Published online Nov 7, 2025. doi: 10.3748/wjg.v31.i41.111022
Revised: August 3, 2025
Accepted: September 29, 2025
Published online: November 7, 2025
Processing time: 138 Days and 20.8 Hours
Balloon-assisted enteroscopy with a specialized overtube has improved the suc
To compare the ERCP-related outcomes between DBE and SBE in patients with SAA.
We retrospectively reviewed the medical records of 1042 patients with SAA who underwent ERCP. After propensity score matching for age and sex, 494 patients were included, with 247 patients in each of the SBE and DBE groups.
The success rates of intubation, cannulation, completion of intended ERCP, and adverse events were similar between the DBE and SBE groups (94.3% vs 96.4%, P = 0.393; 89.5% vs 93.5%, P = 0.147; 88.3% vs 92.7%, P = 0.125; 10.5% vs 14.6%, P = 0.222, respectively). However, the SBE group had significantly longer intubation and procedure times than the DBE group (23.5 ± 22.3 minutes vs 14.1 ± 13.5 mi
DBE and SBE showed comparable clinical success and safety profiles in ERCP for patients with SAA, although SBE required significantly longer procedure times. DBE could provide procedural efficiency benefits in cases where an extended procedure duration is expected. Furthermore, a preserved gastric anatomy and Roux-en-Y reconstruction were identified as independent risk factors for intuba
Core Tip: This multicenter retrospective study compared the performance of double-balloon enteroscopy (DBE) and single-balloon enteroscopy for enteroscope-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy. While both techniques showed comparable success and adverse event rates, DBE demonstrated significantly shorter intubation and total procedure times. Further
- Citation: Han SY, Yang MJ, Lee KJ, Lee J, Park SW. Comparison of clinical outcomes for single- and double-balloon enteroscope-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy. World J Gastroenterol 2025; 31(41): 111022
- URL: https://www.wjgnet.com/1007-9327/full/v31/i41/111022.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i41.111022
