Published online May 26, 2021. doi: 10.4252/wjsc.v13.i5.331
Peer-review started: February 12, 2021
First decision: March 17, 2021
Revised: March 27, 2021
Accepted: April 14, 2021
Article in press: April 14, 2021
Published online: May 26, 2021
Processing time: 102 Days and 20.6 Hours
Ethical concerns about stem cell-based research have delayed important advances in many areas of medicine, including cardiology. The introduction of induced pluripotent stem cells (iPSCs) has supplanted the need to use human stem cells for most purposes, thus eliminating all ethical controversies. Since then, many new avenues have been opened in cardiology research, not only in approaches to tissue replacement but also in the design and testing of antiarrhythmic drugs. This methodology has advanced to the point where induced human cardiomyocyte cell lines can now also be obtained from commercial sources or tissue banks. Initial studies with readily available iPSCs have generally confirmed that their behavioral characteristics accurately predict the behavior of beating cardio
Core Tip: The introduction of induced pluripotent stem cells (iPSCs) has supplanted the need for human stem cells, thus eliminating most ethical controversies. This methodology has advanced to the point where induced human cardiomyocyte cell lines can also be obtained from commercial sources or tissue banks. iPSCs can predict the behavior of cardiomyocytes in vivo, so that new ways are paved in cardiology research to study arrhythmias and heart disease in general, accelerating the development of new, more effective antiarrhythmic drugs, clinical diagnoses, and personalized medical care.
- Citation: Karch SB, Fineschi V, Francia P, Scopetti M, Padovano M, Manetti F, Santurro A, Frati P, Volpe M. Role of induced pluripotent stem cells in diagnostic cardiology. World J Stem Cells 2021; 13(5): 331-341
- URL: https://www.wjgnet.com/1948-0210/full/v13/i5/331.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v13.i5.331
Human induced pluripotent stem cells (iPSCs) are produced by reprogramming adult mesenchymal cells, most often fibroblasts. The process is complicated, requiring the introduction and activation of four gene regulatory networks, each comprised of molecular regulators that interact with each other and with other substances in the cell to control gene expression of mRNA and protein-specific genes. Acting together these four transcription factors can produce mature cells that behave in a completely different manner to the original fibroblasts used to form them, leading to the formation of multiple cell types[1-3].
Myocytes created from fibroblasts are basically identical to native cardiomyocytes. There are three different types of native cardiomyocytes, and iPSC production yields all three types in variable and unpredictable proportions, presenting difficulties for researchers. The most obvious and most publicized cardiological application of iPSCs is the production of new cardiac tissue to replace tissues destroyed by infarction or other diseases[4-9], but this goal has yet to be successfully realized in humans. Initially, this was partly because the subtype of iPSCs could not be assured. Obviously, atrial cardiomyocytes would not be a suitable substitute for damaged ventricular cardiomyocytes and, regardless, there is always the danger that introducing a mixture of cells might lead to teratoma formation[10]. Nonetheless, substantial advances have already been made, and success seems to be mainly a matter of time. Once these problems have been fully resolved, iPSCs, in various configurations, could be used to repair damaged hearts. They could also be used to predict interactions between drugs and the cardiac conduction system.
The occurrence of any specific conduction abnormality - including QT prolongation, altered action potential duration, triggered activity, the blockade of human-ether-a-go-go-related channel (hERG) and other ion conduction channels-and the occurrence of lethal arrhythmias-such as Torsades de Pointes (TdP)-cannot reliably be predicted with currently available screening methods (Langendorf preparations, patch-clamp, or even arterially perfused isolated rabbit left ventricular wedge)[11]. Animal models are problematic predictors of arrhythmia occurrence because of anatomic varia
The problems associated with the use of amiodarone and sotalol illustrate the difficulties of drug development[18,19]. Both drugs are used to treat atrial and ventricular tachyarrhythmias and can be life-saving, but can also produce lethal side effects. Unfortunately, predicting side effects is, at this moment, impossible. Amiodarone’s most feared side effect is fatal pulmonary interstitial fibrosis, but hepatitis, hypothyroidism (probably irreversible) and mixed sensorimotor polyneuropathy have all been reported with some regularity. Amiodarone’s most important complications are QT prolongation and TdP[20]. If new and safer replacement drugs are ever to be developed and approved by the United States Food and Drug Administration and the European Medicines Agency, developers will first have to establish that new drugs do not produce predictable untoward side effects or exacerbate the conditions they were designed to treat.
The availability of iPSCs allows researchers to make reasonably accurate predictions about what effect any new drug will have on the heart and its electrical system. Cultured iPSCs, can be used to construct in vitro models of the human cardiac conduction system. The effects observed in vitro can then be used to predict how, and/or whether, a drug will alter electrical conduction, or produce structural alterations in humans. The process is not as simple as it sounds and some knowledge of the subject is crucial to clinicians for the safe use of new drugs.
Cures for cardiac conduction diseases will only be found when their root causes are fully elucidated. Even physicians who have nothing to do with arrhythmia research should retain some knowledge of the molecular biology that underlies cardiac conduction.
