Published online Jan 26, 2021. doi: 10.4252/wjsc.v13.i1.30
Peer-review started: July 8, 2020
First decision: December 1, 2020
Revised: December 4, 2020
Accepted: December 11, 2020
Article in press: December 11, 2020
Published online: January 26, 2021
Processing time: 196 Days and 11.6 Hours
Adipose-derived stem cells (ADSCs) residing in the stromal vascular fraction (SVF) of white adipose tissue are recently emerging as an alternative tool for stem cell-based therapy in systemic sclerosis (SSc), a complex connective tissue disorder affecting the skin and internal organs with fibrotic and vascular lesions. Several preclinical and clinical studies have reported promising therapeutic effects of fat grafting and autologous SVF/ADSC-based local treatment for facial and hand cutaneous manifestations of SSc patients. However, currently available data indicate that ADSCs may represent a double-edged sword in SSc, as they may exhibit a pro-fibrotic and anti-adipogenic phenotype, possibly behaving as an additional pathogenic source of pro-fibrotic myofibroblasts through the adipocyte-to-myofibroblast transition process. Thus, in the perspective of a larger employ of SSc-ADSCs for further therapeutic applications, it is important to definitely unravel whether these cells present a comparable phenotype and similar immunosuppressive, anti-inflammatory, anti-fibrotic and pro-angiogenic properties in respect to healthy ADSCs. In light of the dual role that ADSCs seem to play in SSc, this review will provide a summary of the most recent insights into the preclinical and clinical studies employing SVF and ADSCs for the treatment of the disease and, at the same time, will focus on the main findings highlighting the possible involvement of these stem cells in SSc-related fibrosis pathogenesis.
Core Tip: Adipose-derived stem cells (ADSCs) represent a promising cell source for cell-based therapy in the treatment of systemic sclerosis (SSc), but at the same time, they may be involved in the disease pathogenesis. In this review, the current status of fat grafting and autologous stromal vascular fraction/ADSC-based therapeutic applications as well as SSc-ADSC functional characterization and possible implication in disease-related fibrosis are discussed.
- Citation: Rosa I, Romano E, Fioretto BS, Matucci-Cerinic M, Manetti M. Adipose-derived stem cells: Pathophysiologic implications vs therapeutic potential in systemic sclerosis. World J Stem Cells 2021; 13(1): 30-48
- URL: https://www.wjgnet.com/1948-0210/full/v13/i1/30.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v13.i1.30
Systemic sclerosis (SSc, scleroderma) is a rare multisystem disease characterized by microvascular dysfunction, abnormal immune system activation and progressive cutaneous and visceral fibrosis resulting from an increase in extracellular matrix (ECM) synthesis and deposition driven by pro-fibrotic myofibroblasts[1,2]. SSc has a chronic course and significantly affects patient’s length and quality of life, with internal organ complications being mainly responsible for the high mortality rate. Furthermore, the disease represents a real burden due to its heavy impact on facial appearance, orofacial functions and everyday life activities[3]. Indeed, if hardening of facial skin is associated with disappearance of mimic folds, thinning of lips and presence of deep wrinkles in the upper and lower face, with consequent loss of expressivity, the sclerosis of the extremities results in significant dysfunction and becomes highly disabling[4]. Since the causes of SSc remain unknown, the treatment of this disease is mostly symptomatic and based on the extent of skin and organ involvement[4]. Over the last two decades, several researchers investigated the potential of cellular therapies with autologous stem cells in the attempt to find new treatments for SSc. In this regard, multipotent mesenchymal stem cells (MSCs) seem to represent a promising therapeutic approach thanks to the number of trophic and pleiotropic properties that they exert. MSCs are a heterogeneous population of cells that have been first identified in the bone marrow (BM) and then isolated from several tissues, including umbilical cord, placenta, dental pulp and adipose tissue[5]. MSCs present a multilineage differentiation potential and are able to home to the sites of damage, where they secrete a number of soluble mediators with anti-fibrotic, anti-apoptotic, pro-angiogenic, immunomodulatory and anti-inflammatory effects[5]. In SSc, the therapeutic potential of BM-derived MSCs (BM-MSCs) has been extensively investigated in different preclinical and clinical studies, but the benefit/risk on the use of such multipotent cells has not yet been fully clarified[5-7]. Among MSCs, adipose-derived stem cells (ADSCs) residing in the so-called stromal vascular fraction (SVF), i.e., the heterogeneous cellular product obtained after adipose tissue digestion and containing several populations of stromal and immune cells, are recently emerging as an alternative tool for stem cell-based therapies[8-12]. Indeed, both the SVF and culture expanded ADSCs, which present similar characteristics to BM-MSCs but can be more easily and less invasively isolated, have the potential to be therapeutic in the field of regenerative medicine as well as in different autoimmune diseases[8-12]. As far as SSc is concerned, increasing literature is rising about the possible efficacy of autologous fat grafting for the treatment of skin fibrosis, together with the characterization of the phenotype and differentiation potential of autologous ADSCs from SSc patients[4-6,13,14]. On the other side, several studies support the idea that ADSCs might directly contribute to SSc fibrosis by reprogramming to pro-fibrotic myofibroblasts[15]. In fact, an important source of myofibroblasts is represented not only by fibroblast activation, but also by the transdifferentiation of other cell types, including pericytes, endothelial cells, epithelial cells and adipocytic precursors, including ADSCs[15]. In this regard, the recently described adipocyte-to-myofibroblast transition (AMT) process could largely explain the evidence that, in SSc, skin fibrosis is accompanied by the loss of subcutaneous adipose tissue, a phenomenon which has also been observed in different mouse models of dermal fibrosis[16-22].
In light of the dual role that ADSCs seem to play in SSc, this review will provide a summary of the most recent insights into the preclinical and clinical studies employing SVF and ADSCs for the treatment of the disease and, at the same time, will focus on the main findings highlighting the possible involvement of these stem cells in SSc pathogenesis.
The clinical hallmark of SSc is represented by connective tissue fibrosis, which predominantly affects the skin and the vessel wall and, to a lesser extent, the gastrointestinal tract, heart, lungs, and kidneys[1,2]. Whereas life-threatening internal organ lesions only occur in a minority of patients, cutaneous manifestations are almost always present and usually represent early clinical signs of the disease[23]. Loss of elasticity and sclerosis of the skin begin at acral areas, particularly at the fingers and hands, where they develop in sclerodactyly. In addition, progressive capillary rarefaction frequently occurs in the periungueal areas, generating painful digital ulcers (DUs) potentially leading to gangrene, atrophy, and eventual amputation[23]. Skin sclerosis usually affects also the face, mainly determining disappearance of mimic folds, sharpening of the nose, thinning of the lips (microcheilia), narrowness of the mouth opening (microstomia), reduction in the size of the tongue (microglossia), loss of cutaneous wrinkles and developing of vertical furrows around the lips[24,25]. Other skin manifestations are represented by changes in skin pigmentation, hair loss and loss of sebaceous glands; fibrosis of the salivary and lacrimal glands can also lead to xerostomia and xerophthalmia[26-29]. Although not life-threatening, cutaneous manifestations are very hard to conceal and, since they cause a relevant worsening of patients’ quality of life, they represent a very high disease burden. The evolution of sclerodactyly and DUs is often accompanied by intense disabling pain and great difficulty in performing daily activities, while facial involvement and oral complications cause esthetic changes, limiting expression and leading to a mask-like stiffness of the face, and difficulties with oral hygiene, speeching and eating. As a consequence, SSc cutaneous manifestations determine significant social disability, isolation and psychological distress and are considered by the majority of SSc patients as the most worrying aspects of the condition, being much more important than any other internal organ involvement[30,31]. Since to date SSc therapy is only symptomatic and focused on alleviating pain or improving organ function, the treatment of cutaneous defects or lesions represents an important challenge for healthcare professionals.
Among the novel therapeutic strategies that are currently being contemplated, the most promising seems to be the MSC-based therapy, which is actually under evaluation in the clinics. MSCs consist of a heterogeneous population of cells possessing multilineage differentiation potential, low immunogenicity, and the ability to home to the sites of damage, where they secrete various cytokines and growth factors with pro-angiogenic, anti-inflammatory and immunomodulatory properties[32]. MSCs can have multiple origins, but those derived from the BM are the first and the most extensively characterized[33]. In SSc, the therapeutic potential of BM-MSCs has been extensively investigated, but their clinical use is limited by the extremely invasive nature of BM harvest and the delay and quality management issues associated with cell culture[5]. Besides from the BM, MSCs have been isolated from several other tissues including umbilical cord, placenta, dental pulp and the adipose stromal compartment[34]. As far as ADSCs, even if they share many biological features with BM-MSCs such as multilineage differentiation potential (i.e., adipogenic, osteogenic, and chondrogenic) and expression of non-specific markers like CD105, CD73, and CD90, they present several advantages, including ease of isolation, less donor morbidity, abundance and rapidity of expansion[35]. In addition, in respect to BM-MSCs, ADSCs display higher proliferative rate, lower senescence, greater genetic stability, faster culture expandability and higher retaining of stem cell phenotypes and mesenchymal multipotency at higher passages in culture[36-38]. ADSCs also exhibit higher immunosuppressive properties[39,40] and a strong pro-angiogenic activity, primarily through the paracrine release of vascular endothelial growth factor and basic fibroblast growth factor[41,42]. Finally, the therapeutic use of ADSCs associates with fewer ethical problems and a lower immunogenicity than that of other stem cell types[43]. For all these reasons, ADSCs are currently considered one of the most attractive and promising sources of adult stem cells for cell therapy.
