Published online Oct 26, 2022. doi: 10.4252/wjsc.v14.i10.756
Peer-review started: May 5, 2022
First decision: June 11, 2022
Revised: June 24, 2022
Accepted: August 7, 2022
Article in press: August 7, 2022
Published online: October 26, 2022
Processing time: 173 Days and 1.4 Hours
The effects of inappropriate dietary calcium intake in early life on later obesity have not been fully elucidated.
To raise the mechanism of maternal calcium intake on the multi-differentiation potential of mesenchymal stem cells among their male offspring.
Four-week-old female C57BL/6N mice were fed by deficient, low, normal and excessive calcium reproductive diets throughout pregnancy and lactation. Bone MSCs (BMSCs) were obtained from 7-day-old male offspring to measure the adipogenic differentiation potential by the Wnt/β-catenin signaling pathway. The other weaning male pups were fed a high-fat diet for 16 wk, along with normal-fat diet as the control. Then the serum was collected for the measurement of biochemical indicators. Meanwhile, the adipose tissues were excised to analyze the adipocyte sizes and inflammatory infiltration. And the target gene expressions on the adipogenic differentiation and Wnt/β-catenin signaling pathway in the adipose tissues and BMSCs were determined by real-time reverse transcription polymerase chain reaction.
Compared with the control group, maternal deficient, low and excessive calcium intake during pregnancy and lactation aggravated dietary-induced obesity, with larger adipocytes, more serious inflammatory infiltration and higher serum metabolism indicators by interfering with higher expressions of adipogenic differentiation (PPARγ, C/EBPα, Fabp4, LPL, Adiponectin, Resistin and/or Leptin) among their male offspring (P < 0.05). And there were significantly different expression of similar specific genes in the BMSCs to successfully polarize adipogenic differentiation and suppress osteogenic differentiation in vivo and in vitro, respectively (P < 0.05). Meanwhile, it was accompanied by more significant disorders on the expressions of Wnt/β-catenin signaling pathway both in BMSCs and adulthood adipose tissues among the offspring from maternal inappropriate dietary calcium intake groups.
Early-life abnormal dietary calcium intake might program the adipogenic differentiation potential of BMSCs from male offspring, with significant expressions on the Wnt/β-catenin signaling pathway to aggravate high-fat-diet-induced obesity in adulthood.
Core tip: Maternal inappropriate dietary calcium intake could aggravate high-fat-diet-induced obesity among male offspring, with larger adipocytes and more serious inflammatory infiltration by interfering with the higher expressions of adipogenic genes, which was accompanied by significant expressions of specific genes on the adipogenic and osteogenic differentiation. It was worsened by the disorders of Wnt/β-catenin signaling pathway both in the BMSCs and adipose tissues. So the importance of this study was that the prevention of adulthood obesity could be moved forward to the appropriate calcium intake in the neonatal period, even the formation of maternal germ cells and fertilized egg.
- Citation: Li P, Wang Y, Li P, Liu YL, Liu WJ, Chen XY, Tang TT, Qi KM, Zhang Y. Maternal inappropriate calcium intake aggravates dietary-induced obesity in male offspring by affecting the differentiation potential of mesenchymal stem cells. World J Stem Cells 2022; 14(10): 756-776
- URL: https://www.wjgnet.com/1948-0210/full/v14/i10/756.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v14.i10.756
Obesity has become a worldwide noncommunicable health crisis with rising prevalence in the past few decades due to excess calorie intake, fat accumulation, and adiposity[1,2]. It can cause severe metabolic disorders such as nonalcoholic steatohepatitis, type 2 diabetes, cardiovascular diseases, and cancer[1-3]. These above pathological complications are characterized by more hypertrophy and hyperplasia of adipocytes to cause dynamic expansion in the adipose tissues, in which hyperplasia is a complicated process including disruption of the commitment of mesenchymal stem cells (MSCs) to form preadipocytes, and terminal differentiation from preadipocytes to mature adipocytes[4-6]. And MSCs (CD29+, CD90+, Sca-1+, CD31-, CD34-, CD45− and CD49d−), as a group of cells with multi-lineage differentiated potential and self-renewal capacity, are the major original sources of mature adipocytes. , in which the key coordinated cascade of transcription factors were mainly included PPARγ, C/EBPα, LPL and FABP4, with the significant secretory molecules such as Leptin, Adiponectin and Resistin[7,8]. In this process, the mechanisms governing the adipogenic differentiation of MSCs can be regulated by the coordination of complex networks in many signaling pathways, such as JAK2/STAT3, SIRT1/SIRT2, ERK1/ERK2, TGF-β/BMP, Wnt/β-catenin and RHO-family GTPase[9,10], in which the activation of Wnt/β-catenin signaling can inhibit adipogenic differentiation and promote osteogenic differentiation through endogenous regulatory genes (CTNNB1, Wnt1, Wnt10a, Wnt10b, Wnt5a, Gsk3β, Axin2 and TGF7L2)[11,12]. It has been demonstrated that the differentiation potential of MSCs mainly occurs in early life, and the numbers and differentiation potential significantly decline with the age[12], so the nutritional status and exposure to adverse factors at this stage, especially pregnancy and lactation, are important for the differentiation potential of MSCs to affect later metabolic disturbances in adulthood[13-16].
Calcium is an important functional nutrient on the regulation of energy balance and glucose uptake in the battle against obesity[17-19]. However, daily calcium intake is still lower than its recommended nutrient intake among pregnant women[20,21], so the imbalance of calcium intake in early life may have detrimental effects on later health. Both our high-fat-diet (HFD) induced obese mouse mode and epidemiological cohorts showed that both dietary insufficient and excessive calcium intake during pregnancy and lactation increased body weight gain by affecting the gut microbiota structure, and abnormal expression of lipolysis and liposynthesis among their male offspring [22-24]. However, the specific mechanisms by which maternal calcium intake modulates body weight and fat and glucose homeostasis of their infants are still not fully understood. Some research had found that Ca2+ formed in the culture medium had osteo-inductive properties to promote osteogenic differentiation of MSCs[25]. Previous studies also had demonstrated that neonatal calcium deficiency could reduce the osteogenic priming of MSCs by enlarging the subpopulation with adipogenic potential in piglets and mice in vivo[26]. Furthermore, it is competing and reciprocal on the balance of adipogenic and osteogenic differentiation of MSCs[27,28]. However, whether maternal inappropriate dietary calcium intake can increase the adipogenic differentiation potential of MSCs among their male offspring is still unclear.
Thus, this study was designed to investigate whether abnormal dietary calcium intake during gestation and lactation affected the multi-differentiation potential of bone MSCs (BMSCs) to aggravate the development of adulthood obesity among their male offspring and explore the possible signaling pathways. This deeper understanding of early-life calcium intake could play a significant role on preventing later obesity.
Sixty 4-week-old C57BL/6N female mice were obtained from Beijing Vital River Laboratory Animal Technology (License SCXK-Beijing) and housed at the Animal Center in the Academy of Military Medical Sciences under a 12-h light/dark cycle (lights-on 08:00 h) with adequate food and water intake at 22°C and 50% humidity. All mice were randomly divided into four groups (n = 15/group) and fed with the deficient (DC, 0.05%), low (LC, 0.25%), normal (NC, 0.70%) and high-calcium (HC, 1.20%) reproductive diets respectively for 6 wk. Five mice in each group (n = 5/group) were killed to determine the maternal contents of calcium and other metabolic indicators in the serum before mating. Then the remaining mice (n = 10/group) were mated with 10-week-old C57BL/6N male mice from Beijing Vital River Laboratory Animal Technology (2:1/cage), and continued on their own diets throughout gestation and lactation. According to the previous studies[21-23], the male offspring were used to study the development of obesity after the different calcium interventions during pregnancy and lactation. The 7-day-old male offspring (n = 9/group from more than three cages) in each group were killed to obtain BMSCs. While at age 21 d, the male offspring in the DC, LC, NC and HC groups (n = 10/group) were respectively weaned onto the HFD (34.9% fat by weight, 60% kcal, No. H10060) for 16 wk (NC-HFD, DC-HFD, LC-HFD and HC-HFD groups); with the normal fat diet (4.3% fat by weight, 10% kcal, No. H10010) as the control (NC-C group). All above diets were prepared by Beijing HFK Bioscience Co. Ltd. (http://www.hfkbio.com/) (Table 1). Body weight, food intake and energy intake in the NC-C, NC-HFD, DC-HFD, LC-HFD and HC-HFD groups were recorded weekly. Their blood samples were collected through the eye-drop, then they were anesthetized by the carbon dioxide inhalation. Immediately, their adipose tissues including the epididymal white adipose tissue (eWAT), inguinal white adipose tissue (iWAT), kidney adipose tissue (KAT) and brown adipose tissue (BAT) were freely dissected from the surrounding tissues, in which some were fixed in 10% phosphate-buffered formalin, some were stored in phosphate-buffered saline (PBS) to analyze the percentage of immune cells, and the remainder was frozen in liquid N2. The serum samples were separated at 3000 r/min for 15 min after they were kept for 30 min at room temperature. All biological samples were stored in a –80°C refrigerator until use.
| Ingredients (g) | Reproductive diets | Feeding diets (0.70%) | ||||
| Deficient calcium diet (0.05%) | Low calcium diet (0.25%) | Normal calcium diet (0.70%) | High calcium diet (1.20%) | Normal fat diet (H10010) | High fat diet (H10060) | |
| Casein | 200.00 | 200.00 | 200.00 | 200.00 | 189.58 | 258.45 |
| Cystine | 3.00 | 3.00 | 3.00 | 3.00 | 2.84 | 3.88 |
| Cornstarch | 396.30 | 391.30 | 380.00 | 367.50 | 298.59 | 161.53 |
| Maltodextrin | 132.00 | 132.00 | 132.00 | 132.00 | 33.18 | 88.91 |
| Sucrose | 100.00 | 100.00 | 100.00 | 100.00 | 331.77 | --- |
| Fibrin | 50.00 | 50.00 | 50.00 | 50.00 | 47.40 | 64.61 |
| Soybean oil | 70.00 | 70.00 | 70.00 | 70.00 | 23.70 | 32.31 |
| Lard oil | --- | --- | --- | --- | 18.96 | 316.60 |
| Mineral mixture without calcium (M1004) | 35.00 | 35.00 | 35.00 | 35.00 | --- | --- |
| Mineral mixture (M1002) | --- | --- | --- | --- | 9.48 | 12.92 |
| Calcium bicarbonate | --- | --- | --- | --- | 12.32 | 16.80 |
| Calcium carbonate | 1.25 | 6.25 | 17.50 | 30.00 | 5.21 | 7.11 |
| Potassium citrate. H2O | --- | --- | --- | --- | 15.64 | 21.32 |
| Vitamin mixture (V1002) | 10.00 | 10.00 | 10.00 | 10.00 | 9.48 | 12.92 |
| Choline Bitartrate | 2.50 | 2.50 | 2.50 | 2.50 | 1.90 | 2.58 |
| Antioxidant (TBHQ) | 0.014 | 0.014 | 0.014 | 0.014 | 0.047 | 0.065 |
All animal studies were approved and conducted in accordance with the Beijing Academy of Military Medical Sciences Guide for the Care and Usage Committee of Laboratory Animals. The animal protocol was approved by the Ethics of Animal Experiments in the Academy of Military Medical Sciences in China (No. IACUC-DWZX-2019-704).