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with surgically altered anatomy (SAA) is technically challenging because of the complexity of the reconstructed gastrointestinal tract. Additionally, the increasing use of alternative modalities, such as percutaneous or endoscopic ultrasound-guided interventions, with comparable or favorable outcomes has further complicated the role of ERCP in this patient population[1]. Although no standardized technique exists, balloon-assisted enteroscopy has enhanced ERCP success in patients with altered anatomy by allowing deep intubation and access to the small bowel[2,3]. The main challenges are: (1) Intu
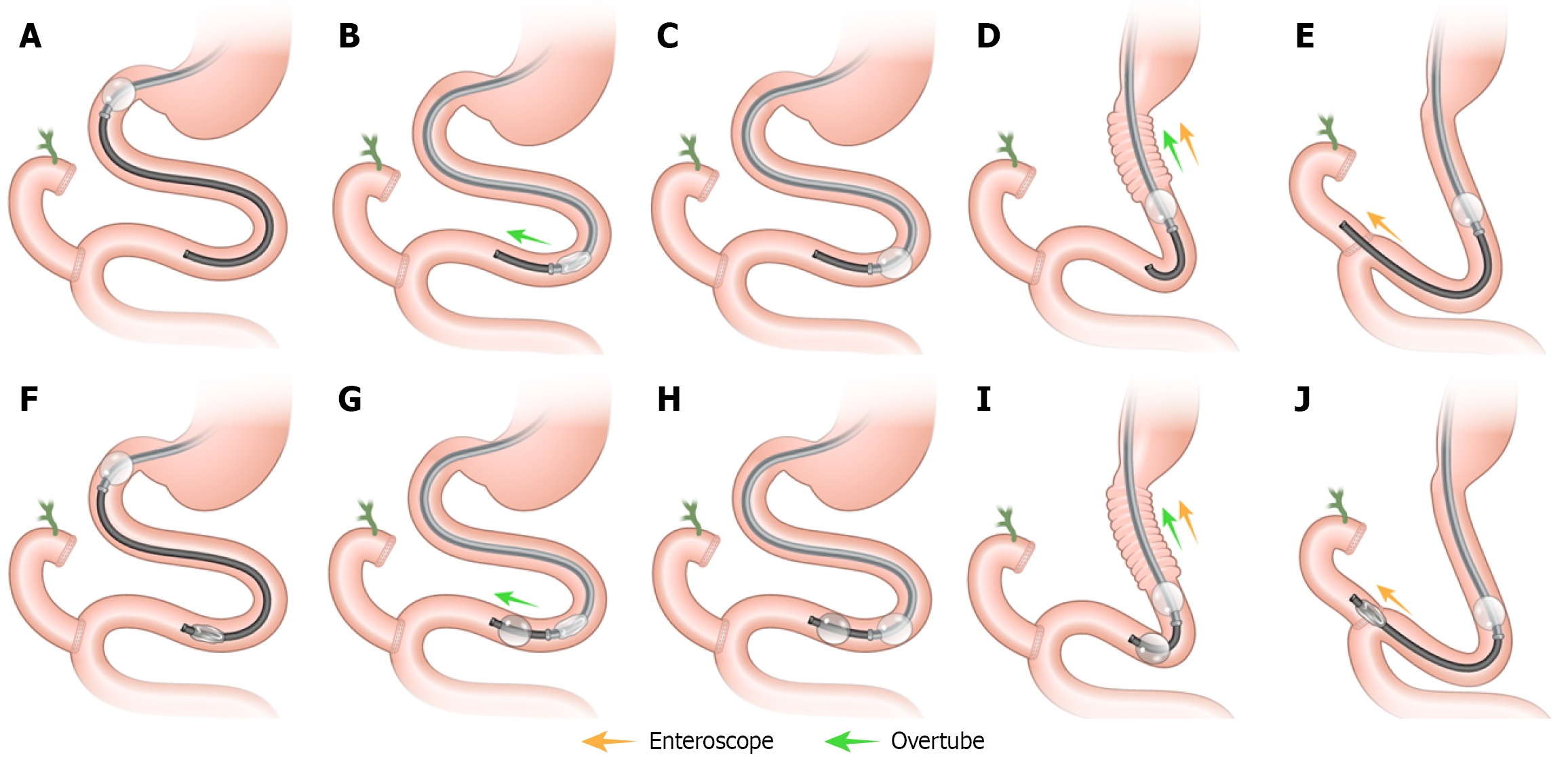
For scope selection, the DBE, equipped with independently inflatable balloons at the tip of the scope and overtube, facilitates deep advancement into the small bowel via alternating balloon inflation and deflation, along with stepwise insertion of the endoscope and overtube[5]. DBE offers deep access, even in Roux-en-Y anatomy, with improved stability and forward-view visualization[6]. However, its long length can lead to looping, reduced maneuverability, and difficult cannulation due to the absence of an elevator[4]. Additionally, long DBE is incompatible with standard ERCP devices, often requiring a scope exchange for therapeutic interventions[7]. Recently, a short DBE has overcome some of these limitations through a 3.2-mm working channel model. In contrast, a SBE features a single inflatable balloon located at the tip of the overtube. The SBE operates based on an alternating sequence of scope advancement and reduction, which progressively shortens and gathers the small bowel onto the overtube, enabling deeper insertion[8].
Several studies have demonstrated no significant differences in overall success or adverse events (AEs) rates between DBE- and SBE-assisted ERCP. In a study by De Koning and Moreels[5], the overall ERCP success rates were 73% for DBE and 75% for SBE, with no statistically significant difference. Similarly, Katanuma and Isayama[4] reported comparable intubation success rates between DBE and SBE in patients with Billroth II reconstruction. However, DBE was associated with a higher success rate in patients who underwent Roux-en-Y reconstruction (94.7% vs 85.1%). However, owing to the technical complexity of these procedures, direct head-to-head comparative studies evaluating DBE and SBE in ERCP for patients with SAA remain limited. This study aimed to provide a comprehensive comparison of the clinical outcomes of DBE and SBE in this population.