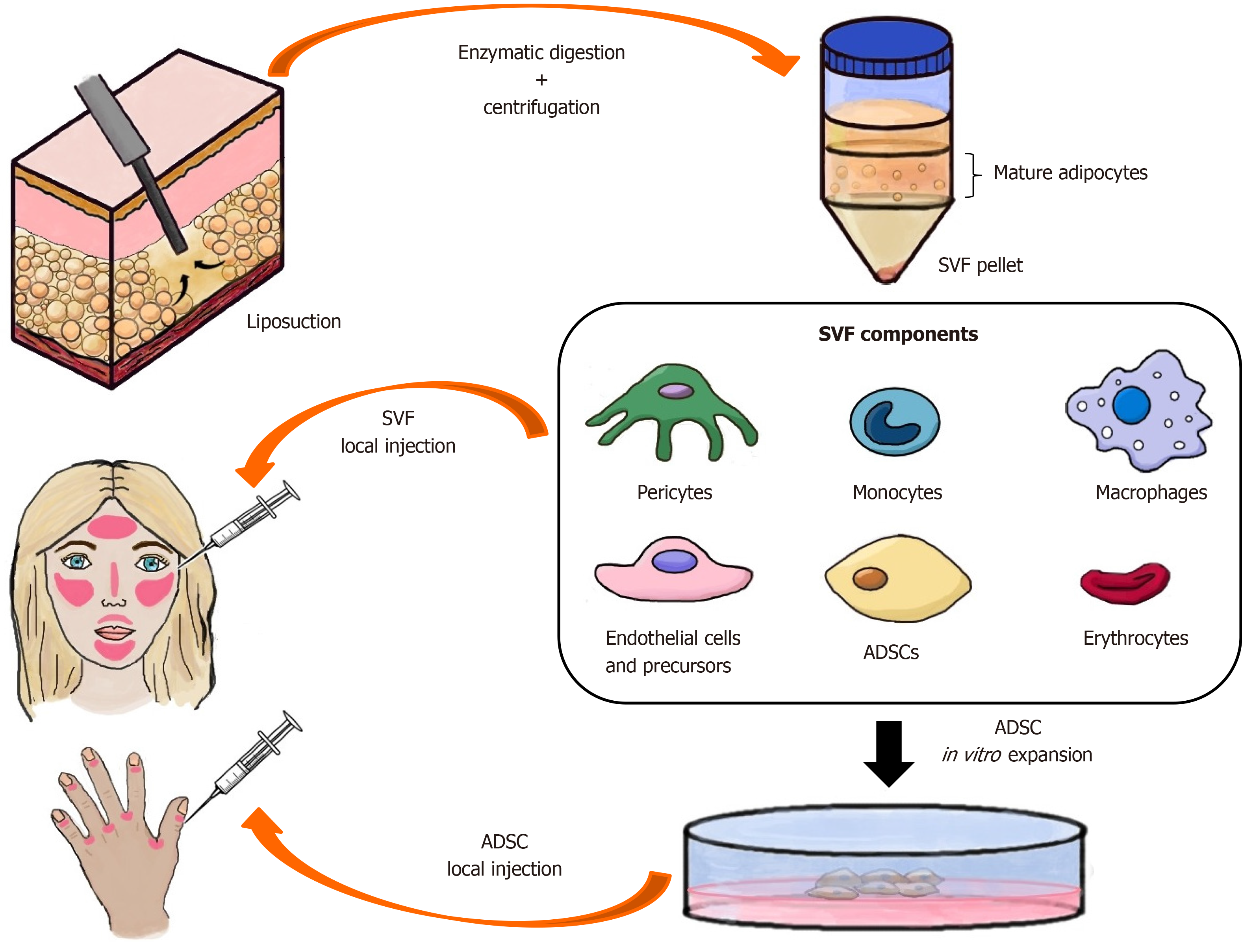
ADSCs are present in any type of white adipose tissue (WAT) (i.e., dermal, subcutaneous and omental) and, together with vascular endothelial cells, pericytes and different numbers of circulating blood-derived cells including leucocytes, macrophages and erythrocytes, constitute a heterogeneous cell population that, after isolation, is termed SVF[35,44] (Figure 1). The most widely used technique for the extraction of SVF, from which ADSCs can be subsequently isolated, is enzymatic and involves several steps: fat harvesting by liposuction, washing with phosphate-buffered saline in order to remove cellular debris, enzymatic digestion with collagenases at 37 °C to release the cell mixture embedded in the ECM between adipocytes, and centrifugation to separate the SVF (lower cellular pellet) from the floating mature adipocyte fraction (Figure 1). Erythrocytes, the major contaminants present in the SVF pellet, can be lysed in order to isolate a purer population of ADSCs[45]. Recently, Tonnard et al[46] have defined a novel method of mechanical SVF isolation called nanofat grafting technique, consisting in rapidly transferring the adipose tissue from one syringe to another in order to break down the ECM and extract the SVF.
Before their application in clinical studies, ADSC-based treatments have been proved to be beneficial in different preclinical models of SSc-like pulmonary and cutaneous fibrosis. Indeed, the administration of human ADSCs in the bleomycin-induced lung fibrosis mouse model ameliorated hyperplasia of cuboidal alveolar epithelial cells, infiltration of the alveolar ducts by inflammatory cells, septal thickening and extensive tissue fibrosis[47]. Furthermore, treatment with ADSCs led to the suppression of epithelial cell apoptosis and reduced the expression of pro-fibrotic transforming growth factor-β (TGF-β)[47]. Of note, in a study relying on the use of an established aged mouse model of bleomycin-induced lung fibrosis that was also demonstrated to present skin fibrosis, a single intravenous injection of allogeneic ADSCs was able to attenuate both pulmonary and skin fibrosis[48]. In a rat model of bleomycin-induced lung injury, intratracheal administration of autologous ADSCs at day 15 after disease induction did not improve the severity of lung injury, but prevented further aggravation of lung damage, suggesting that the time of cell injection may represent an important factor to control for better efficacy of cell therapy[49]. Another parameter that might influence the therapeutic potential of ADSCs may be the age of the stem cell donors. Indeed, in one study comparing ADSCs from aged (> 22 mo) and young (4 mo) mice, only animals receiving young ADSCs at day 21 after bleomycin instillation exhibited decreased pulmonary fibrosis, oxidative stress and markers of apoptosis compared to untreated controls[50]. In a different bleomycin-induced model of scleroderma-like skin sclerosis in nude mice, local subcutaneous injections of human aspirated fat enriched with SVF or isolated ADSCs into the lesions of bleomycin-treated mice significantly decreased the established dermal fibrosis, increased local vascularization, and improved skin texture[51,52]. Moreover, in the bleomycin-induced dermal fibrosis mouse model, subcutaneous injection of autologous ADSCs was able to significantly reduce skin thickness and the total content of hydroxyproline as a measure of collagen deposition and fibrosis[53]. In another study, intravenous administration of allogeneic ADSCs was able to attenuate skin and lung fibrosis in both bleomycin-induced skin scleroderma and sclerodermatous chronic graft-versus-host disease (Scl-cGVHD) models[54]. In addition, in mice with bleomycin-induced skin fibrosis, provision of dendritic cell-derived signals could improve survival and, therefore, effectiveness of therapeutically delivered allogeneic ADSCs[55]. The protective and reparative effects of ADSCs were finally demonstrated in the murine model of hypochlorous acid (HOCl)-induced SSc, consisting in daily intradermal injections of HOCl into Balb/c mice for 6 wk. In particular, in this preclinical SSc model, healthy murine and human ADSCs exhibited higher anti-fibrotic and anti-inflammatory effects respect to corresponding BM-MSCs, leading to a greater decrease in skin and lung fibrotic and pro-inflammatory markers[56]. Table 1 briefly recapitulates the main experimental models of SSc-like pulmonary and skin fibrosis in which therapeutic effects of fat grafting and SVF/ADSCs have been demonstrated.
| Animal model | Treatment | Results | Ref. |
| Bleomycin-induced lung fibrosis mouse model | Human ADSC administration | Amelioration of cuboidal alveolar epithelial cell hyperplasia, alveolar duct infiltration, septal thickening and tissue fibrosis. Suppression of epithelial cell apoptosis and reduction of TGF-β expression | Lee et al[47], 2014 |
| Aged mouse model of bleomycin-induced lung fibrosis | Single intravenous injection of allogeneic ADSCs | Attenuation of lung and skin fibrosis | Rubio et al[48], 2018 |
| Bleomycin-induced lung injury rat model | Intratracheal administration of autologous ADSCs | Prevention of further aggravation of lung damage at day 15 after disease induction | Uji et al[49], 2015 |
| Bleomycin-induced lung fibrosis mouse model | Administration of ADSCs from aged and young mice | Decreased pulmonary fibrosis, oxidative stress, and markers of apoptosis only in animals receiving young ADSCs at day 21 after bleomycin instillation | Tashiro et al[50], 2015 |
| Bleomycin-induced skin sclerosis model in nude mice | Local subcutaneous injections of human micro-fat enriched with SVF | Decrease in the established dermal fibrosis and increase in local vascularization | Serratrice et al[51], 2014 |
| Bleomycin-induced skin sclerosis model in nude mice | Human ADSC-assisted local subcutaneous lipotransfer | Reduced TGF-β1 and type III collagen expression | Chen et al[52], 2018 |
| Bleomycin-induced skin fibrosis mouse model | Subcutaneous injection of autologous ADSCs | Amelioration of dermal fibrosis | Chen et al[53], 2017 |
| Bleomycin-induced scleroderma and Scl-cGVHD mouse models | Intravenous administration of allogeneic ADSCs | Attenuation of skin and lung fibrosis | Okamura et al[54], 2020 |
| Bleomycin-induced skin fibrosis mouse model | Intradermal injection of allogeneic ADSCs | Provision of dendritic cell-derived signals improved survival and effectiveness of therapeutically delivered ADSCs | Chia et al[55], 2016 |
| HOCl-induced mouse model of diffuse SSc | Intravenous injection of healthy murine and human ADSCs | Decrease in skin and lung fibrotic and pro-inflammatory markers | Maria et al[56], 2016 |
Several clinical studies demonstrated the potential benefits of fat grafting and SVF/ADSC-based treatments for SSc patients and, in particular, for disease-related face and hand skin lesions[4,5,10,35,57].
Face: Although usually disregarded, facial handicap in patients with SSc is extremely important for their quality of life. Since in the last decades autologous fat grafting (also known as lipotransfer or lipofilling) has been successfully used to treat clinical conditions characterized by skin atrophy or fibrosis, the efficacy of both autologous fat grafting and isolated ADSCs for the treatment of cutaneous manifestations in the lips and perioral region of SSc patients has been intensively investigated. In one of the first case reports, the upper lip of a 41-year-old female patient with SSc was treated by fat injection in order to improve the perioral aesthetic appearance, and this allowed the patient to obtain a satisfactory recovery[58]. In the following years, autologous fat grafting was shown to ameliorate aesthetic and functional outcomes of SSc patients by improving perioral fullness, facial expression, mastication, oral hygiene and interincisal distance, with a positive effect on speech and food intake[59]. Similarly, the application of autologous fat graft in the perioral region of 20 patients with diffuse cutaneous SSc (dcSSc) significantly increased both the interincisional distance and oral perimeter and led to a consistent skin neovascularization, suggesting that lipotransfer-induced local tissue amelioration might occur via a pro-angiogenic process[60]. An additional surgical method in the treatment of SSc facial handicap was assessed by Sautereau et al[61] through autologous adipose tissue subcutaneous microinjections. Even this microsurgical technique has proved to be beneficial in the treatment of mouth opening limitation, as demonstrated by the evidence that all SSc patients showed an improvement in perioral skin sclerosis, facial pain, mouth opening and sicca syndrome[61]. Satisfying functional and aesthetic results of autologous fat grafting for the treatment of facial scleroderma were finally reported in SSc patients with microstomia and microcheilia[62,63]. In order to increase the survival rate of the autologous adipose tissue graft and to improve the cutaneous trophicity in the grafted areas, a step forward was made by enriching the autologous fat graft with platelet-rich plasma (PRP), which is able to provide nutrients and enhance ADSC proliferation through the release of several growth factors and cytokines[13]. In this regard, the combined use of autologous lipoaspirate and PRP was proved to be effective in the improvement of the buccal rhyme, skin elasticity, and vascularization of the perioral and malar areas of SSc patients[64].
