Published online Sep 26, 2020. doi: 10.4252/wjsc.v12.i9.986
Peer-review started: March 25, 2020
First decision: April 29, 2020
Revised: May 25, 2020
Accepted: June 2, 2020
Article in press: June 2, 2020
Published online: September 26, 2020
Processing time: 180 Days and 9.5 Hours
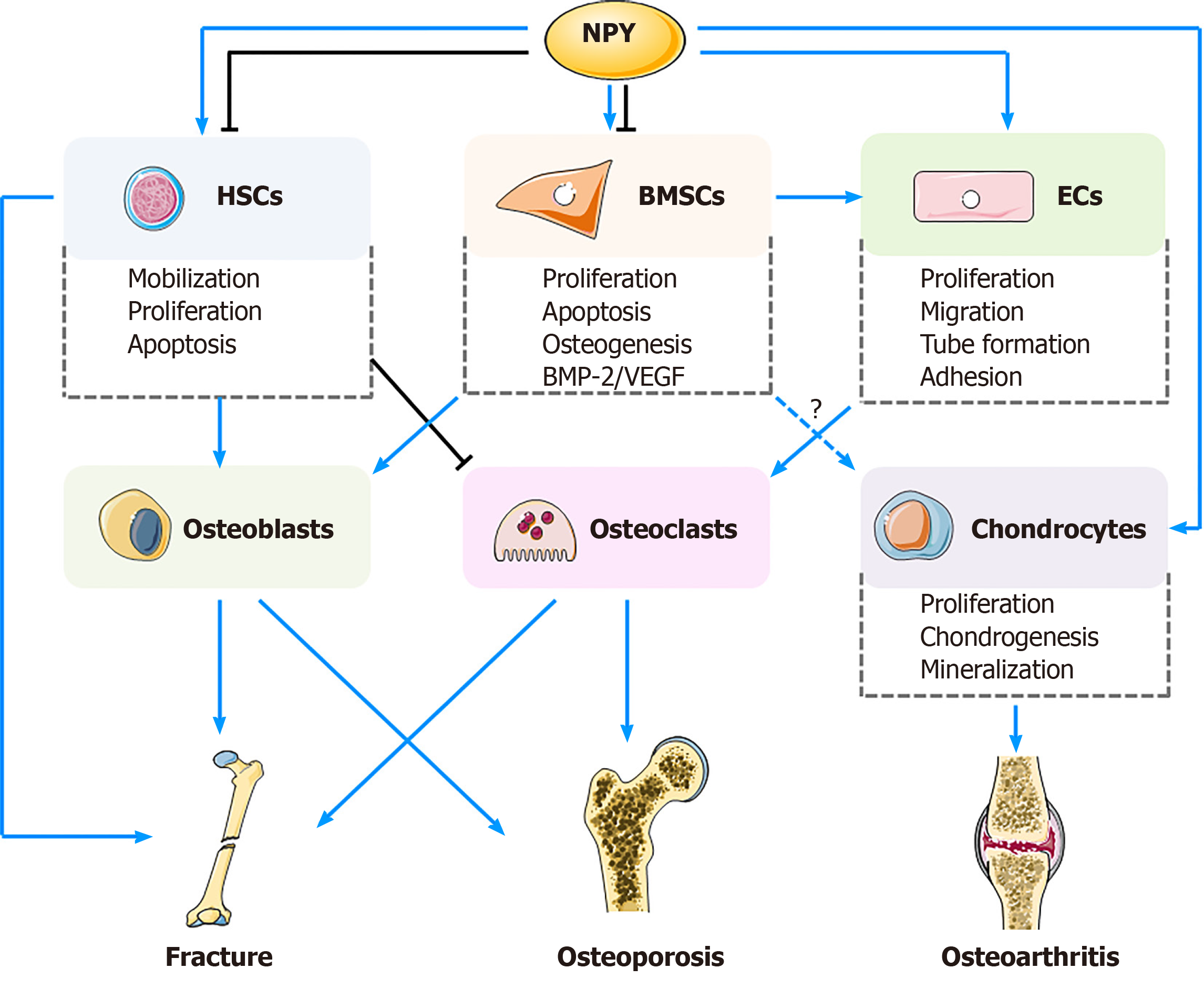
Musculoskeletal disorders are the leading causes of disability and result in reduced quality of life. The neuro-osteogenic network is one of the most promising fields in orthopaedic research. Neuropeptide Y (NPY) system has been reported to be involved in the regulations of bone metabolism and homeostasis, which also provide feedback to the central NPY system via NPY receptors. Currently, potential roles of peripheral NPY in bone metabolism remain unclear. Growing evidence suggests that NPY can regulate biological actions of bone marrow mesenchymal stem cells, hematopoietic stem cells, endothelial cells, and chondrocytes via a local autocrine or paracrine manner by different NPY receptors. The regulative activities of NPY may be achieved through the plasticity of NPY receptors, and interactions among the targeted cells as well. In general, NPY can influence proliferation, apoptosis, differentiation, migration, mobilization, and cytokine secretion of different types of cells, and play crucial roles in the development of bone delayed/non-union, osteoporosis, and osteoarthritis. Further basic research should clarify detailed mechanisms of action of NPY on stem cells, and clinical investigations are also necessary to comprehensively evaluate potential applications of NPY and its receptor-targeted drugs in management of musculoskeletal disorders.
Core tip: Neuropeptide Y (NPY) system is crucial for bone metabolism and homeostasis. NPY can regulate biological effects of different types of cells through central and peripheral nervous systems. Here, we summarize recent findings regarding the roles of NPY and its receptors in bone metabolism and homeostasis, and discuss the biological actions and underlying mechanisms of NPY on bone marrow mesenchymal stem cells, hematopoietic stem cells, endothelial cells, and chondrocytes. We also review the potential applications and efficacy of NPY and NPY receptor-targeted drugs in the treatment of fracture healing, osteoporosis, and osteoarthritis.
- Citation: Wu JQ, Jiang N, Yu B. Mechanisms of action of neuropeptide Y on stem cells and its potential applications in orthopaedic disorders. World J Stem Cells 2020; 12(9): 986-1000
- URL: https://www.wjgnet.com/1948-0210/full/v12/i9/986.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v12.i9.986
As a substantial portion of the whole body, skeletal muscles are integral for locomotion and metabolic health[1]. Musculoskeletal disorders, such as fracture, delayed/non-union, osteoporosis, and osteoarthritis, are the primary causes of disability and lead to reduced life quality. Skeletal metabolism and homeostasis are accurately regulated by neural signal networks between nervous systems and bone cells.
Recently, neuropeptide Y (NPY) has emerged as one of the major regulators of bone metabolism and homeostasis. NPY, a 36-amino-acid peptide first isolated from the porcine brain by Tatemoto[2] in 1982, is widely distributed in the central nervous system (CNS) and peripheral nervous system[3]. It is produced by nerve endings, and acts as a critical molecule in the interactions between nerves and the osseous system through central- and peripheral-mediated pathways[4,5]. NPY can maintain the homeostases of bone, blood vessels, and immune system via different NPY receptors[6,7]. Previous studies have indicated that NPY can stimulate proliferation, promote osteoblastic differentiation, and prevent apoptosis of bone marrow mesenchymal stem cells (BMSCs) though Y1R[8]. In addition, NPY is also able to facilitate neuroprotection, restore bone marrow dysfunction, and thus mediate bone marrow microenvironment[9]. Aside from BMSCs, treatment with NPY caused a decreased number of osteoclasts by promoting mobilization of hematopoietic stem cells (HSCs) via Y2R and Y5R. Furthermore, NPY can accelerate endothelial cell (EC) proliferation and capillary tube formation though Y1R, Y2R, and Y5R[9,10]. As NPY possesses capacities of regulating different types of cells, it determines the relative rates of bone formation and resorption process, which is critical for prevention against bone structure damage and bone metabolic disorders[11].
In recent years, stem cell therapy is a burgeoning field in regeneration and restoration of the impaired musculoskeletal tissues[12]. Enrichment and differentiation of stem cells have been confirmed for the benefits in bone regeneration and maintenance of bone homeostasis. As both experiments and clinical investigations have revealed definite efficacy of stem cells in treatment of fractures, osteoporosis, cartilage, and ligament injuries[13-15], it has become an attractive avenue of research for therapeutic applications in musculoskeletal disorders.
This article reviews the current knowledge of NPY, potential roles of NPY receptors, and interactions among NPY, NPY receptors, and stem cells, primarily BMSCs and HSCs. In addition, the potential influences of NPY on biological functions of ECs and chondrocytes, which are also involved in the development of many orthopaedic disorders, are also discussed. Furthermore, the potential applications and efficacy of NPY and its receptor-targeted drugs in the treatment of fracture, osteoporosis, and osteoarthritis are also summarized.