The concentrations of serum calcium, glucose, triglyceride (TG) and total cholesterol (TC) were respectively measured by the coloristic methods using the enzymatic assay kits (Maccura Biotechnology Co. Ltd., Sichuan, China). The male offspring mice in each group were orally gavaged with 20% glucose (weight/volume: 2.0g/kg) after a 10-h overnight fast and blood samples were collected from the tail vein at 15, 30, 60, 90 and 120 min to determine the glucose content (oral glucose tolerance test, OGTT) at 13 wk. The insulin tolerance test (ITT) was performed 1 wk after the OGTT, in which the blood samples were collected from the tail vein for the determination of blood glucose after 2 h fasting.
Stromal vascular fraction cells (SVFs) were extracted from the eWAT and iWAT in PBS. The infiltration and percentages of M1 macrophages (CD45+CD64+CD11C+), M2 macrophages (CD45+CD64+CD11C–) and adipose tissue dendritic cells (ATDCs, CD45+CD64–CD11C+) were determined using the BD FACSCanto II Flow Cytometer (BD Biosciences, USA), and analyzed by FlowJo flow cytometry software (Treestar Inc., Ashland, OH, USA).
eWAT, iWAT, KAT and BAT in the NC-C, DC-HFD, LC-HFD, NC-HFD and HC-HFD groups were embedded in paraffin and cut into 6-μm sections, and stained with hematoxylin and eosin to measure the adipocyte size and inflammatory infiltration under a light microscope at 200× magnification, and analyzed by Image-pro Plus. All above histological experiments were performed by Servicebio (Beijing, China).
Total RNA in eWAT, iWAT, KAT and BAT was extracted using TRIzol Reagent (Invitrogen, Carlsbad, CA, USA), and cDNA was reverse transcribed by Transcript® One-Step gDNA Removal and cDNA Synthesis SuperMix (TransGen Biotech, China).
The genes related to adipogenic differentiation (PPARγ, C/EBPα, LPL, Fabp4, Adiponectin, Resistin and Leptin) and Wnt/β-catenin signaling pathway (CTNNB1, Wnt1, Wnt10a, Wnt10b, Wnt5a, Gsk3β, Axin2 and TGF7L2) were determined by real-time reverse transcription polymerase chain reaction (RT-PCR) (No. AQ101-03, TransStart® Green qPCR SuperMix, TransGen Biotech, China) (CFX-96; Bio-Rad, USA), and 36B4 was the invariant internal gene (Supplementary Table 1). Gene expression was normalized using the 2CT method.
BMSCs from 7-day-old male offspring in the NC, DC, LC and HC groups were isolated and cultured as follows. The tibia and fibula from three pups with different mothers were isolated after washing with PBS to remove the residual muscle and blood under sterile conditions. They were shredded into small pieces of 2 mm3 and digested in 0.1% type II collagenase (Gibco) at 37C for 40 min, and transferred into α-minimal essential medium (α-MEM) ( Gibco) containing 10% fetal bovine serum (FBS; Gibco), 100 U/mL penicillin, and 100 mg/mL streptomycin. The medium with FBS was changed every 3 d. When the adherent BMSCs reached 80%–90% confluence, they were collected in 0.25% trypsin (Gibco) and subcultured at a ratio of 1:3 for the further expansion and identification until the P3 generation, and used for subsequent experiments.
P3 generation BMSCs (1 × 106) from the DC, LC, NC and HC groups were phenotypically fixed, stained and characterized by the antibody permeabilization process. Mouse phycoerythrin-conjugated monoclonal antibodies Sca-1 (AB_2539218, MA5-17834), CD90 (AB_469640, 25-0900-82) and CD31 (AB_657735, 17-0311-82) (eBioscience, Waltham, MA, USA), and fluorescein-isothiocyanate-conjugated antibodies including CD29 (AB_2572449, 11-0291-82), CD34 (AB_465021, 11-0341-82) and CD45 (AB_465050, 11-0451-82) and CD49d (AB_465083, 11-0492-82) (eBioscience) were used to detect the purity of BMSCs. The Cell Cycle and Apoptosis Analysis kit (Beyotime) was obtained to measure the cell cycle of BMSCs. All above signals were recorded by flow cytometry with the FACScalibur system (Becton Dickinson) and analyzed using FlowJo software (Supplementary Figure 1 and Table 2).
| Indicators (%) | NC group (n = 9) | DC group (n = 9) | LC group (n = 9) | HC group (n = 9) | χ2 | P value |
| Cell cycle | ||||||
| G0G1 Phase | 91.27 ± 3.14 | 94.26 ± 2.09 | 95.08 ± 2.54 | 92.46 ± 5.01 | 1.774 | 0.939 |
| G2M Phase | 0.85 ± 0.0091 | 0.94 ± 0.011 | 1.05 ± 0.013 | 0.79 ± 0.0082 | ||
| S Phase | 7.89 ± 0.81 | 4.81 ± 0.56 | 3.87 ± 0.75 | 6.75 ± 0.94 | ||
| Flow cytometry | ||||||
| Sca-1 (+) | 95.03 ± 4.85 | 98.72 ± 6.12 | 99.31 ± 5.48 | 95.49 ± 3.84 | 4.788 | 0.188 |
| CD90 (+) | 98.12 ± 7.15 | 99.15 ± 2.04 | 99.07 ± 8.12 | 99.31 ± 6.74 | 0.608 | 0.895 |
| CD29 (+) | 99.13 ± 6.48 | 99.90 ± 3.46 | 97.02 ± 8.07 | 99.62 ± 7.01 | 0.549 | 0.908 |
| CD34 (-) | 99.08 ± 7.42 | 96.67 ± 2.93 | 97.94 ± 1.48 | 97.29 ± 1.92 | 0.364 | 0.546 |
| CD31 (-) | 99.46 ± 6.82 | 99.42 ± 4.12 | 98.94 ± 1.38 | 99.26 ± 1.57 | 0.159 | 0.690 |
| CD45 (-) | 99.79 ± 1.08 | 99.83 ± 2.54 | 98.48 ± 1.12 | 98.65 ± 1.75 | 0.287 | 0.963 |
| CD49d (-) | 99.13 ± 6.21 | 98.16 ± 2.32 | 99.06 ± 2.98 | 98.11 ± 1.09 | 5.087 | 0.166 |
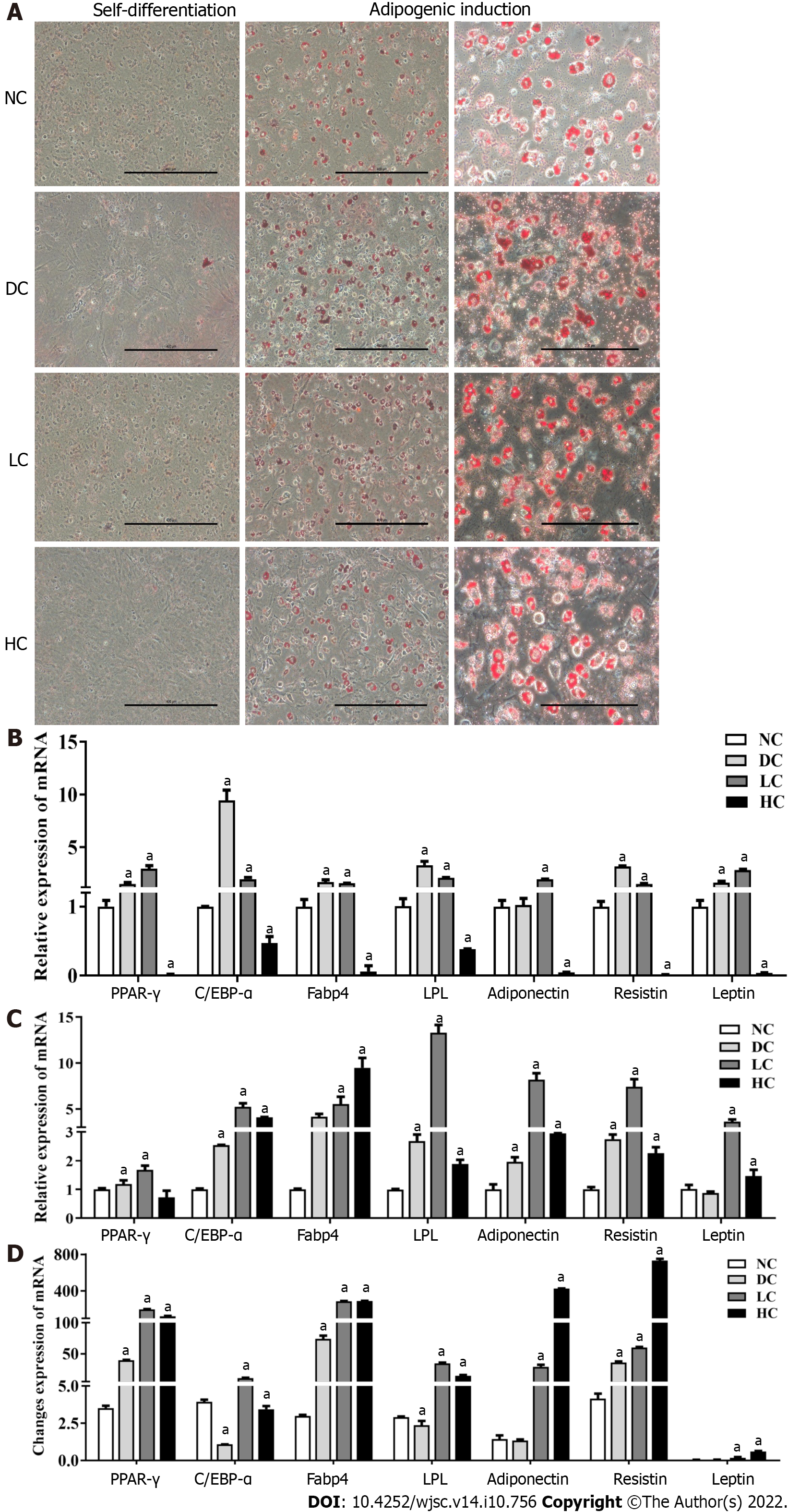
To identify the adipogenic differentiation potential of BMSCs in the NC, DC, LC and HC groups, P3 BMSCs (8 × 104) were cultured with α-MEM containing 10% FBS and the related adipogenic inducer (103 mM dexamethasone, 0.5 mM isobutyl methylxanthine, 0.2 mM indomethacin, and 10 μg/mL insulin) (Sigma, Germany) for 7 d, in which the medium was changed every 3 d. Self-differentiated BMSCs without the above inducers (3 × 104) were as the controls. The induced and self-differentiated BMSCs were stained with Oil Red O (Sigma, Germany) and measured the gene expression related to adipogenic differentiation[29].