As far as ADSCs are concerned, it has been investigated whether, thanks to their regenerative properties, direct injection of these multipotent stem cells could offer increased benefits compared to lipotransfer alone. Local infiltration of autologous ADSCs in combination with a hyaluronic acid solution was firstly tested in both the face and other body areas (i.e., trunk, upper and lower extremities) of a small number of patients, where it was found to considerably improve skin fibrosis[23]. In particular, treated patients manifested an arrest of local disease progression and improvements in skin manifestations, such as regression of dyschromia, better sensitivity, increase in skin softening, and erythema reduction[23]. Of note, the cohort of patients enrolled in this study consisted only in cutaneous local forms of scleroderma (i.e., generalized morphea, linear and/or plaque scleroderma)[23]. Interestingly, the same group subsequently carried out a prospective study comparing autologous fat grafting and injection of an autologous ADSC-enriched hyaluronic acid gel in two different groups of SSc patients, in order to evaluate clinical improvement of mouth opening[65]. At one-year follow-up, both procedures provided significant results but neither technique emerged as a superior option[65]. It is important to consider that all the abovementioned studies were limited by the small number of patients enrolled, few outcome measures and short follow-up. In a very recent study, the effect of autologous ADSC-enriched lipotransfer on the orofacial fibrosis outcomes was analyzed in a larger cohort of SSc patients, using multiple validated outcome measures and a longer follow-up[3]. Notably, the authors demonstrated that injection of autologous ADSC-enriched lipotransfer into the perioral and facial tissue of SSc patients significantly improved mouth function, facial volumetric appearance and psychological outcome[3]. In the same study, ADSCs were co-cultured with SSc fibroblasts and were shown to determine an attenuation of SSc fibroblast pro-fibrotic properties, thus providing a potential mechanism for the clinical benefit observed after autologous ADSC-enriched lipotransfer in SSc[3].
Hands: The regenerative, anti-inflammatory, immunomodulating, and pro-angiogenic effects of autologous fat grafting and ADSC-containing SVF have been exploited also for the treatment of SSc lesions at the fingers, including Raynaud’s phenomenon and painful and recurring DUs. In particular, management of DUs consisting mainly in pharmacologic and local therapy represents a major clinical burden in SSc, as the healing process is usually slow and ulcers can become infected or evolve to gangrene[1]. Autologous fat implantation in the hands of 13 patients with either primary or secondary Raynaud’s phenomenon associated with SSc led to significant pain relief and decrease in the number, duration, and severity of Raynaud’s phenomenon cold attacks[66]. Similarly, autologous fat grafting performed from 2 to 8 mo after ulcer onset and injected at the finger base for smaller DUs or at the border of larger DUs of SSc patients has been shown to be effective in accelerating the healing process, with 80% of DUs completely healed within 8-12 wk[67]. Moreover, the majority of the SSc patients enrolled in this study have also experienced a significant reduction in hand pain and need of pharmacological therapy as early as 2 wk post-operatively[67]. As far as ADSC-containing SVF is concerned, encouraging results on the safety, tolerability and potential efficacy of its injection to treat hand disability in SSc patients have emerged from several clinical trials and subsequent follow-up analyses. In a pilot study, regional injections of autologous SVF in 15 SSc patients with long-lasting DUs showing no tendency to improvement or healing led to good outcomes, with prompt disappearance of local ischemic pain, rapid DU healing and improvement in nailfold capillaroscopy abnormalities[68]. Of note, a subsequent randomized controlled trial performed by the same group further confirmed the abovementioned preliminary data[14]. Similar results were reported in another pilot study where injection of autologous SVF into the fingers of 12 SSc patients proved to be safe, well tolerated and beneficial in terms of pain, grasping capacity, finger edema, Raynaud’s phenomenon, DU outcome and quality of life, as recorded at the 6-month study-completion visit[59,69]. Interestingly, such documented positive effects proved to be long lasting, as they persisted 1 year after SVF injection[70,71] and were still very encouraging even at 22 and 30 mo after treatment[72]. Finally, the beneficial effects of autologous SVF subcutaneous injection were also demonstrated in a case report of a 62-year-old woman affected by SSc who presented progressive digital necrosis, ulceration, gangrene, impaired wound healing and was not responsive to conventional therapy with vasodilator drugs[73].
The main clinical studies reporting the beneficial effects of fat grafting and SVF/ADSC-based treatment in SSc are summarized in Tables 2 and 3.
| No. of patients | Follow-up period | Results (face) | Ref. |
| 1 | - | Autologous fat grafting improved perioral aesthetic appearance and mouth opening | Ho-Asjoe et al[58], 1996 |
| 20 | 3 mo | Autologous fat grafting increased interincisal distance, oral perimeter and induced skin neovascularization | Del Papa et al[60], 2015 |
| 14 | 6 mo | Autologous fat grafting improved perioral skin sclerosis, facial pain, mouth opening and sicca syndrome | Sautereau et al[61], 2016 |
| 7 | 12 mo | Autologous fat grafting improved SSc-related microstomia and microcheilia | Blezien et al[62], 2017 |
| 16 | 3 mo | Autologous fat transfer significantly improved mouth opening capacity | Gheisari et al[63], 2018 |
| 1 | - | Autologous fat grafting enriched with PRP improved skin trophicity | Daumas et al[13], 2020 |
| 6 | 3 mo | The combined use of autologous lipoaspirate and PRP improved buccal rhyme, skin elasticity, and vascularization of the perioral and malar areas | Virzì et al[64], 2017 |
| 6 | 12 mo | Local injection of autologous ADSCs in combination with a hyaluronic acid solution led to arrest of local disease progression, regression of dyschromia, better sensitivity, increase in skin softening and erythema reduction | Scuderi et al[23], 2013 |
| 10 | 12 mo | Both autologous fat grafting and ADSC-enriched hyaluronic acid gel improved mouth opening and interincisal distance | Onesti et al[65], 2016 |
| 62 | 6-53 mo | Autologous ADSC-enriched lipotransfer significantly improved mouth function, facial volumetric appearance and psychological outcome | Almadori et al[3], 2019 |
| No. of patients | Follow-up period | Results (hands) | Ref. |
| 13 | 9.4 to 24.3 mo | Autologous fat implantation led to significant pain relief and decrease in the number, duration, and severity of Raynaud’s phenomenon cold attacks | Bank et al[66], 2014 |
| 9 | 12 wk | Autologous fat grafting was effective in accelerating the healing process of DUs and led to a significant reduction in hand pain and need of pharmacological therapy | Bene et al[67], 2014 |
| 15 | 6 mo | Autologous SVF injections led to prompt disappearance of local ischemic pain, rapid DU healing and improvement in nailfold capillaroscopy abnormalities | Del Papa et al[68], 2015 |
| 38 | 8 wk | Autologous fat grafting induced DU healing, restoration of the capillary bed and a rapid resolution of local ischemic pain | Del Papa et al[14], 2019 |
| 12 | 6 mo | Injection of autologous SVF proved to be safe, well tolerated and beneficial in terms of pain, grasping capacity, finger edema, Raynaud’s phenomenon, DU outcome and quality of life | Granel et al[69], 2015 |
| 12 | 12 mo | The effects recorded by Granel et al[69] proved to be long lasting, as they persisted 1 yr after SVF injection | Guillaume-Jugnot et al[70], 2016 |
| 12 | 22-30 mo | The effects recorded by Granel et al[69] were still very encouraging even at 22 and 30 mo after treatment | Daumas et al[72], 2017 |
| 1 | - | Autologous SVF subcutaneous injections had beneficial effects on digital necrosis, ulceration, gangrene and impaired wound healing | Song et al[73], 2017 |
Collectively, these clinical studies demonstrate the efficacy and safety of all types of autologous fat grafting procedures in the treatment of SSc-related skin fibrotic and vasculopathic lesions, regardless of the type of fat preparation and/or purification. However, an important question that should be addressed is whether ADSCs isolated from SSc patients are able to maintain their ability to exert beneficial immunosu-ppressive, anti-inflammatory, anti-fibrotic and pro-angiogenic activities. In this regard, conflicting results are currently available. Indeed, while some authors did not notice any significant differences in proliferative capacities and pro-angiogenic and anti-fibrotic properties between ADSCs from SSc patients and healthy donors[23,74,75], other studies reported opposite results[7,64,76-79]. In particular, adipose-derived SVF from SSc patients was shown to display an altered cell composition (i.e., reduced number of cells with a stem-like phenotype, high content of pro-inflammatory cytokines and a shortage of angiogenic factors) and SVF-derived ADSCs, though retaining high multipotency, failed in differentiating into fully mature adipocytes, osteocytes and chondrocytes[64]. In another study, when compared to healthy ADSCs, ADSCs isolated from SSc patients were found to display reduced proliferative rate, metabolic activity and migration capacity, even if showing similar surface phenotype, differentiation potential and pro-angiogenic effects[76]. In addition, a differential cellular and molecular signature reflecting a deregulation of angiogenesis, endothelial activation and fibrosis was detected in SSc SVF when compared with healthy SVF[77]. Moreover, it was recently reported that both ADSCs isolated from the abdominal fat of SSc patients and ADSCs harvested from bleomycin-treated mice present a pro-fibrotic and anti-adipogenic phenotype characterized by high levels of the myofibroblast marker α-smooth muscle actin (α-SMA) and low expression of both anti-fibrotic caveolin-1 and the adipogenic marker fatty acid binding protein 4 (FABP4)[78]. Through a comparative analysis of microRNA (miRNA) profiles, it was also demonstrated that both BM-MSCs and ADSCs of SSc patients display an upregulation of pathways promoting their senescence and pro-fibrotic phenotype with a parallel downregulation of the miRNAs controlling cell survival-related genes[7]. Finally, in an attempt to clarify the controversy over the use of autologous or allogeneic ADSCs in the clinic, a very recent study has compared the phenotype and secretory potential of ADSCs from different rheumatic diseases, including SSc, with the corresponding features of ADSCs originating from healthy donors[79]. From this comparison, it has emerged that ADSCs isolated from SSc patients are characterized by several abnormalities in the expression of cell surface markers that may modify their biological activities and contribute to inadequate immunoregulatory functions[79].
SSc-related fibrosis is characterized by tissue stiffening and impaired function due to an excessive deposition of ECM proteins and is driven by activated myofibroblasts, a population of mesenchymal cells displaying increased production of fibrillar type I and type III collagens, expression and incorporation into stress fibers of α-SMA and shortage of ECM-degrading enzymes[15,80]. The initial events leading to the appearance of activated myofibroblasts still remain a matter of debate, as these pro-fibrotic cells can originate from several sources including resident fibroblasts, pericytes, epithelial and endothelial cells[15,80,81]. Increasing evidence also suggests that WAT and related adipocytes may be involved in the development of SSc fibrosis[82]. As previously discussed, WAT is composed of mature adipocytes with the ability to store energy and secrete adipokines, and SVF comprising ADSCs with regenerative and reparative capacity. Two types of WAT can be distinguished at the skin level: the subcutaneous WAT (sWAT, also called hypoderma) located beneath the skin, and the dermal WAT (dWAT) located directly under the reticular dermis[83]. In rodents, dWAT can be easily recognized as a discrete layer of fat cells situated between the dermis and the panniculus carnosus muscle, whereas in humans, who lack panniculus carnosus, it is located around the pilosebaceous units in the so-called dermal cones, which are characterized by a portion situated in the dermis and another one passing through the dermis and infiltrating into the sWAT[84]. dWAT has an independent developmental origin from sWAT, and during embryogenesis shares common precursors with dermal fibroblasts[85].