This propensity score-matched multicenter retrospective study compared the clinical outcomes of SBE- and DBE-assisted ERCP in patients with SAA. Data were collected from three high-volume tertiary referral hospitals in South Korea, including patients who underwent enteroscope-assisted ERCP between April 2018 and December 2024. Patient data were retrospectively reviewed using electronic medical records, procedural images, and the corresponding reports. Relevant clinical information, including demographics, ERCP indications, technical success rates, procedural AEs, and overall clinical outcomes were extracted and anonymized for analysis. The study adhered to the ethical guidelines of the Declaration of Helsinki and received approval from the Institutional Review Boards of each participating hospital (representative institution: Hallym University Hospital, No. 2022-04-008).
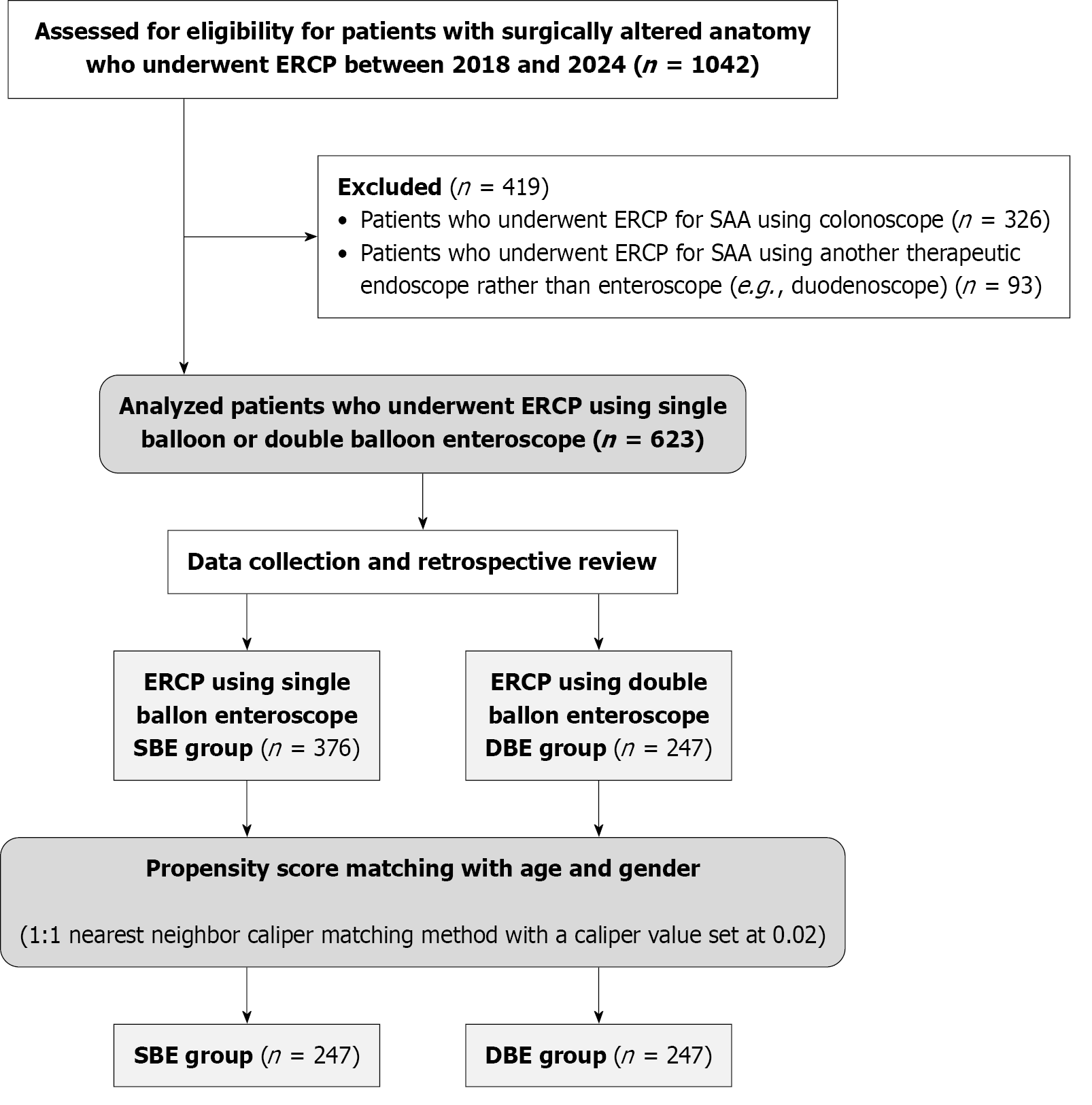
A total of 1042 patients with SAA who underwent ERCP during study period were assessed for eligibility (Figure 1). After data collection and retrospective review, 419 patients were excluded: 326 patients who underwent ERCP using a colonoscope and 93 who underwent ERCP with other non-enteroscopic therapeutic endoscopes, such as a duodenoscope. The remaining 623 patients were reviewed, with 247 in the DBE group and 376 in the SBE group. A comparison of the baseline characteristics between the two groups showed significant differences in age (DBE vs SBE: 66.7 ± 15.3 vs 70.6 ± 10.7, P < 0.001) and sex distribution (male ratio: 61.6% vs 74.7%, P = 0.001). To account for these differences, propensity score matching (PSM) was conducted, resulting in a final cohort of 247 matched patients in each group for further analyses.
The primary endpoint was the overall technical success rate, defined as successful intubation followed by successful cannulation and therapeutic intervention. The secondary endpoints included the technical success rate in the first endoscopic session, procedure-AEs, and risk factors associated with intubation failure and AEs. Intubation success was defined as the successful advancement of the enteroscope to the target site, such as the native papilla or biliopancreatoenteric anastomosis. Selective cannulation success referred to