without precut (75.5 ± 13.0 years vs 73.6 ± 13.4 years; P = 0.016). The incidence of malignant disease was significantly higher among patients who received precut compared to those without precut. The PEP incidence rate did not significantly differ between the two groups (7.1% vs 5.4%; P = 0.27). However, there were significant differences in the cannulation success rate (96.3% vs 99.0%; P < 0.01), cannulation time (20.3 ± 12.6 min vs 5.1 ± 7.2 min; P < 0.01), and total procedure time (40.4 ± 16.0 min vs 29.7 ± 17.9 min; P < 0.01).
| Characteristic | NKPP, n = 294 | Non-NKPP, n = 1262 | P value |
| Age | 75.5 ± 13.0 | 73.6 ± 13.4 | 0.016 |
| Sex, male | 159 (53.7) | 690 (54.6) | 0.80 |
| Diagnosis | < 0.01 | ||
| Benign | 205 (69.3) | 980 (77.6) | |
| Malignancy | 91 (30.7) | 283 (22.4) | |
| Diverticula | 77 (26.0) | 380 (30.1) | 0.18 |
| First endoscopist | 0.050 | ||
| Trainee, n = 903 | 156 (53.0) | 747 (59.2) | |
| Success rate of cannulation | 283 (96.3) | 1250 (99.0) | < 0.01 |
| Cannulation time in min | 20.3 ± 12.6 | 5.1 ± 7.2 | < 0.01 |
| Total procedure time in min | 40.4 ± 16.0 | 29.7 ± 17.9 | < 0.01 |
| PEP | 21 (7.1) | 68 (5.4) | 0.27 |
The EP and DP groups did not significantly differ in terms of age, sex, diagnosis, or diverticula. Precut techniques were initiated at 5.7 ± 3.1 min into the procedure in the EP group, and 17.1 ± 5.6 min into the procedure in the DP group. The PEP incidence was significantly lower in the EP group, compared to the DP group (3.5% vs 10.5%; P = 0.02). The EP and DP group also significantly differed in the cannulation success rate (98.6% vs 94.1%; P = 0.03), cannulation time (13.2 ± 8.6 min vs 27.3 ± 12.0 min; P < 0.01), and total procedure time (35.0 ± 15.7 min vs 45.8 ± 14.4 min; P < 0.01) (Table 2).
| Characteristic | EP group, n = 142 | DP group, n = 152 | P value |
| Age | 74.8 ± 13.6 | 76.3 ± 12.4 | 0.39 |
| Sex, male | 81 (57) | 77 (50.7) | 0.29 |
| Diagnosis | |||
| Benign | 101 (71.1) | 103 (67.8) | 0.61 |
| Malignancy | 41 (28.9) | 49 (32.2) | |
| Diverticula | 30 (21.1) | 47 (37.6) | 0.064 |
| First endoscopist | < 0.01 | ||
| Trainee, n = 154 | 43 (30.3) | 111 (73.0) | |
| Trainer, n = 141 | 99 (69.7) | 41 (27.0) | |
| NKPP start time in min | 5.7 ± 3.1 | 17.1 ± 5.6 | < 0.01 |
| Success rate of cannulation | 140 (98.6) | 143 (94.1) | 0.027 |
| Cannulation time in min | 13.2 ± 8.6 | 27.3 ± 12.0 | < 0.01 |
| Total procedure time in min | 35.0 ± 15.7 | 45.8 ± 14.4 | < 0.01 |
| PEP | 5 (3.5) | 16 (10.5) | 0.023 |
We inserted an endoscopic pancreatic stent (EPS) in 140 patients (47.6%) who received precut, including 63 patients (44.4%) in the EP group, and 77 patients (50.7%) in the DP group. The findings are presented in Table 3. Notably, patients in the DP group without an EPS had a significantly higher incidence of PEP (17.3%) compared with the incidence rates in other cases (P < 0.01). Conversely, among patients in the EP group, the PEP incidence did not differ according to EPS use. Notably, cases with delayed precut and EPS placement exhibited a PEP incidence comparable to cases involving early precut without an EPS.
| Complication | EP group, n = 142 | DP group, n = 152 | P value | ||
| Without EPS, n = 79 | With EPS, n = 63 | Without EPS, n = 75 | With EPS, n = 77 | ||
| PEP | 3 (3.8) | 2 (3.2) | 13 (17.3) | 3 (3.9) | < 0.01a |
The present study yielded three key findings. First, the precut technique itself was not a risk factor for PEP. Second, the PEP incidence was lower following early implementation of the precut technique, compared to delayed precut procedures. Third, EPS insertion after delayed precut had a PEP-preventive effect similar to that of early precut.