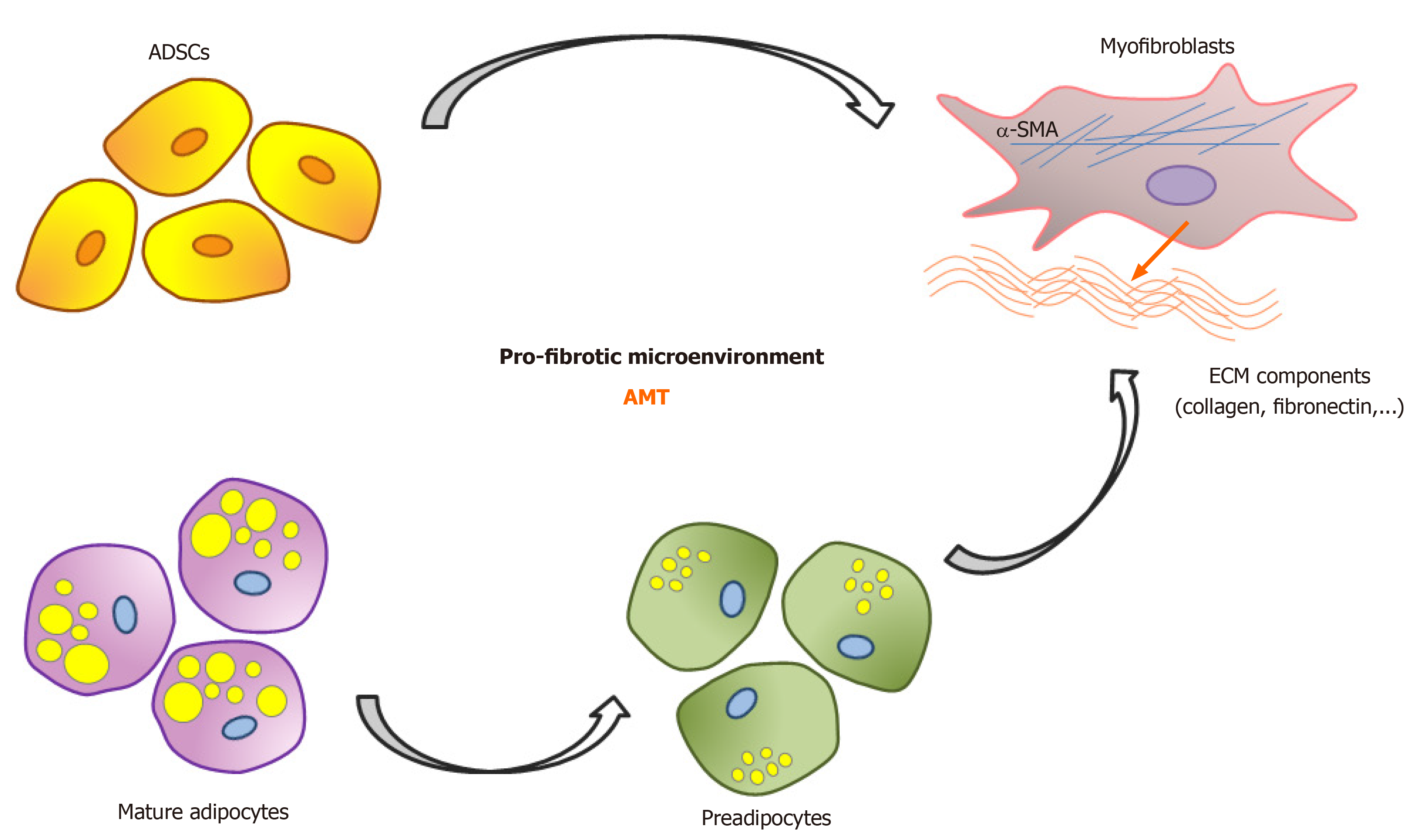
The hypothesis of a possible involvement of WAT in SSc-related fibrosis was firstly raised in the seventies from the observations of the dermatologist Raul Fleischmajer who, after describing WAT atrophy and its replacement by collagen-rich fibrotic tissue as consistent features of SSc, speculated that fat loss could represent a key pathogenic event of the disease[86,87]. During the years, atrophy of WAT accompanying skin fibrosis has also been highlighted in various animal models of SSc, including the experimental models of cutaneous fibrosis induced by bleomycin[88,89], HOCl[90], angiotensin II[18], overexpression of constitutively active TGF-β receptor type I (TGF-βRI)[91], and in murine Scl-cGVHD[92,93]. Mice with heritable cutaneous fibrosis, including Fra-2 transgenic[20], fibrillin-1–mutant[21], tight skin 1[94], and tight skin 2 mice[95], also display a comparable atrophy of WAT. A similar phenotype has been observed in the urokinase type plasminogen activator receptor (uPAR)-deficient mouse as well. Indeed, uPAR deficiency attenuated adipocyte differentiation[96], and uPAR-/- mice presented significant dermal fibrosis accompanied by a parallel reduction of WAT[19]. Interestingly, several therapeutic strategies known to ameliorate experimental fibrosis, such as treatment with TGF-β neutralizing antibodies or the peroxisome proliferator-activated receptor-γ (PPAR-γ) agonist rosiglitazone, were found to promote adipogenesis[97,98]. Of note, time-course studies performed both in transgenic mice with adipocyte-specific expression of Wnt-10b, a well-known fibrogenic regulator, and in the bleomycin-induced skin fibrosis mouse model established that the loss of dermal adipocytes precedes the onset of myofibroblast accumulation and consequent dermal thickening[22,55]. Similarly, by using an adipocyte-specific genetic lineage tracing analysis, Marangoni and colleagues observed that bleomycin-induced fibrosis in mice caused WAT involution preceding the onset of dermal fibrosis, with adiponectin-expressing progenitor cells, normally confined to the intradermal adipose tissue compartment, downregulating their adipocytic markers, migrating into the dermis and acquiring the expression of α-SMA[99]. By performing additional ex vivo studies, the same authors reported that whereas healthy ADSCs cultivated for 10 d in adipocytic differentiation medium acquired a rounded shape, with accumulation of intracytoplasmic lipid droplets and immunopositivity for both adiponectin and perilipin, the subsequent application of TGF-β determined a rapid modulation of their cell morphology[99]. In particular, after 24 h these cells were in a transition state and expressed both perilipin and α-SMA, while later they lost their adipogenic markers and increased α-SMA expression, acquiring the typical features of contractile myofibroblasts[99]. Besides ADSCs committed toward adipocytes, other studies reported that a pro-fibrotic myofibroblastic phenotype can be induced by treatment with TGF-β also in cultured undifferentiated ADSCs[78,100]. Noteworthy, it appears that an additional source of pro-fibrotic myofibroblasts may be represented even by mature adipocytes[101]. This may happen through a two-step process during which mature adipocytes de-differentiate into the so-called adipose-derived preadipocytes that then transdifferentiate into myofibroblasts[101] (Figure 2). Collectively, these findings strongly support the notion that WAT loss accompanying SSc dermal fibrosis can not be explained only by adipocyte apoptosis, but also by a direct AMT process of both mature adipocytes and ADSCs (Figure 2). Besides reflecting a pathophysiologic process, WAT involution may therefore also play a pivotal pathogenic role in SSc skin fibrosis. Additional in vitro experiments further demonstrated that the AMT process can be driven not only by TGF-β[78,99], but also by treatment with sera from patients with early dcSSc[100] and by other molecules/signaling pathways such as found in inflammatory zone 1 (FIZZ1)[102] and Wnt/β-catenin[22], suggesting that the SSc pathologic microenvironment might be relevant in determining an unwanted pro-fibrotic fate of mature adipocytes and ADSCs[103]. In particular, FIZZ1, whose levels have been found to be increased in SSc sera[102], has been reported to suppress adipogenesis and stimulate myofibroblast differentiation in 3T3-L1 preadipocytes via Notch1 signaling[102]. In addition, mice lacking FIZZ1 retained more adipose tissue and developed less fibrosis in response to bleomycin skin injury[102]. As far as Wnt/β-catenin signaling is concerned, Wnt-3a was shown to inhibit adipogenesis in healthy human subcutaneous preadipocytes by repressing the adipogenic master regulator PPAR-γ and promoting the differentiation of these cells into myofibroblasts[104]. Of note, PPAR-γ is considered the principal mediator of adipogenic differentiation and its loss is known to be associated with the transdifferentiation of quiescent ADSCs into activated myofibroblasts[105-107]. The involvement of Wnt/β-catenin signaling in WAT involution and its parallel replacement by fibrotic tissue was further demonstrated in transgenic mice with FABP4-directed Wnt10b expression[22]. Moreover, topical application of C-82, a therapeutic that inhibits canonical Wnt signaling by blocking the interaction of the cyclic AMP response element-binding protein with β-catenin and suppressing Wnt-activated genes, was shown to rescue cutaneous adipogenesis in patients with SSc[108]. It has been recently demonstrated that pro-fibrotic TGF-β induces the activity of cyclin-dependent kinase 5 (CDK5) and the expression of the CDK5R1 subunit p35, which is essential for CDK5 function[109]. In this regard, markedly elevated levels of p35 have been detected in the fibrotic skin of both SSc patients and experimental scleroderma[109]. Moreover, ectopic expression of p35 in 3T3-L1 preadipocytes was found to suppress adipogenic markers and stimulate myofibroblast markers with consequent collagen production, whereas pharmacological inhibition of CDK5 in experimental bleomycin-induced skin fibrosis prevented and reversed dermal fibrosis[109]. In another study, transgenic mice with platelet-derived growth factor receptor α+/stem cell antigen 1 (Sca1)+ progenitor cells (i.e., lower dermis reticular fibroblasts with a preadipocyte signature) constitutively expressing active β-catenin were shown to be characterized by attrition of dWAT paralleled by an increase in dermal fibrosis[110]. Further insights into the fate of ADSCs in skin fibrosis have come from another study in which the investigators reported a significant decrease in the dermal murine population of Sca1+ ADSCs and a parallel increase in dermal thickness and accumulation of Sca1+ myofibroblasts[55]. Survival of the remaining Sca1+ ADSCs in fibrotic skin was maintained by CD11b+ dendritic cells via lymphotoxin-β and downstream integrin activation. Moreover, when mice with skin fibrosis were intradermally injected with ADSCs in combination with stimulation of lymphotoxin-β receptor, the injected ADSCs showed enhanced engraftment and survival, and both dWAT loss and dermal fibrosis were ameliorated[55]. Besides cutaneous fibrosis, lineage-tracing approaches in bleomycin-induced lung fibrosis revealed that lipofibroblasts (i.e., lipid droplet-containing interstitial fibroblasts resembling adipocytes) are able to transdifferentiate into myofibroblasts[111]. Interestingly, during fibrosis resolution, myofibroblasts transitioned to a lipofibroblast-like phenotype[111], a phenomenon that has also been observed in mouse skin[112].
Finally, it has been recently hypothesized that the local ratio of adipocyte progenitors/ADSCs to mature adipocytes in WAT might be of particular importance in the pathogenesis of SSc skin fibrosis[113]. In fact, these cells have been proposed to give rise to different types of fibroblast-like cells, with adipocyte progenitors/ADSCs being mainly involved in the production of active synthetic myofibroblasts, while mature adipocytes being mostly inclined to transform into less active synthetically fibroblast-like cells[113].