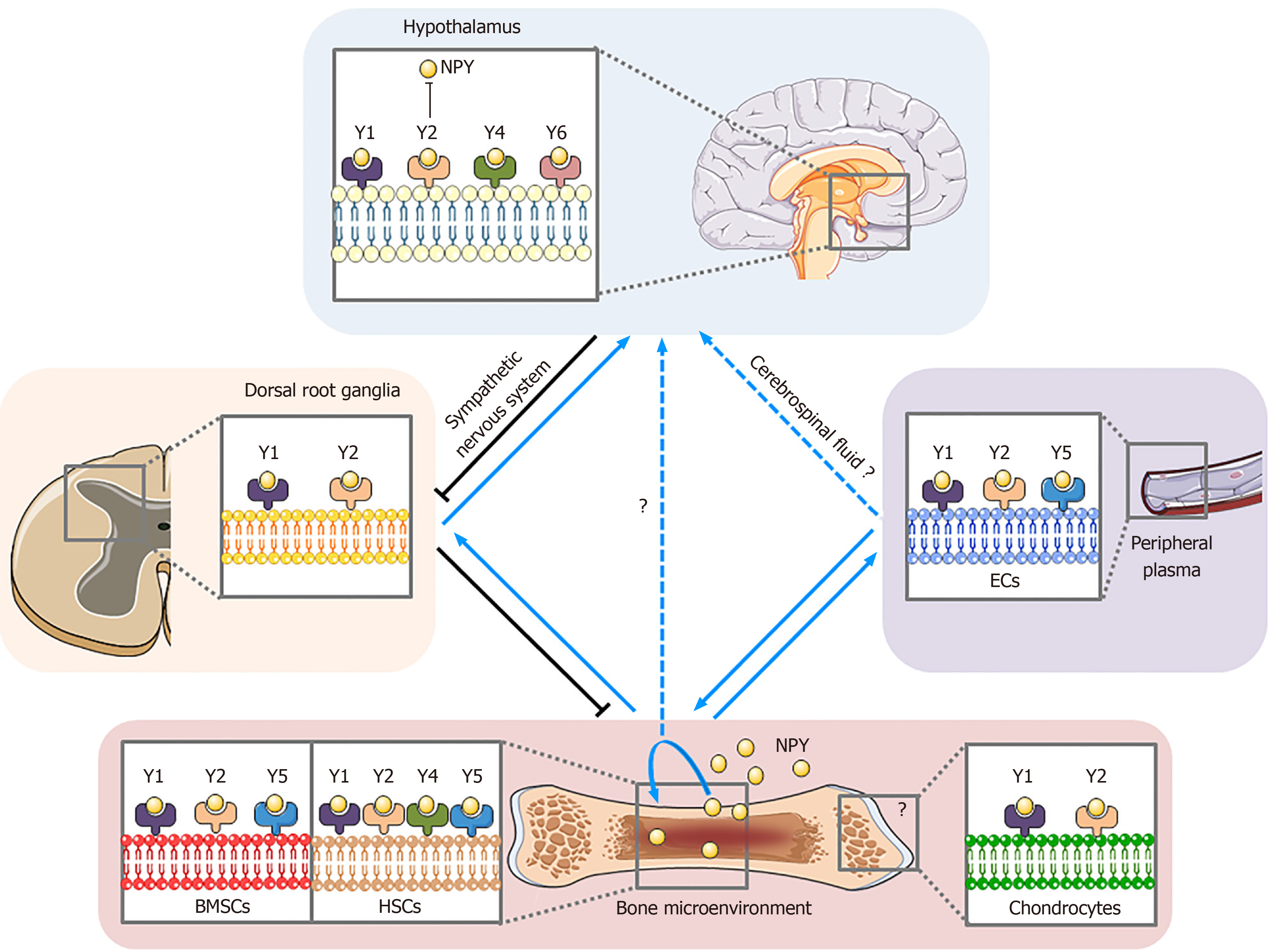
Recent studies have shown that NPY participates in many physiological and psychological processes, such as inhibition of vascular smooth muscle contraction and alleviation of anxiety and depression[16,17]. Till now, five primary NPY receptors (Y1R, Y2R, Y4R, Y5R, and y6R) have been found in mammals, and all of them belong to the superfamily of G protein-coupled receptors[18]. Different receptors are distributed differently in the human body, play different biological functions, and have different affinities for NPY (Y2R > Y1R > Y5R, Y4R = y6R)[19]. Y1R and Y2R are reported to be involved in bone homeostasis. Y4R is distributed in both brain and peripheral tissues[20]. Y5R, predominant in the CNS, consistently co-localizes with Y1R[21]. y6R, also observed in rat genome, seems to be non-functional in humans[22].
Current evidence indicates that hypothalamic secreted NPY inhibits bone formation. Previous in vivo studies found that an increase of NPY in the hypothalamus led to a decreased volume of cancellous bone and inhibition of the osteoblasts activity[23,24]. These results are similar to the finding of another study that overexpression of hypothalamus-specific NPY in the wild-type (WT) mice displayed anti-osteogenic effects[25]. Likewise, both deficiency of NPY [NPY (-/-)] in mice and inhibition of central NPY signaling pathway can induce bone gain[5,26]. As targeted deletion of the NPY gene in the hypothalamus has not been realized yet, current research of the potential effects of hypothalamus-specific NPY on peripheral stem cells may be conducted via the approach of isolating BMSCs or other stem cells from mice deficient in hypothalamus-specific NPY.
It is known that both Y1R and Y2R are distributed abundantly in the CNS. As an auto-receptor, Y2R is primarily located presynaptically, and inhibits NPY expression and release[27,28]. Both hypothalamus and germline deletions of Y2R produce an identically promotive bone anabolic phenotype, implying that hypothalamic Y2R may modulate bone formation via CNS mechanism, and also protect against central NPY-induced bone loss[26,29]. A previous study showed that the osteoblastic activity of the mice with double knockout of Y4R and Y2R in the hypothalamus was more obvious than those with only knockout of Y2R, demonstrating the probably synergistic role of Y4R in hypothalamic control of the bone mass[30]. Nonetheless, targeted deletion of Y1R in the hypothalamus failed to recapitulate this increased bone mass phenotype, which had been observed in systematic deficiency of Y1R [Y1R (-/-)] mice. This implies that Y1R may participate in the regulation of bone regulation by non-hypothalamic pathways[31]. Interestingly, double deletions of global Y1R and Y2R in mice did not result in any additive effects on bone phenotype, suggesting that Y1R and Y2R may share a common pathway in regulation of bone homeostasis[31]. As for y6R, its mRNA is only expressed in the hypothalamus but not in bone components, such as BMSCs, osteoblasts, or osteoclasts. Compared to the WT controls, significantly decreased bone density and volumes of cortical and cancellous bone were found in the mice with y6R(-/-) in the hypothalamus, which is primarily attributed to the increasing number of osteoclast precursors in y6R(-/-) mice[22].
Peripheral NPY acts directly in a paracrine fashion to maintain the bone homeostasis. Growing evidence shows that NPY is expressed in non-neuronal cells in the bone marrow microenvironment, such as osteoblasts[32], osteocytes[33], BMSCs[8,34], and ECs[35]. In vitro studies have indicated that NPY has direct effects on osteoblast lineage by inhibiting differentiation of mesenchymal progenitors and mineralization of mature osteoblasts[33,36]. Overexpression of osteoblasts-specific NPY (Col2.3NPY) resulted in decreases in bone trabecular number, thickness, and volume[37], whereas changes of serological NPY levels did not reveal such effects[37]. These results imply that overexpression of local NPY may cause changes of bone phenotypes. Outcomes of clinical studies have revealed that patients with craniocerebral injury had accelerated fracture healing and higher serological NPY levels, the latter of which showed a positive correlation with the severity of craniocerebral injury[38]. Gu et al[38] inferred that serum NPY may originate from cerebrospinal fluid, as the NPY level in the serum was almost equal to that in the cerebrospinal fluid among the patients with craniocerebral injury, and severe craniocerebral injury may cause leakage of cerebrospinal fluid[38,39].
It is definite that Y1R is expressed in osseous tissue, including adipocytes, osteoblasts, and bone marrow cells[8,33,40-42]; however, whether Y2R is expressed in the bone or not remains in debate. Some studies reported that Y2R can be found in MC3T3 and BMSCs[41,42], but not in osteoblasts[43]. It is speculated that such differences may be explained by two reasons. The first reason is that Y2R exists in the bone, but may be expressed under specific conditions, and thus, it cannot always be detected. Second, potential limitations of the current techniques may also affect the detection rate. As for Y1R, both in vitro and in vivo studies have shown that the mice with knockout of osteoblast-specific Y1R recapitulate the bone phenotype of germline Y1R deficient mice[5,36]. These findings confirm the role of Y1R in inhibiting bone formation, as well as in enlarging the negative effects of NPY on osteocytes. Although the selective deletion of Y1R from osteoblasts did not hinder the process of fracture healing, lack of systemic Y1R caused delays of endochondral fracture repair[44]. Considering that Y1R plays important roles in many physiological functions, aside from the above-mentioned issues, other underlying mechanisms may also account for the effects of global Y1R deletion on bone healing process (Figure 1).