The cardiomyocyte repolarization/depolarization cycle begins with a current generated by the outward flow of potassium ions through specific pores or channels. Potassium pores exist in all life forms and many different types have been identified (more than 20). Two types of potassium channels are absolutely critical to the process of cardiac repolarization: The rapid delayed rectifier current (identified as IKr) and the slow delayed rectifier current (identified as IKs). If a drug or a mutation disrupts either of these two currents, the action potential of the cell is prolonged with an increase in the time required for electrical depolarization and repolarization of the ventricles[21]. Prolonged repolarization leads to the occurrence of early after depolarization (EAD) currents. EADs are dangerous because they favor the occurrence of triggered activity (defined as the occurrence of spontaneous action potentials occurring during phase 2 or phase 3 of repolarization, leading to the production of inappropriate action potentials and arrhythmia)[12]. Blockade of the IKr also causes the QT interval to be prolonged, leading to the triggered activity via a slightly different mechanism[22]. Such a situation is likely to occur when a drug molecule interferes with potassium channels as in the case of type III antiarrhythmic drugs. Slowing of the potassium current is associated with a repolarization dispersion, where one area of the myocardium recovers from depolarization faster than an adjoining region, which also makes TdP more likely to occur[23]. Repolarization dispersion is thought to be the reason that myocardial hypertrophy is associated with arrhythmias[24]. The farther the depolarization front has to travel, the greater the interval between depolarization and repolarization. Dispersion is especially likely to occur if the area of abnormal delay and dispersion is located within the Purkinje system or, alternatively, if the area is located in the mid-wall of the left ventricle where the “M cells” are located. These cells have prolonged action potentials that act to further increase the dispersion of repolarization, making the occurrence of TdP ever more likely[25]. For a new antiarrhythmic drug to be introduced, it must first be proven that it exerts none of the effects enumerated above.
Sudden cardiac death (SCD) due to ventricular tachycardia (VT) or ventricular fibrillation (VF) accounts for approximately half of all deaths in patients with heart failure (HF) and may be considered a heritable trait[26-32]. Current guidelines[33] recommend an implantable cardioverter-defibrillator (ICD) in patients with symptomatic and severe left ventricular dysfunction of any origin. However, SCD may occur in asymptomatic patients with only mild HF. On the contrary, as many as two-thirds of patients with severe HF implanted with an ICD do not experience device interventions over 3 to 5 years follow-up[34]. A similar clinical scenario leaves unanswered the question of whether selected gene variants may affect the risk of SCD in HF patients. Genomic science provides us with new approaches to identify gene variants or mutations that predispose patients with inherited electrical diseases to SCD. However, a growing body of evidence suggests that DNA changes in the same genes that convey risk in primary electrical diseases may enhance susceptibility to VT/VF even in a polygenic condition such as HF. Sustained VT and VF often occur as a consequence of delayed after-depolarizations triggered by diastolic sarcoplasmic reticulum (SR) calcium leak[35]. Genes encoding calcium handling proteins involved in electrical homeostasis of the failing heart may represent suitable candidates for defining individual susceptibility to life-threatening arrhythmia[26,27]. However, only very few genes belonging to the major candidate systems have been characterized and screened for possible association with SCD in HF. The cardiac ryanodine receptor 2 (RyR2), a calcium-releasing channel located in the SR membrane, plays a key role in the electrical homeostasis of cardiomyocytes. RyR2 dysfunction has been described in both HF patients and animal models and is critical to many of the aspects of the disease, including life-threatening arrhythmia[36]. In a large cohort of HF patients, Ran et al[37] found that the A allele of RYR2 c.5656G>A was associated with an increased risk of SCD. Arvanitis et al[38] reported that the Ser96Ala variant in histidine-rich calcium-binding protein was associated with ventricular arrhythmia in idiopathic dilated cardiomyopathy. It is known that a serine residue replacing glycine at position 1886 (G1886S or rs3766871) in the RyR2 gene prompts a significant increase in intracellular calcium oscillation and creates a site of phosphorylation for protein kinase C (PKC) entailing PKC-mediated calcium diastolic leak from the SR[39,40]. While the RYR2 rs3766871 variant has been previously described only in the setting of arrhythmogenic right ventricular cardiomyopathy, a role of RyR2 rs3766871 minor allele for increased susceptibility to VT/VF has been recently reported also in patients with HF[41]. The SERCA calcium ATPase (ATP2A2) belongs to a large family of P-type cation pumps that couple adenosine triphosphate (ATP) hydrolysis with cation transport across membranes[42]. Alternative splicing of the ATP2A2 gene produces two isoforms, SERCA2a (primarily located in the heart and slow-twitch skeletal muscle) and SERCA2b (present in smooth muscle and non-muscle tissues). Mutations in the ATP2A2 gene affect the expression level, ATP affinity, calcium affinity, and phosphorylation of ATP. In an attempt to investigate whether variants of the genes encoding major calcium handling proteins affect the occurrence of VT/VF in HF patients, it was found that the ATP2A2 c.2741+54G>A gene variant was associated with decreased susceptibility to life-threatening arrhythmia. Indeed, patients carrying the ATP2A2 c.2741+54A allele variant had an approximately 70% reduction in the relative risk of VT/VF during follow-up[43]. Defective calcium handling in failing cardiomyocytes has long been recognized as a cause of ventricular arrhythmia, and recent evidence suggests that selected calcium gene variants may modify the risk of SCD even in a complex and polygenic disease such as HF. While statistically associated with a modified risk of SCD, the biological role of many of these gene variants is presently unknown. The recent breakthrough discovery of iPSCs could enable the investigation of mutated cardiomyocytes generated from patient’s somatic cells, allowing functional characterization of iPSC-derived mutated cardiomyocytes. A similar approach represents an interesting and promising solution for the biological relevance of genetic substrates in secondary arrhythmogenic conditions.
Microelectrode arrays are used in many fields of study, although the basics of the system are the same no matter what kind of test is being performed; improvements and refinements in this methodology are being reported almost continuously. These tests are performed in wells that look just like those in any clinical laboratory test plate used to observe chemical reactions, however, they differ in one important respect; electrodes are located at the bottom of each well.
When the electrodes and iPSCs are joined together they form the backbone of the system. The idea was derived from earlier networking studies, designed to test neural interactions. Networking electrodes were originally made of titanium salts and gold conductors[44], but other materials have been used. The system is now so advanced that these wells, indeed, the entire networking system, including software, are all available off the shelf.
IPSCs, can either be studied singly or as part of an integrated network. For most intents and purposes these cells have all the same capabilities as embryonic stem cells that have been allowed to mature. In 2012, Shinya Yamanaka outlined a method to induce pluripotency by inserting genes that acted as reprogramming factors, also called transduction factors, by attaching them to carrier viruses and inserting the virus into the cells, which eventually causes the cells to express the exogenous genes. The cells are then cultured and finally harvested[45]. Since the technique was first introduced, many other iPSCs, and related transcription factors, have been identified and used, including, miRNAs (a type of non-coding RNA that inhibits translation in many species). Whatever the precise role of these diverse factors, other epigenetic processes are critical for the process of converting maturing stem cells back to inducible pluripotent cells[46].