An additional contribution of WAT to SSc pathogenesis could derive from a dysregulated production of adipocyte-released adipokines[114-116]. Among them, serum levels of adiponectin, an adipokine directly regulated by PPAR-γ, were found to be significantly decreased in SSc patients at the early stages (< 18 mo from the first non-Raynaud manifestation), when progression of skin fibrosis is thought to be the most active, in comparison with patients with later stage disease (> 36 mo)[117]. Moreover, a significant inverse correlation between adiponectin levels and the modified Rodnan skin score (mRSS) was observed, suggesting that circulating adiponectin levels may represent a possible biomarker of fibrogenic activity[117]. Adiponectin seems also to exert anti-fibrotic effects, as mice lacking adiponectin develop exaggerated dermal fibrosis upon bleomycin treatment, while transgenic mice with constitutively elevated adiponectin show selective dWAT expansion and protection from skin fibrosis[118,119]. The anti-fibrotic properties of this adipokine was further confirmed in a murine model of SSc, where an orally-active adiponectin receptor agonist was able to mitigate dermal fibrosis, inflammation and microvascular damage[120]. Leptin is another adipokine that seems to be involved in SSc pathogenesis. Indeed, it has been found to be significantly decreased in the sera of patients with the active phase of SSc[121]. Since this adipokine polarizes T lymphocytes into Th1 and suppresses Th2 phenotype, its reduction in the circulation may contribute to the observed Th2 lymphocyte domination at the early, active stages of the disease[121]. Visfatin is an adipokine predominantly secreted by visceral adipose tissue whose serum levels were found significantly elevated in late-stage dcSSc (disease duration > 6 years), a disease phase generally characterized by the spontaneous resolution of skin sclerosis, compared with healthy controls[122]. Moreover, in vitro experiments showed that visfatin was able to reverse the pro-fibrotic phenotype of SSc dermal fibroblasts, suggesting a direct anti-fibrotic effect of this adipokine[122]. Vaspin is another adipokine predominantly expressed in visceral adipose tissue whose circulating levels were found significantly decreased in SSc patients with DUs compared with those without, suggesting a protective role of this adipokine to DU development[123]. As far as adipsin is concerned, since elevated serum levels of this adipokine were correlated with pulmonary arterial hypertension (PAH) in SSc patients, it has been proposed as a potential biomarker of this disease-related complication[124]. Apelin is an endogenous ligand of the G protein-coupled receptor APJ that is widely expressed in the central nervous system and in many peripheral tissues, including WAT[125]. The apelin/APJ complex was shown to alleviate renal, myocardial and lung fibrosis in different diseases[126], and to inhibit TGF-β-induced skin fibrosis in SSc[125]. Moreover, apelin expression was significantly reduced in SSc fibroblasts compared to normal fibroblasts, and serum apelin levels negatively correlated with mRSS in SSc patients[125]. However, since the differences in serum apelin levels between SSc patients and healthy controls vary among studies[125,127], further analyses are necessary to establish its role in SSc pathogenesis. The possible contribution of omentin, which is abundantly produced by visceral adipose tissue, to SSc pathogenesis and clinical outcome has been so far investigated only by one study[128]. Although omentin serum concentration was comparable between SSc patients and healthy controls, its levels were decreased in dcSSc patients compared to limited cutaneous SSc patients. Additionally, omentin levels in dcSSc patients positively correlated with disease duration. Furthermore, increased right ventricular systolic pressure was observed in SSc patients with elevated omentin concentration, suggesting a possible role of this adipokine as a biomarker of vascular involvement leading to SSc-related PAH[128].
Collectively, all the aforementioned studies suggest that in SSc WAT and the adipocytic cell lineage not only may make an important contribution to the development of tissue fibrosis, but likely also participate to other aspects of this complex disease, including SSc-related vasculopathy.
A number of preclinical and relatively small clinical studies have investigated the efficacy and safety of fat grafting and adipose-derived SVF/ADSC-based treatments in SSc, generally reporting promising therapeutic effects regardless of the type of fat and fat-derived cell preparation and/or purification. In particular, the use of SVF-isolated and culture expanded ADSCs is increasingly gaining attention due to the extremely high potential of these mesenchymal stem cells. Indeed, when compared to BM-MSCs, ADSCs present a variety of advantages, including ease and non-invasiveness of collection, as well as higher differentiation ability and regenerative properties. Nevertheless, in the perspective of a larger employ of SSc-derived ADSCs for further therapeutic applications, it is important to definitely unravel whether these cells present a comparable phenotype and similar immunosuppressive, anti-inflammatory, anti-fibrotic and pro-angiogenic properties in respect to healthy ADSCs. In this regard, although some authors reported no significant differences between ADSCs from SSc patients and healthy donors[23,74,75], others found that this kind of progenitor cells isolated from SSc adipose-derived SVF are characterized by reduced proliferative rates, metabolic activities, migration capacities and differentiation potential[7,64,76-79]. Most importantly, SSc-ADSCs have also been shown to present a pro-fibrotic and anti-adipogenic phenotype[7,78], suggesting that these cells may behave as an additional pathogenic source of pro-fibrotic myofibroblasts through the recently described AMT transdifferentiation process. Furthermore, there is also experimental evidence supporting the notion that the disease microenvironment may substantially affect the fate of ADSCs by directing their pathologic activation[100,103]. Collectively, the currently available data indicate that ADSCs may represent a double-edged sword in SSc, since they have shown beneficial therapeutic effects when used for topical applications in clinical practice but, at the same time, they seem to be potentially involved in tissue fibrosis and disease progression. Therefore, the possibility that ADSCs may behave as a source of pro-fibrotic myofibroblasts should not be overlooked when planning SVF-based therapeutic approaches to treat SSc patients. Clearly, only an in-depth cellular and molecular characterization of adipose-derived SVF and in vitro-expanded ADSCs in larger cohorts of SSc patients, including different disease subsets reflecting the remarkable disease heterogeneity, might help in identifying and predicting which patients will be more likely to benefit from an autologous therapeutic approach. From a clinical point of view, besides the need to standardize the optimal dosage, time and technique of administration of such multipotent stem cells, it is important to consider that up to now ADSC-based therapeutic application in SSc has been shown to be effective only for the local treatment of facial and hand cutaneous manifestations, while very little is known about their possible efficacy at the systemic level. Finally, a deeper understanding of the putative role of the adipocytic cell lineage in the development of SSc-related tissue fibrosis may pave the way for the discovery of novel therapeutic targets to prevent or reverse fibrosis by reducing disease progression, including pharmacological enhancement of adipogenesis and other strategies to disrupt the differentiation of ADSCs into pro-fibrotic myofibroblasts.
| 1. | Varga J, Trojanowska M and Kuwana M. Pathogenesis of systemic sclerosis: recent insights of molecular and cellular mechanisms and therapeutic opportunities. J Scleroderma Relat Disord. 2017;2:137-152. [RCA] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 259] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 2. | Denton CP, Khanna D. Systemic sclerosis. Lancet. 2017;390:1685-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1065] [Cited by in RCA: 1628] [Article Influence: 180.9] [Reference Citation Analysis (0)] |
| 3. | Almadori A, Griffin M, Ryan CM, Hunt DF, Hansen E, Kumar R, Abraham DJ, Denton CP, Butler PEM. Stem cell enriched lipotransfer reverses the effects of fibrosis in systemic sclerosis. PLoS One. 2019;14:e0218068. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Strong AL, Rubin JP, Kozlow JH, Cederna PS. Fat Grafting for the Treatment of Scleroderma. Plast Reconstr Surg. 2019;144:1498-1507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 5. | Rozier P, Maria A, Goulabchand R, Jorgensen C, Guilpain P, Noël D. Mesenchymal Stem Cells in Systemic Sclerosis: Allogenic or Autologous Approaches for Therapeutic Use? Front Immunol. 2018;9:2938. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Peltzer J, Aletti M, Frescaline N, Busson E, Lataillade JJ, Martinaud C. Mesenchymal Stromal Cells Based Therapy in Systemic Sclerosis: Rational and Challenges. Front Immunol. 2018;9:2013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 7. | Di Benedetto P, Panzera N, Cipriani P, Mastroiaco V, Tessitore A, Liakouli V, Ruscitti P, Berardicurti O, Carubbi F, Guggino G, Bianchi A, Di Marco A, Ciccia F, Alesse E, Giacomelli R. Mesenchymal stem cells of Systemic Sclerosis patients, derived from different sources, show a profibrotic microRNA profiling. Sci Rep. 2019;9:7144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Sabol RA, Bowles AC, Côté A, Wise R, Pashos N, Bunnell BA. Therapeutic Potential of Adipose Stem Cells. Adv Exp Med Biol. 2018;Online ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Gimble JM, Katz AJ, Bunnell BA. Adipose-derived stem cells for regenerative medicine. Circ Res. 2007;100:1249-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1660] [Cited by in RCA: 1941] [Article Influence: 102.2] [Reference Citation Analysis (0)] |
| 10. | Maria AT, Maumus M, Le Quellec A, Jorgensen C, Noël D, Guilpain P. Adipose-Derived Mesenchymal Stem Cells in Autoimmune Disorders: State of the Art and Perspectives for Systemic Sclerosis. Clin Rev Allergy Immunol. 2017;52:234-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 98] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 11. | Torres-Torrillas M, Rubio M, Damia E, Cuervo B, Del Romero A, Peláez P, Chicharro D, Miguel L, Sopena JJ. Adipose-Derived Mesenchymal Stem Cells: A Promising Tool in the Treatment of Musculoskeletal Diseases. Int J Mol Sci. 2019;20:3105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 12. | Shukla L, Yuan Y, Shayan R, Greening DW, Karnezis T. Fat Therapeutics: The Clinical Capacity of Adipose-Derived Stem Cells and Exosomes for Human Disease and Tissue Regeneration. Front Pharmacol. 2020;11:158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 137] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 13. | Daumas A, Magalon J, Delaunay F, Abellan M, Philandrianos C, Sabatier F, Granel B, Magalon G. Fat Grafting for Treatment of Facial Scleroderma. Clin Plast Surg. 2020;47:155-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Del Papa N, Di Luca G, Andracco R, Zaccara E, Maglione W, Pignataro F, Minniti A, Vitali C. Regional grafting of autologous adipose tissue is effective in inducing prompt healing of indolent digital ulcers in patients with systemic sclerosis: results of a monocentric randomized controlled study. Arthritis Res Ther. 2019;21:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 15. | Rosa I, Romano E, Fioretto BS, Manetti M. The contribution of mesenchymal transitions to the pathogenesis of systemic sclerosis. Eur J Rheumatol. 2020;7:S157-S164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 16. | Beyer C, Schett G, Distler O, Distler JH. Animal models of systemic sclerosis: prospects and limitations. Arthritis Rheum. 2010;62:2831-2844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 124] [Article Influence: 7.8] [Reference Citation Analysis (1)] |