BMSCs, isolated from bone marrow, are termed as a “fibroblast-like” osteogenic cell population. With plastic-adherent culture characteristics, BMSCs express specific surface antigens CD105 and CD90 (> 95%) but not CD45 or CD34 (< 2%)[45], and are capable of differentiating into osteoblasts, chondrocytes, and adipocytes[19,46]. As BMSCs play a vital role in repairing musculoskeletal tissues, fracture healing and spinal injury regeneration can be accelerated following application of BMSCs[47]. Local injection of BMSCs has also yielded promising results in the treatment of bone nonunion and bone defect[48].
Currently, conflicting results still exist regarding the potential role of NPY in proliferation of BMSCs[8,36,42]. Our previous study revealed that NPY can enhance proliferation and prevent apoptosis of BMSCs in a concentration-dependent manner by activating the Wnt/β-catenin signaling pathway. Such NPY-induced activities were partially blocked by PD160170, a Y1R antagonist[8], implying that NPY-induced proliferative and anti-apoptotic effects of BMSCs may be partially achieved through Y1R. Another study also found that NPY is able to stimulate proliferation of BMSCs derived from rats of different ages, and this capacity was blocked by Y5R antagonist, demonstrating an inhibitory role of Y5R in the proliferation of rat BMSCs. In addition, Igura et al[42] found that NPY increased the proliferation of BMSCs of transgenic overexpression of Y5R in the elder rats by activating extracellular signal-regulated kinase 1/2 (Erk1/2) pathways. Aside from BMSCs, NPY can also promote the proliferation of human embryonic stem cells, which was achieved via NPY/Y1R/Y5R by activation of ERK1/2 pathways[49]. However, one study failed to find a promotive role of NPY on BMSC proliferation. Lee et al[36] reported that BMSCs isolated from Y1R (-/-) mice formed a greater number and larger size of colonies than the WT controls, implying that NPY may inhibit BMSC proliferation.
Apart from its potential influences on BMSC proliferation, NPY can also facilitate the migration of BMSCs by upregulated expression of CXC chemokin receptor 4[50], which is in accordance with the finding of our study that NPY therapy significantly increased the total migration distance and speed of BMSCs[51].
In addition to the controversy regarding the effect of NPY on the proliferation of BMSCs, the potential activities of NPY on osteogenic differentiation of BMSCs and the underlying mechanisms are also in debate. Some studies found that NPY stimulated the differentiation of BMSCs into osteoblasts, which was supported by upregulating the expression of alkaline phosphatase (ALP), collagen type I (COL-I), osteocalcin (OCN), and runt-related transcription factor 2 (Runx2) through the Wnt signaling pathway[51,52]. Other studies reported that NPY inhibited osteogenic differentiation of BMSCs, evidenced by the findings of decreased ALP and OCN expression, and reduced mineralization of BMSCs as well[41]. Besides, another study also found the inhibitory effect of NPY on isoprenaline-induced differentiation into osteoblasts from BMSCs[40]. Interestingly, BMSCs isolated from NPY (-/-) mice display an increased ability in osteogenic differentiation, which was confirmed by increases in ALP activity, OCN gene expression, and mineralization[52]. These diverse outcomes can be explained by the fact that NPY-induced osteogenic differentiation of BMSCs may be achieved via auto-regulation mechanisms.
Growing evidence has revealed that auto-regulation mechanisms of NPY may correlate to the plasticity of its receptors. It has been noted that NPY led to upregulated expression of Y1R throughout BMSC osteogenic differentiation[36,38,41]. In a recent study, Wee et al[52] found that during osteogenic differentiation of BMSCs in the WT mice, the expression of Y1R was increased while NPY was decreased. However, as in NPY (-/-) mice, Y1R expression level did not alter during differentiation, demonstrating that increased Y1R expression during BMSC differentiation may be assisted or induced by NPY. Outcomes of NPY or its receptor gene knockout animal models revealed that the presence of functional Y1R directly hindered the osteogenesis of BMSCs or bone cells, as evidenced by the finding that BMSCs isolated from Y1R (-/-) mice displayed an increased capacity of osteogenic differentiation[36]. An in vitro experiment showed that blockade of Y1R by PD160170 facilitated osteogenic differentiation of BMSCs[53]. On the contrary, Dong et al[34] reported that melatonin can upregulate the expression of NPY and Y1R, and promote MSC osteoblastic differentiation. Apart from BMSCs, lack of Y1R also promoted differentiation of mesenchymal progenitor cells and activated mature osteoblasts[36]. Yahara et al[54] also noticed that inhibition of Y1R increased the ALP activity and mineralization in mouse pre-osteoblast MC3T3-E1 cells.
Aside Y1R, Y2R may also participate in osteogenic differentiation of BMSCs, which is supported by the finding that BMSCs, treated with either NPY1–36 (universal Y2R agonist) or PYY3-36 (Y2R preferring agonist), revealed significantly elevated levels of ALP activity and OCN expression. Such effects of NPY1-36 were blocked by a Y2R antagonist, BII0246, and a marked decrease of Y1R protein level was also found following treatment with exogenous PYY3–36 or NPY1–36[41].
During osteogenic differentiation of BMSCs, potential interactions may exist between Y1R and Y2R[42,43]. By detecting the NPY ligand-receptor system in BMSCs derived from rats of different ages, Igura et al[42] found that, although NPY expression increased with age, Y1R protein was upregulated whereas Y2R protein was downregulated with an increase in age. In addition, Lundberg et al[43] found that the lack of Y2R signaling mediated downregulation of Y1R in BMSCs, which was proved by the finding of decreased expression of Y1R in BMSCs from Y2R (-/-) mice. They inferred that downregulation of Y1R is possibly due to the lack of feedback inhibition of NPY release and resulted in elevated levels of NPY, which in turn caused subsequent overstimulation of Y1R, following desensitization and downregulation of the Y1R population[43]. Moreover, alternation of Y1R expression may have different effects on NPY. The precursor osteogenic cells (e.g., BMSCs and osteoblast precursor cells), which are able to inhibit osteogenic differentiation through Y1R, have low expression levels of Y1R. However, in osteogenic conditions (e.g., osteogenic induction medium), Y1R expression in these cells is increased, with Y2R expression decreased.
In addition to Y1R and Y2R, y6R may also be involved in the regulation of BMSC differentiation into osteoblasts. BMSCs isolated from y6R (-/-) mice showed significant reductions of ALP, osterix, and mineralizing surface, implying possibly opposite roles of Y6R to those of Y1R and Y2R in BMSC differentiation and activities[22].
Currently, some studies also reported potential mechanisms of NPY in mediation of BMSC osteogenic differentiation from another perspectives. Gu et al[38] indicated that NPY can directly promote the osteogenic differentiation of MSCs by upregulating Runx2. Ma et al[55] reported that the anabolic activity of osteoblasts treated with NPY may also enhance the gap junction intercellular communication (GJIC). Tang et al[56] noticed that the levels of NPY and p-ERK1/2 in fracture model rats were significantly higher than those in the controls. They also found that use of BIBP3226, a Y1R antagonist, inhibited the fracture healing process by downregulating the p-ERK expression in the fracture site, indicating that the ERK pathway may participate in the NPY-induced effects on fracture healing. Additionally, Sharma et al[57] also observed that activation of ERK could facilitate osteogenic differentiation of human MSCs.
In summary, considering the still existing controversies regarding the role of NPY in BMSCs and still not-well-understood mechanisms, future more studies are warranted to provide more definitive evidence regarding the links between NPY/NPY receptors and BMSCs.
HSCs, or hematopoietic stem/progenitor cells, responsible for regeneration and repopulation of all blood cell lineages, contact osteoblasts in endosteal microenvironments or sinusoidal endothelium[58]. NPY receptors Y1, Y2, Y4, and Y5 were found to be highly expressed in HSCs, and NPY plays a crucial role in the proliferation and mobilization of HSCs[59,60].
Growing evidence has suggested that NPY acts directly or indirectly in the regulation of HSC proliferation. NPY can directly inhibit the proliferation of HSCs in cell cultures, as confirmed by an increased number of HSCs in G0 phase, with decreased numbers of cells in S and G2/M phases[60]. Besides, the number of HSCs in NPY (-/-) mice is decreased, suggesting that NPY may protect HSCs in the bone marrow microenvironment[9,61].