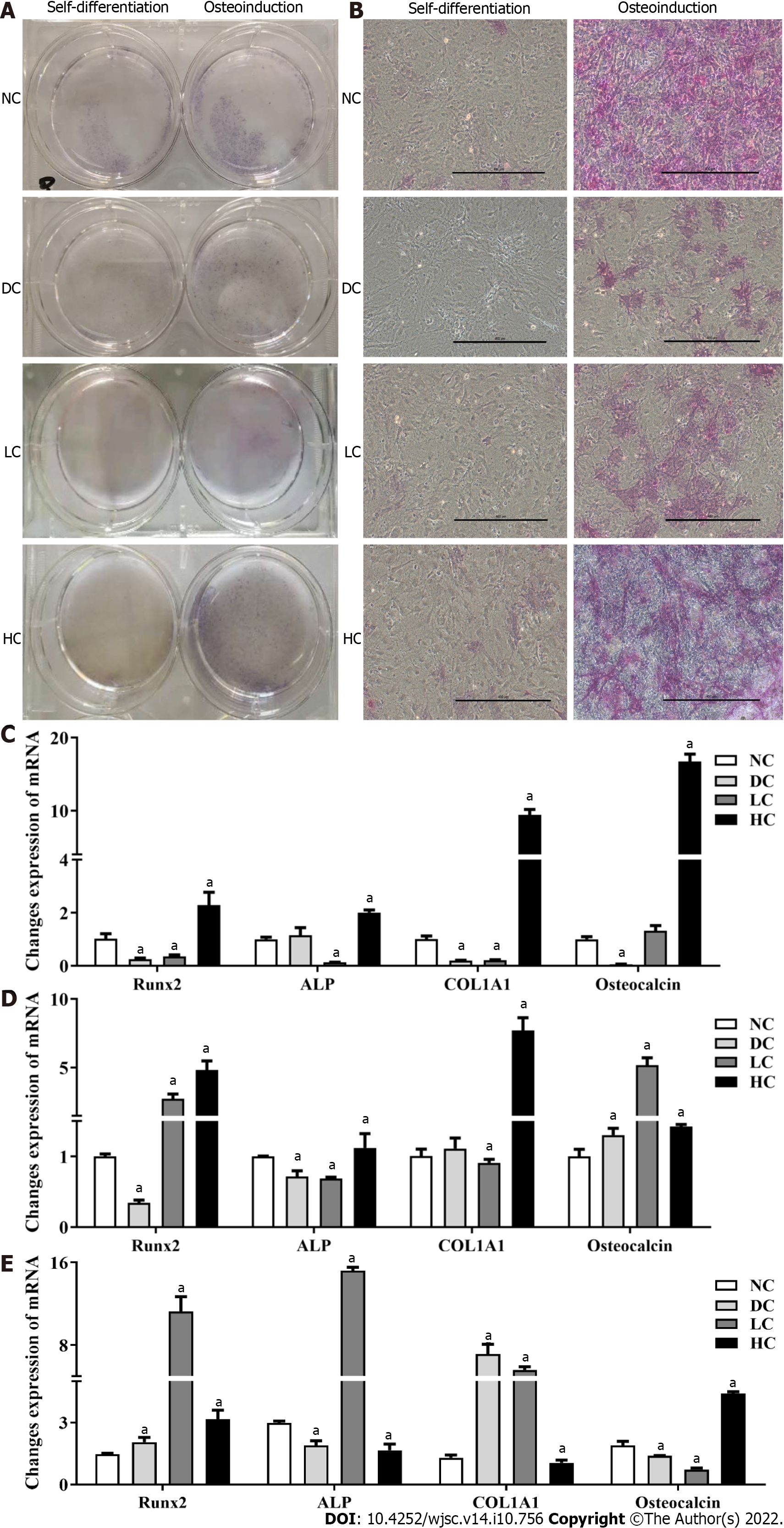
The osteogenic differentiation capacity of BMSCs was assessed by incubating the cells (3 × 104) with α-MEM containing 10% FBS and osteogenic inducer (107 mM dexamethasone, 0.5 mM ascorbic acid, and 10 mM β-glycerol phosphate) (Sigma, Germany) for 10 d, while the self-differentiated BMSCs without the above inducers (3 × 104) were as the controls. To demonstrate the osteogenic differentiation capacity of BMSCs, they were identified by immunocytochemical staining with alkaline phosphatase[29]. Expression of genes related to osteogenic differentiation were determined by RT-PCR.
Total RNA was extracted from the P3 BMSCs, adipogenic and osteogenic differentiated BMSCs and their related self-differentiated BMSCs using TRIzol Reagent (Invitrogen), and their cDNA samples were reverse transcribed by Transcript® One-Step gDNA Removal and cDNA Synthesis SuperMix (TransGen Biotech, China). The genes involved in adipogenic differentiation (PPARγ, C/EBPα, LPL, Fabp4, Adiponectin, Resistin and Leptin), osteogenic differentiation (Runx2, ALP, COL1A1, Osteocalcin and Osteopontin) and Wnt/β-catenin signaling pathway (Wnt1, Wnt10a, Wnt10b, Wnt5a, CTNNB1, Gsk3β, Axin2 and TGF7L2) (Supplementary Table 1) were determined by the RT-PCR (No. AQ101-03, TransStart® Green qPCR SuperMix, TransGen Biotech, China), and 36B4 was the invariant internal control. The assays were performed in triplicate and normalized to the internal standard mRNA levels using the 2CT method.
All statistical analyses were conducted using SPSS 21.0, with an α level of 0.05 and effect coefficient of 0.90. All values were expressed as mean ± standard deviation (or standard error), in which the Percent–Percent plot was chosen to determine data normality. The differences among all groups were tested and analyzed for the repeated measurement data based on whether the data were normally distributed (normal distribution: t test and ANOVA for continuous variables and χ2 test for categorical variables; non-normal distribution: Kruskal Wallis H test). P < 0.05 was considered to be statistically significant.
As shown in Supplementary Figure 2, there were no significant differences in body weight, daily dietary intake, related indexes of glucose (OGTT and ITT) and lipid (TC and TG), and bone Ca/P among the maternal DC, LC, NC and HC groups (P > 0.05), with lower bone calcium and phosphorus in the DC and LC groups than in the NC group and higher levels in the HC group (P < 0.05), which all proved that the animal model was successful.
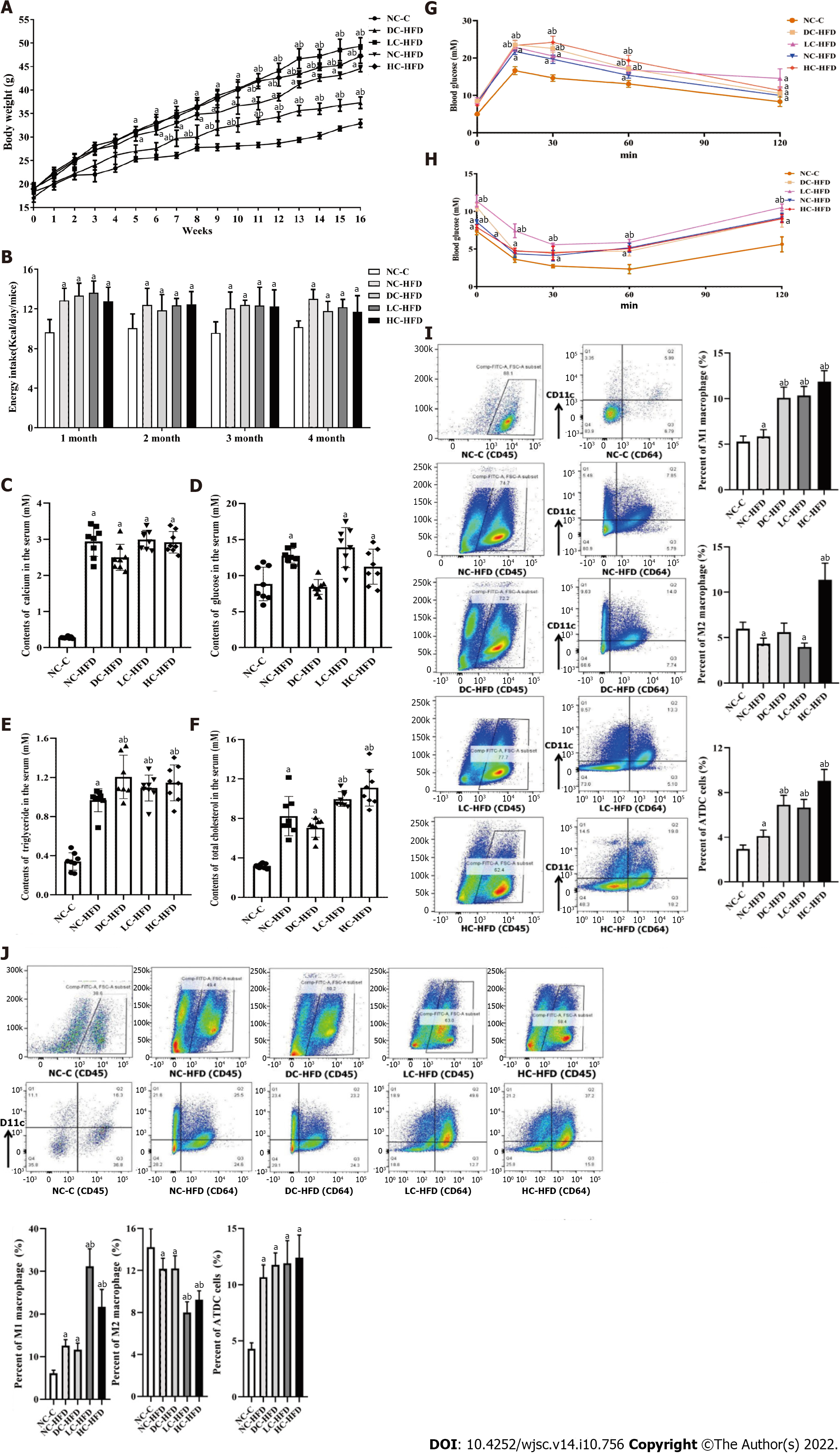
Among the male offspring, the body weight and mental state at weaning were not significantly different among the NC-C, DC-HFD, LC-HFD, NC-HFD and HC-HFD groups (P > 0.05, Figure 1A). During the HFD-induced adulthood, body weight (Figure 1A), energy intake (Figure 1B) and concentrations of serum metabolism-related indicators (TG, TC and glucose; Figure 1C-F) were all higher in the HFD groups (DC-HFD, LC-HFD, NC-HFD and HC-HFD) than in the NC-C group (P < 0.05). Likewise, the circulating glucose responses to the glucose load, as indicated by OGTT and ITT (Figure 1G and H), showed that there were higher glucose levels in the HFD groups after intraperitoneal glucose administration (P < 0.05). Compared with those in the NC-HFD group, maternal low (LC-HFD) and excess (HC-HFD) dietary calcium intake aggravated development of obesity, with significantly higher TC and TG (P < 0.05). In contrast, body weight in the DC-HFD group was lower. However, the content of TG was higher than in the NC-HFD group (P < 0.05).
