Copyright
©The Author(s) 2021.
World J Stem Cells. Oct 26, 2021; 13(10): 1480-1512
Published online Oct 26, 2021. doi: 10.4252/wjsc.v13.i10.1480
Published online Oct 26, 2021. doi: 10.4252/wjsc.v13.i10.1480
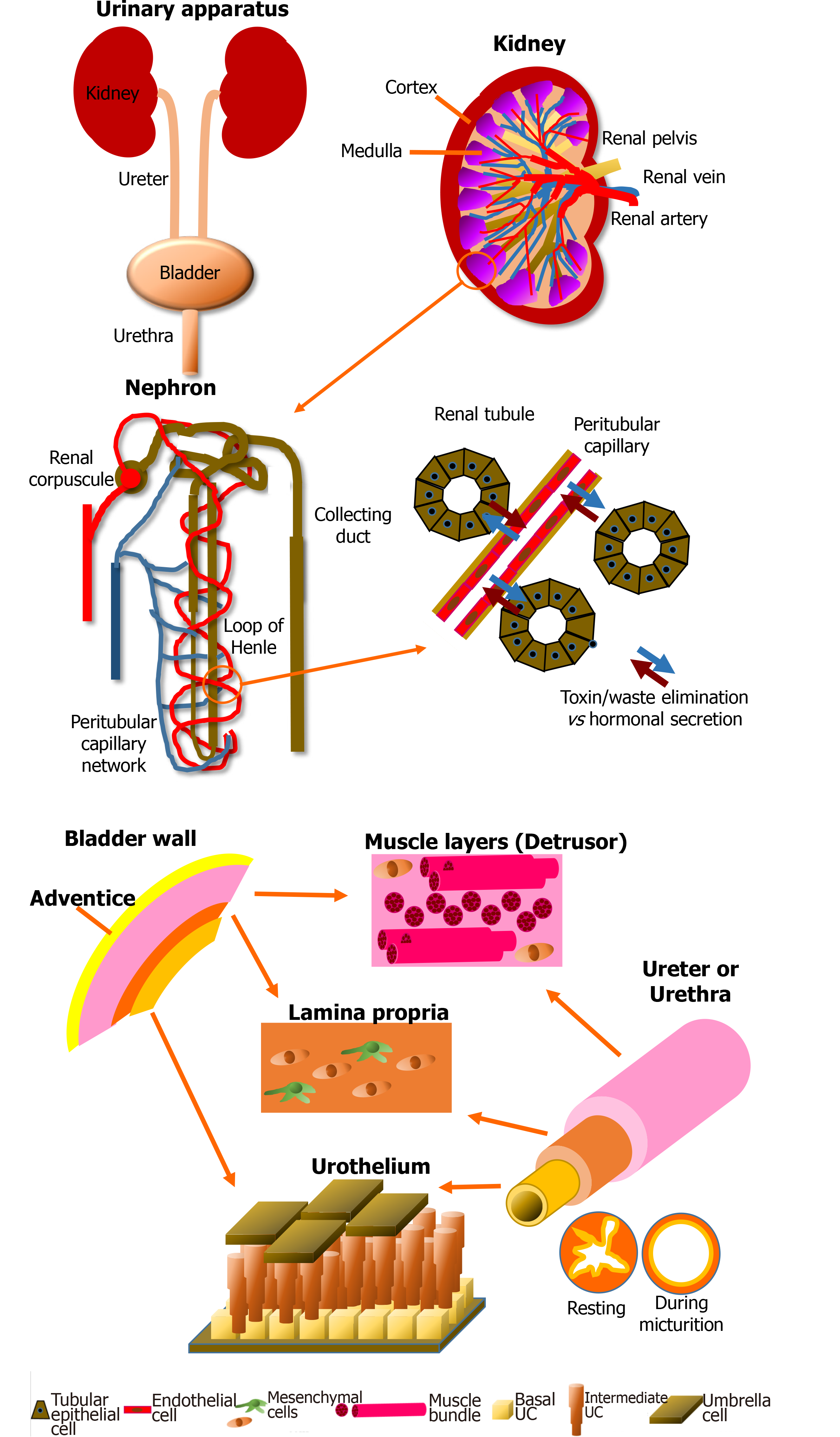
Figure 1 Schematic of the anatomy of the urinary apparatus.