In addition to potential influences on HSC proliferation, NPY and its receptors are also involved in regulating the survival and mobilization of HSCs. It was reported that NPY/Y1R can improve the survival and apoptosis of HSCs, which maintains the survival of nestin+ cells, and thus be linked to retention of HSCs[9]. NPY-induced biological effects on HSCs, osteoblasts, and osteoclasts play an important role in the process of fracture healing. Nonetheless, detailed mechanisms of such effects remain largely unclear. Several studies explored the underlying mechanisms from different perspectives. Park et al[61] indicated that the effect of NPY on HSC mobilization might be achieved by increasing the expression levels of matrix metalloproteinase 9 (MMP-9) in osteoblasts via Y1R, which was strengthened by the finding that NPY failed to display a positive activity on HSC mobilization in mice with Y1R (-/-) in osteoblasts. Singh et al[59] reported that NPY3-36, a agonist of Y2R and Y5R, facilitated the mobilization of HSCs to the peripheral blood, whereas selective Y2R and Y5R antagonists hindered such activity. It has been noted that NPY can be also secreted by HSCs, indicating that HSCs may exert regulatory feedback on itself by releasing NPY[9]. In ovariectomized mice, NPY therapy could help reduce the bone loss due to HSC mobilization, and result in an increased number of osteoblasts and a decreased number of osteoclasts[61]. Using an ovariectomy-induced osteoporosis mouse model, Park et al[62] also found that NPY-based recombinant peptides could relieve ovariectomy-induced bone loss and may be used for osteoporosis treatment.
In summary, current evidence suggests that NPY is able to induce the rapid mobilization of HSCs into the peripheral blood, and increase the number of osteoblasts. Therefore, it is reasonable to believe that a comprehensive understanding of the role of NPY in HSCs may pave the way for its future clinical applications[63].
NPY-positive fibers predominantly localize alongside blood vessels in bone tissue and bone marrow, and associate with EC migration, capillary tube formation, and self-renewal[10,64,65]. ECs express Y1R and Y2R and can produce, store, and respond to NPY, suggesting an autocrine regulatory mechanism of NPY in the endothelium (Figure 2)[10,35,66].
In vitro studies have revealed that NPY can promote the migration and capillary tube formation of human ECs via Y1R, Y2R, and Y5R[10,65]. Previous studies also indicated that NPY-induced angiogenic effect on ECs was achieved primarily through Y2R[65,67]. Furthermore, NPY can regulate the angiogenic process by influencing the proliferation of ECs, which was achieved mainly via Y5R[10]. NPY3-36, an agonist of Y2R and Y5R, was found to be able to reduce EC contact and increase vascular permeability, and selective Y2R and Y5R antagonists restored the vascular integrity[59]. Interactions may exist among BMSCs, HSCs, and ECs via NPY. It has been observed that NPY originating from platelet lysate caused an decreased angiogenic activity of human adipose stromal cells, which may be linked to reduced expression of vascular endothelial growth factor (VEGF) and a lower intracellular calcium level[68]. As a ubiquitous and potent peptide, VEGF is involved in many angiogenic cascades. Increased levels of VEGF facilitate angiogenesis and osteoblastic differentiation of BMSCs[69], and the level of VEGF secreted by BMSCs is elevated following treatment with NPY[51]. Wang et al[50] found that NPY promoted endothelial differentiation and tube formation of BMSCs, the latter of which is involved in all the stages of EC angiogenesis, including survival and proliferation, migration, tube formation, and maturation of blood vessels[70].
Although chondroblasts and osteoblasts share the same progenitor reservoir (BMSCs), specific effects of NPY on chondrocytes have not been clarified. However, anatomical studies have indicated that NPY-positive sympathetic nerve fibers are located in cartilage, and chondrocytes can also secret NPY[32].
NPY can promote the proliferation of both chondrocytes and articular cartilage, and the effect of NPY on chondrogenesis may be achieved through autocrine mechanisms via Y1R[32]. A new study found that intra-articular injection of NPY caused more severe osteoarthritis phenotypes, which was evidenced by more severe cartilage degradation and fibrillation, whereas a combination of NPY with BIIE0246 (Y2R antagonist) but not BIBO3304 (Y1R antagonist) significantly alleviated the above negative effects, indicating that Y2R may play an important role in NPY-induced chondrocyte hypertrophy and cartilage matrix degradation[71]. In addition, NPY-induced chondrocyte hypertrophy was also marked by increased levels of col10a1 (a biomarker indicating hypertrophy of chondrocytes), MMP-13, and ADAMTS-5 through activation of mTORC1 in a Y2R-dependent manner[71]. Chen et al[72] found that NPY markedly augmented the expression of Col2a1 (a biomarker indicating proliferation of chondrocytes), Col10a1, and OCN in the murine chondrogenic cell line ATDC5. And inhibition of Y1R partly hindered the capability of NPY, demonstrating that Y1R may participate in NPY-induced activities (proliferation, chondrogenesis, and mineralization) in ATDC5 cells[72]. It is known that Runx2 and Osterix are biomarkers for chondrocyte differentiation and cartilage mineralization. In the Y1R (-/-) mice, the expression levels of Runx2 and Osterix increased in the long bones[36], both of which facilitated the formation of cartilage callus. Based on current findings, potential strategies to solve NPY-related hypertrophy of chondrocytes and cartilage degradation may be a research hotspot in the future.
Fracture healing process can be divided into inflammatory, reparative, and remodeling stages. During the initial phase, BMSCs are recruited to the fracture site and differentiate into chondrocytes simultaneously, and the level of NYP in the peripheral blood is increased[56]. NPY- and Y1R-positive BMSCs and osteoblasts can be found in the new osseous tissue[64]. Innervation of NPY occurs in a spatio-temporal dependent manner in the inflammatory and remodeling stages[73], demonstrating different functions of NPY among different fracture stages. Previous studies found that the volumes of cortical and cancellous bones in NPY-deficient mice were significantly increased, which may result from elevated osteoblast activities and upregulated expression of Runx2 and Osterix[23,24]. Lundberg et al[43] reported that, compared with the WT controls, Y2R (-/-) mice presented with greater bone mass, which may correlate with the reinforced abilities of BMSCs, thus being able to produce more mineralized extracellular matrix as well as increased expression of ALP and OCN. As mentioned previously, NPY can directly increase the number and viability of BMSCs by promoting their proliferation and inhibiting apoptosis[8], together with increased osteogenic differentiation and BMP-2 expression[51]. Aside from in vitro and in vivo experiments, clinical observations also confirmed the role of NPY in fracture healing process. Gu et al[38] reported that, compared with those with a single fracture, patients with a fracture and accompanying traumatic brain injury had higher serological levels of NPY and accelerated fracture healing process. This finding can be explained by the fact that NPY can directly promote osteogenic differentiation of MSCs[38]. Besides, Y1R antagonist play a direct role in regulation of BMSCs. Liu et al[53] noted that treatment with PD160170, a Y1R antagonist, promoted osteogenic differentiation of BMSCs, with higher expression of COL-I, OCN, and Runx2. The in vivo outcomes also showed increases in bone volume/total volume (BV/TV), bone mineral density, and bone trabeculae number after PD160170 intervention[53]. However, considering the still limited evidence from clinical investigations, more studies are necessary. In short, NPY can induce proliferation and angiogenic and osteogenic differentiation of BMSCs, facilitating bone regeneration.
VEGF is one of the most important components in angiogenesis, which is regarded as an essential factor that directly influences the fracture healing process[74]. BMSCs can promote vessel sprouting and vascularization, which is considered to be important for bone formation, whilst ECs can accelerate bone repair by facilitating the recruitment of osteoclast precursors and stimulating the osteoclastogenic process[75]. NPY can also facilitate vessel sprouting, adhesion, migration, proliferation, and capillary tube formation in ECs[10,59,65]. Also, during the process of angiogenesis, NPY receptors are indispensable. For example, Lee et al[67] observed that NPY-induced aortic sprouting and in vivo matrigel capillary formation were decreased by 50% after deleting Y2R gene or using its antagonists, implying the vital role of Y2R in angiogenesis. During the angiogenesis process, continuous nutrients and cytokines are transported to the fracture site, providing synergistic effects in fracture healing.
Osteoporosis, a disorder characterized by progressive bone loss and thus an increased risk of fracture, often results from menopausal loss of estrogen in women[76]. Currently, the primary methods to investigate the effects of NPY system on osteoporosis include examining bone phenotypes in gene knockout models and using NPY receptor antagonists.