The percentages of M1 macrophages, M2 macrophages and ATDC cells were demonstrated in eWAT (Figure 1I) and iWAT (Figure 1J). The percentages of M1 macrophages and ATDCs in eWAT were higher, and M2 macrophages were lower in the obese (DC-HFD, LC-HFD, NC-HFD and/or HC-HFD) groups than in the NC-C group (P < 0.05). Further comparison among all the HFD groups showed that the percentages of M1 macrophages and ATDCs were increased in the DC-HFD, LC-HFD and HC-HFD groups when compared with the NC-HFD group (P < 0.05). In iWAT, the percentages of M1 macrophages and ATDCs were significant higher, and M2 macrophages were lower in the HFD groups than in the NC-C group (P < 0.05). Compared with the NC-HFD group, maternal low (LC-HFD) and high (HC-HFD) dietary calcium intake aggravated disorder of M1 and M2 macrophages (P < 0.05), which was not found in the DC-HFD group (P > 0.05).
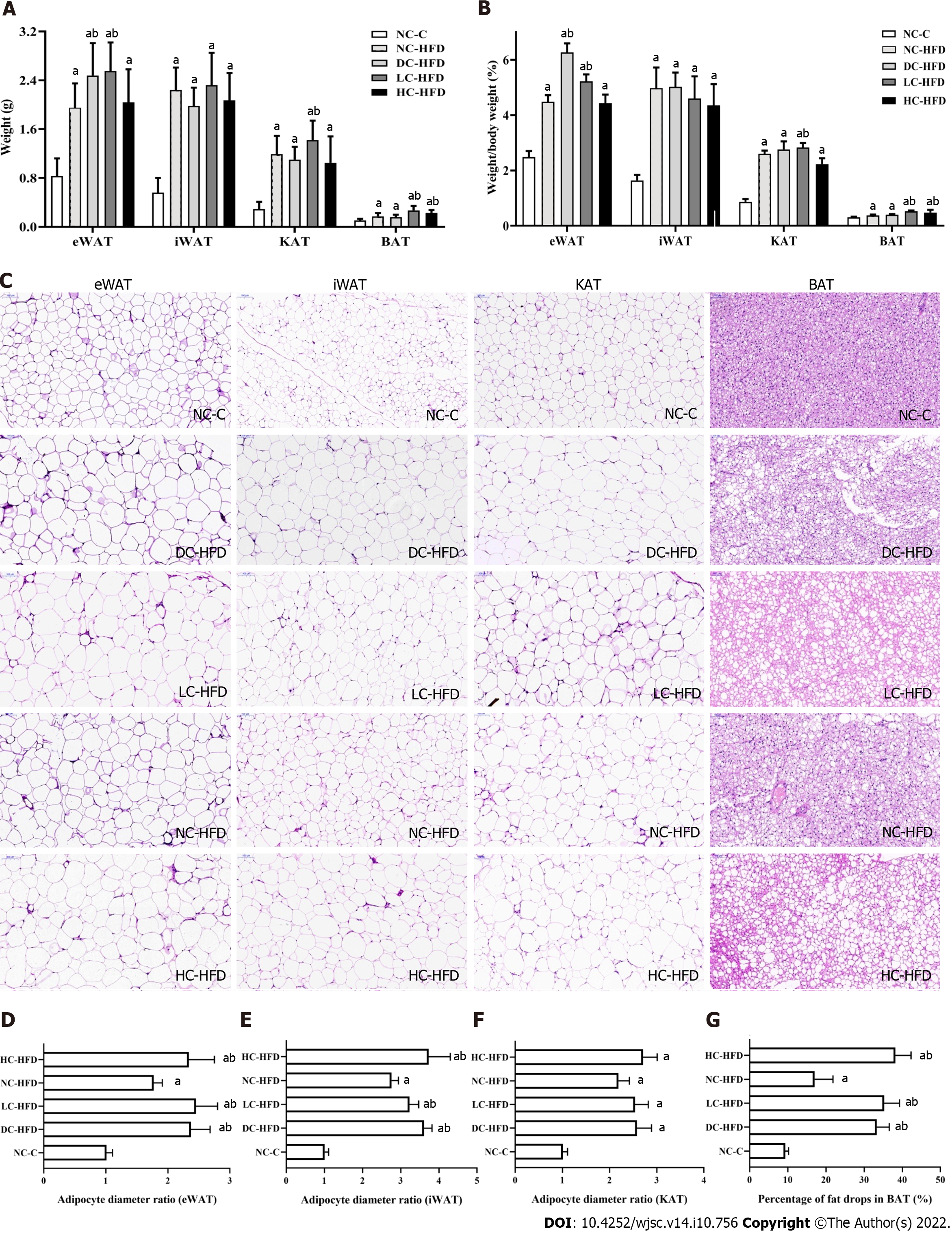
The weights of eWAT, iWAT, KAT and BAT (Figure 2A) and adipose tissue weight/body weight (Figure 2B) were all higher in the four HFD groups than in the NC-C group (P < 0.05). Compared the NC-HFD group, maternal deficient (DC-HFD, eWAT and eWAT/body weight), low (LC-HFD, eWAT, KAT, BAT, eWAT/body weight, KAT/body weight and BAT/body weight) and excess (HC-HFD, BAT and BAT/body weight) dietary calcium intake groups showed increased weights of eWAT, iWAT, KAT and/or BAT, and related adipose tissue weight/body weight (P < 0.05). Compared with the NC-C group, the differentiation of adipocytes (number and diameter) in eWAT (Figure 2C and D), iWAT (Figure 2C and E), KAT (Figure 2C and F) and BAT (Figure 2C and G), was more prominent in the DC-HFD, LC-HFD, NC-HFD and HC-HFD groups (P < 0.05). Compared with the NC-HFD group, maternal abnormal dietary calcium intake (DC-HFD, LC-HFD and HC-HFD groups) aggravated disorder of proliferation and differentiation of adipocytes in eWAT, iWAT and BAT among male offspring, with larger adipocytes (P < 0.05).
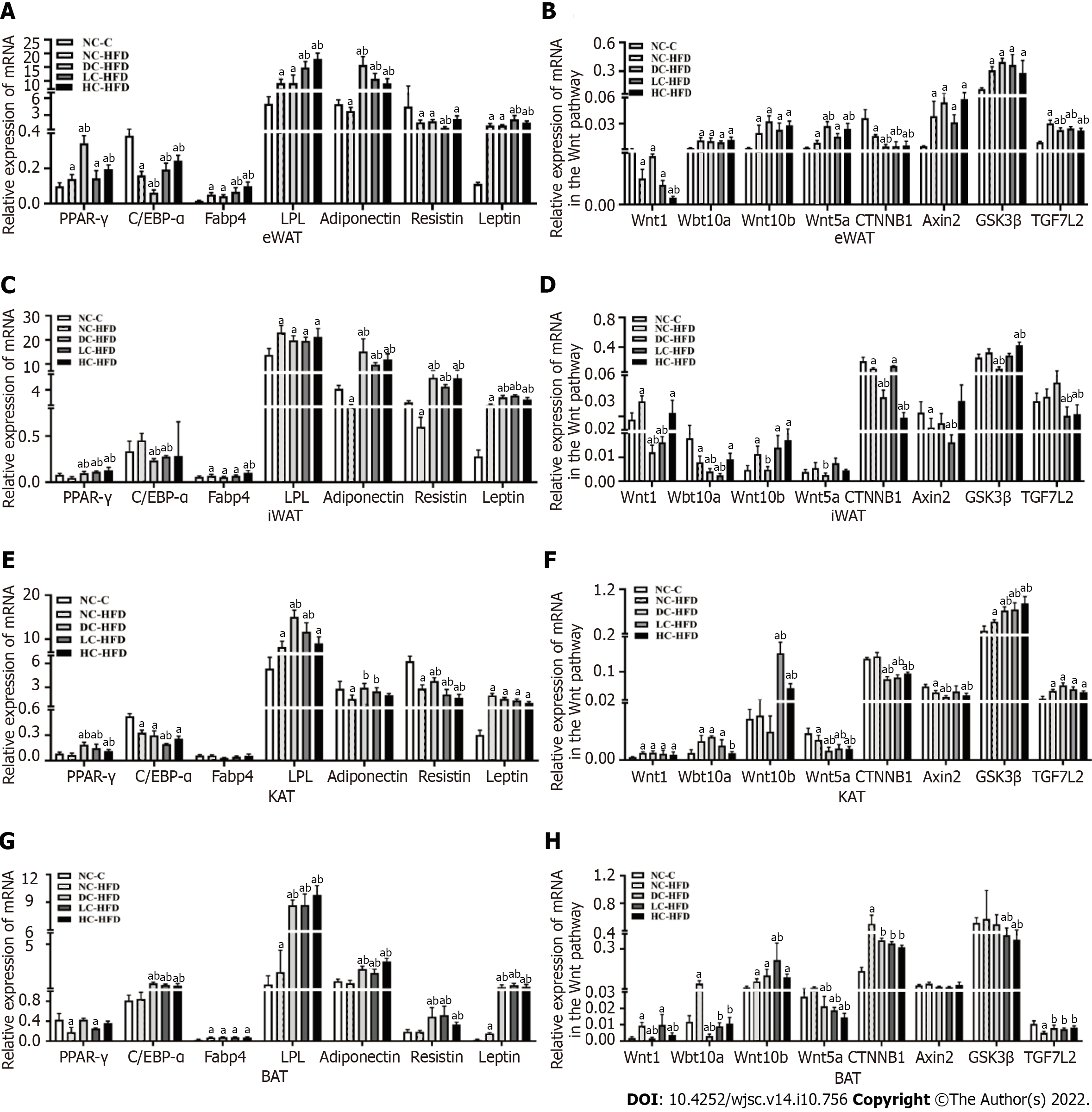
As shown in Figure 3, compared with the NC-HFD group, gene expression related to adipogenic differentiation (PPARγ, C/EBPα, LPL, Fabp4, Adiponectin, Resistin and Leptin) and Wnt/β-catenin signaling pathway (Wnt1, Wnt10a, Wnt10b, Wnt5a, CTNNB1, Gsk3β, Axin2 and TGF7L2) in eWAT, iWAT, KAT and BAT among the DC-HFD, LC-HFD and HC-HFD groups was more disordered.