The precut technique has been considered a PEP risk factor[7,12,13], but it has been unclear whether this association is due to the precut itself or to the prolonged procedure and inadvertent pancreatic duct cannulation. Previous studies have suggested that the reduced PEP incidence with early precut indicated an influence of prolonged procedures[9-11]. Our present findings confirmed that the precut technique itself was not linked to higher PEP risk; however, a delay in precut performance significantly increased the PEP incidence. Bailey et al[14] reported that NKPP was not an independent predictor of PEP. Conversely, our findings demonstrated that early precut could prevent PEP. Hence, we infer that PEP may be induced by prolonged stimulation of the papilla and pancreatic duct leading up to the precut, rather than by the precut technique itself, which has been previously reported[14-16]. Notably, our study focused on the technique itself, and further research is needed to investigate the safety of DP independently of the prolonged stimulation. Future studies should endeavor to isolate these variables, to better understand their individual contributions to PEP risk.
There are situations where early implementation of the precut technique is not feasible. Notably, in ERCP training facilities, trainees often initiate the procedure as the operator. Among the cases in the present study, trainees initiated the procedure in 30.3% of cases in the EP group, and 73.0% in the DP group (P < 0.01). Many aspects of ERCP training require hands-on experience, and some cases pose difficulties such that precut cannot be performed within 10 min. In this study, such cases exhibited a higher risk of PEP. Moreover, it was evident that EPS could prevent PEP in DP cases. EPS insertion reduced the PEP incidence in cases where precut could not be performed within 10 min, bringing it to a level comparable to that in cases with early precut. In other words, EPS prevented PEP as well as early precut did. Zagalsky et al[17] also reported that early precut had a PEP-preventive effect comparable to that of a pancreatic stent. The ESGE guidelines recommend that a pancreatic duct stent should be placed when NKPP is performed, even when pancreatic cannulation is easily obtained[18]. However, we found that EPS placement had no significant PEP-preventative effect in cases where precut was performed within 10 min. We suggest that EPS placement might not be necessary in cases with early precut, but should be performed in cases with delayed precut.
This study had several limitations, including the retrospective study design, and the fact that it was conducted only in our hospital. Additionally, there was no standard definition of early precut, and many other PEP risk factors were included during the procedure. We could not strictly evaluate the risk of precut, because we did not compare precut cases vs difficult cannulation cases without precut. Finally, the study included a variety of endoscopists, whose technical skill differences may have affected the PEP incidence. To more thoroughly evaluate the early precut technique, we should plan a multicenter prospective study.
In conclusion, our findings indicate that early precut may reduce the incidence of PEP. When encountering cases in which it is difficult to achieve biliary cannulation, it may be preferable to choose the early precut technique rather than repeating conventional cannulation. If the precut decision is delayed, a pancreatic stent should be inserted to prevent PEP.
We gratefully acknowledge all of the participants who participated in the study and the study team for their support.