Increasing number of studies indicated that Y2R is essential in medicating bone gain and loss. For example, mice lacking Y2R globally or specifically in the hypothalamus are characterized by greater bone loss compared to the WT controls, indicating that Y2R is critical in protection against bone loss[77,78]. In addition, ovariectomized mice injected with JNJ-31020028, a Y2R antagonist, showed increases in the whole-body bone mineral density, vertebral trabecular bone volume, and trabecular thickness[79] (Table 1). NPY3-36, an agonist of Y2R and Y5R, strongly lowered the expression level of receptor activator of Nfkb ligand (RANKL) and upregulated the basal levels of osteoprotegerin (OPG) in BMSCs, suggesting that Y2R may induce bone formation by affecting the expression of RANKL and OPG in BMSCs[40,41]. These results also hint that selective pharmacological manipulation of Y2R may be a potential strategy for anabolic treatment of osteoporosis.
| Antagonist | Bone phenotype | Administration and subjects |
| Y1R antagonist BIBP3226[56] | Callus tissue volume ↓, callus bone volume and callus ↓, BV/TV↓ | Intraperitoneal injection |
| Sprague-Dawley rats | ||
| Y2R antagonist JNJ-31020028[79] | Vertebral trabecular bone volume ↑, bone mineral density ↑, trabecular thickness ↑; P1NP and CTX biomarkers ↓ | Intraperitoneal injection |
| Ovariectomized Mice | ||
| Y1R antagonist BIBO3304[80] | Osteoblast activity ↑, cortical and cancellous bone volumes ↑; no adverse effects | Oral administration |
| Mice |
Aside from Y2R, Y1R may be also involved in regulation of bone homeostasis. Sousa et al[80] found that in mice, oral administration of BIBO3304, a Y1R antagonist, led to increased rates of mineral deposition in both cortical and cancellous bones, which may result from an increased number of osteoblasts following direct actions of NPY/Y1R on osteoclasts[80] (Table 1). Although there is still a lack of enough evidence to support the belief that NPY can improve the status of osteoporosis via direct regulations of BMSCs, based on the potential role of Y1R in osteogenic differentiation of BMSCs, it can be speculated that inhibition of Y1R may be a potential anabolic strategy for prevention of bone loss.
Nonetheless, other studies displayed different outcomes. Tang et al[56] reported that, compared with the controls, the rats treated with the Y1R antagonist BIBP3226 showed remarkable reductions in volumes of callus bone and tissue, and BV/TV as well. This demonstrates a potential negative effect of Y1R antagonist on bone healing (Table 1). Similarly, Sousa et al[44] also observed a lower rate of bone healing in Y1R (-/-) mice, with a decreased volume of bone callus and a weaker bone strength. Osteoclasts of hematopoietic origin also express high levels of NPY and Y1R[33]. Since osteoclasts are differentiated from HSCs, NPY can effectively alleviate ovariectomy-induced bone loss by decreasing the number of osteoclasts in bone marrow microenvironment through HSC mobilization, and increasing the number of osteoblasts as well[61]. These findings imply that NPY may act as a potential indicator of HSC mobilization, and supplementation of NPY may provide a therapeutic effect for bone loss.
Stem cells can provide preventive and regenerative effects in early stages of osteoarthritis[81]. Neurotransmitters, such as substance P (SP) and calcitonin gene-related peptide (CGRP), modulate osteo-chondrogenic differentiation of mesenchymal progenitor cells during endochondral ossification in limb development[82]. Guo et al[83] found that fracture- related pain in a rat model was partially relieved by an NK1 (substance P receptor) antagonist LY303870. In a rat knee model evaluating SP coupled with self-assembled peptide hydrogels, Kim et al[84] observed that cartilage regeneration and regenerative properties were markedly improved by recruiting MSCs. However, to date, few studies have addressed the role of NPY and its receptors in chondrocytes and their potential applications in osteoarthritis therapy.
One of the most frequent symptoms of osteoarthritis is pain of the affected joint, which associates with irritation of sensory nerve endings following pathological changes in the subchondral bone and synovial lining, with neuropeptide-containing nerves in the joint tissue as an important regulatory element[85,86]. NPY is able to bind to free nerve endings in accessory ligaments, synovium, subchondral bone, menisci, articular cartilage, and periosteum[87], and changes afferent sensitivity[88]. The visual analog scale (VAS) score, used to rate pain, was negatively correlated with the mean optical density values for NPY by immunohistochemical analysis in all patients with osteoarthritis, implying that NPY may be involved in the generation of pain[89]. Similarly, the mean level of CGRP in the synovial tissue of patients with severe osteoarthritis-related pain (VAS > 6) was significantly higher than that of patients with moderate to lower pain (VAS < 6)[90]. In another study, higher levels of CGRP were detected in the infrapatellar fat pad in patients with knee osteoarthritis, which is implicated as a possible cause of osteoarthritis development and related pain[91].
Traditionally, the rationale application of MSCs for management of osteoarthritis stems from their ability to differentiate into chondrogenic lineage rather than osteoblasts, which can help improve degeneration of the cartilage, and alleviate joint damage and related pain[92]. A decrease in the subchondral bone lesions may help reduce joint pain, which may be a future treatment target in relief of osteoarthritis-related pain[93]. Besides, NPY can increase the VEGF expression and promote osteoblastic differentiation and angiogenesis of BMSCs[38,51,55]. As cartilage does not contain blood vessels, it may be considered a hostile environment for spreading of vascular channels[82]. VEGF, a crucial regulator of angiogenesis, can induce tube formation activity into cartilage channels, likely resulting in calcification and stiffness of subchondral bone, accompanied by increased innervation and subsequent increases in nociceptors[94]. Therefore, blocking NPY could be of interest in pain treatment and osteoarthritis prevention.
Inflammation plays a crucial role in the pathogenesis of osteoarthritis. Prostaglandins are the key mediators of inflammation and pain in osteoarthritis[87]. NPY is considered to have pro-inflammatory effects. In a clinical study, Hernanz et al[95] found that the level of NPY in the synovial fluid of the knee joint in patients with rheumatoid arthritis was higher than the healthy controls, and NPY stimulated the expression of interleukin-1β (IL-1β), IL-6, and tumor necrosis factor-α (TNF-α). In a murine chondrogenic cell line, NPY was found to be able to promote proliferation and increase viable cell count of ATDC5 cells. Besides, the chondrogenic differentiation of ATDC5 can be enhanced by NPY via upregulating Runx2 and Col10a1. In the tissue engineering field, stem cell-scaffold-NPY combinations may be used to repair cartilage and tissues.
As mentioned previously, Y1R and Y2R antagonists have been applied to minimize the bone loss caused by different musculoskeletal disorders. Y1R and Y2R have been identified as novel therapeutic targets for the treatment of obesity and cancer[96,97]. Recently, a group of Y1R antagonists have been commercially available. Among these, BIBO3304, a Y1R antagonist, is the most potent[98]. However, the effect and efficacy of BIBO3304 have been only evaluated in animals, and clinical trials are required to confirm its role[56,79,80](Table 1).
This review introduces NPY and NPY receptors, and the potential mechanisms of actions of NPY on BMSCs, HSCs, ECs, and chondrocytes. NPY exerts different biological effects in different types of cells, including proliferation, apoptosis, differentiation, migration, mobilization, and cytokine secretion. NPY and its receptors play important roles in promoting bone union and anti-osteoporosis by regulating relative cell functions. Currently, limited studies have investigated the role of NPY in chondrocytes and its efficacy in controlling pain and inflammation in osteoarthritis. Improved clinical investigations addressing the role of NPY and its receptors in orthopaedic disorders may provide new insights into the stem cell research and therapy.