Exactly, in eWAT (Figure 3A and B), compared with the NC-HFD group, there were higher expressions of PPARγ, Adiponectin and Wnt5a, and lower expressions of C/EBPα, CTNNB1 and TCF7L2 in the DC-HFD group (P < 0.05), and higher expressions of C/EBPα, Fabp4, LPL, Adiponectin and Leptin, and lower expressions of Resist, CTNNB1 and TCF7L2 in the LC-HFD group (P < 0.05). Higher expressions of PPARγ, C/EBPα, LPL, Fabp4, Adiponectin, Leptin and Wnt5a, and lower expressions of Wnt1, CTNNB1 and TCF7L2 were demonstrated in the HC-HFD group (P < 0.05). In iWAT (Figure 3C and D), expressions of PPARγ, Adiponectin, Resistin and Leptin were higher in the DC-HFD, LC-HFD, and HC-HFD groups (with higher Fabp4 in the HC-HFD) than in the NC-HFD group (P < 0.05), with significantly lower expressions of C/EBPα, Wnt1,Wnt10a, Wnt10b, Wnt5a, CTNNB1 and Gsk3β in the DC-HFD group (P < 0.05), lower expressions of C/EBPα, Wnt1,Wnt10a, Axin2 and TCF7L2 in the LC-HFD group (P < 0.05), and lower expressions of CTNNB1 and TCF7L2 in the HC-HFD group (P < 0.05). As shown in KAT among the four HFD groups (Figure 3E and F), expressions of PPARγ, LPL, Wnt10b and Gsk3β were higher, with the significantly low levels of Wnt5a, CTNNB1 and Axin2 in the DC-HFD (accompanied with higher expressions of Adiponectin and Resistin), LC-HFD (higher expressions of Adiponectin, with lower expressions of C/EBPα and Resistin), and HC-HFD (lower expressions of Wnt10a and Resistin) groups than in the NC-HFD group (P < 0.05). In BAT (Figure 3G and H), expressions of C/EBPα, LPL, Adiponectin, Resistin, Leptin and TGF7L2 were higher, with the significantly lower expressions of Wnt10a, Wnt5a and CTNNB1 in the DC-HFD (lower expressions of Wnt1), LC-HFD (higher Wnt10b and lower Gsk3β expressions), and HC-HFD groups (lower expressions of Wnt1 and Gsk3β) than in the NC-HFD group (P < 0.05).
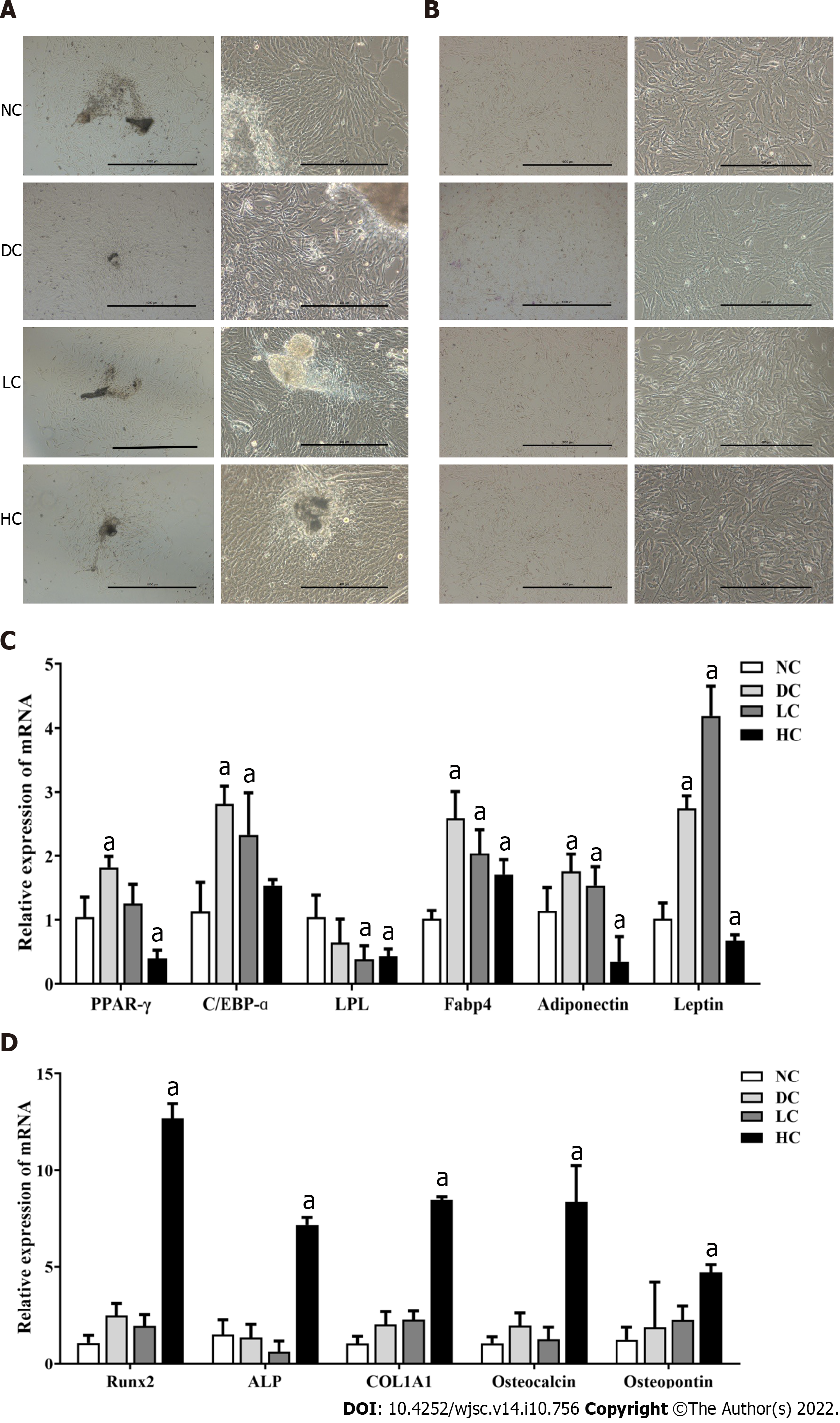
The morphology of BMSCs at P0 (Figure 4A) and P3 generations (Figure 4B) was similar in the DC, LC, NC and HC groups, with no significant differences in the pluripotent stem cells (G0/G1 phase) and purity of BMSCs (Sca-1+, CD90+, CD29+, CD34, CD31, CD45 and CD49d) in the P3 generation (P > 0.05, Table 2 and Supplementary Figure 1).
In the P3 generation of BMSCs, compared with the NC group, maternal deficient (DC group) and low (LC group) dietary calcium intake promoted adipogenic differentiation potential of BMSCs, with higher levels of PPARγ, C/EBPα, Fabp4, Adiponectin and Leptin (Figure 4C, P < 0.05). Maternal excess dietary calcium intake (HC group) induced osteogenic differentiation and inhibited adipogenic differentiation of BMSCs, with higher levels of Runx2, ALP, COL1A1, Osteocalcin and Osteopontin, and lower levels of PPARγ, LPL, Adiponectin and Leptin (Figure 4C and D, P < 0.05).
Under the adipogenic induction (Figure 5), compared with the NC group, maternal abnormal dietary calcium intake (DC, LC and HC groups) promoted adipogenic differentiation of BMSCs, with more lipid drops (Figure 5A) and higher expressions of PPARγ, C/EBPα, Fabp4, LPL, Adiponectin, Resistin and Leptin (Figure 5C and D). As with expressions of genes related to adipogenic differentiation in the P3 generation (Figure 4C), compared with that in the NC group, expressions of PPARγ, C/EBPα, Fabp4, LPL, Adiponectin, Resistin and Leptin in the DC and LC groups were higher under the self-differentiation status (Figure 5B), with lower expressions in the HC group. Under osteogenic induction (Figure 6), compared with the NC group, maternal excess dietary calcium intake (HC group) promoted osteogenic differentiation of BMSCs, with more calcium nodules (Figure 6A) and higher expressions of Runx2, ALP, COL1A1 and Osteocalcin (Figure 6C and D), which was similar to that under the self-differentiation status (Figure 6B). Furthermore, compared with the NC group, the osteogenic differentiation potential of BMSCs was weaker in the DC and LC groups under osteogenic induction and self-differentiation status (Figure 6A, C and D), with lower expressions of Runx2, ALP, COL1A1 and Osteocalcin.