| 17. | Marangoni RG, Varga J, Tourtellotte WG. Animal models of scleroderma: recent progress. Curr Opin Rheumatol. 2016;28:561-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Stawski L, Han R, Bujor AM, Trojanowska M. Angiotensin II induces skin fibrosis: a novel mouse model of dermal fibrosis. Arthritis Res Ther. 2012;14:R194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 19. | Manetti M, Rosa I, Milia AF, Guiducci S, Carmeliet P, Ibba-Manneschi L, Matucci-Cerinic M. Inactivation of urokinase-type plasminogen activator receptor (uPAR) gene induces dermal and pulmonary fibrosis and peripheral microvasculopathy in mice: a new model of experimental scleroderma? Ann Rheum Dis. 2014;73:1700-1709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 20. | Maurer B, Distler JH, Distler O. The Fra-2 transgenic mouse model of systemic sclerosis. Vascul Pharmacol. 2013;58:194-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 21. | Gerber EE, Gallo EM, Fontana SC, Davis EC, Wigley FM, Huso DL, Dietz HC. Integrin-modulating therapy prevents fibrosis and autoimmunity in mouse models of scleroderma. Nature. 2013;503:126-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 154] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 22. | Wei J, Melichian D, Komura K, Hinchcliff M, Lam AP, Lafyatis R, Gottardi CJ, MacDougald OA, Varga J. Canonical Wnt signaling induces skin fibrosis and subcutaneous lipoatrophy: a novel mouse model for scleroderma? Arthritis Rheum. 2011;63:1707-1717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 169] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 23. | Scuderi N, Ceccarelli S, Onesti MG, Fioramonti P, Guidi C, Romano F, Frati L, Angeloni A, Marchese C. Human adipose-derived stromal cells for cell-based therapies in the treatment of systemic sclerosis. Cell Transplant. 2013;22:779-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 24. | Bajraktari IH, Kryeziu A, Sherifi F, Bajraktari H, Lahu A, Bajraktari G. Oral manifestations of Systemic Sclerosis and Correlation with anti-Topoisomerase I Antibodies (SCL-70). Med Arch. 2015;69:153-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Crincoli V, Fatone L, Fanelli M, Rotolo RP, Chialà A, Favia G, Lapadula G. Orofacial Manifestations and Temporomandibular Disorders of Systemic Scleroderma: An Observational Study. Int J Mol Sci. 2016;17:1189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 26. | Vincent C, Agard C, Barbarot S, N'Guyen JM, Planchon B, Durant C, Pistorius MA, Dreno B, Ponge T, Stalder JF, Mercier JM, Hamidou M. [Orofacial manifestations of systemic sclerosis: a study of 30 consecutive patients]. Rev Med Interne. 2009;30:5-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Albilia JB, Lam DK, Blanas N, Clokie CM, Sándor GK. Small mouths ... Big problems? J Can Dent Assoc. 2007;73:831-836. [PubMed] |
| 28. | Salem B, Rim BH, Sihem BK, Maher B. [Oral manifestations of systemic sclerosis]. Pan Afr Med J. 2013;16:114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Panchbhai A, Pawar S, Barad A, Kazi Z. Review of orofacial considerations of systemic sclerosis or scleroderma with report of analysis of 3 cases. Indian J Dent. 2016;7:134-139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Thombs BD, Jewett LR, Kwakkenbos L, Hudson M, Baron M; Canadian Scleroderma Research Group. Major depression diagnoses among patients with systemic sclerosis: baseline and one-month followup. Arthritis Care Res (Hoboken). 2015;67:411-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Kwakkenbos L, Delisle VC, Fox RS, Gholizadeh S, Jewett LR, Levis B, Milette K, Mills SD, Malcarne VL, Thombs BD. Psychosocial Aspects of Scleroderma. Rheum Dis Clin North Am. 2015;41:519-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 32. | Caplan AI. Adult Mesenchymal Stem Cells: When, Where, and How. Stem Cells Int. 2015;2015:628767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 148] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 33. | Ohishi M, Schipani E. Bone marrow mesenchymal stem cells. J Cell Biochem. 2010;109:277-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 34. | da Silva Meirelles L, Chagastelles PC, Nardi NB. Mesenchymal stem cells reside in virtually all post-natal organs and tissues. J Cell Sci. 2006;119:2204-2213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1715] [Cited by in RCA: 1721] [Article Influence: 86.1] [Reference Citation Analysis (0)] |
| 35. | Del Papa N, Zaccara E, Di Luca G, Andracco R, Maglione W, Vitali C. Adipose-derived cell transplantation in systemic sclerosis: state of the art and future perspectives. J Scleroderma Relat Disord. 2017;2:33-41. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 36. | Uzbas F, May ID, Parisi AM, Thompson SK, Kaya A, Perkins AD, Memili E. Molecular physiognomies and applications of adipose-derived stem cells. Stem Cell Rev Rep. 2015;11:298-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 37. | Kern S, Eichler H, Stoeve J, Klüter H, Bieback K. Comparative analysis of mesenchymal stem cells from bone marrow, umbilical cord blood, or adipose tissue. Stem Cells. 2006;24:1294-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2248] [Cited by in RCA: 2386] [Article Influence: 119.3] [Reference Citation Analysis (1)] |
| 38. | Neri S, Bourin P, Peyrafitte JA, Cattini L, Facchini A, Mariani E. Human adipose stromal cells (ASC) for the regeneration of injured cartilage display genetic stability after in vitro culture expansion. PLoS One. 2013;8:e77895. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 39. | Puissant B, Barreau C, Bourin P, Clavel C, Corre J, Bousquet C, Taureau C, Cousin B, Abbal M, Laharrague P, Penicaud L, Casteilla L, Blancher A. Immunomodulatory effect of human adipose tissue-derived adult stem cells: comparison with bone marrow mesenchymal stem cells. Br J Haematol. 2005;129:118-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 685] [Cited by in RCA: 696] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 40. | Yañez R, Lamana ML, García-Castro J, Colmenero I, Ramírez M, Bueren JA. Adipose tissue-derived mesenchymal stem cells have in vivo immunosuppressive properties applicable for the control of the graft-versus-host disease. Stem Cells. 2006;24:2582-2591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 518] [Cited by in RCA: 525] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 41. | Minteer DM, Marra KG, Rubin JP. Adipose stem cells: biology, safety, regulation, and regenerative potential. Clin Plast Surg. 2015;42:169-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 42. | Sterodimas A, de Faria J, Nicaretta B, Pitanguy I. Tissue engineering with adipose-derived stem cells (ADSCs): current and future applications. J Plast Reconstr Aesthet Surg. 2010;63:1886-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 190] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 43. | Strioga M, Viswanathan S, Darinskas A, Slaby O, Michalek J. Same or not the same? Stem Cells Dev. 2012;21:2724-2752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 540] [Cited by in RCA: 612] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 44. | Bourin P, Bunnell BA, Casteilla L, Dominici M, Katz AJ, March KL, Redl H, Rubin JP, Yoshimura K, Gimble JM. Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: a joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy. 2013;15:641-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1199] [Cited by in RCA: 1406] [Article Influence: 108.2] [Reference Citation Analysis (10)] |
| 45. | Bora P, Majumdar AS. Adipose tissue-derived stromal vascular fraction in regenerative medicine: a brief review on biology and translation. Stem Cell Res Ther. 2017;8:145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 224] [Cited by in RCA: 367] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 46. | Tonnard P, Verpaele A, Peeters G, Hamdi M, Cornelissen M, Declercq H. Nanofat grafting: basic research and clinical applications. Plast Reconstr Surg. 2013;132:1017-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 421] [Article Influence: 32.4] [Reference Citation Analysis (1)] |
| 47. | Lee SH, Lee EJ, Lee SY, Kim JH, Shim JJ, Shin C, In KH, Kang KH, Uhm CS, Kim HK, Yang KS, Park S, Kim HS, Kim YM, Yoo TJ. The effect of adipose stem cell therapy on pulmonary fibrosis induced by repetitive intratracheal bleomycin in mice. Exp Lung Res. 2014;40:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 48. | Rubio GA, Elliot SJ, Wikramanayake TC, Xia X, Pereira-Simon S, Thaller SR, Glinos GD, Jozic I, Hirt P, Pastar I, Tomic-Canic M, Glassberg MK. Mesenchymal stromal cells prevent bleomycin-induced lung and skin fibrosis in aged mice and restore wound healing. J Cell Physiol. 2018;233:5503-5512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 49. | Uji M, Nakada A, Nakamura T, Hirata K. Effect of Intratracheal Administration of Adipose-derived Stromal Cells on Bleomycin-induced Lung Injury in a Rat Model. Osaka City Med J. 2015;61:81-91. [PubMed] |