The authors are grateful to Dr. Song Y, from Nanfang Hospital, Southern Medical University for her help in figure preparation.
| 1. | Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev. 2012;40:4-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 607] [Article Influence: 43.4] [Reference Citation Analysis (0)] |
| 2. | Tatemoto K. Neuropeptide Y: complete amino acid sequence of the brain peptide. Proc Natl Acad Sci USA. 1982;79:5485-5489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 760] [Cited by in RCA: 739] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 3. | Lee NJ, Herzog H. NPY regulation of bone remodelling. Neuropeptides. 2009;43:457-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Apel PJ, Crane D, Northam CN, Callahan M, Smith TL, Teasdall RD. Effect of selective sensory denervation on fracture-healing: an experimental study of rats. J Bone Joint Surg Am. 2009;91:2886-2895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Lee NJ, Nguyen AD, Enriquez RF, Doyle KL, Sainsbury A, Baldock PA, Herzog H. Osteoblast specific Y1 receptor deletion enhances bone mass. Bone. 2011;48:461-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Peng S, Zhou YL, Song ZY, Lin S. Effects of Neuropeptide Y on Stem Cells and Their Potential Applications in Disease Therapy. Stem Cells Int. 2017;2017:6823917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Aerts-Kaya F, Ulum B, Mammadova A, Köse S, Aydin G, Korkusuz P, Uçkan-Çetinkaya D. Neurological Regulation of the Bone Marrow Niche. Adv Exp Med Biol. 2020;1212:127-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Wu J, Liu S, Meng H, Qu T, Fu S, Wang Z, Yang J, Jin D, Yu B. Neuropeptide Y enhances proliferation and prevents apoptosis in rat bone marrow stromal cells in association with activation of the Wnt/β-catenin pathway in vitro. Stem Cell Res. 2017;21:74-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Park MH, Jin HK, Min WK, Lee WW, Lee JE, Akiyama H, Herzog H, Enikolopov GN, Schuchman EH, Bae JS. Neuropeptide Y regulates the hematopoietic stem cell microenvironment and prevents nerve injury in the bone marrow. EMBO J. 2015;34:1648-1660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Movafagh S, Hobson JP, Spiegel S, Kleinman HK, Zukowska Z. Neuropeptide Y induces migration, proliferation, and tube formation of endothelial cells bimodally via Y1, Y2, and Y5 receptors. FASEB J. 2006;20:1924-1926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 104] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Im GI. Clinical use of stem cells in orthopaedics. Eur Cell Mater. 2017;33:183-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 12. | Luby AO, Ranganathan K, Lynn JV, Nelson NS, Donneys A, Buchman SR. Stem Cells for Bone Regeneration: Current State and Future Directions. J Craniofac Surg. 2019;30:730-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 13. | Eagan MJ, Zuk PA, Zhao KW, Bluth BE, Brinkmann EJ, Wu BM, McAllister DR. The suitability of human adipose-derived stem cells for the engineering of ligament tissue. J Tissue Eng Regen Med. 2012;6:702-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Lee SY, Kwon B, Lee K, Son YH, Chung SG. Therapeutic Mechanisms of Human Adipose-Derived Mesenchymal Stem Cells in a Rat Tendon Injury Model. Am J Sports Med. 2017;45:1429-1439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 65] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 15. | Sanghani-Kerai A, McCreary D, Lancashire H, Osagie L, Coathup M, Blunn G. Stem Cell Interventions for Bone Healing: Fractures and Osteoporosis. Curr Stem Cell Res Ther. 2018;13:369-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Saraf R, Mahmood F, Amir R, Matyal R. Neuropeptide Y is an angiogenic factor in cardiovascular regeneration. Eur J Pharmacol. 2016;776:64-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Reichmann F, Holzer P. Neuropeptide Y: A stressful review. Neuropeptides. 2016;55:99-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 348] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 18. | Mörl K, Beck-Sickinger AG. Intracellular Trafficking of Neuropeptide Y Receptors. Prog Mol Biol Transl Sci. 2015;132:73-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Horsnell H, Baldock PA. Osteoblastic Actions of the Neuropeptide Y System to Regulate Bone and Energy Homeostasis. Curr Osteoporos Rep. 2016;14:26-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Blomqvist AG, Herzog H. Y-receptor subtypes--how many more? Trends Neurosci. 1997;20:294-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 424] [Cited by in RCA: 414] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 21. | Gerald C, Walker MW, Criscione L, Gustafson EL, Batzl-Hartmann C, Smith KE, Vaysse P, Durkin MM, Laz TM, Linemeyer DL, Schaffhauser AO, Whitebread S, Hofbauer KG, Taber RI, Branchek TA, Weinshank RL. A receptor subtype involved in neuropeptide-Y-induced food intake. Nature. 1996;382:168-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 733] [Cited by in RCA: 698] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 22. | Khor EC, Yulyaningsih E, Driessler F, Kovaĉić N, Wee NKY, Kulkarni RN, Lee NJ, Enriquez RF, Xu J, Zhang L, Herzog H, Baldock PA. The y6 receptor suppresses bone resorption and stimulates bone formation in mice via a suprachiasmatic nucleus relay. Bone. 2016;84:139-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Baldock PA, Lee NJ, Driessler F, Lin S, Allison S, Stehrer B, Lin EJ, Zhang L, Enriquez RF, Wong IP, McDonald MM, During M, Pierroz DD, Slack K, Shi YC, Yulyaningsih E, Aljanova A, Little DG, Ferrari SL, Sainsbury A, Eisman JA, Herzog H. Neuropeptide Y knockout mice reveal a central role of NPY in the coordination of bone mass to body weight. PLoS One. 2009;4:e8415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 132] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 24. | Baldock PA, Sainsbury A, Allison S, Lin EJ, Couzens M, Boey D, Enriquez R, During M, Herzog H, Gardiner EM. Hypothalamic control of bone formation: distinct actions of leptin and y2 receptor pathways. J Bone Miner Res. 2005;20:1851-1857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 109] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 25. | Allison SJ, Baldock PA, Enriquez RF, Lin E, During M, Gardiner EM, Eisman JA, Sainsbury A, Herzog H. Critical interplay between neuropeptide Y and sex steroid pathways in bone and adipose tissue homeostasis. J Bone Miner Res. 2009;24:294-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 26. | Baldock PA, Sainsbury A, Couzens M, Enriquez RF, Thomas GP, Gardiner EM, Herzog H. Hypothalamic Y2 receptors regulate bone formation. J Clin Invest. 2002;109:915-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 128] [Article Influence: 5.3] [Reference Citation Analysis (1)] |
| 27. | Chen X, DiMaggio DA, Han SP, Westfall TC. Autoreceptor-induced inhibition of neuropeptide Y release from PC-12 cells is mediated by Y2 receptors. Am J Physiol. 1997;273:H1737-H1744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 38] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Broberger C, Landry M, Wong H, Walsh JN, Hökfelt T. Subtypes Y1 and Y2 of the neuropeptide Y receptor are respectively expressed in pro-opiomelanocortin- and neuropeptide-Y-containing neurons of the rat hypothalamic arcuate nucleus. Neuroendocrinology. 1997;66:393-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 233] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 29. | Allison SJ, Baldock P, Sainsbury A, Enriquez R, Lee NJ, Lin EJ, Klugmann M, During M, Eisman JA, Li M, Pan LC, Herzog H, Gardiner EM. Conditional deletion of hypothalamic Y2 receptors reverts gonadectomy-induced bone loss in adult mice. J Biol Chem. 2006;281:23436-23444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 30. | Sainsbury A, Baldock PA, Schwarzer C, Ueno N, Enriquez RF, Couzens M, Inui A, Herzog H, Gardiner EM. Synergistic effects of Y2 and Y4 receptors on adiposity and bone mass revealed in double knockout mice. Mol Cell Biol. 2003;23:5225-5233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 85] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 31. | Baldock PA, Allison SJ, Lundberg P, Lee NJ, Slack K, Lin EJ, Enriquez RF, McDonald MM, Zhang L, During MJ, Little DG, Eisman JA, Gardiner EM, Yulyaningsih E, Lin S, Sainsbury A, Herzog H. Novel role of Y1 receptors in the coordinated regulation of bone and energy homeostasis. J Biol Chem. 2007;282:19092-19102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 156] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 32. | Nunes AF, Liz MA, Franquinho F, Teixeira L, Sousa V, Chenu C, Lamghari M, Sousa MM. Neuropeptide Y expression and function during osteoblast differentiation--insights from transthyretin knockout mice. FEBS J. 2010;277:263-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Igwe JC, Jiang X, Paic F, Ma L, Adams DJ, Baldock PA, Pilbeam CC, Kalajzic I. Neuropeptide Y is expressed by osteocytes and can inhibit osteoblastic activity. J Cell Biochem. 2009;108:621-630. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 95] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 34. | Dong P, Gu X, Zhu G, Li M, Ma B, Zi Y. Melatonin Induces Osteoblastic Differentiation of Mesenchymal Stem Cells and Promotes Fracture Healing in a Rat Model of Femoral Fracture via Neuropeptide Y/Neuropeptide Y Receptor Y1 Signaling. Pharmacology. 2018;102:272-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 35. | Silva AP, Kaufmann JE, Vivancos C, Fakan S, Cavadas C, Shaw P, Brunner HR, Vischer U, Grouzmann E. Neuropeptide Y expression, localization and cellular transducing effects in HUVEC. Biol Cell. 2005;97:457-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 36. | Lee NJ, Doyle KL, Sainsbury A, Enriquez RF, Hort YJ, Riepler SJ, Baldock PA, Herzog H. Critical role for Y1 receptors in mesenchymal progenitor cell differentiation and osteoblast activity. J Bone Miner Res. 2010;25:1736-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 96] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 37. | Matic I, Matthews BG, Kizivat T, Igwe JC, Marijanovic I, Ruohonen ST, Savontaus E, Adams DJ, Kalajzic I. Bone-specific overexpression of NPY modulates osteogenesis. J Musculoskelet Neuronal Interact. 2012;12:209-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 38. | Gu XC, Zhang XB, Hu B, Zi Y, Li M. Neuropeptide Y accelerates post-fracture bone healing by promoting osteogenesis of mesenchymal stem cells. Neuropeptides. 2016;60:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 39. | Liao KH, Wang JY, Lin HW, Lui TN, Chen KY, Yen DH, Jeng MJ. Risk of death in patients with post-traumatic cerebrospinal fluid leakage--analysis of 1773 cases. J Chin Med Assoc. 2016;79:58-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 40. | Amano S, Arai M, Goto S, Togari A. Inhibitory effect of NPY on isoprenaline-induced osteoclastogenesis in mouse bone marrow cells. Biochim Biophys Acta. 2007;1770:966-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 41. | Teixeira L, Sousa DM, Nunes AF, Sousa MM, Herzog H, Lamghari M. NPY revealed as a critical modulator of osteoblast function in vitro: new insights into the role of Y1 and Y2 receptors. J Cell Biochem. 2009;107:908-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 42. | Igura K, Haider HKh, Ahmed RP, Sheriff S, Ashraf M. Neuropeptide y and neuropeptide y y5 receptor interaction restores impaired growth potential of aging bone marrow stromal cells. Rejuvenation Res. 2011;14:393-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 43. | Lundberg P, Allison SJ, Lee NJ, Baldock PA, Brouard N, Rost S, Enriquez RF, Sainsbury A, Lamghari M, Simmons P, Eisman JA, Gardiner EM, Herzog H. Greater bone formation of Y2 knockout mice is associated with increased osteoprogenitor numbers and altered Y1 receptor expression. J Biol Chem. 2007;282:19082-19091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 111] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 44. | Sousa DM, McDonald MM, Mikulec K, Peacock L, Herzog H, Lamghari M, Little DG, Baldock PA. Neuropeptide Y modulates fracture healing through Y1 receptor signaling. J Orthop Res. 2013;31:1570-1578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 45. | Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop Dj, Horwitz E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11055] [Cited by in RCA: 13031] [Article Influence: 685.8] [Reference Citation Analysis (12)] |
| 46. | L PK, Kandoi S, Misra R, S V, K R, Verma RS. The mesenchymal stem cell secretome: A new paradigm towards cell-free therapeutic mode in regenerative medicine. Cytokine Growth Factor Rev. 2019;46:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 337] [Article Influence: 48.1] [Reference Citation Analysis (0)] |
| 47. | Sheyn D, Shapiro G, Tawackoli W, Jun DS, Koh Y, Kang KB, Su S, Da X, Ben-David S, Bez M, Yalon E, Antebi B, Avalos P, Stern T, Zelzer E, Schwarz EM, Gazit Z, Pelled G, Bae HM, Gazit D. PTH Induces Systemically Administered Mesenchymal Stem Cells to Migrate to and Regenerate Spine Injuries. Mol Ther. 2016;24:318-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 48. | Maiti SK, Shivakumar MU, Mohan D, Kumar N, Singh KP. Mesenchymal Stem Cells of Different Origin-Seeded Bioceramic Construct in Regeneration of Bone Defect in Rabbit. Tissue Eng Regen Med. 2018;15:477-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 49. | Son MY, Kim MJ, Yu K, Koo DB, Cho YS. Involvement of neuropeptide Y and its Y1 and Y5 receptors in maintaining self-renewal and proliferation of human embryonic stem cells. J Cell Mol Med. 2011;15:152-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 50. | Wang Y, Zhang D, Ashraf M, Zhao T, Huang W, Ashraf A, Balasubramaniam A. Combining neuropeptide Y and mesenchymal stem cells reverses remodeling after myocardial infarction. Am J Physiol Heart Circ Physiol. 2010;298:H275-H286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 51. | Liu S, Jin D, Wu JQ, Xu ZY, Fu S, Mei G, Zou ZL, Ma SH. Neuropeptide Y stimulates osteoblastic differentiation and VEGF expression of bone marrow mesenchymal stem cells related to canonical Wnt signaling activating in vitro. Neuropeptides. 2016;56:105-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 52. | Wee NKY, Sinder BP, Novak S, Wang X, Stoddard C, Matthews BG, Kalajzic I. Skeletal phenotype of the neuropeptide Y knockout mouse. Neuropeptides. 2019;73:78-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 53. | Liu S, Wu JQ, Hu JJ, Wang L, Wang Z, Meng H, Zhuo LJ, Zheng JX. [Neuropeptide Y Y1 receptor antagonist PD160170 promotes osteogenic differentiation of rat bone marrow mesenchymal stem cells in vitro and femoral defect repair in rats]. Nan Fang Yi Ke Da Xue Xue Bao. 2018;38:669-676. [PubMed] |
| 54. | Yahara M, Tei K, Tamura M. Inhibition of neuropeptide Y Y1 receptor induces osteoblast differentiation in MC3T3-E1 cells. Mol Med Rep. 2017;16:2779-2784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 55. | Ma WH, Liu YJ, Wang W, Zhang YZ. Neuropeptide Y, substance P, and human bone morphogenetic protein 2 stimulate human osteoblast osteogenic activity by enhancing gap junction intercellular communication. Braz J Med Biol Res. 2015;48:299-307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 56. | Tang P, Duan C, Wang Z, Wang C, Meng G, Lin K, Yang Q, Yuan Z. NPY and CGRP Inhibitor Influence on ERK Pathway and Macrophage Aggregation during Fracture Healing. Cell Physiol Biochem. 2017;41:1457-1467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 57. | Sharma R, Wu X, Rhodes SD, Chen S, He Y, Yuan J, Li J, Yang X, Li X, Jiang L, Kim ET, Stevenson DA, Viskochil D, Xu M, Yang FC. Hyperactive Ras/MAPK signaling is critical for tibial nonunion fracture in neurofibromin-deficient mice. Hum Mol Genet. 2013;22:4818-4828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 58. | Park MH, Min WK, Jin HK, Bae JS. Role of neuropeptide Y in the bone marrow hematopoietic stem cell microenvironment. BMB Rep. 2015;48:645-646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 59. | Singh P, Hoggatt J, Kamocka MM, Mohammad KS, Saunders MR, Li H, Speth J, Carlesso N, Guise TA, Pelus LM. Neuropeptide Y regulates a vascular gateway for hematopoietic stem and progenitor cells. J Clin Invest. 2017;127:4527-4540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 60. | Ulum B, Mammadova A, Özyüncü Ö, Uçkan-Çetinkaya D, Yanık T, Aerts-Kaya F. Neuropeptide Y is involved in the regulation of quiescence of hematopoietic stem cells. Neuropeptides. 2020;80:102029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 61. | Park MH, Lee JK, Kim N, Min WK, Lee JE, Kim KT, Akiyama H, Herzog H, Schuchman EH, Jin HK, Bae JS. Neuropeptide Y Induces Hematopoietic Stem/Progenitor Cell Mobilization by Regulating Matrix Metalloproteinase-9 Activity Through Y1 Receptor in Osteoblasts. Stem Cells. 2016;34:2145-2156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 62. | Park MH, Kim N, Jin HK, Bae JS. Neuropeptide Y-based recombinant peptides ameliorate bone loss in mice by regulating hematopoietic stem/progenitor cell mobilization. BMB Rep. 2017;50:138-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 63. | Szczesny G. Molecular aspects of bone healing and remodeling. Pol J Pathol. 2002;53:145-153. [PubMed] |
| 64. | Alves CJ, Alencastre IS, Neto E, Ribas J, Ferreira S, Vasconcelos DM, Sousa DM, Summavielle T, Lamghari M. Bone Injury and Repair Trigger Central and Peripheral NPY Neuronal Pathways. PLoS One. 2016;11:e0165465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 65. | Zukowska-Grojec Z, Karwatowska-Prokopczuk E, Rose W, Rone J, Movafagh S, Ji H, Yeh Y, Chen WT, Kleinman HK, Grouzmann E, Grant DS. Neuropeptide Y: a novel angiogenic factor from the sympathetic nerves and endothelium. Circ Res. 1998;83:187-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 285] [Article Influence: 10.2] [Reference Citation Analysis (13)] |