successful ductal cannulation and acquisition of cholangiopancreatography in cases of successful intubation. Overall technical success was defined as the completion of all procedural steps, including intubation, selective cannulation, and the intended therapeutic intervention (e.g., stone extraction or stent placement)[9]. Total technical failure was defined as the inability to complete the procedure at any stage, from endoscope intubation to the intended therapeutic intervention[10]. In cases of initial failure, the final success rate included outcomes from subsequent attempts. Intubation time was defined as the interval from endoscope insertion to arrival at the target site[7]. Total procedure time was measured from endoscope insertion to withdrawal[11]. The parameter “intubation to jejunojejunostomy (JJstomy) time” was defined only for patients with a JJstomy (e.g., Roux-en-Y or Braun anastomosis). Cases without a JJstomy, such as Billroth II reconstruction, were excluded from this specific analysis. AEs, including post-procedure pancreatitis, perforation, bleeding, and cholangitis, were classified and graded according to the severity grading system of the American Society for Gastrointestinal Endoscopy lexicon[12].
In this study, surgical anatomy was categorized as follows: (1) Bile duct resection (BDR) with Roux-en-Y reconstruc
During the study period, three endoscopists independently performed the procedures, each with an annual volume of more than 1000 ERCP. ERCP procedures were conducted by experienced endoscopist at each institution using either a SBE (Olympus SIF-H290S, Olympus Medical Systems, Tokyo, Japan) or a DBE (Fujifilm EI-580BT, Fujifilm, Tokyo, Japan). The choice of DBE or SBE was not determined by patient- or procedure-related factors but by the availability of equipment at each institution. One center used the DBE system exclusively, while the other two centers used the SBE system. Therefore, the selection of enteroscope was institution-driven rather than based on operator discretion. Deep sedation was maintained using a combination of midazolam and propofol[13]. Carbon dioxide insufflation was used during the ERCP procedure at a rate of 1.8 L/minute through a carbon dioxide insufflator (UCR; Olympus, Japan) in all patients.