Kidney: Kidneys are the blood filtration unit of the body, extracting toxins and metabolic waste to produce the urine purifying 180 L of blood every day. The nephron is the element which allows exchange between blood and urine through the renal tubules and the capillaries. Another role of the kidney is the regulation of the water balance when the body is sweating or in the presence of abundant/inadequate hydration by reabsorption of components during blood filtration. Kidneys also produce hormones essential for blood pressure regulation, such as renin, which will cause, via angiotensin II, stimulation of the secretion of aldosterone. Finally, 90% of the erythropoietin is secreted by this organ. This glycoprotein stimulates the proliferation and differentiation of erythrocyte precursors. Pathologies can impair these functions and endanger the patient’s life. Bladder: The central role of the bladder is to receive and dynamically store the urine produced by the kidneys through structural and regulatory mechanisms. The urine is brought to the bladder via the ureters. The bladder is also a complex organ composed of various layers. It is described from its outer surface to the lumen with the adventice (layer of fatty tissue), the detrusor muscle, the lamina propria (a connective tissue including a muscularis mucosae) and the epithelium, which is named the urothelium. The latter can be divided in three layers: basal, intermediate and superficial (umbrella). The impermeability is due to a thin asymmetric unitary membrane of uroplakin, expressed at the apical surface of mature urothelial cells called umbrella cells. Ureter and urethra: Ureters and urethra share a common primary role: to transport urine, allowing its excretion outside of the body. Anatomic organization of these organs are histologically related to the bladder due to their similar protective role against urine through the urothelial cell layers. From the inside to the outside, these two organs are composed of the transitional urothelial cell layer, a submucosa comprising fibroblasts and extracellular matrix, especially type I and III collagens, a muscular cell layer of smooth muscle cells, and an adventitia surrounding the organ. During the micturition, the star-shaped configuration of the urethra allows to compensate the increase in pressure. The muscular layers also play a critical role in the maintenance of the tubular shape.
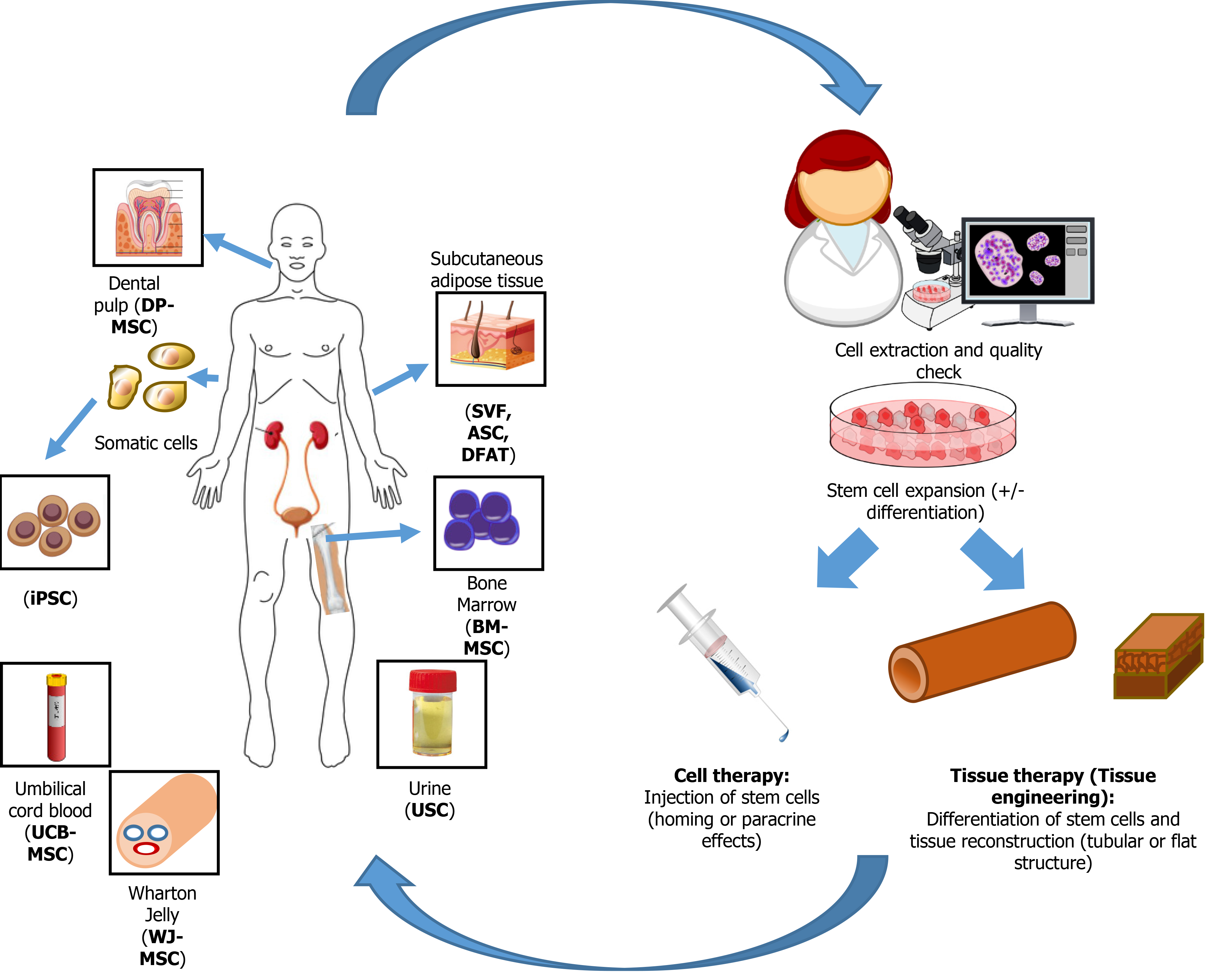
Figure 2 Source of stem cells used for genitourinary regenerative medicine.
After extraction from various tissues, stem cells are expanded and eventually differentiated, depending on their origin, before to be reinjected to the patients or used to reconstruct genitourinary engineered tissues. DP-MSC: Dental pulp-mesenchymal stem cells; BM-MSC: Bone marrow-mesenchymal stem cells; iPSC: Induced pluripotent stem cells; SVF: Stromal vascular fraction; ASC: Adipose-derived stromal/stem cells; DFAT: Dedifferentiated fat; UCB-MSC: Umbilical cord blood-mesenchymal stem cells; WJ-MSC: Wharton Jelly-mesenchymal stem cells.