| 66. | Kuo LE, Kitlinska JB, Tilan JU, Li L, Baker SB, Johnson MD, Lee EW, Burnett MS, Fricke ST, Kvetnansky R, Herzog H, Zukowska Z. Neuropeptide Y acts directly in the periphery on fat tissue and mediates stress-induced obesity and metabolic syndrome. Nat Med. 2007;13:803-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 464] [Cited by in RCA: 469] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 67. | Lee EW, Grant DS, Movafagh S, Zukowska Z. Impaired angiogenesis in neuropeptide Y (NPY)-Y2 receptor knockout mice. Peptides. 2003;24:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 64] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 68. | Businaro R, Scaccia E, Bordin A, Pagano F, Corsi M, Siciliano C, Capoano R, Procaccini E, Salvati B, Petrozza V, Totta P, Vietri MT, Frati G, De Falco E. Platelet Lysate-Derived Neuropeptide y Influences Migration and Angiogenesis of Human Adipose Tissue-Derived Stromal Cells. Sci Rep. 2018;8:14365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 69. | Zhang LF, Qi J, Zuo G, Jia P, Shen X, Shao J, Kang H, Yang H, Deng L. Osteoblast-secreted factors promote proliferation and osteogenic differentiation of bone marrow stromal cells via VEGF/heme-oxygenase-1 pathway. PLoS One. 2014;9:e99946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 70. | Duffy GP, Ahsan T, O'Brien T, Barry F, Nerem RM. Bone marrow-derived mesenchymal stem cells promote angiogenic processes in a time- and dose-dependent manner in vitro. Tissue Eng Part A. 2009;15:2459-2470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 114] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 71. | Kang X, Qian Z, Liu J, Feng D, Li H, Zhang Z, Jin X, Ma Z, Xu M, Li F, Zhang Y, Gao X, Sun H, Wu S. Neuropeptide Y Acts Directly on Cartilage Homeostasis and Exacerbates Progression of Osteoarthritis Through NPY2R. J Bone Miner Res. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 72. | Chen R, Hao Z, Chen X, Fu Q, Ma Y. Neuropeptide Y enhances proliferation and chondrogenic differentiation of ATDC5 cells. Neuropeptides. 2020;80:102022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 73. | Long H, Ahmed M, Ackermann P, Stark A, Li J. Neuropeptide Y innervation during fracture healing and remodeling. A study of angulated tibial fractures in the rat. Acta Orthop. 2010;81:639-646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 74. | Keramaris NC, Calori GM, Nikolaou VS, Schemitsch EH, Giannoudis PV. Fracture vascularity and bone healing: a systematic review of the role of VEGF. Injury. 2008;39 Suppl 2:S45-S57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 230] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 75. | Cui Y, Fu S, Hou T, Wu X. Endothelial Progenitor Cells Enhance the Migration and Osteoclastic Differentiation of Bone Marrow-Derived Macrophages in vitro and in a Mouse Femur Fracture Model through Talin-1. Cell Physiol Biochem. 2018;49:555-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 76. | Hart EC, Charkoudian N. Sympathetic neural regulation of blood pressure: influences of sex and aging. Physiology (Bethesda). 2014;29:8-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 77. | Baldock PA, Lin S, Zhang L, Karl T, Shi Y, Driessler F, Zengin A, Hörmer B, Lee NJ, Wong IP, Lin EJ, Enriquez RF, Stehrer B, During MJ, Yulyaningsih E, Zolotukhin S, Ruohonen ST, Savontaus E, Sainsbury A, Herzog H. Neuropeptide y attenuates stress-induced bone loss through suppression of noradrenaline circuits. J Bone Miner Res. 2014;29:2238-2249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 78. | Baldock PA, Allison S, McDonald MM, Sainsbury A, Enriquez RF, Little DG, Eisman JA, Gardiner EM, Herzog H. Hypothalamic regulation of cortical bone mass: opposing activity of Y2 receptor and leptin pathways. J Bone Miner Res. 2006;21:1600-1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 84] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 79. | Seldeen KL, Halley PG, Volmar CH, Rodríguez MA, Hernandez M, Pang M, Carlsson SK, Suva LJ, Wahlestedt C, Troen BR, Brothers SP. Neuropeptide Y Y2 antagonist treated ovariectomized mice exhibit greater bone mineral density. Neuropeptides. 2018;67:45-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 80. | Sousa DM, Baldock PA, Enriquez RF, Zhang L, Sainsbury A, Lamghari M, Herzog H. Neuropeptide Y Y1 receptor antagonism increases bone mass in mice. Bone. 2012;51:8-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 81. | Goldberg A, Mitchell K, Soans J, Kim L, Zaidi R. The use of mesenchymal stem cells for cartilage repair and regeneration: a systematic review. J Orthop Surg Res. 2017;12:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 171] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 82. | Grässel SG. The role of peripheral nerve fibers and their neurotransmitters in cartilage and bone physiology and pathophysiology. Arthritis Res Ther. 2014;16:485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 174] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 83. | Guo TZ, Offley SC, Boyd EA, Jacobs CR, Kingery WS. Substance P signaling contributes to the vascular and nociceptive abnormalities observed in a tibial fracture rat model of complex regional pain syndrome type I. Pain. 2004;108:95-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 152] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 84. | Kim SJ, Kim JE, Kim SH, Kim SJ, Jeon SJ, Kim SH, Jung Y. Therapeutic effects of neuropeptide substance P coupled with self-assembled peptide nanofibers on the progression of osteoarthritis in a rat model. Biomaterials. 2016;74:119-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 85. | Dirmeier M, Capellino S, Schubert T, Angele P, Anders S, Straub RH. Lower density of synovial nerve fibres positive for calcitonin gene-related peptide relative to substance P in rheumatoid arthritis but not in osteoarthritis. Rheumatology (Oxford). 2008;47:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 86. | Mapp PI, Walsh DA. Mechanisms and targets of angiogenesis and nerve growth in osteoarthritis. Nat Rev Rheumatol. 2012;8:390-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 462] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 87. | Witt KL, Vilensky JA. The anatomy of osteoarthritic joint pain. Clin Anat. 2014;27:451-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 88. | Grässel S, Muschter D. Peripheral Nerve Fibers and Their Neurotransmitters in Osteoarthritis Pathology. Int J Mol Sci. 2017;18:931. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 89. | Xiao J, Yu W, Wang X, Wang B, Chen J, Liu Y, Li Z. Correlation between neuropeptide distribution, cancellous bone microstructure and joint pain in postmenopausal women with osteoarthritis and osteoporosis. Neuropeptides. 2016;56:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 90. | Takano S, Uchida K, Inoue G, Minatani A, Miyagi M, Aikawa J, Iwase D, Onuma K, Mukai M, Takaso M. Increase and regulation of synovial calcitonin gene-related peptide expression in patients with painful knee osteoarthritis. J Pain Res. 2017;10:1099-1104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 91. | Aikawa J, Uchida K, Takano S, Inoue G, Minatani A, Miyagi M, Iwase D, Sekiguchi H, Mukai M, Takaso M. Expression of calcitonin gene-related peptide in the infrapatellar fat pad in knee osteoarthritis patients. J Orthop Surg Res. 2017;12:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 92. | Jayaram P, Ikpeama U, Rothenberg JB, Malanga GA. Bone Marrow-Derived and Adipose-Derived Mesenchymal Stem Cell Therapy in Primary Knee Osteoarthritis: A Narrative Review. PM R. 2019;11:177-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 93. | Gatenholm B, Brittberg M. Neuropeptides: important regulators of joint homeostasis. Knee Surg Sports Traumatol Arthrosc. 2019;27:942-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 94. | Bonnet CS, Walsh DA. Osteoarthritis, angiogenesis and inflammation. Rheumatology (Oxford). 2005;44:7-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 484] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 95. | Hernanz A, Tato E, De la Fuente M, de Miguel E, Arnalich F. Differential effects of gastrin-releasing peptide, neuropeptide Y, somatostatin and vasoactive intestinal peptide on interleukin-1 beta, interleukin-6 and tumor necrosis factor-alpha production by whole blood cells from healthy young and old subjects. J Neuroimmunol. 1996;71:25-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 65] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 96. | Yulyaningsih E, Zhang L, Herzog H, Sainsbury A. NPY receptors as potential targets for anti-obesity drug development. Br J Pharmacol. 2011;163:1170-1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 113] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 97. | Ailanen L, Vähätalo LH, Salomäki-Myftari H, Mäkelä S, Orpana W, Ruohonen ST, Savontaus E. Peripherally Administered Y2-Receptor Antagonist BIIE0246 Prevents Diet-Induced Obesity in Mice With Excess Neuropeptide Y, but Enhances Obesity in Control Mice. Front Pharmacol. 2018;9:319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 98. | Dailey MJ, Bartness TJ. Appetitive and consummatory ingestive behaviors stimulated by PVH and perifornical area NPY injections. Am J Physiol Regul Integr Comp Physiol. 2009;296:R877-R892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited manuscript
Specialty type: Cell and tissue engineering
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Emara KM S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Xing YX