| 50. | Tashiro J, Elliot SJ, Gerth DJ, Xia X, Pereira-Simon S, Choi R, Catanuto P, Shahzeidi S, Toonkel RL, Shah RH, El Salem F, Glassberg MK. Therapeutic benefits of young, but not old, adipose-derived mesenchymal stem cells in a chronic mouse model of bleomycin-induced pulmonary fibrosis. Transl Res. 2015;166:554-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 51. | Serratrice N, Bruzzese L, Magalon J, Véran J, Giraudo L, Aboudou H, Ould-Ali D, Nguyen PS, Bausset O, Daumas A, Casanova D, Granel B, Andrac-Meyer L, Sabatier F, Magalon G. New fat-derived products for treating skin-induced lesions of scleroderma in nude mice. Stem Cell Res Ther. 2014;5:138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 52. | Chen B, Wang X, Long X, Zhang M, Huang J, Yu N, Xu J. Supportive Use of Adipose-Derived Stem Cells in Cell-Assisted Lipotransfer for Localized Scleroderma. Plast Reconstr Surg. 2018;141:1395-1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 53. | Chen W, Xia ZK, Zhang MH, Ding GC, Zhang XY, Wang ZX, Yang RY. Adipose tissue-derived stem cells ameliorates dermal fibrosis in a mouse model of scleroderma. Asian Pac J Trop Med. 2017;10:52-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 54. | Okamura A, Matsushita T, Komuro A, Kobayashi T, Maeda S, Hamaguchi Y, Takehara K. Adipose-derived stromal/stem cells successfully attenuate the fibrosis of scleroderma mouse models. Int J Rheum Dis. 2020;23:216-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 55. | Chia JJ, Zhu T, Chyou S, Dasoveanu DC, Carballo C, Tian S, Magro CM, Rodeo S, Spiera RF, Ruddle NH, McGraw TE, Browning JL, Lafyatis R, Gordon JK, Lu TT. Dendritic cells maintain dermal adipose-derived stromal cells in skin fibrosis. J Clin Invest. 2016;126:4331-4345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 56. | Maria AT, Toupet K, Maumus M, Fonteneau G, Le Quellec A, Jorgensen C, Guilpain P, Noël D. Human adipose mesenchymal stem cells as potent anti-fibrosis therapy for systemic sclerosis. J Autoimmun. 2016;70:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 95] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 57. | Daumas A, Eraud J, Hautier A, Sabatier F, Magalon G, Granel B. [Interests and potentials of adipose tissue in scleroderma]. Rev Med Interne. 2013;34:763-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 58. | Ho-Asjoe M, Khan J, Frame JD. Dermal grafting for a patient with scleroderma. Case report. Scand J Plast Reconstr Surg Hand Surg. 1996;30:325-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 59. | Magalon G, Daumas A, Sautereau N, Magalon J, Sabatier F, Granel B. Regenerative Approach to Scleroderma with Fat Grafting. Clin Plast Surg. 2015;42:353-364, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 60. | Del Papa N, Caviggioli F, Sambataro D, Zaccara E, Vinci V, Di Luca G, Parafioriti A, Armiraglio E, Maglione W, Polosa R, Klinger F, Klinger M. Autologous fat grafting in the treatment of fibrotic perioral changes in patients with systemic sclerosis. Cell Transplant. 2015;24:63-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 61. | Sautereau N, Daumas A, Truillet R, Jouve E, Magalon J, Veran J, Casanova D, Frances Y, Magalon G, Granel B. Efficacy of Autologous Microfat Graft on Facial Handicap in Systemic Sclerosis Patients. Plast Reconstr Surg Glob Open. 2016;4:e660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 62. | Blezien O, D'Andrea F, Nicoletti GF, Ferraro GA. Effects of Fat Grafting Containing Stem Cells in Microstomia and Microcheilia Derived from Systemic Sclerosis. Aesthetic Plast Surg. 2017;41:839-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 63. | Gheisari M, Ahmadzadeh A, Nobari N, Iranmanesh B, Mozafari N. Autologous Fat Grafting in the Treatment of Facial Scleroderma. Dermatol Res Pract. 2018;2018:6568016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 64. | Virzì F, Bianca P, Giammona A, Apuzzo T, Di Franco S, Mangiapane LR, Colorito ML, Catalano D, Scavo E, Nicotra A, Benfante A, Pistone G, Caputo V, Dieli F, Pirrello R, Stassi G. Combined platelet-rich plasma and lipofilling treatment provides great improvement in facial skin-induced lesion regeneration for scleroderma patients. Stem Cell Res Ther. 2017;8:236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 65. | Onesti MG, Fioramonti P, Carella S, Fino P, Marchese C, Scuderi N. Improvement of Mouth Functional Disability in Systemic Sclerosis Patients over One Year in a Trial of Fat Transplantation versus Adipose-Derived Stromal Cells. Stem Cells Int. 2016;2016:2416192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 66. | Bank J, Fuller SM, Henry GI, Zachary LS. Fat grafting to the hand in patients with Raynaud phenomenon: a novel therapeutic modality. Plast Reconstr Surg. 2014;133:1109-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 67. | Bene MD, Pozzi MR, Rovati L, Mazzola I, Erba G, Bonomi S. Autologous fat grafting for scleroderma-induced digital ulcers. An effective technique in patients with systemic sclerosis. Handchir Mikrochir Plast Chir. 2014;46:242-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 68. | Del Papa N, Di Luca G, Sambataro D, Zaccara E, Maglione W, Gabrielli A, Fraticelli P, Moroncini G, Beretta L, Santaniello A, Sambataro G, Ferraresi R, Vitali C. Regional implantation of autologous adipose tissue-derived cells induces a prompt healing of long-lasting indolent digital ulcers in patients with systemic sclerosis. Cell Transplant. 2015;24:2297-2305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 69. | Granel B, Daumas A, Jouve E, Harlé JR, Nguyen PS, Chabannon C, Colavolpe N, Reynier JC, Truillet R, Mallet S, Baiada A, Casanova D, Giraudo L, Arnaud L, Veran J, Sabatier F, Magalon G. Safety, tolerability and potential efficacy of injection of autologous adipose-derived stromal vascular fraction in the fingers of patients with systemic sclerosis: an open-label phase I trial. Ann Rheum Dis. 2015;74:2175-2182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 145] [Cited by in RCA: 140] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 70. | Guillaume-Jugnot P, Daumas A, Magalon J, Jouve E, Nguyen PS, Truillet R, Mallet S, Casanova D, Giraudo L, Veran J, Dignat-George F, Sabatier F, Magalon G, Granel B. Autologous adipose-derived stromal vascular fraction in patients with systemic sclerosis: 12-month follow-up. Rheumatology (Oxford). 2016;55:301-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 71. | Guillaume-Jugnot P, Daumas A, Magalon J, Sautereau N, Veran J, Magalon G, Sabatier F, Granel B. State of the art. Autologous fat graft and adipose tissue-derived stromal vascular fraction injection for hand therapy in systemic sclerosis patients. Curr Res Transl Med. 2016;64:35-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 72. | Daumas A, Magalon J, Jouve E, Truillet R, Casanova D, Giraudo L, Veran J, Benyamine A, Dignat-George F, Magalon G, Sabatier F, Granel B. Long-term follow-up after autologous adipose-derived stromal vascular fraction injection into fingers in systemic sclerosis patients. Curr Res Transl Med. 2017;65:40-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 73. | Song JI, Volz S, Liodaki ME, Mailänder P, Kalousis K. Stem cells therapy: the future in the management of systemic sclerosis? Hell J Nucl Med. 2017;20 Suppl:164. [PubMed] |
| 74. | Capelli C, Zaccara E, Cipriani P, Di Benedetto P, Maglione W, Andracco R, Di Luca G, Pignataro F, Giacomelli R, Introna M, Vitali C, Del Papa N. Phenotypical and Functional Characteristics of In Vitro-Expanded Adipose-Derived Mesenchymal Stromal Cells From Patients With Systematic Sclerosis. Cell Transplant. 2017;26:841-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 75. | Velier M, Simoncini S, Abellan M, Francois P, Eap S, Lagrange A, Bertrand B, Daumas A, Granel B, Delorme B, Dignat George F, Magalon J, Sabatier F. Adipose-Derived Stem Cells from Systemic Sclerosis Patients Maintain Pro-Angiogenic and Antifibrotic Paracrine Effects In Vitro. J Clin Med. 2019;8:1979. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 76. | Griffin M, Ryan CM, Pathan O, Abraham D, Denton CP, Butler PE. Characteristics of human adipose derived stem cells in scleroderma in comparison to sex and age matched normal controls: implications for regenerative medicine. Stem Cell Res Ther. 2017;8:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 77. | Magalon J, Velier M, Simoncini S, François P, Bertrand B, Daumas A, Benyamine A, Boissier R, Arnaud L, Lyonnet L, Fernandez S, Dignat-George F, Casanova D, Guillet B, Granel B, Paul P, Sabatier F. Molecular profile and proangiogenic activity of the adipose-derived stromal vascular fraction used as an autologous innovative medicinal product in patients with systemic sclerosis. Ann Rheum Dis. 2019;78:391-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 78. | Lee R, Del Papa N, Introna M, Reese CF, Zemskova M, Bonne, M, Carmen-Lopez G, Helke K, Hoffman S, Tourkina E. Adipose-derived mesenchymal stromal/stem cells in systemic sclerosis: alterations in function and beneficial effect on lung fibrosis are regulated by caveolin-1. J Scleroderma Relat Disord. 2019;4:127-136. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 79. | Kuca-Warnawin E, Skalska U, Janicka I, Musiałowicz U, Bonek K, Głuszko P, Szczęsny P, Olesińska M, Kontny E. The Phenotype and Secretory Activity of Adipose-Derived Mesenchymal Stem Cells (ASCs) of Patients with Rheumatic Diseases. Cells. 2019;8:1659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 80. | van Caam A, Vonk M, van den Hoogen F, van Lent P, van der Kraan P. Unraveling SSc Pathophysiology; The Myofibroblast. Front Immunol. 2018;9:2452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 111] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 81. | Ebmeier S, Horsley V. Origin of fibrosing cells in systemic sclerosis. Curr Opin Rheumatol. 2015;27:555-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 82. | Varga J, Marangoni RG. Systemic sclerosis in 2016: Dermal white adipose tissue implicated in SSc pathogenesis. Nat Rev Rheumatol. 2017;13:71-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 83. | Driskell RR, Jahoda CA, Chuong CM, Watt FM, Horsley V. Defining dermal adipose tissue. Exp Dermatol. 2014;23:629-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 211] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 84. | Kruglikov IL, Scherer PE. Dermal adipocytes and hair cycling: is spatial heterogeneity a characteristic feature of the dermal adipose tissue depot? Exp Dermatol. 2016;25:258-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 85. | Driskell RR, Lichtenberger BM, Hoste E, Kretzschmar K, Simons BD, Charalambous M, Ferron SR, Herault Y, Pavlovic G, Ferguson-Smith AC, Watt FM. Distinct fibroblast lineages determine dermal architecture in skin development and repair. Nature. 2013;504:277-281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 722] [Cited by in RCA: 947] [Article Influence: 78.9] [Reference Citation Analysis (0)] |
| 86. | Fleischmajer R, Damiano V, Nedwich A. Scleroderma and the subcutaneous tissue. Science. 1971;171:1019-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 100] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 87. | Fleischmajer R, Damiano V, Nedwich A. Alteration of subcutaneous tissue in systemic scleroderma. Arch Dermatol. 1972;105:59-66. [PubMed] |
| 88. | Yamamoto T, Takagawa S, Katayama I, Yamazaki K, Hamazaki Y, Shinkai H, Nishioka K. Animal model of sclerotic skin. I: Local injections of bleomycin induce sclerotic skin mimicking scleroderma. J Invest Dermatol. 1999;112:456-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 321] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 89. | Ohgo S, Hasegawa S, Hasebe Y, Mizutani H, Nakata S, Akamatsu H. Bleomycin inhibits adipogenesis and accelerates fibrosis in the subcutaneous adipose layer through TGF-β1. Exp Dermatol. 2013;22:769-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 90. | Servettaz A, Goulvestre C, Kavian N, Nicco C, Guilpain P, Chéreau C, Vuiblet V, Guillevin L, Mouthon L, Weill B, Batteux F. Selective oxidation of DNA topoisomerase 1 induces systemic sclerosis in the mouse. J Immunol. 2009;182:5855-5864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 162] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 91. | Sonnylal S, Denton CP, Zheng B, Keene DR, He R, Adams HP, Vanpelt CS, Geng YJ, Deng JM, Behringer RR, de Crombrugghe B. Postnatal induction of transforming growth factor beta signaling in fibroblasts of mice recapitulates clinical, histologic, and biochemical features of scleroderma. Arthritis Rheum. 2007;56:334-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 162] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 92. | Zhang Y, McCormick LL, Desai SR, Wu C, Gilliam AC. Murine sclerodermatous graft-versus-host disease, a model for human scleroderma: cutaneous cytokines, chemokines, and immune cell activation. J Immunol. 2002;168:3088-3098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 190] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 93. | Ruzek MC, Jha S, Ledbetter S, Richards SM, Garman RD. A modified model of graft-versus-host-induced systemic sclerosis (scleroderma) exhibits all major aspects of the human disease. Arthritis Rheum. 