Once the multiple electrode arrays have been constructed, beating cardiomyocytes, derived from pluripotent stem cells are plated over each well, without the electrodes ever actually penetrating the cells. Such a methodology essentially recreates many aspects of a working myocardium, including the generation of waveforms not very different from those seen on clinical electrocardiograms. Introducing an experimental drug into the system, the probable effect on a beating human heart can be confirmed with a high degree of accuracy.
For example, experimental drugs have been tested in networked iPSCs that alter the duration and shape of the QT interval in almost exactly the same pattern as seen in humans. Not only do drugs produce the same electrocardiographic changes, but physiological stressors also produce changes similar to those that occur in vivo with the same rate and QT interval alterations seen in humans[47,48]. If animal studies suggest that a drug can cause dangerous QT prolongation, it is simple enough to test the drug on networked beating human cardiomyocytes. Another obvious application of this technology is the measurement of calcium transients by using fluorescence microscopy. Calcium indicators are introduced into the cells and the resulting fluorescence can be quantitated noninvasively and used to measure calcium ion flux, which controls inotropy. In the past, such experiments required the use of isolated small animal muscle[49].
The same type of cellular network can be used to study the effect of genetic mutations known to cause cardiac arrhythmias, including channelopathies such as hERG; more than 90 long QT syndrome (LQTS) mutations have been mapped to date. It is possible to measure the effect of mutations on IKr and IKs, although debate still exists over the exact mechanism by which some mutations alter potassium flow, answers to at least some of these questions should soon be forthcoming[50]. With the availability of high-throughput networked cardiomyocytes, it is now possible to evaluate a drug’s effects on potassium flow before it is ever given to an animal, let alone evaluated in human clinical trials.
IPSCs from a patient with a novel KCNQ mutation were used by Egashira et al[51] to identify the mutation. The patient had survived VF, thanks to the nearby presence of an automated external defibrillator. Using a slight variation multi-electrode array system (where the electrical activity of clumps of cells, rather than sheets of cells was measured), abnormal repolarization, as manifested by electrical field potential duration, was observed in the spontaneously beating iPSC cardiomyocytes. Egashira et al[51] then added an assortment of potassium ingress and egress blockers to prove that the repolarization abnormality lay within the slow inward potassium channel[51]. At present, the technology is too cumbersome for routine clinical use. In the future, however, it should be possible to use this approach when exome screening fails to identify one of the usual culprits.
The recent discovery of the TECRL gene, an arrhythmia-inducing gene that produces features of catecholaminergic VT (CPVT) and LQTS, was accomplished using much the same technology[52]. Three patients were studied; two with a history of cardiac arrest and one with an episode of recorded CPVT. Once iPSCs had been produced and the mutation identified and sequenced, electrophysiological studies were then performed. These demonstrated exactly the same features (catecholamine sensitivity, triggered activity, delayed afterdepolarizations as had been seen in the patients. The abnormalities were all reversed by the addition of flecainide, a class 1c antiarrhythmic drug. Had iPSCs not been available, finding a remedy would have been purely by empiric trial and error. However, the real significance of the study is that there is now a reliable methodology with which to screen drugs for effectiveness.
Even without going to the effort of creating an entire iPSCs network, it is still possible to clinically diagnose some disorders from the electrical behavior of a single iPSC. A very recent report describes two patients with known Brugada Syndrome. When compared to the findings in two healthy controls, it was observed that each of the Brugada Syndrome patients carried one of two different sodium voltage-gated channel alpha and subunit 5 variants. The electrical characteristics of iPSCs produced from the patient's own skin fibroblasts were studied. The studies showed reductions in inward sodium current density and reduced maximal upstroke velocity of action potential when compared with healthy controls. Furthermore, iPSC cardiomyocytes from the Brugada Syndrome patients demonstrated increased triggered activity, abnormal calcium (Ca2fl) transients, and beating interval variation, the very same abnormalities previously reported in other studies, using different methodologies[53]. Late in 2016, a study using individual iPSCs was used to confirm results observed in a previous knock out mouse study. The studies had suggested the existence of a new cardiac regulatory mechanism that appeared to play a key role in the association between arrhythmias and myocardial hypertrophy. When the mouse studies were repeated in human iPSCs, it was possible to confirm that the same stress-activated kinase was operative in human cells[54].
Another obvious application for iPSCs is screening for suspected heart disease, and for determining the significance of a mutation once it has been identified. Hypertrophic cardiomyopathy (HCM) is a very good example. The clinical diagnosis can be difficult to make (left ventricular hypertrophy with wall thickness > 15 mm, in the absence of ventricular dilation or any apparent disease that could cause hypertrophy)[55]. Unfortunately, it is not uncommon for there to be a complete disconnect between phenotype and genotype: Abnormal genes may be present but symptoms and signs absent.
Both sarcomeric mutations and non-sarcomeric mutations in HCM can be identified by whole-exome sequencing, and these studies demonstrate that the same genotype may be responsible for sudden death in one individual, but remain asymptomatic in another[56]. Multiple mutations have been detected in patients with HCM: Nine sarcomeric genes are known to carry most HCM-related mutations and encode sarcomeric mutations, while an additional nine mutations code for sarcomeric Z-disc proteins such as muscle LIM protein, α-actinin, or telethonin[57,58].
Since iPSCs cardiomyocytes became available, the pathogenic effects of some mutations (MYH7 and MYBPC3) associated with HCM have already been identified[59], and calcium blockade has been found to be an effective treatment for another HCM mutation (MYH7-R663H)[60]. Whole-exome sequencing almost never yields the identity of a single culprit gene, but rather detects multiple mutations, some of which may be relevant and some not. If one single mutation is responsible for the obvious phenotype of HCM, it has yet to be identified. It hardly needs saying, but exactly the same methodology used to identify culprit genes could be applied to genomic studies of countless other disorders, just by inducing the required cell type from transformed fibroblasts.