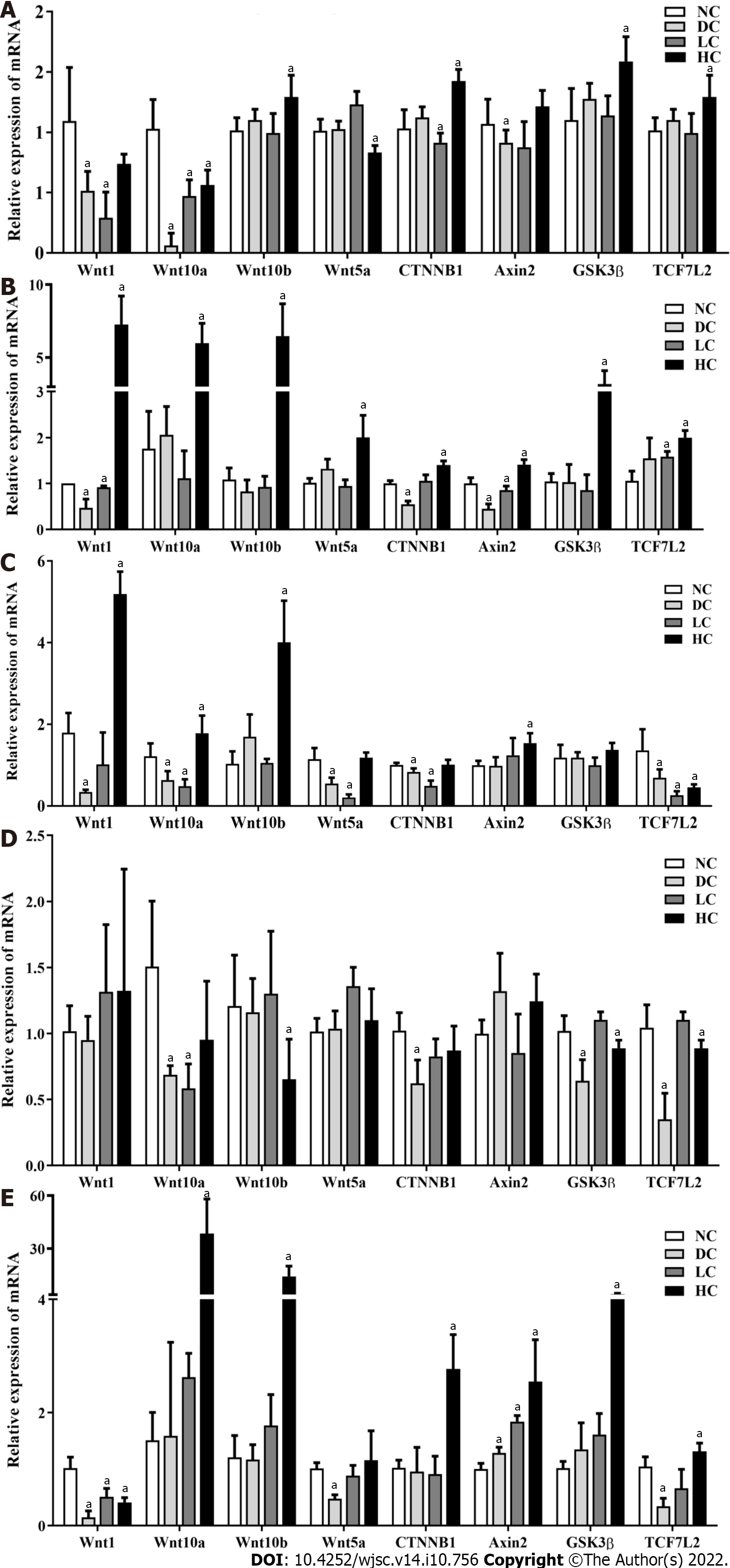
In the P3 generation of BMSCs without induction, compared with the NC group, maternal deficient (DC group) and low (LC group) dietary calcium intake inhibited expressions of Wnt1, Wnt10a, CTNNB1 and Axin2 (P < 0.05) (Figure 7), while there were significantly higher expressions of Wnt10b, CTNNB1, Gsk3β and TGF7L2, with lower expressions of Wnt10a and Wnt5a in the HC group (P < 0.05) (Figure 7A).
Under adipogenic induction, compared with the NC group, maternal abnormal dietary calcium intake (DC, LC and HC groups) decreased expressions of Wnt10a, Wnt10b, CTNNB1, Gsk3β and TGF7L2 to promote the adipogenic differentiation potential of BMSCs (Figure 7D, P < 0.05), while under the self-differentiation status, maternal deficient (DC group) and low (LC group) dietary calcium intake inhibited expressions of Wnt1, CTNNB1 and Axin2 (P < 0.05), while there were significantly higher levels of Wnt1, Wnt10a, Wnt10b, Wnt5a, CTNNB1, Axin2, Gsk3β and TGF7L2 in the HC group compared with the NC group (Figure 7B, P < 0.05), which was consist with the P3 BMSCs.
Under osteogenic induction, compared with the NC group, expressions of Wnt1, Wnt5a and TGF7L2 were lower in the DC group (P < 0.05), Wnt1 expressions was lower in the LC group (P < 0.05), and there were significantly higher levels of Wnt10a, Wnt10b, CTNNB1, Axin2, Gsk3β and TGF7L2 in the HC group (Figure 7E, P < 0.05). Under the self-differentiation status, maternal DC and LC intake inhibited expressions of Wnt1, Wnt10a, Wnt5a, CTNNB1 and TGF7L2 (P < 0.05), while there were significantly higher expressions of Wnt1, Wnt10a, Wnt10b and Axin2 in the HC group than in the NC group (Figure 7C, P < 0.05).
The correlation between the inappropriate consumption of nutrient and occurrence of obesity presents a greatest global public health problem, which needs more novel therapies[30]. A lot of researches have demonstrated that chronically deficient and excessive calcium exposure is as an important contributing factor to the development of obesity by controlling the de novo lipogenesis and lipolytic signals through regulating related gene expressions[31-33]. There is also compelling evidence that maternal calcium dysfunction directly affects fat synthesis and metabolism of their offspring[34-37]. In agreement with our findings using a mouse model that maternal inappropriate dietary calcium intake during pregnancy and lactation aggravated development of obesity by elevating cytosolic calcium, with more and larger adipocytes, and disorders of immune cells (M1 macrophages, M2 macrophages and ATDC cells) in the adipose tissues.
It is agreed that the development of obesity is driven by hypertrophy and hyperplasia of the adipocytes in the process of adipogenic differentiation to cause the expansion of fat depots[38]. Lineage-tracing models have shown that the numbers of adipocytes are primarily determined in early life and mostly stable through to adulthood for the remarkable hypertrophic potential of differentiated adipocytes with HFD induction[39-42]. The modulation of cytosolic calcium can regulate the early stage of adipocyte differentiation and thermogenic capacity of BAT in mice[43]. The propensity of adipogenesis to generate new adipocytes in different adipose tissues (eWAT, iWAT, KAT and BAT) highlights the unique characteristics of fat depots. Thus, we should discuss the roles of abnormal dietary calcium intake during pregnancy and lactation on the adipogenic differentiation potential in different adipose tissues among male offspring. This was consistent with our findings that the imbalance of dietary calcium intake in early life could affect the proliferation and differentiation of eWAT, iWAT and BAT, with higher weight of adipose tissue. However, the mechanism remains to be elucidated.
Lineage-tracing studies in animal models have suggested that there are two-step phases in the adipogenic differentiation, including specific preadipocyte formation (MSCs to preadipocytes) and terminal adipocyte maturation (preadipocytes to mature adipocytes), in which the committed preadipocytes from the pluripotent MSCs are activated by a number of critical transcription factors (PPARγ, C/EBPα, C/EBPβ and FABP4) and related extracellular signals. At the differentiation of mature adipocytes (second stage), they express all the biomarkers of early adipocyte differentiation as well as the peptide hormones, such as Adiponectin, Resistin, Leptin, ATGL, LPL and Perilipin 1[44,45]. All the above transcription factors are involved in the specific Wnt signaling pathway to affect adipogenic differentiation[46-48]. In our study, abnormal dietary calcium intake during pregnancy and lactation (DC-HFD, LC-HFD and HC-HFD) aggravated expressions of genes related to proliferation and differentiation of adipocytes and Wnt/β-catenin signaling pathway in eWAT, iWAT, KAT or BAT in the adulthood of their male offspring, which could more clearly explain the possible causes for the development of obesity. In the early stage, MSCs, as multipotential progenitor cells, are delicately balanced for their terminal adipo-osteogenic differentiation commitment[49-51]. It has also been reported that this decision process of MSCs is competing and reciprocal, and is precisely achieved by a variety of critical and external cues, including phytocannabinoids, conjugated linoleic acid, calcium, and chemical, physical and biological factors[52-58]. Many investigations in vitro had demonstrated that deficient calcium exposure inhibited osteogenesis[59-61]. Conversely, little was known about the effects of inappropriate dietary calcium intake during pregnancy and lactation on adipogenic differentiation, to aggravate the development of obesity in adulthood under HFD induction[55,62]. The major novel finding of our study was that maternal deficient and low dietary calcium intake aggravated the potential adipogenic differentiation and suppressed osteogenic differentiation of BMSCs. Maternal excess dietary calcium intake could play an opposing differentiation role without the exogenous stimuli. In response to reagent induction, both maternal deficient, low and excessive dietary calcium intake could polarize adipogenic differentiation and suppress osteogenic differentiation. All the above results were consistent with the results in the adult offspring with HFD induction.
Terminal differentiation of BMSCs is achieved through a coordinated and highly orchestrated program of triggering different signaling pathways, and activated by various transcription factors that guide the programming alterations of BMSCs to commit the lineage to cause the pathophysiological processes of obesity[63-66]. Thus, it is necessary that our research for screening out the roles of different calcium exposure in early life on the expressions of related transcription factors and signaling pathways could regulate both osteogenic and adipogenic differentiation of BMSCs. This proves that the imbalance of terminal adipo-osteogenic differentiation by abnormal calcium exposure in early life results from the above disorders of gene expressions and Wnt/β-catenin signaling pathway on the differentiation of BMSCs among male offspring.
There were some limitations to this study. Firstly, we required more complex and explicit procedures, including western blotting, to explore the related mechanisms more clearly. Secondly, our conclusions need to be verified in other MSCs and animal models to ensure their feasibility and effectiveness. Finally, the inconsistent results of maternal deficient calcium intake still need to be further discussed.
Our results suggest that abnormal dietary calcium intake during gestation and lactation aggravates the development of obesity by programming the adipogenic differentiation potential of BMSCs among male offspring, which is related to the significantly different expressions of target genes for adipogenic differentiation on the Wnt/β-catenin signaling pathway to aggravate dietary-induced obesity in the adulthood. Maternal deficient calcium exposure can inhibit the osteogenic differentiation to cause low body weight. So the importance of this study is that the prevention of adulthood obesity could be moved forward to the appropriate calcium intake in the neonatal period, even the formation of maternal germ cells and fertilized egg.
Obesity is characterized by the hypertrophy and hyperplasia of adipocytes, in which the commitment from bone mesenchymal stem cells (BMSCs) to preadipocytes is the important process for their hyperplasia. Our previous study showed that dietary insufficient and excessive calcium intake during pregnancy and lactation increased the body weight of offspring, using a high-fat-diet-induced obese mouse model and epidemiological cohorts. However, whether maternal inappropriate dietary calcium intake could affect the adipogenic differentiation potential of MSCs is still unclear.