2004;50:1319-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 78] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 94. | Manne J, Markova M, Siracusa LD, Jimenez SA. Collagen content in skin and internal organs of the tight skin mouse: an animal model of scleroderma. Biochem Res Int. 2013;2013:436053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 95. | Christner PJ, Peters J, Hawkins D, Siracusa LD, Jiménez SA. The tight skin 2 mouse. An animal model of scleroderma displaying cutaneous fibrosis and mononuclear cell infiltration. Arthritis Rheum. 1995;38:1791-1798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 62] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 96. | Kanno Y, Matsuno H, Kawashita E, Okada K, Suga H, Ueshima S, Matsuo O. Urokinase-type plasminogen activator receptor is associated with the development of adipose tissue. Thromb Haemost. 2010;104:1124-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 97. | Wu M, Melichian DS, Chang E, Warner-Blankenship M, Ghosh AK, Varga J. Rosiglitazone abrogates bleomycin-induced scleroderma and blocks profibrotic responses through peroxisome proliferator-activated receptor-gamma. Am J Pathol. 2009;174:519-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 189] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 98. | Shi-wen X, Eastwood M, Stratton RJ, Denton CP, Leask A, Abraham DJ. Rosiglitazone alleviates the persistent fibrotic phenotype of lesional skin scleroderma fibroblasts. Rheumatology (Oxford). 2010;49:259-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 99. | Marangoni RG, Korman BD, Wei J, Wood TA, Graham LV, Whitfield ML, Scherer PE, Tourtellotte WG, Varga J. Myofibroblasts in murine cutaneous fibrosis originate from adiponectin-positive intradermal progenitors. Arthritis Rheumatol. 2015;67:1062-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 269] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 100. | Manetti M, Romano E, Rosa I, Fioretto BS, Praino E, Guiducci S, Iannone F, Ibba-Manneschi L, Matucci-Cerinic M. Systemic Sclerosis Serum Steers the Differentiation of Adipose-Derived Stem Cells Toward Profibrotic Myofibroblasts: Pathophysiologic Implications. J Clin Med. 2019;8:1256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 101. | Kruglikov IL, Zhang Z, Scherer PE. The Role of Immature and Mature Adipocytes in Hair Cycling. Trends Endocrinol Metab. 2019;30:93-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 102. | Martins V, Gonzalez De Los Santos F, Wu Z, Capelozzi V, Phan SH, Liu T. FIZZ1-induced myofibroblast transdifferentiation from adipocytes and its potential role in dermal fibrosis and lipoatrophy. Am J Pathol. 2015;185:2768-2776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 103. | Taki Z, Gostjeva E, Thilly W, Yaseen B, Lopez H, Mirza M, Hassuji Z, Vigneswaran S, Ahmed Abdi B, Hart A, Arumalla N, Thomas G, Denton CP, Suleman Y, Liu H, Venturini C, O'Reilly S, Xu S, Stratton R. Pathogenic Activation of Mesenchymal Stem Cells Is Induced by the Disease Microenvironment in Systemic Sclerosis. Arthritis Rheumatol. 2020;72:1361-1374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 104. | Wei J, Fang F, Lam AP, Sargent JL, Hamburg E, Hinchcliff ME, Gottardi CJ, Atit R, Whitfield ML, Varga J. Wnt/β-catenin signaling is hyperactivated in systemic sclerosis and induces Smad-dependent fibrotic responses in mesenchymal cells. Arthritis Rheum. 2012;64:2734-2745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 201] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 105. | Wei J, Bhattacharyya S, Jain M, Varga J. Regulation of Matrix Remodeling by Peroxisome Proliferator-Activated Receptor-γ: A Novel Link Between Metabolism and Fibrogenesis. Open Rheumatol J. 2012;6:103-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 106. | Wei J, Bhattacharyya S, Tourtellotte WG, Varga J. Fibrosis in systemic sclerosis: emerging concepts and implications for targeted therapy. Autoimmun Rev. 2011;10:267-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 137] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 107. | Korman B, Marangoni RG, Lord G, Olefsky J, Tourtellotte W, Varga J. Adipocyte-specific Repression of PPAR-gamma by NCoR Contributes to Scleroderma Skin Fibrosis. Arthritis Res Ther. 2018;20:145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 108. | Lafyatis R, Mantero JC, Gordon J, Kishore N, Carns M, Dittrich H, Spiera R, Simms RW, Varga J. Inhibition of β-Catenin Signaling in the Skin Rescues Cutaneous Adipogenesis in Systemic Sclerosis: A Randomized, Double-Blind, Placebo-Controlled Trial of C-82. J Invest Dermatol. 2017;137:2473-2483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 109. | Wei J, Marangoni RG, Fang F, Wang W, Huang J, Distler JHW, Varga J. The non-neuronal cyclin-dependent kinase 5 is a fibrotic mediator potentially implicated in systemic sclerosis and a novel therapeutic target. Oncotarget. 2018;9:10294-10306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 110. | Mastrogiannaki M, Lichtenberger BM, Reimer A, Collins CA, Driskell RR, Watt FM. β-Catenin Stabilization in Skin Fibroblasts Causes Fibrotic Lesions by Preventing Adipocyte Differentiation of the Reticular Dermis. J Invest Dermatol. 2016;136:1130-1142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 111. | El Agha E, Moiseenko A, Kheirollahi V, De Langhe S, Crnkovic S, Kwapiszewska G, Szibor M, Kosanovic D, Schwind F, Schermuly RT, Henneke I, MacKenzie B, Quantius J, Herold S, Ntokou A, Ahlbrecht K, Braun T, Morty RE, Günther A, Seeger W, Bellusci S. Two-Way Conversion between Lipogenic and Myogenic Fibroblastic Phenotypes Marks the Progression and Resolution of Lung Fibrosis. Cell Stem Cell 2017; 20: 261-273. e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 214] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 112. | Plikus MV, Guerrero-Juarez CF, Ito M, Li YR, Dedhia PH, Zheng Y, Shao M, Gay DL, Ramos R, Hsi TC, Oh JW, Wang X, Ramirez A, Konopelski SE, Elzein A, Wang A, Supapannachart RJ, Lee HL, Lim CH, Nace A, Guo A, Treffeisen E, Andl T, Ramirez RN, Murad R, Offermanns S, Metzger D, Chambon P, Widgerow AD, Tuan TL, Mortazavi A, Gupta RK, Hamilton BA, Millar SE, Seale P, Pear WS, Lazar MA, Cotsarelis G. Regeneration of fat cells from myofibroblasts during wound healing. Science. 2017;355:748-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 464] [Article Influence: 51.6] [Reference Citation Analysis (0)] |
| 113. | Kruglikov IL. Interfacial Adipose Tissue in Systemic Sclerosis. Curr Rheumatol Rep. 2017;19:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 114. | Żółkiewicz J, Stochmal A, Rudnicka L. The role of adipokines in systemic sclerosis: a missing link? Arch Dermatol Res. 2019;311:251-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 115. | Stochmal A, Czuwara J, Zaremba M, Rudnicka L. Altered serum level of metabolic and endothelial factors in patients with systemic sclerosis. Arch Dermatol Res. 2020;312:453-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 116. | Olewicz-Gawlik A, Danczak-Pazdrowska A, Kuznar-Kaminska B, Batura-Gabryel H, Katulska K, Wojciech S, Trzybulska D, Hrycaj P. Circulating adipokines and organ involvement in patients with systemic sclerosis. Acta Reumatol Port. 2015;40:156-162. [PubMed] |
| 117. | Lakota K, Wei J, Carns M, Hinchcliff M, Lee J, Whitfield ML, Sodin-Semrl S, Varga J. Levels of adiponectin, a marker for PPAR-gamma activity, correlate with skin fibrosis in systemic sclerosis: potential utility as biomarker? Arthritis Res Ther. 2012;14:R102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 118. | Fang F, Liu L, Yang Y, Tamaki Z, Wei J, Marangoni RG, Bhattacharyya S, Summer RS, Ye B, Varga J. The adipokine adiponectin has potent anti-fibrotic effects mediated via adenosine monophosphate-activated protein kinase: novel target for fibrosis therapy. Arthritis Res Ther. 2012;14:R229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 93] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 119. | Marangoni RG, Masui Y, Fang F, Korman B, Lord G, Lee J, Lakota K, Wei J, Scherer PE, Otvos L, Yamauchi T, Kubota N, Kadowaki T, Asano Y, Sato S, Tourtellotte WG, Varga J. Adiponectin is an endogenous anti-fibrotic mediator and therapeutic target. Sci Rep. 2017;7:4397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 120. | Yamashita T, Lakota K, Taniguchi T, Yoshizaki A, Sato S, Hong W, Zhou X, Sodin-Semrl S, Fang F, Asano Y, Varga J. An orally-active adiponectin receptor agonist mitigates cutaneous fibrosis, inflammation and microvascular pathology in a murine model of systemic sclerosis. Sci Rep. 2018;8:11843. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 121. | Budulgan M, Dilek B, Dağ ŞB, Batmaz I, Yıldız İ, Sarıyıldız MA, Çevik R, Nas K. Relationship between serum leptin level and disease activity in patients with systemic sclerosis. Clin Rheumatol. 2014;33:335-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 122. | Masui Y, Asano Y, Shibata S, Noda S, Akamata K, Aozasa N, Taniguchi T, Takahashi T, Ichimura Y, Toyama T, Sumida H, Yanaba K, Tada Y, Sugaya M, Sato S, Kadono T. A possible contribution of visfatin to the resolution of skin sclerosis in patients with diffuse cutaneous systemic sclerosis via a direct anti-fibrotic effect on dermal fibroblasts and Th1 polarization of the immune response. Rheumatology (Oxford). 2013;52:1239-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 123. | Miura S, Asano Y, Saigusa R, Yamashita T, Taniguchi T, Takahashi T, Ichimura Y, Toyama T, Tamaki Z, Tada Y, Sugaya M, Sato S, Kadono T. Serum vaspin levels: A possible correlation with digital ulcers in patients with systemic sclerosis. J Dermatol. 2015;42:528-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 124. | Korman BD, Marangoni RG, Hinchcliff M, Shah SJ, Carns M, Hoffmann A, Ramsey-Goldman R, Varga J. Brief Report: Association of Elevated Adipsin Levels With Pulmonary Arterial Hypertension in Systemic Sclerosis. Arthritis Rheumatol. 2017;69:2062-2068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 125. | Yokoyama Y, Sekiguchi A, Fujiwara C, Uchiyama A, Uehara A, Ogino S, Torii R, Ishikawa O, Motegi SI. Inhibitory Regulation of Skin Fibrosis in Systemic Sclerosis by Apelin/APJ Signaling. Arthritis Rheumatol. 2018;70:1661-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 126. | Huang S, Chen L, Lu L, Li L. The apelin-APJ axis: A novel potential therapeutic target for organ fibrosis. Clin Chim Acta. 2016;456:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 127. | Aozasa N, Asano Y, Akamata K, Noda S, Masui Y, Yamada D, Tamaki Z, Tada Y, Sugaya M, Kadono T, Sato S. Serum apelin levels: clinical association with vascular involvements in patients with systemic sclerosis. J Eur Acad Dermatol Venereol. 2013;27:37-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 128. | Miura S, Asano Y, Saigusa R, Yamashita T, Taniguchi T, Takahashi T, Ichimura Y, Toyama T, Tamaki Z, Tada Y, Sugaya M, Sato S, Kadono T. Serum omentin levels: A possible contribution to vascular involvement in patients with systemic sclerosis. J Dermatol. 2015;42:461-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Cell and tissue engineering
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kosalka-Wegiel J S-Editor: Gao CC L-Editor: A P-Editor: Xing YX