Overcoming the ethical problems related to the use of stem cells through the introduction of iPSCs opens up an interesting scenario on the study of the cellular basis of diseases[61,62]. The use of pluripotent cells makes it possible to reproduce models for the study of cardiological pathologies which frequently cause SCD and are often diagnosed post-mortem such as structural cardiomyopathies and channel
Furthermore, iPSCs can be exploited in the personalization of therapies in relation to the possibility of carrying out pharmacological tests on cells derived from the patient[67-70].
Although the principles are easy to understand, at present there are some important caveats. One is that fibroblast generated iPSCs demonstrate an immature phenotype so that they more closely resemble mid-gestation human fetal hearts[71-73]. These differences may well alter final experimental and clinical results, depending on the stage of development of the iPSCs being used. When used in other fields, the same caveat applies. Now that this difference has been recognized, finding ways to make sure the cells are organized and function as adult cells is the object of intense research, which has already begun to generate results. Recent reports indicate that iPSCs can be stimulated and made to mature by a combination of pacing and increasing mechanical stress[74-77].
Another issue that had been delaying progress is that protocols used to produce iPSCs do not produce just one kind of cell, but rather yield a mixed population of cardiomyocyte subtypes including ventricular-, atrial- and pacemaker-like cells[78-81]. Birket and colleagues[82] made the early observation that even though the iPSCs can behave like normal human cardiomyocytes, the production process leads to unequal numbers of each of the subtypes. Obviously, different results will be generated depending on which type of cell predominates. Many laboratories are working on effective cell separation methods and standardized methods should soon be available.
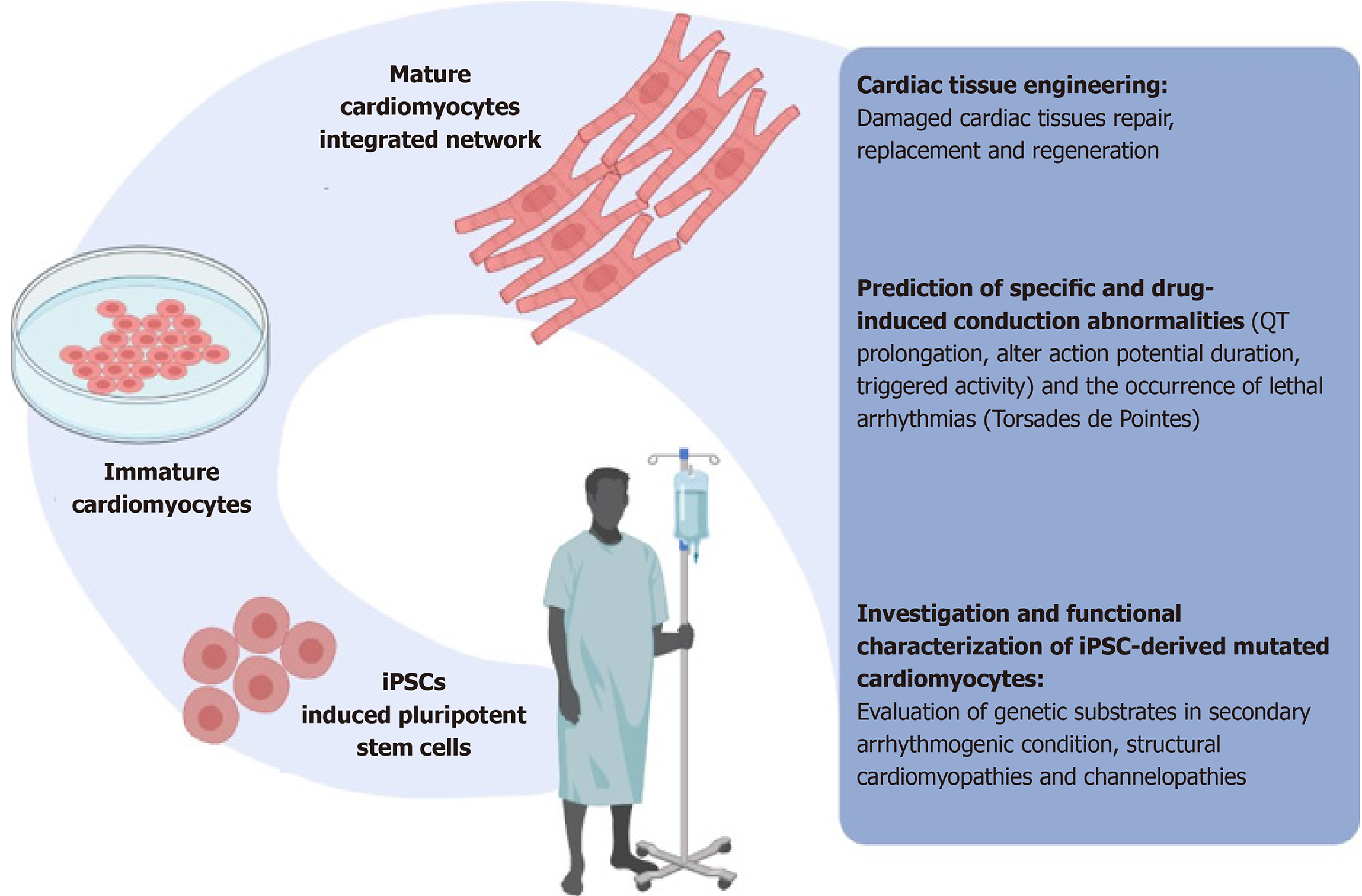
In summary, the main applications of stem cells include disease modeling, cell diagnostics, and therapy personalization (Figure 1). Such tasks involve molecular profiling, the identification of biomarkers of the expression of the pathological phenotype, as well as the identification and testing of targeted therapies. The availability of pluripotent cardiac stem cells, especially networked beating cardiomyocytes, is likely to revolutionize our understanding of many cardiac rhythm disorders and diseases, provide a rational testing method for the development of drugs, permit clinicians to assess effectiveness before drug administration and, most importantly, save lives.
