Published online Dec 27, 2025. doi: 10.4254/wjh.v17.i12.110764
Revised: July 8, 2025
Accepted: November 14, 2025
Published online: December 27, 2025
Processing time: 195 Days and 18.1 Hours
Laparoscopic hepatectomy has been widely accepted for the treatment of liver tumors. Compared with open surgery, it provides a reduced hospital stay, less intraoperative blood loss, less trauma, and fewer incisional infections, without af
To investigate the safety and efficacy of laparoscopic retroperitoneal partial hepa
The clinical data of 72 patients who underwent laparoscopic retroperitoneal partial hepatectomy for liver tumors between January 2018 and December 2024 at the First People’s Hospital of Yunnan Province were analyzed. Of the 72 patients included, 34 were male and 38 were female, with ages ranging from 34 years to 72 years (median age, 45 years). The tumors were all located in the right lobe of the liver, with 30 cases in segment S6, 27 cases in segment S7, and 15 cases in segment S8; the mean tumor diameter was 7.5 ± 3.4 cm. The postoperative tumor indices, liver function, and postoperative complications were analyzed to evaluate the clinical efficacy of laparoscopic partial hepatectomy via the retroperitoneal approach.
The surgeries were successfully completed in all patients, and conversion to open surgery was required in 10 patients. The mean operative time, blood loss, drain retention time, and length of postoperative hospital stay were 140 ± 30 minutes, 150 ± 46 mL, 3.8 ± 1.2 days, and 8.3 ± 5.3 days, respectively. Liver function tests returned to normal in all patients within two weeks of surgery. Fifteen patients developed atelectasis and pleural effusion and were managed with incision and drainage and antibiotics. Two patients developed uncomplicated minimal ascites, and the remaining patients had no perioperative complications, such as abdominal hemorrhage, infection, liver failure, bile leakage, and other adverse events. All patients were successfully treated.
Laparoscopic retroperitoneal partial hepatectomy is a safe and effective approach for right hepatic space-occupying lesions, particularly in segments S6, S7, and S8, with fewer postoperative complications, less trauma, and faster recovery times. This procedure provides a new surgical access for resection of deep tumors in the right lobe of the liver and has clear clinical implications.
Core Tip: Laparoscopic retroperitoneal partial hepatectomy is a safe and effective approach for right hepatic space-occupying lesions, particularly in segments S6, S7, and S8, with fewer postoperative complications, less trauma, and faster recovery times.
- Citation: Fei ZH, Duan XF, Feng LH, Wang ZN, Chen YS, Sun ZW. Clinical study on the efficacy of laparoscopic hepatectomy via the retroperitoneal approach for treating liver tumors. World J Hepatol 2025; 17(12): 110764
- URL: https://www.wjgnet.com/1948-5182/full/v17/i12/110764.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i12.110764
Laparoscopic hepatectomy has been widely accepted for the treatment of liver tumors[1-3]. Compared with open surgery, it provides reduced hospital stay, less intraoperative blood loss, less trauma, and fewer incisional infections, without affecting tumor outcomes[4-6]. However, lesions in the right lobe of the liver are deep and obstructed by the ribs, making exposure difficult and increasing the degree of surgical difficulty. Liver tumors in the deep right lobe pose technical challenges in standard laparoscopic surgery[7-9]. To address this challenge, various techniques and approaches have been proposed, such as changing the surgical approach[8], fluorescence laparoscopy-assisted surgery[10], liver sus
A total of 72 patients underwent laparoscopic hepatectomy via the retroperitoneal approach at the First People's Hospital of Yunnan Province from January 2017 to December 2024. This procedure was performed by the same surgical team, and the patients’ general data, perioperative outcomes, and follow-up data were recorded.
The inclusion criteria were as follows: (1) Tumor location confined to hepatic segments S6, S7, or S8; (2) No vascular, bile duct, or lymph node invasion by the tumor; (3) Preoperative Child-Pugh class A or B liver function; and (4) Normal cardiorespiratory function without contraindications to anesthesia.
