Copyright
©The Author(s) 2025.
World J Hepatol. Sep 27, 2025; 17(9): 110264
Published online Sep 27, 2025. doi: 10.4254/wjh.v17.i9.110264
Published online Sep 27, 2025. doi: 10.4254/wjh.v17.i9.110264
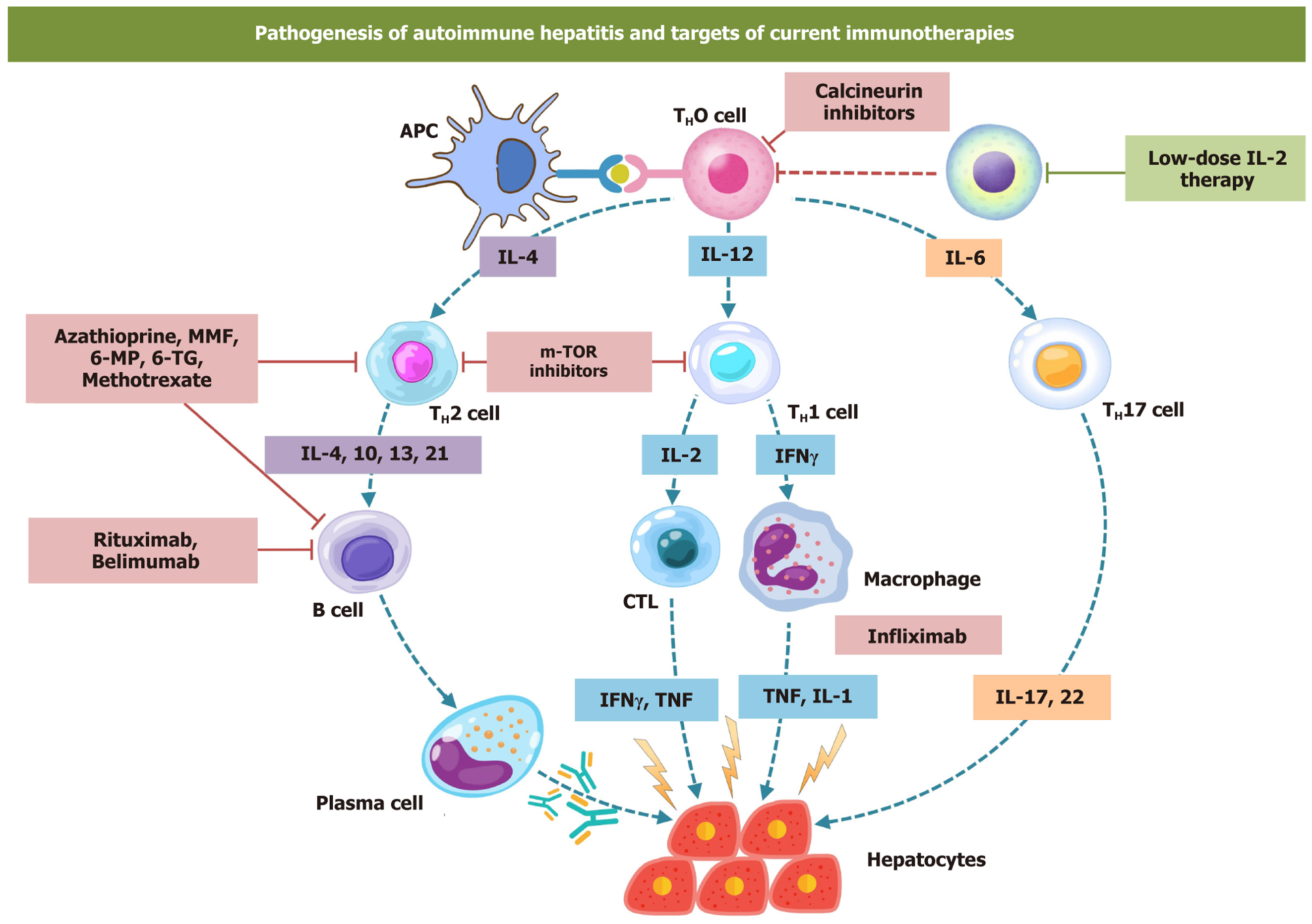
Figure 1 Pathogenesis of autoimmune hepatitis and pharmacological targets.
Immunopathogenesis of autoimmune hepatitis (AIH) involves adaptive and innate immune systems. Molecular mimicry and breakdown of self-antigenic tolerance lead to activation of B and T cells. B cells in turn stimulate plasma cells which secret autoantibodies. Cytotoxic T cells and autoantibodies lead to hepatotoxicity. Immunosuppressive therapies target various pathways of the pathogenesis in AIH as depicted in the figure. Methotrexate, azathioprine, 6-mercaptopurine, and 6-thioguanine interfere with cell cycles and arrest the proliferation of B and T cells. Infliximab is a chimeric anti-tumor necrosis factor antibody that acts on the downstream inflammatory pathways. Rituximab and belimumab deplete B cells and attenuate B-cell-mediated activations of plasma cells. Calcineurin inhibitors like tacrolimus and cyclosporine preferably act on T cell proliferation. Sirolimus is a mammalian target of rapamycin inhibitor that ameliorates helper T cells-mediated tissue damage in the liver cells. MMF: Mycophenolate mofetil; 6-MP: 6-mercaptopurine; 6-TG: 6-thioguanine; IL: Interleukin; m-TOR: Mammalian-target of rapamycin; IFNγ: Interferon-gamma; CTL: Cytotoxic T lymphocytes; TNF: Tumor necrosis factor.