| 1. | Sasaki K, Makiyama T, Yoshida Y, Wuriyanghai Y, Kamakura T, Nishiuchi S, Hayano M, Harita T, Yamamoto Y, Kohjitani H, Hirose S, Chen J, Kawamura M, Ohno S, Itoh H, Takeuchi A, Matsuoka S, Miura M, Sumitomo N, Horie M, Yamanaka S, Kimura T. Patient-Specific Human Induced Pluripotent Stem Cell Model Assessed with Electrical Pacing Validates S107 as a Potential Therapeutic Agent for Catecholaminergic Polymorphic Ventricular Tachycardia. PLoS One. 2016;11:e0164795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Staerk J, Dawlaty MM, Gao Q, Maetzel D, Hanna J, Sommer CA, Mostoslavsky G, Jaenisch R. Reprogramming of human peripheral blood cells to induced pluripotent stem cells. Cell Stem Cell. 2010;7:20-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 354] [Cited by in RCA: 320] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 3. | Peerani R, Rao BM, Bauwens C, Yin T, Wood GA, Nagy A, Kumacheva E, Zandstra PW. Niche-mediated control of human embryonic stem cell self-renewal and differentiation. EMBO J. 2007;26:4744-4755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 300] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 4. | Radisic M, Christman KL. Materials science and tissue engineering: repairing the heart. Mayo Clin Proc. 2013;88:884-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Marion MH, Bax NA, Spreeuwel AC, van der Schaft DW, Bouten CV. Material-based engineering strategies for cardiac regeneration. Curr Pharm Des. 2014;20:2057-2068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Venugopal JR, Prabhakaran MP, Mukherjee S, Ravichandran R, Dan K, Ramakrishna S. Biomaterial strategies for alleviation of myocardial infarction. J R Soc Interface. 2012;9:1-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 156] [Cited by in RCA: 139] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Wu J, Zeng F, Weisel RD, Li RK. Stem cells for cardiac regeneration by cell therapy and myocardial tissue engineering. Adv Biochem Eng Biotechnol. 2009;114:107-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Finosh GT, Jayabalan M. Regenerative therapy and tissue engineering for the treatment of end-stage cardiac failure: new developments and challenges. Biomatter. 2012;2:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Roccio M, Goumans MJ, Sluijter JP, Doevendans PA. Stem cell sources for cardiac regeneration. Panminerva Med. 2008;50:19-30. [PubMed] |
| 10. | Talkhabi M, Aghdami N, Baharvand H. Human cardiomyocyte generation from pluripotent stem cells: A state-of-art. Life Sci. 2016;145:98-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Lu HR, Gallacher DJ, Yan GX. Assessment of drug-induced proarrhythmia: The importance of study design in the rabbit left ventricular wedge model. J Pharmacol Toxicol Methods. 2016;81:151-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Hundahl LA, Tfelt-Hansen J, Jespersen T. Rat Models of Ventricular Fibrillation Following Acute Myocardial Infarction. J Cardiovasc Pharmacol Ther. 2017;22:514-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Dobrev D, Wehrens XHT. Mouse Models of Cardiac Arrhythmias. Circ Res. 2018;123:332-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Yong SL, Wang QK. Animal models for cardiac arrhythmias. Methods Mol Med. 2006;129:127-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Schwartz PJ. Do animal models have clinical value? Am J Cardiol. 1998;81:14D-20D. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Clauss S, Bleyer C, Schüttler D, Tomsits P, Renner S, Klymiuk N, Wakili R, Massberg S, Wolf E, Kääb S. Animal models of arrhythmia: classic electrophysiology to genetically modified large animals. Nat Rev Cardiol. 2019;16:457-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 159] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 17. | Dubois VF, Casarotto E, Danhof M, Della Pasqua O. Pharmacokinetic-pharmacodynamic modelling of drug-induced QTc interval prolongation in man: prediction from in vitro human ether-à-go-go-related gene binding and functional inhibition assays and conscious dog studies. Br J Pharmacol. 2016;173:2819-2832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | van Opstal JM, Schoenmakers M, Verduyn SC, de Groot SH, Leunissen JD, van Der Hulst FF, Molenschot MM, Wellens HJ, Vos MA. Chronic amiodarone evokes no torsade de pointes arrhythmias despite QT lengthening in an animal model of acquired long-QT syndrome. Circulation. 2001;104:2722-2727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 139] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Semasinghe Bandaralage SP, Nirthanan S, Niranjan S. Does Sotalol Still Have a Role in the Management of Arrhythmias? Am J Ther. 2019;26:e161-e169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Tran HT, Chow MS, Kluger J. Amiodarone induced torsades de pointes with excessive QT dispersion following quinidine induced polymorphic ventricular tachycardia. Pacing Clin Electrophysiol. 1997;20:2275-2278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Yap YG, Camm AJ. Drug induced QT prolongation and torsades de pointes. Heart. 2003;89:1363-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 694] [Cited by in RCA: 684] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 22. | Zhou YY, Liu TF. The ionic mechanisms of early after depolarization in mouse ventricular myocytes: the role of IK1. Methods Find Exp Clin Pharmacol. 1997;19:443-453. [PubMed] |