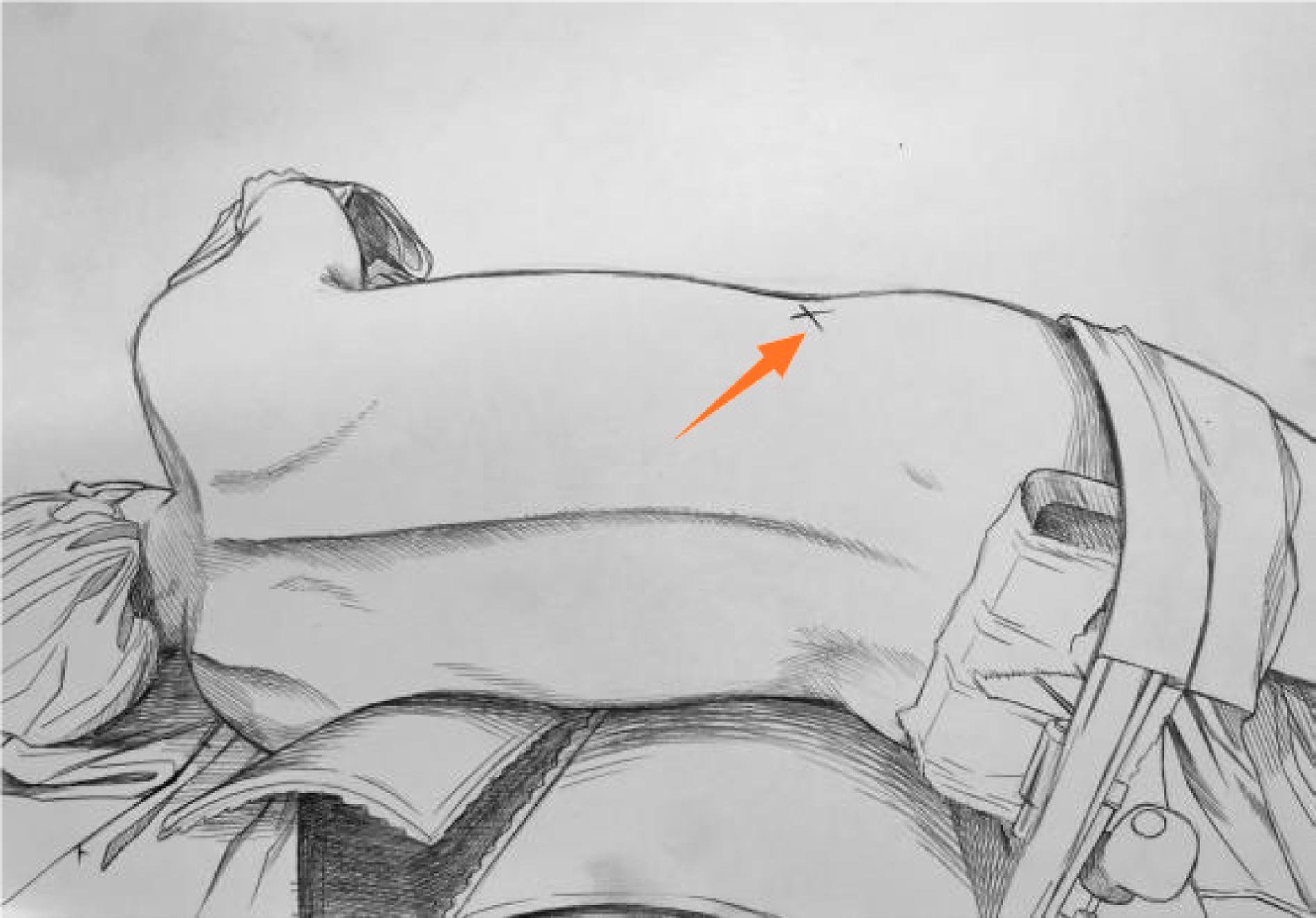
The patient was placed in the left lateral decubitus position for the procedure. After successful general anesthesia, the left lumbar bridge was elevated, and routine disinfection and draping were carried out. A 4-cm transverse incision was made three finger-breadths above the intersection of the right mid-axillary line and iliac crest (the incision site is indicated by the arrow in Figure 1). Blunt finger dissection was performed to create a space that was expanded using a self-made balloon from surgical gloves (a 12-mm trocar and grasping forceps were inserted at the site indicated by the arrow in Figure 2). A 10–12-mm trocar and a grasper were inserted and sutured in place. (Intraoperative laparoscopic instruments demonstrated an inverted triangular configuration in Figure 3).