When a long-length DBE (EN-580T, Fujifilm, Tokyo, Japan) or SBE (SIF-Q260, Olympus Medical Systems, Tokyo, Japan) was used, long-length devices were utilized for selective cannulation, including commercially available catheters such as the controlled radial expansion balloon catheter (Boston Scientific Korea, Seoul, Korea) or manually modified devices were used. If necessary, the long enteroscope was replaced with a short enteroscope while keeping the balloon overtube in place[14]. Conversely, in cases of failure with a short enteroscope, the enteroscope was exchanged for a long enteroscope, maintaining the balloon overtube in position[14]. In a short-type enteroscope, the effective length is approximately 150 cm, allowing compatibility with nearly all devices required for standard ERCP procedures. The enteroscope was selectively and retrogradely advanced into the afferent loop until it reached the blind end (Figure 2). Once the target site was accessed, biliopancreatic duct cannulation was attempted using an ERCP catheter. In this study, “difficult cannulation” was defined as any of the following: (1) More than five cannulation attempts involving contact with the papilla; (2) More than five minutes of cannulation effort after the papilla was initially visualized; or (3) More than one inadvertent cannulation or contrast injection into the pancreatic duct[12]. The overtube balloon was then inflated to stabilize the intestinal tract, allowing secure endoscope handling and optimal access to the bile duct for ERCP-related interventions. Following diagnosis via cholangiopancreatography, endoscopic procedures, including sphincterotomy, balloon dilation of the anastomosis stricture, stone extraction, and stent placement, were performed according to clinical guidelines.
Continuous variables are expressed as means ± SD or medians with interquartile ranges, as appropriate, and categorical variables are presented as frequencies with proportions. For normally distributed continuous variables, comparisons were performed using Student’s t-test, whereas for skewed variables (e.g., length of hospital stay), the Mann-Whitney U test was applied. Categorical variables were analyzed using the χ² test. Risk factors for intubation failure and AEs were assessed using univariable and multivariable logistic regression analyses. Variables with P values < 0.2 in the univariable analysis were included as covariates in the multivariable analysis. Furthermore, descriptive comparison by surgical resection type in Supplementary Tables 1 and 2 were conducted for exploratory purposes, and therefore, formal statistical correction for multiple comparisons (e.g., Bonferroni adjustment) was not applied. Accordingly, the results should be interpreted with caution. All reported P values were two-sided, with P values < 0.05 considered to be statistically significant. All statistical analyses were conducted using R statistical software (version 4.0.2; R Foundation for Statistical Computing, Vienna, Austria). PSM was performed using a 1:1 nearest-neighbor caliper matching method with a caliper value set at 0.02.
Table 1 compares the baseline characteristics of the patients who underwent either DBE (n = 247) or SBE (n = 247). Other demographic and clinical characteristics, such as body mass index, smoking status, alcohol intake, and presence of acute cholangitis, were comparable between the two groups. However, a significant difference was noted in the proportion of patients who had undergone prior percutaneous transhepatic biliary drainage, with a higher percentage in the SBE group (12.6% vs 0.8%, P < 0.001), while the proportion of percutaneous transhepatic gallbladder drainage did not differ. Laboratory values, including white blood cell count and C-reactive protein, also showed significant differences between the two groups, with higher white blood cell count and C-reactive protein values in the DBE group. Notably, there were significant differences in the final diagnoses between the two groups, although bile duct stones were the most common diagnosis in both. The most common indication for primary surgery in both groups was gastric cancer. In terms of surgical reconstruction, PD with Roux-en-Y anastomosis was the most frequent procedure in the DBE group, whereas TG with Roux-en-Y anastomosis was the most common procedure in the SBE group.