| 23. | Burton FL, Cobbe SM. Dispersion of ventricular repolarization and refractory period. Cardiovasc Res. 2001;50:10-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 91] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 24. | Kang YJ. Cardiac hypertrophy: a risk factor for QT-prolongation and cardiac sudden death. Toxicol Pathol. 2006;34:58-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Henry H, Rappel WJ. The role of M cells and the long QT syndrome in cardiac arrhythmias: simulation studies of reentrant excitations using a detailed electrophysiological model. Chaos. 2004;14:172-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Darbar D. Genomics, heart failure and sudden cardiac death. Heart Fail Rev. 2010;15:229-238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Gollob MH. Genetic profiling as a marker for risk of sudden cardiac death. Curr Opin Cardiol. 2006;21:42-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Osman J, Tan SC, Lee PY, Low TY, Jamal R. Sudden Cardiac Death (SCD) - risk stratification and prediction with molecular biomarkers. J Biomed Sci. 2019;26:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 29. | Backer J, Braverman AC. Heart failure and sudden cardiac death in heritable thoracic aortic disease caused by pathogenic variants in the SMAD3 gene. Mol Genet Genomic Med. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 30. | Wei D, Tao L, Huang M. Genetic variations involved in sudden cardiac death and their associations and interactions. Heart Fail Rev. 2016;21:401-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Arking DE, Chugh SS, Chakravarti A, Spooner PM. Genomics in sudden cardiac death. Circ Res. 2004;94:712-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 66] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Kolder IC, Tanck MW, Bezzina CR. Common genetic variation modulating cardiac ECG parameters and susceptibility to sudden cardiac death. J Mol Cell Cardiol. 2012;52:620-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 33. | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147-e239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4116] [Cited by in RCA: 4716] [Article Influence: 362.8] [Reference Citation Analysis (1)] |
| 34. | Yap YG, Duong T, Bland M, Malik M, Torp-Pedersen C, Køber L, Connolly SJ, Marchant B, Camm J. Temporal trends on the risk of arrhythmic vs. non-arrhythmic deaths in high-risk patients after myocardial infarction: a combined analysis from multicentre trials. Eur Heart J. 2005;26:1385-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 35. | Scoote M, Williams AJ. Myocardial calcium signalling and arrhythmia pathogenesis. Biochem Biophys Res Commun. 2004;322:1286-1309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Periasamy M, Bhupathy P, Babu GJ. Regulation of sarcoplasmic reticulum Ca2+ ATPase pump expression and its relevance to cardiac muscle physiology and pathology. Cardiovasc Res. 2008;77:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 189] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 37. | Ran Y, Chen J, Li N, Zhang W, Feng L, Wang R, Hui R, Zhang S, Pu J. Common RyR2 variants associate with ventricular arrhythmias and sudden cardiac death in chronic heart failure. Clin Sci (Lond). 2010;119:215-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 38. | Arvanitis DA, Sanoudou D, Kolokathis F, Vafiadaki E, Papalouka V, Kontrogianni-Konstantopoulos A, Theodorakis GN, Paraskevaidis IA, Adamopoulos S, Dorn GW 2nd, Kremastinos DT, Kranias EG. The Ser96Ala variant in histidine-rich calcium-binding protein is associated with life-threatening ventricular arrhythmias in idiopathic dilated cardiomyopathy. Eur Heart J. 2008;29:2514-2525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 39. | Koop A, Goldmann P, Chen SR, Thieleczek R, Varsányi M. ARVC-related mutations in divergent region 3 alter functional properties of the cardiac ryanodine receptor. Biophys J. 2008;94:4668-4677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 40. | Milting H, Lukas N, Klauke B, Körfer R, Perrot A, Osterziel KJ, Vogt J, Peters S, Thieleczek R, Varsányi M. Composite polymorphisms in the ryanodine receptor 2 gene associated with arrhythmogenic right ventricular cardiomyopathy. Cardiovasc Res. 2006;71:496-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 41. | Francia P, Adduci C, Semprini L, Stanzione R, Serdoz A, Caprinozzi M, Santini D, Cotugno M, Palano F, Musumeci MB, Rubattu S, Volpe M. RyR2 Common Gene Variant G1886S and the Risk of Ventricular Arrhythmias in ICD Patients with Heart Failure. J Cardiovasc Electrophysiol. 2015;26:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Sakuntabhai A, Burge S, Monk S, Hovnanian A. Spectrum of novel ATP2A2 mutations in patients with Darier's disease. Hum Mol Genet. 1999;8:1611-1619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 120] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 43. | Lelakowski J, Piekarz J, Rydlewska A, Majewski J, Senderek T, Ząbek A, Małecka B. Factors predisposing to ventricular tachyarrhythmia leading to appropriate ICD intervention in patients with coronary artery disease or non-ischaemic dilated cardiomyopathy. Kardiol Pol. 2012;70:1264-1275. [PubMed] |
| 44. | Asai Y, Tada M, Otsuji TG, Nakatsuji N. Combination of functional cardiomyocytes derived from human stem cells and a highly-efficient microelectrode array system: an ideal hybrid model assay for drug development. Curr Stem Cell Res Ther. 2010;5:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 45. | Shi Y, Desponts C, Do JT, Hahm HS, Schöler HR, Ding S. Induction of pluripotent stem cells from mouse embryonic fibroblasts by Oct4 and Klf4 with small-molecule compounds. Cell Stem Cell. 2008;3:568-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 666] [Cited by in RCA: 643] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 46. | Lakshmipathy U, Davila J, Hart RP. miRNA in pluripotent stem cells. Regen Med. 2010;5:545-555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 47. | Clements M, Thomas N. High-throughput multi-parameter profiling of electrophysiological drug effects in human embryonic stem cell derived cardiomyocytes using multi-electrode arrays. Toxicol Sci. 2014;140:445-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 126] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 48. | Nozaki Y, Honda Y, Watanabe H, Saiki S, Koyabu K, Itoh T, Nagasawa C, Nakamori C, Nakayama C, Iwasaki H, Suzuki S, Washio I, Takahashi E, Miyamoto K, Yamanishi A, Endo H, Shinozaki J, Nogawa H, Kunimatsu T. CSAHi study: Validation of multi-electrode array systems (MEA60/2100) for prediction of drug-induced proarrhythmia using human iPS cell-derived cardiomyocytes -assessment of inter-facility and cells lot-to-lot-variability. Regul Toxicol Pharmacol. 