| 1. | Wang X, Luo H, Tao Q, Ren G, Wang X, Liang S, Zhang L, Chen L, Shi X, Guo X, Pan Y. Difficult biliary cannulation in ERCP procedures with or without trainee involvement: a comparative study. Endoscopy. 2022;54:447-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 2. | Cortas GA, Mehta SN, Abraham NS, Barkun AN. Selective cannulation of the common bile duct: a prospective randomized trial comparing standard catheters with sphincterotomes. Gastrointest Endosc. 1999;50:775-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Gonzalez JM, Debourdeau A, Barthet M. How to facilitate cannulation of an intradiverticular papilla: a technique with two devices in one channel using pediatric forceps. Endoscopy. 2019;51:1095-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Zhou PH, Yao LQ, Xu MD, Zhong YS, Gao WD, He GJ, Zhang YQ, Chen WF, Qin XY. Application of needle-knife in difficult biliary cannulation for endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int. 2006;5:590-594. [PubMed] |
| 5. | Cennamo V, Fuccio L, Repici A, Fabbri C, Grilli D, Conio M, D'Imperio N, Bazzoli F. Timing of precut procedure does not influence success rate and complications of ERCP procedure: a prospective randomized comparative study. Gastrointest Endosc. 2009;69:473-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 6. | Zhang QS, Xu JH, Dong ZQ, Gao P, Shen YC. Success and Safety of Needle Knife Papillotomy and Fistulotomy Based on Papillary Anatomy: A Prospective Controlled Trial. Dig Dis Sci. 2022;67:1901-1909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 7. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1703] [Article Influence: 56.8] [Reference Citation Analysis (2)] |
| 8. | Testoni PA, Mariani A, Giussani A, Vailati C, Masci E, Macarri G, Ghezzo L, Familiari L, Giardullo N, Mutignani M, Lombardi G, Talamini G, Spadaccini A, Briglia R, Piazzi L; SEIFRED Group. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol. 2010;105:1753-1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 210] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 9. | Mariani A, Di Leo M, Giardullo N, Giussani A, Marini M, Buffoli F, Cipolletta L, Radaelli F, Ravelli P, Lombardi G, D'Onofrio V, Macchiarelli R, Iiritano E, Le Grazie M, Pantaleo G, Testoni PA. Early precut sphincterotomy for difficult biliary access to reduce post-ERCP pancreatitis: a randomized trial. Endoscopy. 2016;48:530-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 10. | Manes G, Di Giorgio P, Repici A, Macarri G, Ardizzone S, Porro GB. An analysis of the factors associated with the development of complications in patients undergoing precut sphincterotomy: a prospective, controlled, randomized, multicenter study. Am J Gastroenterol. 2009;104:2412-2417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Tang SJ, Haber GB, Kortan P, Zanati S, Cirocco M, Ennis M, Elfant A, Scheider D, Ter H, Dorais J. Precut papillotomy versus persistence in difficult biliary cannulation: a prospective randomized trial. Endoscopy. 2005;37:58-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Chiriac S, Sfarti CV, Stanciu C, Cojocariu C, Zenovia S, Nastasa R, Trifan A. The Relation between Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis and Different Cannulation Techniques: The Experience of a High-Volume Center from North-Eastern Romania. Life (Basel). 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Ding X, Zhang F, Wang Y. Risk factors for post-ERCP pancreatitis: A systematic review and meta-analysis. Surgeon. 2015;13:218-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 111] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 14. | Bailey AA, Bourke MJ, Kaffes AJ, Byth K, Lee EY, Williams SJ. Needle-knife sphincterotomy: factors predicting its use and the relationship with post-ERCP pancreatitis (with video). Gastrointest Endosc. 2010;71:266-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 98] [Article Influence: 6.1] [Reference Citation Analysis (1)] |
| 15. | Glomsaker T, Hoff G, Kvaløy JT, Søreide K, Aabakken L, Søreide JA; Norwegian Gastronet ERCP Group. Patterns and predictive factors of complications after endoscopic retrograde cholangiopancreatography. Br J Surg. 2013;100:373-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 16. | Katsinelos P, Lazaraki G, Chatzimavroudis G, Gkagkalis S, Vasiliadis I, Papaeuthimiou A, Terzoudis S, Pilpilidis I, Zavos C, Kountouras J. Risk factors for therapeutic ERCP-related complications: an analysis of 2,715 cases performed by a single endoscopist. Ann Gastroenterol. 2014;27:65-72. [PubMed] |
| 17. | Zagalsky D, Guidi MA, Curvale C, Lasa J, de Maria J, Ianniccillo H, Hwang HJ, Matano R. Early precut is as efficient as pancreatic stent in preventing post-ERCP pancreatitis in high-risk subjects - A randomized study. Rev Esp Enferm Dig. 2016;108:258-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Dumonceau JM, Andriulli A, Elmunzer BJ, Mariani A, Meister T, Deviere J, Marek T, Baron TH, Hassan C, Testoni PA, Kapral C; European Society of Gastrointestinal Endoscopy. Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - updated June 2014. Endoscopy. 2014;46:799-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 378] [Cited by in RCA: 417] [Article Influence: 34.8] [Reference Citation Analysis (0)] |