| Variable | DBE (n = 247) | SBE (n = 247) | P value |
| Age, years | 66.0 ± 15.4 | 68.4 ± 11.6 | 0.051 |
| Sex | 0.406 | ||
| Male | 146 (59.1) | 156 (63.2) | |
| Female | 101 (40.9) | 91 (36.8) | |
| BMI, kg/m2 | 21.6 ± 2.8 | 21.6 ± 3.3 | 0.919 |
| Smoking | 40 (16.2) | 34 (13.8) | 0.528 |
| Alcohol intake | 27 (10.9) | 33 (13.4) | 0.491 |
| Amounts of alcohol (bottle/week) | 4.3 ± 5.0 | 2.3 ± 2.1 | 0.064 |
| Presence of acute cholangitis on admission | 104 (42.1) | 92 (37.2) | 0.312 |
| PTBD prior ERCP | 2 (0.8) | 31 (12.6) | < 0.001 |
| PTGBD prior ERCP | 12 (4.9) | 14 (5.7) | 0.840 |
| Initial laboratory findings | |||
| WBC, /μL | 6900.0 (5300.0-9500.0) | 5950.0 (4630.0-8345.0) | 0.003 |
| Hb, g/dL | 11.8 (10.3-13.1) | 11.4 (10.1-12.6) | 0.140 |
| Platelet, /μL | 209.0 (164.0-272.0) | 198.0 (157.0-248.5) | 0.072 |
| AST, IU/L | 33.0 (24.0-81.0) | 42.0 (25.0-92.0) | 0.157 |
| ALT, IU/L | 30.0 (17.0-59.0) | 36.0 (18.0-81.0) | 0.151 |
| Total bilirubin, mg/dL | 0.8 (0.6-1.8) | 0.8 (0.4-2.2) | 0.411 |
| Amylase, IU/L | 61.0 (41.0-84.0) | 65.0 (45.0-91.0) | 0.325 |
| Lipase, U/L | 30.0 (16.0-60) | 27.0 (18.0-50.0) | 0.970 |
| CRP, mg/L | 2.0 (0.1-9.1) | 1.2 (0.1-5.8) | 0.011 |
| Final diagnosis | < 0.001 | ||
| Malignant biliary obstruction | 53 (21.5) | 33 (13.4) | |
| Benign biliary obstruction | 73 (29.6) | 42 (17.0) | |
| Bile duct stones | 94 (38.1) | 156 (63.2) | |
| Pancreatic duct stones | 3 (1.2) | 0 (0.0) | |
| Pancreatic duct stricture | 8 (3.2) | 5 (2.0) | |
| Others | 16 (6.5) | 11 (4.5) | |
| Reason of primary surgery | < 0.001 | ||
| AOV cancer | 21 (8.5) | 7 (2.8) | |
| Cholangiocarcinoma (or suspected) | 36 (14.6) | 33 (13.4) | |
| Duodenal cancer | 2 (0.8) | 3 (1.2) | |
| Gastric cancer | 107 (43.3) | 164 (66.4) | |
| GB cancer | 5 (2.0) | 10 (4.0) | |
| Pancreatic cancer (or suspected) | 42 (17.0) | 3 (1.2) | |
| Other tumors | 0 (0.0) | 2 (0.8) | |
| Bile duct or IHD stones | 5 (2.0) | 3 (1.2) | |
| Biliary atresia | 6 (2.4) | 0 (0.0) | |
| Choledochal cyst | 5 (2.0) | 5 (2.0) | |
| PUD complication | 12 (4.9) | 9 (3.6) | |
| Trauma or surgical injury | 6 (2.4) | 8 (3.2) | |
| Type of primary surgery | < 0.001 | ||
| PD with B-II | 10 (4.0) | 28 (11.3) | |
| PD with B-II and Braun anastomosis | 2 (0.8) | 5 (2.0) | |
| PD with R-Y | 77 (31.2) | 1 (0.4) | |
| STG with B-II | 49 (19.8) | 42 (17.0) | |
| STG with B-II and Braun anastomosis | 7 (2.8) | 37 (15.0) | |
| STG with R-Y | 40 (16.2) | 30 (12.1) | |
| TG with R-Y | 23 (9.3) | 69 (27.9) | |
| BDR with R-Y | 39 (15.8) | 35 (14.2) |
Table 2 summarizes the endoscopic findings between the DBE and SBE groups. The type of JJstomy differed significantly between the groups, with side-to-side anastomosis performed in 56.7% of the DBE group and 41.3% of the SBE group. The DBE group also had a significantly higher proportion of preserved gastric anatomy (50.2% vs 27.9%, P < 0.001). Procedure-related parameters, including intubation to JJstomy time and total intubation time, were significantly longer in the SBE group. The mean intubation to JJstomy time was 11.2 ± 10.8 minutes in the SBE group compared to 6.4 ± 7.7 minutes in the DBE group (P < 0.001). Similarly, the total intubation time was longer in the SBE group (23.5 ± 22.3 minutes) than in the DBE group (14.1 ± 13.5 minutes, P < 0.001). The total procedure time was significantly longer in the SBE group than in the DBE group (65.2 ± 37.9 minutes vs 31.0 ± 18.5 minutes, P < 0.001), whereas the selective deep cannulation time showed no significant difference between the two groups. Furthermore, the successful intubation and selective cannulation rates did not differ statistically between the two groups.