This study was designed to investigate the effects of abnormal dietary calcium intake during gestation and lactation on the muti-differentiation potential of BMSCs among male offspring, and explore the possible role of the Wnt/β-catenin signaling pathway, which might aggravate the development of obesity, with more excessive lipid accumulation in adulthood.
We presented the possibility that abnormal dietary calcium intake during pregnancy and lactation could derive hyperplasic adipogenesis from BMSCs by regulating target gene expressions profiles through the fetus to adulthood among their male offspring.
Four-week-old female C57BL/6N mice were fed by deficient, low, normal and excessive calcium reproductive diets throughout pregnancy and lactation. The BMSCs were obtained from 7-day-old male offspring to measure their adipogenic differentiation potential through the Wnt/β-catenin signaling pathway. The other weaning male pups were fed a high-fat diet for 16 wk along with a normal-fat diet as the control. Serum was collected for biochemical analysis. Adipose tissues were excised for histological examination, immunohistochemistry, determining the proportions of immune cells by flow cytometry, and gene expressions related to adipogenic differentiation and Wnt/β-catenin signaling pathway by real-time reverse transcription polymerase chain reaction.
Maternal deficient, low and excess dietary calcium intake aggravated dietary-induced obesity with more/larger adipocytes and higher serum metabolism indicators, along with disordered expressions of genes related to adipogenic differentiation (PPARγ, C/EBPα, Fabp4, LPL, Adiponectin, Resistin and Leptin) in the adipose tissues among the male offspring. We also showed significantly different expressions of similarly specific genes in BMSCs to successfully polarize adipogenic differentiation and suppress osteogenic differentiation in vivo and in vitro, respectively. The related mechanistic insights were gained to worsen this adipogenic differentiation through the Wnt/β-catenin signaling pathway in the BMSCs and adult adipose tissues.
Abnormal dietary calcium intake during pregnancy and lactation might program the adipogenic differentiation potential of BMSCs among male offspring, which was related to the significantly different expressions of target genes in the Wnt/β-catenin signaling pathway to preserve more adipocytes to aggravate dietary-induced obesity in adulthood.
The importance of this study is that the prevention of adulthood obesity could be moved forward to the appropriate calcium intake in the neonatal period, even the formation of maternal germ cells and fertilized egg.
We would like to thank Yuan-Lin Liu and Yi Zhang for their helps on the experiments of BMSCs and Servicebio Co. Ltd. for their morphological analysis service.
| 1. | Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1143] [Cited by in RCA: 1852] [Article Influence: 264.6] [Reference Citation Analysis (0)] |
| 2. | Lavie CJ, Pandey A, Lau DH, Alpert MA, Sanders P. Obesity and Atrial Fibrillation Prevalence, Pathogenesis, and Prognosis: Effects of Weight Loss and Exercise. J Am Coll Cardiol. 2017;70:2022-2035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 367] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 3. | Rivera JÁ, de Cossío TG, Pedraza LS, Aburto TC, Sánchez TG, Martorell R. Childhood and adolescent overweight and obesity in Latin America: a systematic review. Lancet Diabetes Endocrinol. 2014;2:321-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 287] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 4. | Tencerova M, Figeac F, Ditzel N, Taipaleenmäki H, Nielsen TK, Kassem M. High-Fat Diet-Induced Obesity Promotes Expansion of Bone Marrow Adipose Tissue and Impairs Skeletal Stem Cell Functions in Mice. J Bone Miner Res. 2018;33:1154-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 190] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 5. | Li SN, Wu JF. TGF-β/SMAD signaling regulation of mesenchymal stem cells in adipocyte commitment. Stem Cell Res Ther. 2020;11:41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 130] [Article Influence: 21.7] [Reference Citation Analysis (1)] |
| 6. | Ambrosi TH, Scialdone A, Graja A, Gohlke S, Jank AM, Bocian C, Woelk L, Fan H, Logan DW, Schürmann A, Saraiva LR, Schulz TJ. Adipocyte Accumulation in the Bone Marrow during Obesity and Aging Impairs Stem Cell-Based Hematopoietic and Bone Regeneration. Cell Stem Cell. 2017;20:771-784.e6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 393] [Cited by in RCA: 628] [Article Influence: 69.8] [Reference Citation Analysis (0)] |
| 7. | Lin YH, Kang L, Feng WH, Cheng TL, Tsai WC, Huang HT, Lee HC, Chen CH. Effects of Lipids and Lipoproteins on Mesenchymal Stem Cells Used in Cardiac Tissue Regeneration. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Louwen F, Ritter A, Kreis NN, Yuan J. Insight into the development of obesity: functional alterations of adipose-derived mesenchymal stem cells. Obes Rev. 2018;19:888-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 9. | Cristancho AG, Lazar MA. Forming functional fat: a growing understanding of adipocyte differentiation. Nat Rev Mol Cell Biol. 2011;12:722-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 904] [Cited by in RCA: 1102] [Article Influence: 73.5] [Reference Citation Analysis (0)] |
| 10. | Porro S, Genchi VA, Cignarelli A, Natalicchio A, Laviola L, Giorgino F, Perrini S. Dysmetabolic adipose tissue in obesity: morphological and functional characteristics of adipose stem cells and mature adipocytes in healthy and unhealthy obese subjects. J Endocrinol Invest. 2021;44:921-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 11. | Rosen ED, MacDougald OA. Adipocyte differentiation from the inside out. Nat Rev Mol Cell Biol. 2006;7:885-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1830] [Cited by in RCA: 2030] [Article Influence: 106.8] [Reference Citation Analysis (0)] |
| 12. | Matsushita K, Dzau VJ. Mesenchymal stem cells in obesity: insights for translational applications. Lab Invest. 2017;97:1158-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 13. | Zhang P, Zhang H, Lin J, Xiao T, Xu R, Fu Y, Zhang Y, Du Y, Cheng J, Jiang H. Insulin impedes osteogenesis of BMSCs by inhibiting autophagy and promoting premature senescence via the TGF-β1 pathway. Aging (Albany NY). 2020;12:2084-2100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 14. | Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, Li N, Hu G, Corrado F, Rode L, Kim YJ, Haugen M, Song WO, Kim MH, Bogaerts A, Devlieger R, Chung JH, Teede HJ. Association of Gestational Weight Gain With Maternal and Infant Outcomes: A Systematic Review and Meta-analysis. JAMA. 2017;317:2207-2225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 830] [Cited by in RCA: 1223] [Article Influence: 135.9] [Reference Citation Analysis (0)] |
| 15. | Gingras V, Hivert MF, Oken E. Early-Life Exposures and Risk of Diabetes Mellitus and Obesity. Curr Diab Rep. 2018;18:89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Hoffman DJ, Reynolds RM, Hardy DB. Developmental origins of health and disease: current knowledge and potential mechanisms. Nutr Rev. 2017;75:951-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 259] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 17. | Soares MJ, Pathak K, Calton EK. Calcium and vitamin D in the regulation of energy balance: where do we stand? Int J Mol Sci. 2014;15:4938-4945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Li P, Fan C, Lu Y, Qi K. Effects of calcium supplementation on body weight: a meta-analysis. Am J Clin Nutr. 2016;104:1263-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Zemel MB, Miller SL. Dietary calcium and dairy modulation of adiposity and obesity risk. Nutr Rev. 2004;62:125-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 104] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | Gernand AD, Schulze KJ, Stewart CP, West KP Jr, Christian P. Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nat Rev Endocrinol. 2016;12:274-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 366] [Cited by in RCA: 433] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 21. | Bolland MJ, Leung W, Tai V, Bastin S, Gamble GD, Grey A, Reid IR. Calcium intake and risk of fracture: systematic review. BMJ. 2015;351:h4580. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 211] [Cited by in RCA: 201] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 22. | Li P, Tang T, Chang X, Fan X, Chen X, Wang R, Fan C, Qi K. Abnormality in Maternal Dietary Calcium Intake During Pregnancy and Lactation Promotes Body Weight Gain by Affecting the Gut Microbiota in Mouse Offspring. Mol Nutr Food Res. 2019;63:e1800399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Li P, Yan K, Chang X, Chen X, Wang R, Fan X, Tang T, Zhan D, Qi K. Sex-specific maternal calcium requirements for the prevention of nonalcoholic fatty liver disease by altering the intestinal microbiota and lipid metabolism in the high-fat-diet-fed offspring mice. Gut Microbes. 2020;11:1590-1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Chang XL, Shang Y, Liu YJ, Li P, Wang YY, Liang AM, Qi KM. Effects of calcium supplementation during the pregnancy and early infancy stage on the body mass index and gut microbiota in the infants. Chinese journal of preventive medicine. 2018;52:642-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 25. | Chen XR, Bai J, Yuan SJ, Yu CX, Huang J, Zhang TL, Wang K. Calcium phosphate nanoparticles are associated with inorganic phosphate-induced osteogenic differentiation of rat bone marrow stromal cells. Chem Biol Interact. 2015;238:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Lei Q, Chen J, Huang W, Wu D, Lin H, Lai Y. Proteomic analysis of the effect of extracellular calcium ions on human mesenchymal stem cells: Implications for bone tissue engineering. Chem Biol Interact. 2015;233:139-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Jothimani G, Di Liddo R, Pathak S, Piccione M, Sriramulu S, Banerjee A. Wnt signaling regulates the proliferation potential and lineage commitment of human umbilical cord derived mesenchymal stem cells. Mol Biol Rep. 2020;47:1293-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 28. | Park JS, Kim M, Song NJ, Kim JH, Seo D, Lee JH, Jung SM, Lee JY, Lee J, Lee YS, Park KW, Park SH. A Reciprocal Role of the Smad4-Taz Axis in Osteogenesis and Adipogenesis of Mesenchymal Stem Cells. Stem Cells. 2019;37:368-381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 29. | Liu W, Zhou N, Liu Y, Zhang W, Li X, Wang Y, Zheng R, Zhang Y. Mesenchymal stem cell exosome-derived miR-223 alleviates acute graft-versus-host disease via reducing the migration of donor T cells. Stem Cell Res Ther. 2021;12:153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 30. | Gao P, Jiang Y, Wu H, Sun F, Li Y, He H, Wang B, Lu Z, Hu Y, Wei X, Cui Y, He C, Wang L, Zheng H, Yang G, Liu D, Yan Z, Zhu Z. Inhibition of Mitochondrial Calcium Overload by SIRT3 Prevents Obesity- or Age-Related Whitening of Brown Adipose Tissue. Diabetes. 2020;69:165-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 31. | Fu S, Yang L, Li P, Hofmann O, Dicker L, Hide W, Lin X, Watkins SM, Ivanov AR, Hotamisligil GS. Aberrant lipid metabolism disrupts calcium homeostasis causing liver endoplasmic reticulum stress in obesity. Nature. 2011;473:528-531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 873] [Cited by in RCA: 862] [Article Influence: 57.5] [Reference Citation Analysis (0)] |