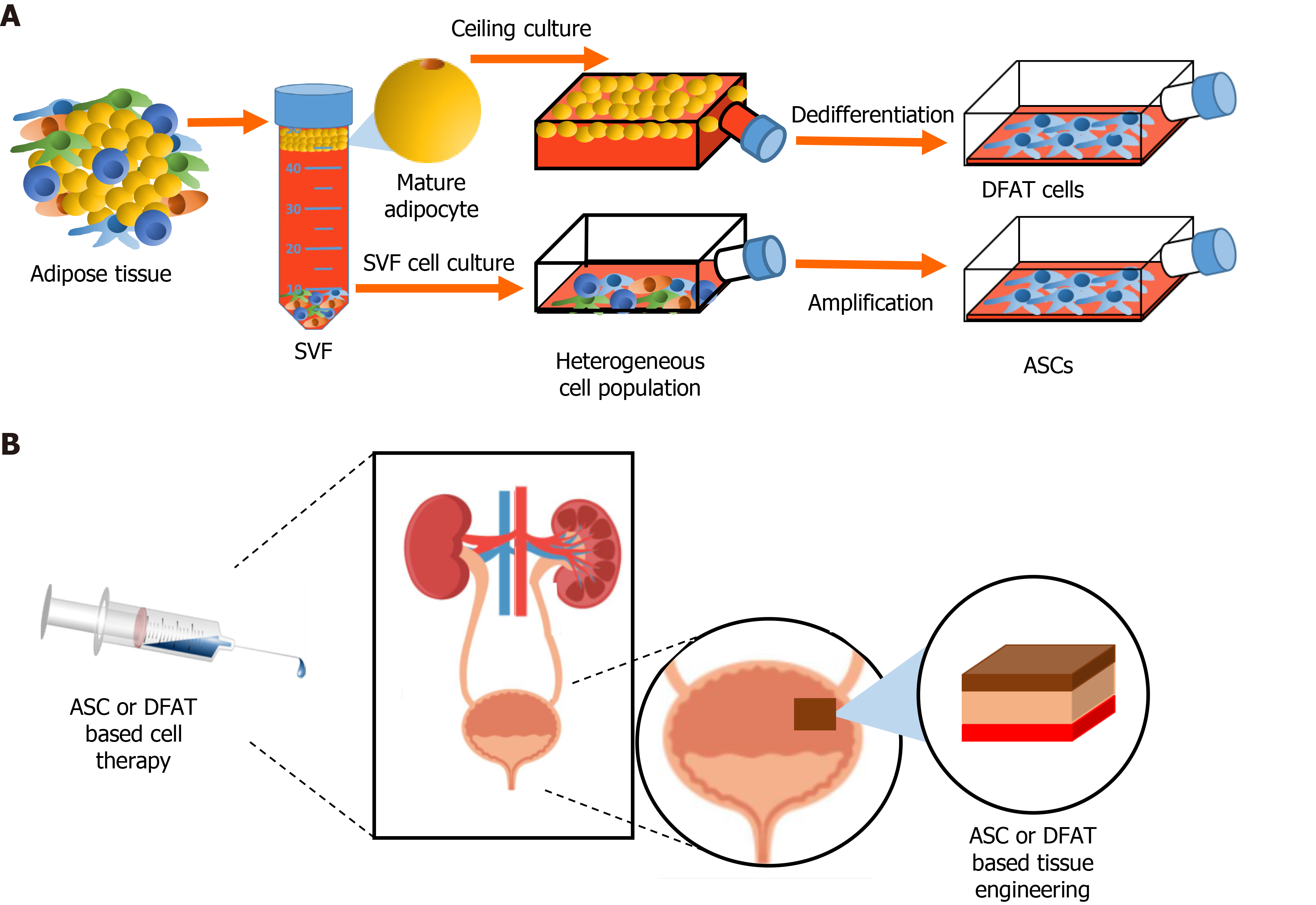
Figure 3 Stem cells from adipose tissue in regenerative medicine.
A: Extraction of the stromal vascular fraction from adipose tissue and obtention of adipose-derived stromal/stem cells (ASCs) after cell culture. Ceiling culture of mature adipocytes and resulting populations of dedifferentiated fat (DFAT) cells; B: Potential uses of ASCs and/or DFAT cell-based therapies in genitourinary regenerative medicine. SVF: Stromal vascular fraction; ASC: Adipose-derived stromal/stem cells; DFAT: Dedifferentiated fat.
- Citation: Caneparo C, Sorroza-Martinez L, Chabaud S, Fradette J, Bolduc S. Considerations for the clinical use of stem cells in genitourinary regenerative medicine. World J Stem Cells 2021; 13(10): 1480-1512
- URL: https://www.wjgnet.com/1948-0210/full/v13/i10/1480.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v13.i10.1480