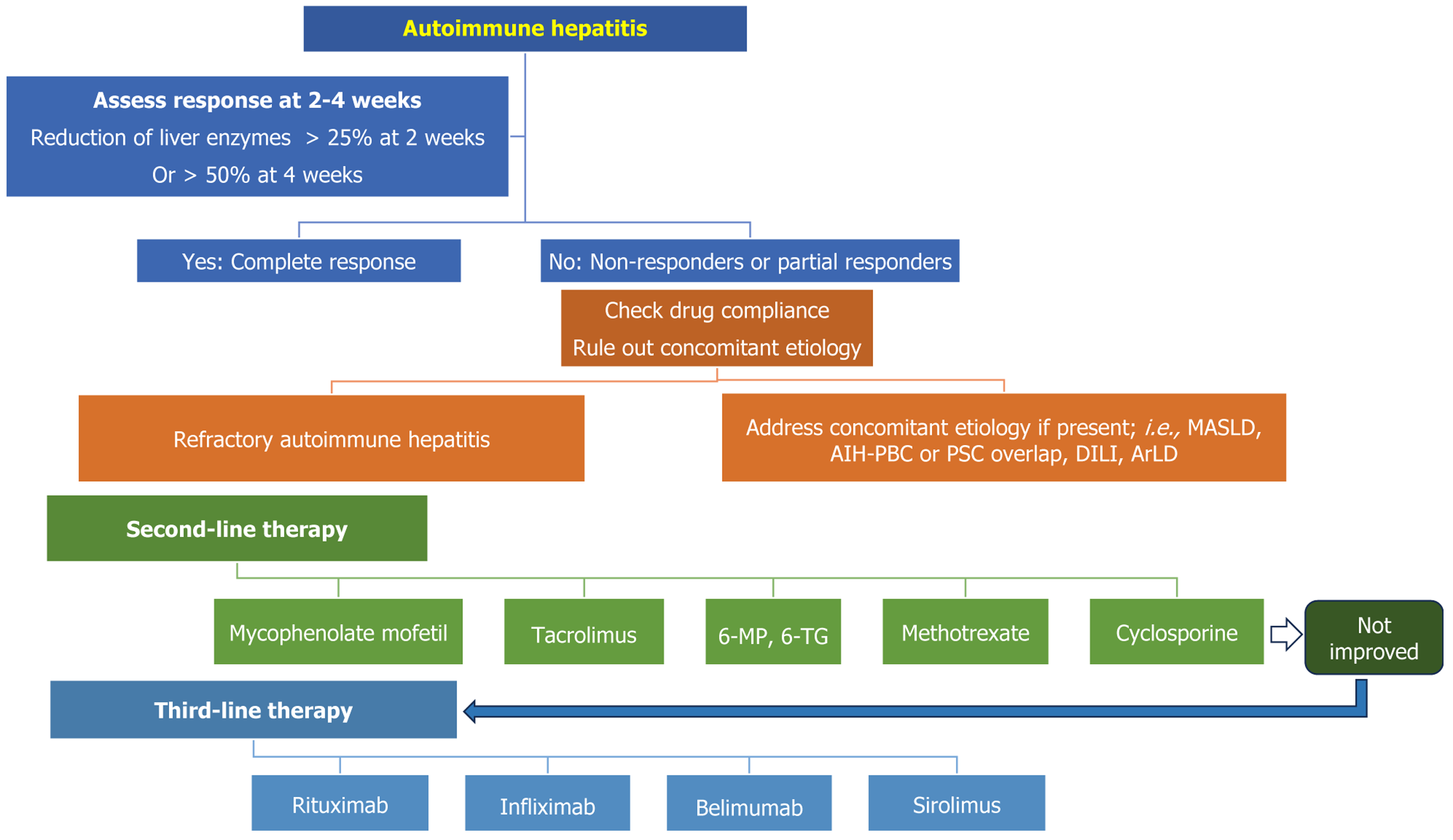
Figure 2 Indication of second- and third-line immunosuppressive therapy in patients with autoimmune hepatitis.