| 32. | Yang TT, Suk HY, Yang X, Olabisi O, Yu RY, Durand J, Jelicks LA, Kim JY, Scherer PE, Wang Y, Feng Y, Rossetti L, Graef IA, Crabtree GR, Chow CW. Role of transcription factor NFAT in glucose and insulin homeostasis. Mol Cell Biol. 2006;26:7372-7387. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 33. | Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5683] [Cited by in RCA: 6638] [Article Influence: 349.4] [Reference Citation Analysis (2)] |
| 34. | Marangoni F, Cetin I, Verduci E, Canzone G, Giovannini M, Scollo P, Corsello G, Poli A. Maternal Diet and Nutrient Requirements in Pregnancy and Breastfeeding. An Italian Consensus Document. Nutrients. 2016;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 204] [Cited by in RCA: 167] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 35. | Wang Q, Zhu C, Sun M, Maimaiti R, Ford SP, Nathanielsz PW, Ren J, Guo W. Maternal obesity impairs fetal cardiomyocyte contractile function in sheep. FASEB J. 2019;33:2587-2598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 36. | Ng SF, Lin RC, Laybutt DR, Barres R, Owens JA, Morris MJ. Chronic high-fat diet in fathers programs β-cell dysfunction in female rat offspring. Nature. 2010;467:963-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 989] [Cited by in RCA: 985] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 37. | Marotte C, Bryk G, Gonzales Chaves MM, Lifshitz F, de Portela ML, Zeni SN. Low dietary calcium and obesity: a comparative study in genetically obese and normal rats during early growth. Eur J Nutr. 2014;53:769-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Ghaben AL, Scherer PE. Adipogenesis and metabolic health. Nat Rev Mol Cell Biol. 2019;20:242-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 1035] [Article Influence: 147.9] [Reference Citation Analysis (0)] |
| 39. | Wang QA, Tao C, Gupta RK, Scherer PE. Tracking adipogenesis during white adipose tissue development, expansion and regeneration. Nat Med. 2013;19:1338-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 807] [Cited by in RCA: 1022] [Article Influence: 78.6] [Reference Citation Analysis (0)] |
| 40. | Spalding KL, Arner E, Westermark PO, Bernard S, Buchholz BA, Bergmann O, Blomqvist L, Hoffstedt J, Näslund E, Britton T, Concha H, Hassan M, Rydén M, Frisén J, Arner P. Dynamics of fat cell turnover in humans. Nature. 2008;453:783-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1579] [Cited by in RCA: 1623] [Article Influence: 90.2] [Reference Citation Analysis (0)] |
| 41. | Lin H, An Y, Tang H, Wang Y. Alterations of Bile Acids and Gut Microbiota in Obesity Induced by High Fat Diet in Rat Model. J Agric Food Chem. 2019;67:3624-3632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 181] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 42. | Vishvanath L, MacPherson KA, Hepler C, Wang QA, Shao M, Spurgin SB, Wang MY, Kusminski CM, Morley TS, Gupta RK. Pdgfrβ+ Mural Preadipocytes Contribute to Adipocyte Hyperplasia Induced by High-Fat-Diet Feeding and Prolonged Cold Exposure in Adult Mice. Cell Metab. 2016;23:350-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 282] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 43. | Knittle JL, Timmers K, Ginsberg-Fellner F, Brown RE, Katz DP. The growth of adipose tissue in children and adolescents. Cross-sectional and longitudinal studies of adipose cell number and size. J Clin Invest. 1979;63:239-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 240] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 44. | Merrick D, Sakers A, Irgebay Z, Okada C, Calvert C, Morley MP, Percec I, Seale P. Identification of a mesenchymal progenitor cell hierarchy in adipose tissue. Science. 2019;364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 489] [Article Influence: 69.9] [Reference Citation Analysis (0)] |
| 45. | Rosen ED, Sarraf P, Troy AE, Bradwin G, Moore K, Milstone DS, Spiegelman BM, Mortensen RM. PPAR gamma is required for the differentiation of adipose tissue in vivo and in vitro. Mol Cell. 1999;4:611-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1516] [Cited by in RCA: 1590] [Article Influence: 58.9] [Reference Citation Analysis (0)] |
| 46. | Farmer SR. Transcriptional control of adipocyte formation. Cell Metab. 2006;4:263-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1499] [Cited by in RCA: 1459] [Article Influence: 73.0] [Reference Citation Analysis (0)] |
| 47. | Aamir K, Khan HU, Sethi G, Hossain MA, Arya A. Wnt signaling mediates TLR pathway and promote unrestrained adipogenesis and metaflammation: Therapeutic targets for obesity and type 2 diabetes. Pharmacol Res. 2020;152:104602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 75] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 48. | Chen X, Ayala I, Shannon C, Fourcaudot M, Acharya NK, Jenkinson CP, Heikkinen S, Norton L. The Diabetes Gene and Wnt Pathway Effector TCF7L2 Regulates Adipocyte Development and Function. Diabetes. 2018;67:554-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 95] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 49. | Chen Q, Shou P, Zheng C, Jiang M, Cao G, Yang Q, Cao J, Xie N, Velletri T, Zhang X, Xu C, Zhang L, Yang H, Hou J, Wang Y, Shi Y. Fate decision of mesenchymal stem cells: adipocytes or osteoblasts? Cell Death Differ. 2016;23:1128-1139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 606] [Cited by in RCA: 961] [Article Influence: 96.1] [Reference Citation Analysis (0)] |
| 50. | Woeller CF, Lim SA, Roztocil E, Yee M, Beier EE, Puzas JE, O'Reilly MA. Neonatal hyperoxia impairs adipogenesis of bone marrow-derived mesenchymal stem cells and fat accumulation in adult mice. Free Radic Biol Med. 2021;167:287-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 51. | Ishikane S, Ikushima E, Igawa K, Tomooka K, Takahashi-Yanaga F. Differentiation-inducing factor-1 potentiates adipogenic differentiation and attenuates the osteogenic differentiation of bone marrow-derived mesenchymal stem cells. Biochim Biophys Acta Mol Cell Res. 2021;1868:118909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 52. | Oh JH, Karadeniz F, Lee JI, Seo Y, Kong CS. Ligustrum japonicum Thunb. Fruits Exert Antiosteoporotic Properties in Bone Marrow-Derived Mesenchymal Stromal Cells via Regulation of Adipocyte and Osteoblast Differentiation. Stem Cells Int. 2021;2021:8851884. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 53. | Baer PC, Koch B, Hickmann E, Schubert R, Cinatl J Jr, Hauser IA, Geiger H. Isolation, Characterization, Differentiation and Immunomodulatory Capacity of Mesenchymal Stromal/Stem Cells from Human Perirenal Adipose Tissue. Cells. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 54. | Qu P, Wang L, Min Y, McKennett L, Keller JR, Lin PC. Vav1 Regulates Mesenchymal Stem Cell Differentiation Decision Between Adipocyte and Chondrocyte via Sirt1. Stem Cells. 2016;34:1934-1946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 55. | Fan J, Lee CS, Kim S, Zhang X, Pi-Anfruns J, Guo M, Chen C, Rahnama M, Li J, Wu BM, Aghaloo TL, Lee M. Trb3 controls mesenchymal stem cell lineage fate and enhances bone regeneration by scaffold-mediated local gene delivery. Biomaterials. 2021;264:120445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 56. | Li Y, Stahl CH. Dietary calcium deficiency and excess both impact bone development and mesenchymal stem cell lineage priming in neonatal piglets. J Nutr. 2014;144:1935-1942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 57. | Casado-Díaz A, Anter J, Müller S, Winter P, Quesada-Gómez JM, Dorado G. Transcriptomic Analyses of Adipocyte Differentiation From Human Mesenchymal Stromal-Cells (MSC). J Cell Physiol. 2017;232:771-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 58. | Fellous T, De Maio F, Kalkan H, Carannante B, Boccella S, Petrosino S, Maione S, Di Marzo V, Iannotti FA. Phytocannabinoids promote viability and functional adipogenesis of bone marrow-derived mesenchymal stem cells through different molecular targets. Biochem Pharmacol. 2020;175:113859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 59. | Platt ID, El-Sohemy A. Regulation of osteoblast and adipocyte differentiation from human mesenchymal stem cells by conjugated linoleic acid. J Nutr Biochem. 2009;20:956-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 60. | Ye J, Gong P. NGF-CS/HA-coating composite titanium facilitates the differentiation of bone marrow mesenchymal stem cells into osteoblast and neural cells. Biochem Biophys Res Commun. 2020;531:290-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 61. | Salehi A, Mobarhan MA, Mohammadi J, Shahsavarani H, Shokrgozar MA, Alipour A. Efficient mineralization and osteogenic gene overexpressions of mesenchymal stem cells on decellularized spinach leaf scaffold. Gene. 2020;757:144852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 62. | Bae YK, Kim GH, Kwon JH, Kim M, Choi SJ, Oh W, Um S, Jin HJ. Primary Cilia Mediate Wnt5a/β-catenin Signaling to Regulate Adipogenic Differentiation of Human Umbilical Cord Blood-Derived Mesenchymal Stem Cells Following Calcium Induction. Tissue Eng Regen Med. 2020;17:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 63. | Karam M, Younis I, Elareer NR, Nasser S, Abdelalim EM. Scalable Generation of Mesenchymal Stem Cells and Adipocytes from Human Pluripotent Stem Cells. Cells. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 64. | Lorthongpanich C, Thumanu K, Tangkiettrakul K, Jiamvoraphong N, Laowtammathron C, Damkham N, U-Pratya Y, Issaragrisil S. YAP as a key regulator of adipo-osteogenic differentiation in human MSCs. Stem Cell Res Ther. 2019;10:402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 65. | Hu L, Yin C, Zhao F, Ali A, Ma J, Qian A. Mesenchymal Stem Cells: Cell Fate Decision to Osteoblast or Adipocyte and Application in Osteoporosis Treatment. Int J Mol Sci. 2018;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 317] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 66. | Meyer MB, Benkusky NA, Sen B, Rubin J, Pike JW. Epigenetic Plasticity Drives Adipogenic and Osteogenic Differentiation of Marrow-derived Mesenchymal Stem Cells. J Biol Chem. 2016;291:17829-17847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 136] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cell and tissue engineering
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li Y, China; Prasetyo EP, Indonesia; Wei Z, United States S-Editor: Fan JR L-Editor: Kerr C P-Editor: Zhang XD