2016;77:75-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 49. | Laurila E, Ahola A, Hyttinen J, Aalto-Setälä K. Methods for in vitro functional analysis of iPSC derived cardiomyocytes - Special focus on analyzing the mechanical beating behavior. Biochim Biophys Acta. 2016;1863:1864-1872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 50. | Keating MT, Sanguinetti MC. Molecular and cellular mechanisms of cardiac arrhythmias. Cell. 2001;104:569-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 766] [Cited by in RCA: 710] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 51. | Egashira T, Yuasa S, Suzuki T, Aizawa Y, Yamakawa H, Matsuhashi T, Ohno Y, Tohyama S, Okata S, Seki T, Kuroda Y, Yae K, Hashimoto H, Tanaka T, Hattori F, Sato T, Miyoshi S, Takatsuki S, Murata M, Kurokawa J, Furukawa T, Makita N, Aiba T, Shimizu W, Horie M, Kamiya K, Kodama I, Ogawa S, Fukuda K. Disease characterization using LQTS-specific induced pluripotent stem cells. Cardiovasc Res. 2012;95:419-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 134] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 52. | Devalla HD, Gélinas R, Aburawi EH, Beqqali A, Goyette P, Freund C, Chaix MA, Tadros R, Jiang H, Le Béchec A, Monshouwer-Kloots JJ, Zwetsloot T, Kosmidis G, Latour F, Alikashani A, Hoekstra M, Schlaepfer J, Mummery CL, Stevenson B, Kutalik Z, de Vries AA, Rivard L, Wilde AA, Talajic M, Verkerk AO, Al-Gazali L, Rioux JD, Bhuiyan ZA, Passier R. TECRL, a new life-threatening inherited arrhythmia gene associated with overlapping clinical features of both LQTS and CPVT. EMBO Mol Med. 2016;8:1390-1408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 100] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 53. | Liang P, Sallam K, Wu H, Li Y, Itzhaki I, Garg P, Zhang Y, Vermglinchan V, Lan F, Gu M, Gong T, Zhuge Y, He C, Ebert AD, Sanchez-Freire V, Churko J, Hu S, Sharma A, Lam CK, Scheinman MM, Bers DM, Wu JC. Patient-Specific and Genome-Edited Induced Pluripotent Stem Cell-Derived Cardiomyocytes Elucidate Single-Cell Phenotype of Brugada Syndrome. J Am Coll Cardiol. 2016;68:2086-2096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 171] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 54. | Chowdhury SK, Liu W, Zi M, Li Y, Wang S, Tsui H, Prehar S, Castro S, Zhang H, Ji Y, Zhang X, Xiao R, Zhang R, Lei M, Cyganek L, Guan K, Millar CB, Liao X, Jain MK, Boyett MR, Cartwright EJ, Shiels HA, Wang X. Stress-Activated Kinase Mitogen-Activated Kinase Kinase-7 Governs Epigenetics of Cardiac Repolarization for Arrhythmia Prevention. Circulation. 2017;135:683-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 55. | Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, Nishimura RA, Ommen SR, Rakowski H, Seidman CE, Towbin JA, Udelson JE, Yancy CW; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58:e212-e260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 815] [Cited by in RCA: 851] [Article Influence: 56.7] [Reference Citation Analysis (0)] |
| 56. | McNally EM, Barefield DY, Puckelwartz MJ. The genetic landscape of cardiomyopathy and its role in heart failure. Cell Metab. 2015;21:174-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 57. | Knöll R, Kostin S, Klede S, Savvatis K, Klinge L, Stehle I, Gunkel S, Kötter S, Babicz K, Sohns M, Miocic S, Didié M, Knöll G, Zimmermann WH, Thelen P, Bickeböller H, Maier LS, Schaper W, Schaper J, Kraft T, Tschöpe C, Linke WA, Chien KR. A common MLP (muscle LIM protein) variant is associated with cardiomyopathy. Circ Res. 2010;106:695-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 58. | Kraker J, Viswanathan SK, Knöll R, Sadayappan S. Recent Advances in the Molecular Genetics of Familial Hypertrophic Cardiomyopathy in South Asian Descendants. Front Physiol. 2016;7:499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 59. | Ross SB, Fraser ST, Semsarian C. Induced pluripotent stem cells in the inherited cardiomyopathies: From disease mechanisms to novel therapies. Trends Cardiovasc Med. 2016;26:663-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 60. | Lan F, Lee AS, Liang P, Sanchez-Freire V, Nguyen PK, Wang L, Han L, Yen M, Wang Y, Sun N, Abilez OJ, Hu S, Ebert AD, Navarrete EG, Simmons CS, Wheeler M, Pruitt B, Lewis R, Yamaguchi Y, Ashley EA, Bers DM, Robbins RC, Longaker MT, Wu JC. Abnormal calcium handling properties underlie familial hypertrophic cardiomyopathy pathology in patient-specific induced pluripotent stem cells. Cell Stem Cell. 2013;12:101-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 472] [Cited by in RCA: 533] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 61. | Frati P, Scopetti M, Santurro A, Gatto V, Fineschi V. Stem Cell Research and Clinical Translation: A Roadmap about Good Clinical Practice and Patient Care. Stem Cells Int. 2017;2017:5080259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 62. | Scopetti M, Santurro A, Gatto V, La Russa R, Manetti F, D'Errico S, Frati P, Fineschi V. Mesenchymal stem cells in neurodegenerative diseases: Opinion review on ethical dilemmas. World J Stem Cells. 