Using a harmonic scalpel, the perirenal fascia and adipose tissue were dissected to access the perirenal space (Figure 4A and B). The abdominal cavity was explored, and the hepatic ligaments were mobilized to release adhesions on the liver surface, fully exposing the right hepatic lobe. Elevation of the liver revealed the first hepatic hilum. A laparoscopic ultrasound probe was used to localize the lesions. The Pringle maneuver was used for portal triad clamping. A pre-resection line was marked 1 cm from the tumor margin. Small blood vessels and bile ducts were clipped and divided, and large structures were transected and stapled using a linear cutter. The tumor was completely resected (the tumor measured approximately 7 cm in diameter as shown in Figure 4C), and retrieved in a specimen bag, and a drain was placed on the hepatic resection surface (Figure 4D).
Statistical analyses were performed using SPSS software (version 22.0). Normally distributed data, such as operative time, are expressed as mean ± SD, while skewed distributed data, such as postoperative hospital stay, are presented as M (Min–Max). Categorical data are expressed as n (%).
A total of 72 patients were included, consisting of 34 males (47.2%) and 38 females (52.8%), with a median age of 45 years (range: 34-72 years). The mean body mass index was 23.14 ± 3.27 kg/m². Liver function was Child-Pugh class A in 67 patients (93%) and class B in 5 patients (7%). Comorbid cirrhosis was present in 20 patients (27.8%), and 10 patients (13.8%) had a history of abdominal surgery.
Of the 72 patients, 21 had benign diseases, including 16 with hemangiomas (22%), 4 with focal nodular hyperplasia (FNH, 6%), and 1 with intrahepatic bile duct stone (1%). Malignant tumors accounted for 51 cases, including 45 hepatocellular carcinomas (63%) and 6 colorectal liver metastases (all non-synchronous surgeries, 8%). The mean tumor diameter was 7.5 ± 3.4 cm. All tumors were in the right liver lobe, with 30 cases in segment S6 (42%), 27 in segment S7 (38%), and 15 in segment S8 (20%). Preoperative aspartate aminotransferase (AST) level was 25.52 ± 4.23 U/L, and preoperative alanine transferase (ALT) level was 27 ± 11.42 U/L.
All patients successfully completed surgery, with an average operative time of 140 ± 30 minutes and intraoperative blood loss of 150 ± 46 mL. Ten cases (13.8%) were converted to open surgery: 5 (50%) due to uncontrolled bleeding on the hepatic resection surface; 3 (30%) due to deeply located tumors adjacent to major blood vessels, making exposure difficult; and 2 (20%) due to large tumor size (both > 5 cm in diameter).
Postoperative AST levels were 124.35 ± 29.35 U/L and ALT levels were (109 ± 32.75) U/L on day 1, decreasing to (57.89 ± 19.35) U/L (AST) and (55 ± 21.75) U/L (ALT) by day 3. Liver function normalized in all patients within two weeks postoperatively.
Postoperative complications of mild atelectasis and pleural effusion occurred in 15 patients, which resolved with incision and drainage and antibiotics, and minimal ascites occurred in two patients. The average postoperative hospital stay was 8.3 ± 5.3 days. Pathological examination confirmed negative resection margins in all 51 malignant tumor cases, with clear diagnostic confirmation (Tables 1, 2, and 3).
| Variables | n (%) |
| Sex (male) | 34 (47) |
| Age (years, mean ± SD) | 45 (34-72) |
| BMI (kg/m², mean ± SD) | 23.14 ± 3.27 |
| Child-Pugh classification | |
| Child-Pugh A | 67 (93) |
| Child-Pugh B | 5 (7) |
| Past medical history | |
| Liver cirrhosis | 20 (28) |
| History of lung surgery | 10 (14) |
| Benign liver diseases | |
| Hemangioma | 16 (22) |
| FNH | 4 (6) |
| Hepatolithiasis | 1 (1) |
| Malignant liver tumors | |
| HCC | 45 (63) |
| CRLM | 6 (8) |
| Tumor diameter (cm) | 7.5 ± 3.4 |
| Anatomical location | |
| S6 | 30 (42) |
| S7 | 27 (38) |
| S8 | 15 (20) |
| Variables | mean ± SD/n (%) |
| Operative time (minutes) | 140 ± 30 |
| Intraoperative blood loss (mL) | 150 ± 46 |
| Conversion to open surgery | 10 (13.8) |
| Postoperative complications | |
| Atelectasis and pleural effusion | 15 |
| Ascites | 2 |
| Postoperative length of stay (days) | 8.3 ± 5.3 |
| Times | mean ± SD |
| Preoperative AST | 25.52 ± 4.23 |
| Preoperative ALT | 27.00 ± 11.42 |
| Postoperative day 1 AST | 124.35 ± 29.35 |
| Postoperative day 1 ALT | 109.00 ± 32.75 |
| Postoperative day 3 AST | 57.89 ± 19.55 |
| Postoperative day 3 ALT | 55.00 ± 21.75 |
The retroperitoneal laparoscopic approach was used initially for urological surgery, during which renal and adrenal tumors often infiltrate the liver, requiring a combined hepatectomy[14-16]. The retroperitoneal laparoscopic approach is feasible as it provides clear exposure to the surrounding anatomy during resection.