Following primary immu
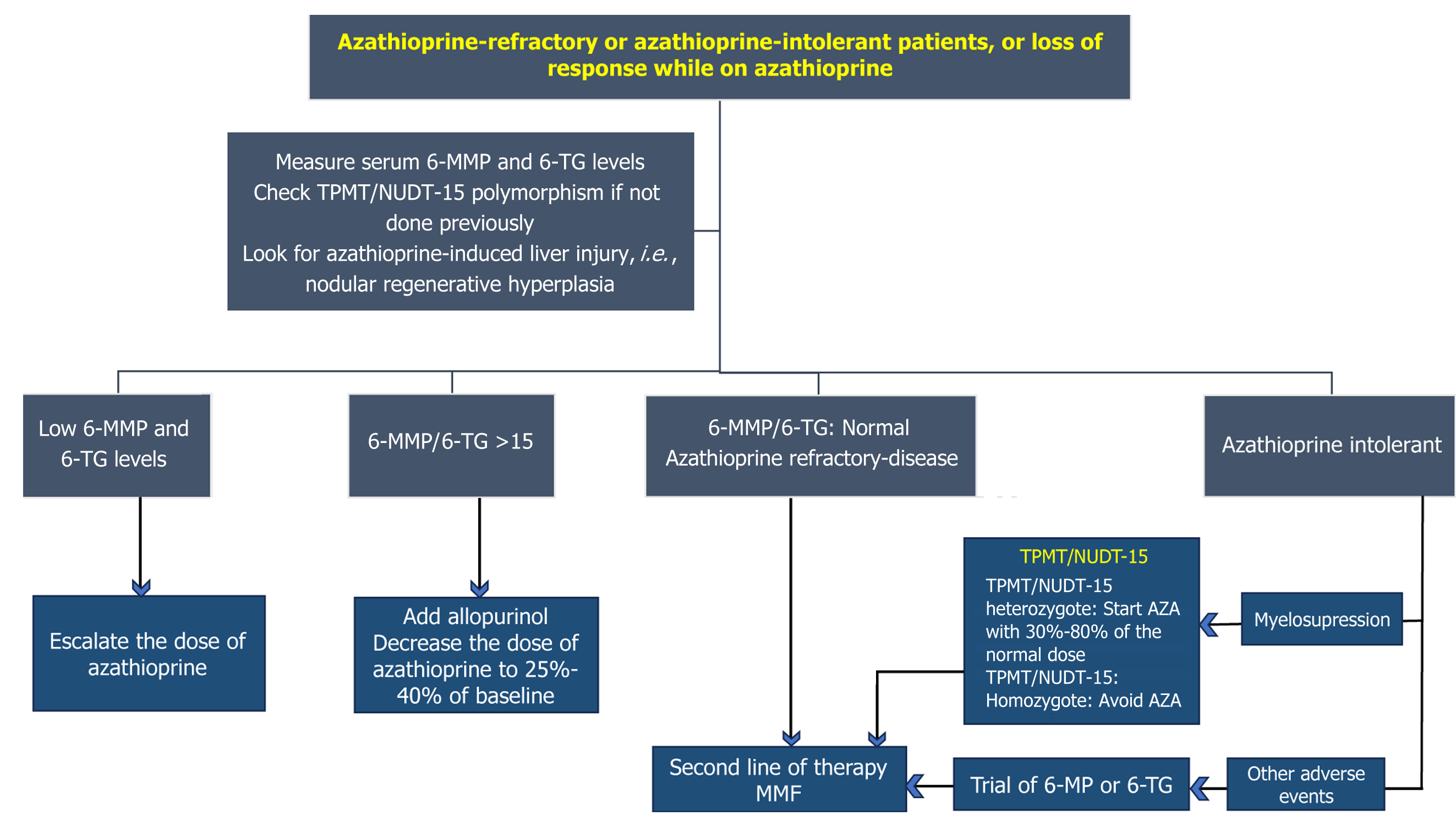
Figure 3 Managing patients with autoimmune hepatitis who are intolerant or refractory to azathioprine or 6-mercaptopurine.
Azathioprine and 6-mercaptopurine are associated with bone marrow suppression and hepatotoxicity. Baseline TPMT and NUDT-15 genetic polymorphism testing is advocated to avoid myelosuppression. It should be avoided in patients who are homozygous for both enzymes. About 10%–20% of patients who are intolerant to azathioprine can be salvaged with 6-MP or MMF; however, AZA-refractory cases do not respond well to 6-MP. They will often require a third line of therapy or MMF. Metabolite assays can help guide us regarding the need for allopurinol. 6-MMP: 6-methylmercaptopurine; 6-MP: 6-mercaptopurine; 6-TG: 6-thioguanine; TPMT: Thiopurine methy
- Citation: Malakar S, Shamsul Hoda U, Giri S, Samanta A, Roy A, Gupta R, Kumar SR, Agarwal M, Pawar A, Rungta S, Ghoshal UC. Difficult to treat and refractory autoimmune hepatitis: Recent advances in pharmacological management. World J Hepatol 2025; 17(9): 110264
- URL: https://www.wjgnet.com/1948-5182/full/v17/i9/110264.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i9.110264