2020;12:168-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 63. | De Marco E, Vacchiano G, Frati P, La Russa R, Santurro A, Scopetti M, Guglielmi G, Fineschi V. Evolution of post-mortem coronary imaging: from selective coronary arteriography to post-mortem CT-angiography and beyond. Radiol Med. 2018;123:351-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 64. | La Russa R, Catalano C, Di Sanzo M, Scopetti M, Gatto V, Santurro A, Viola RV, Panebianco V, Frati P, Fineschi V. Postmortem computed tomography angiography (PMCTA) and traditional autopsy in cases of sudden cardiac death due to coronary artery disease: a systematic review and meta-analysis. Radiol Med. 2019;124:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 65. | Pinchi E, Frati P, Aromatario M, Cipolloni L, Fabbri M, La Russa R, Maiese A, Neri M, Santurro A, Scopetti M, Viola RV, Turillazzi E, Fineschi V. miR-1, miR-499 and miR-208 are sensitive markers to diagnose sudden death due to early acute myocardial infarction. J Cell Mol Med. 2019;23:6005-6016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 66. | Schwendener N, Jackowski C, Persson A, Warntjes MJ, Schuster F, Riva F, Zech WD. Detection and differentiation of early acute and following age stages of myocardial infarction with quantitative post-mortem cardiac 1.5T MR. Forensic Sci Int. 2017;270:248-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 67. | Borro M, Gentile G, Cipolloni L, Foldes-Papp Z, Frati P, Santurro A, Lionetto L, Simmaco M. Personalised Healthcare: The DiMA Clinical Model. Curr Pharm Biotechnol. 2017;18:242-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 68. | Stratakis CA. Genetics and the New (Precision) Medicine and Endocrinology: In Medias Res or Ab Initio? Endocrinol Metab Clin North Am. 2017;46:xv-xvi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 69. | La Russa R, Fineschi V, Di Sanzo M, Gatto V, Santurro A, Martini G, Scopetti M, Frati P. Personalized Medicine and Adverse Drug Reactions: The Experience of An Italian Teaching Hospital. Curr Pharm Biotechnol. 2017;18:274-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 70. | Maeda H, Ishikawa T, Michiue T. Forensic molecular pathology: its impacts on routine work, education and training. Leg Med (Tokyo). 2014;16:61-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 71. | Rajamohan D, Matsa E, Kalra S, Crutchley J, Patel A, George V, Denning C. Current status of drug screening and disease modelling in human pluripotent stem cells. Bioessays. 2013;35:281-298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 72. | Fonoudi H, Ansari H, Abbasalizadeh S, Larijani MR, Kiani S, Hashemizadeh S, Zarchi AS, Bosman A, Blue GM, Pahlavan S, Perry M, Orr Y, Mayorchak Y, Vandenberg J, Talkhabi M, Winlaw DS, Harvey RP, Aghdami N, Baharvand H. A Universal and Robust Integrated Platform for the Scalable Production of Human Cardiomyocytes From Pluripotent Stem Cells. Stem Cells Transl Med. 2015;4:1482-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 73. | Geng L, Kong CW, Wong AOT, Shum AM, Chow MZY, Che H, Zhang C, Yau KL, Chan CW, Keung W, Li RA. Probing flecainide block of INa using human pluripotent stem cell-derived ventricular cardiomyocytes adapted to automated patch-clamping and 2D monolayers. Toxicol Lett. 2018;294:61-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 74. | Ruan JL, Tulloch NL, Razumova MV, Saiget M, Muskheli V, Pabon L, Reinecke H, Regnier M, Murry CE. Mechanical Stress Conditioning and Electrical Stimulation Promote Contractility and Force Maturation of Induced Pluripotent Stem Cell-Derived Human Cardiac Tissue. Circulation. 2016;134:1557-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 349] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 75. | Gao L, Gregorich ZR, Zhu W, Mattapally S, Oduk Y, Lou X, Kannappan R, Borovjagin AV, Walcott GP, Pollard AE, Fast VG, Hu X, Lloyd SG, Ge Y, Zhang J. Large Cardiac Muscle Patches Engineered From Human Induced-Pluripotent Stem Cell-Derived Cardiac Cells Improve Recovery From Myocardial Infarction in Swine. Circulation. 2018;137:1712-1730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 350] [Article Influence: 43.8] [Reference Citation Analysis (0)] |
| 76. | Ruan JL, Tulloch NL, Saiget M, Paige SL, Razumova MV, Regnier M, Tung KC, Keller G, Pabon L, Reinecke H, Murry CE. Mechanical Stress Promotes Maturation of Human Myocardium From Pluripotent Stem Cell-Derived Progenitors. Stem Cells. 2015;33:2148-2157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 99] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 77. | Yang X, Pabon L, Murry CE. Engineering adolescence: maturation of human pluripotent stem cell-derived cardiomyocytes. Circ Res. 2014;114:511-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 656] [Cited by in RCA: 756] [Article Influence: 63.0] [Reference Citation Analysis (0)] |
| 78. | Denning C, Borgdorff V, Crutchley J, Firth KS, George V, Kalra S, Kondrashov A, Hoang MD, Mosqueira D, Patel A, Prodanov L, Rajamohan D, Skarnes WC, Smith JG, Young LE. Cardiomyocytes from human pluripotent stem cells: From laboratory curiosity to industrial biomedical platform. Biochim Biophys Acta. 2016;1863:1728-1748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 185] [Cited by in RCA: 228] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 79. | Shaheen N, Shiti A, Gepstein L. Pluripotent Stem Cell-Based Platforms in Cardiac Disease Modeling and Drug Testing. Clin Pharmacol Ther. 2017;102:203-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 80. | Tan SH, Ye L. Maturation of Pluripotent Stem Cell-Derived Cardiomyocytes: a Critical Step for Drug Development and Cell Therapy. J Cardiovasc Transl Res. 2018;11:375-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 81. | Del Álamo JC, Lemons D, Serrano R, Savchenko A, Cerignoli F, Bodmer R, Mercola M. High throughput physiological screening of iPSC-derived cardiomyocytes for drug development. Biochim Biophys Acta. 2016;1863:1717-1727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 97] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 82. | Birket MJ, Mummery CL. Pluripotent stem cell derived cardiovascular progenitors--a developmental perspective. Dev Biol. 2015;400:169-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Cell and tissue engineering
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tang BP S-Editor: Fan JR L-Editor: Webster JR P-Editor: Xing YX