The bare area of the liver can be directly accessed by creating a channel through the anatomical space between the bare area of the liver and the right adrenal gland. With sufficient mobilization of the perihepatic ligaments, an operative space can be created. Additionally, the retroperitoneal approach causes less interference in cardiopulmonary function and avoids dissection of the intra-abdominal organs[17]. In 2011, studies reported[17] that retroperitoneal hepatectomy for small tumors in the superficial right posterior segment of the liver was safe and feasible. This approach can significantly shorten operative time and reduce extensive liver resection, although it is not suitable for all right lobe tumors.
Survival analysis of patients with malignant tumors was not carried out in this study due to the long time span and missing follow-up information of some patients, which affects the evaluation of surgical outcomes.
In this study, 10 patients required conversion to open surgery, indicating the limitation of the technique. The retroperitoneal approach is challenging for large and deep parenchymal hepatic tumors as the single-channel setup complicates hemostatic suturing during significant bleeding. Common postoperative complications are pleural effusion and atelectasis, likely due to diaphragmatic irritation from liver manipulation during surgery[18].
Compared with relevant studies[19-21], our study showed reduced intraoperative blood loss and shorter operative time with laparoscopic hepatectomy. However, the retroperitoneal approach to the liver’s bare area precludes routine abdominal cavity exploration, requiring positional changes for anterior access and potentially causing procedural inconvenience[22]. Based on this study, the recommended indications for this procedure are tumor diameter ≤ 5 cm; preoperative confirmation of no vascular, biliary, or lymph node metastasis; subcapsular or superficial tumor position.
This study has some shortcomings, being a single-center retrospective study, there is inevitably selection bias. As a new surgical procedure, no control group was included in the study, but this procedure was not inferior to the concurrent transabdominal laparoscopic surgery in terms of operative time and intraoperative bleeding over the same time period. Retroperitoneal laparoscopic hepatectomy is a useful clinical technique that further expands the indications and surgical options for laparoscopic liver resection. However, this procedure is difficult and surgically skillful as it lacks the abdominal exploration step and requires strict preoperative evaluation. We will further refine the surgical indications for the transperitoneal retroperitoneal approach in subsequent studies.
| 1. | Goh BKP, Teo JY, Chan CY, Lee SY, Cheow PC, Chung AYF. Laparoscopic repeat liver resection for recurrent hepatocellular carcinoma. ANZ J Surg. 2017;87:E143-E146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Katkhouda N, Mavor E. Laparoscopic management of benign liver disease. Surg Clin North Am. 2000;80:1203-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Mondragón-Sánchez R, Gómez-Gómez E, Mondragón-Sánchez A, Bernal-Maldonado R, Hernández-Castillo E. [Laparoscopic liver surgery]. Rev Gastroenterol Mex. 2004;69 Suppl 1:91-98. [PubMed] |
| 4. | Han HS, Shehta A, Ahn S, Yoon YS, Cho JY, Choi Y. Laparoscopic versus open liver resection for hepatocellular carcinoma: Case-matched study with propensity score matching. J Hepatol. 2015;63:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 211] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 5. | Sotiropoulos GC, Machairas N, Stamopoulos P, Kostakis ID, Dimitroulis D, Mantas D, Kouraklis G. Laparoscopic versus open liver resection for hepatocellular carcinoma: initial experience in Greece. Ann Gastroenterol. 2016;29:521-529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Komatsu S, Brustia R, Goumard C, Perdigao F, Soubrane O, Scatton O. Laparoscopic versus open major hepatectomy for hepatocellular carcinoma: a matched pair analysis. Surg Endosc. 2016;30:1965-1974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Cao J, Li WD, Zhou R, Shang CZ, Zhang L, Zhang HW, Lau WY, Chen YJ. Totally laparoscopic anatomic S7 segmentectomy using in situ split along the right intersectoral and intersegmental planes. Surg Endosc. 2021;35:174-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Peng JX, Li HL, Ye Q, Mo JQ, Wang JY, Liu ZY, He JM. Laparoscopic anatomical SVIII resection via middle hepatic fissure approach: Caudal or cranio side. World J Gastrointest Surg. 2024;16:3685-3693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Imamura T, Yamamoto Y, Morimura R, Ikoma H, Arita T, Konishi H, Shiozaki A, Kubota T, Fujiwara H, Otsuji E. Association between surgical difficulty and tumor location based on subsegments of the Glisson branches in laparoscopic liver resection. Ann Gastroenterol Surg. 2025;9:546-558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Ji L, Wang X, Li J, Cao J. ASO Author Reflections: Laparoscopic Anatomic S8 Resection: The Taping Game has Taken the Stage. Ann Surg Oncol. 2024;31:9233-9234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Kim JH. Modified liver hanging maneuver focusing on outflow control in pure laparoscopic left-sided hepatectomy. Surg Endosc. 2018;32:2094-2100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Kong X, Niu Z, Wang H, Liu M, Ma C, Lu J, Zhou X, Zhu H. Left-lateral decubitus jackknife position for laparoscopic resection of right posterior liver tumors: A safe and effective approach. Langenbecks Arch Surg. 2025;410:25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Chen Y. Clinical Experience Of The Single-Incision “Plus” Laparoscopic Hepatectomy:A Single-Center Study With 301 Cases. HPB. 2019;21:S196. [DOI] [Full Text] |
| 14. | Takamori H, Uetani M, Yoshida T, Ban D, Nakamura E, Fujimoto H, Matsui Y. [A Case of Metastatic Adrenal Tumor with Liver Infiltration which was Successfully Resected by Laparoscopic Surgery Using Both Intraperitoneal and Retroperitoneal Approaches]. Hinyokika Kiyo. 2022;68:179-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Otsuka I, Kida K, Terada N, Kiwaki T, Nanashima A, Kamoto T. Malignant pheochromocytoma with liver invasion treated successfully by combined retroperitoneal laparoscopic control of arterial in-flow followed by open hepatectomy: A case report. Int J Surg Case Rep. 2021;81:105763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Ong KH, Huang SK, Yen CS, Tian YF, Sun DP. Simultaneous Retroperitoneal Robotic Partial Nephrectomy and Hepatectomy for Synchronous Renal-Cell Carcinoma and Hepatocellular Carcinoma in a Cirrhotic Patient. J Endourol Case Rep. 2016;2:215-217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Hu M, Zhao G, Xu D, Ma X, Liu R. Retroperitoneal laparoscopic hepatectomy: a novel approach. Surg Laparosc Endosc Percutan Tech. 2011;21:e245-e248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Matsuo Y, Nomi T, Hokuto D, Yoshikawa T, Kamitani N, Sho M. Pulmonary complications after laparoscopic liver resection. Surg Endosc. 2021;35:1659-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Gon H, Komatsu S, Soyama H, Tanaka M, Kido M, Fukushima K, Urade T, So S, Yoshida T, Arai K, Tsugawa D, Yanagimoto H, Toyama H, Fukumoto T. Impact of depth of body cavity at the upper-right portion of the abdomen on open and laparoscopic liver resection of segment 7. Langenbecks Arch Surg. 2025;410:37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Jang EJ, Kim KW. Early experience of laparoscopic liver resection: A single institution experience with 37 consecutive cases. Ann Hepatobiliary Pancreat Surg. 2019;23:115-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 21. | Wang Y, Lu S, Tan X, Xie S, Liang G, Liang H, Guo J, Yuan G, Yu S, He S. Liver resection in stage 0-A HCC in segments 7/8: a propensity-matched analysis comparing open, laparoscopic, and robotic approach. Surg Endosc. 2025;39:1902-1914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 22. | Hirose S, Ban D, Matsui Y, Mizui T, Miyata A, Nara S, Esaki M. Laparoscopic liver resection with retroperitoneoscopy for the treatment of right dorsal liver tumors (with video). Surg Today. 2025;55:723-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/