| Variable | DBE (n = 247) | SBE (n = 247) | P value |
| Type of JJstomy | 0.002 | ||
| None | 59 (23.9) | 70 (28.3) | |
| End to side | 48 (19.4) | 75 (30.4) | |
| Side to side | 140 (56.7) | 102 (41.3) | |
| Preserved gastric anatomy | 124 (50.2) | 69 (27.9) | < 0.001 |
| Used scope | < 0.001 | ||
| Long DBE | 15 (6.1) | 0 (0.0) | |
| Short DBE | 222 (89.9) | 0 (0.0) | |
| Short DBE ≥ long DBE | 2 (0.8) | 0 (0.0) | |
| Long DBE ≥ short DBE | 8 (3.2) | 0 (0.0) | |
| Short SBE | 0 (0.0) | 230 (93.1) | |
| Short SBE ≥ long SBE | 0 (0.0) | 3 (1.2) | |
| Long SBE ≥ short SBE | 0 (0.0) | 14 (5.7) | |
| Periampullary diverticulum | 16 (6.5) | 21 (8.5) | 0.494 |
| Time for intubation to JJ, minutes | 6.4 ± 7.7 | 11.2 ± 10.8 | < 0.001 |
| Successful intubation time, minutes | 14.1 ± 13.5 | 23.5 ± 22.3 | < 0.001 |
| Total procedure time, minutes | 31.0 ± 18.5 | 65.2 ± 37.9 | < 0.001 |
| Selective cannulation time, minutes | 3.9 ± 8.1 | 3.7 ± 6.8 | 0.780 |
| Naive papilla | 111 (44.9) | 123 (49.8) | 0.247 |
| Intubation failure | 14 (5.7) | 9 (3.6) | 0.393 |
| Selective cannulation failure | 26 (10.5) | 16 (6.5) | 0.147 |
| Difficult cannulation | 48 (19.4) | 50 (20.2) | 0.910 |
| Double guidewire method | 9 (3.6) | 20 (8.1) | 0.056 |
| Pancreatic duct injection | 14 (5.7) | 3 (1.2) | 0.014 |
| Pancreatic sphincterotomy | 0 (0.0) | 2 (0.8) | 0.479 |
| EPBD | 59 (23.9) | 152 (61.5) | < 0.001 |
| EST | 5 (2.0) | 70 (28.3) | < 0.001 |
| Endobiliary biopsy | 10 (4.0) | 32 (13.0) | 0.001 |
| Intraductal balloon dilation | 35 (14.2) | 29 (11.7) | 0.503 |
| Biliary stent placement | 90 (36.4) | 69 (27.9) | 0.054 |
| Pancreatic stent placement | 36 (14.6) | 21 (8.5) | 0.049 |
Descriptive comparison based on resection type demonstrated that the DBE group consistently achieved shorter times to JJstomy intubation and total procedure completion than the SBE group, particularly in BDR, PD, and STG cases. For example, among patients with BDR, the time for JJstomy intubation was significantly shorter with DBE (Video 1) than with SBE (Video 2) (10.8 ± 6.6 minutes vs 20.8 ± 17.0 minutes, P = 0.002), as was the total procedure time (37.4 ± 17.0 minutes vs 87.8 ± 47.3 minutes, P < 0.001). Similar trends were observed in PD (intubation time: 14.8 ± 13.4 minutes vs
Table 3 compares the clinical outcomes between the DBE and SBE groups. There was no statistically significant difference between the two groups in terms of the technical success rate in the first session (87.9% for DBE and 91.5% for SBE, P = 0.237) and overall technical success (88.3% vs 92.7%, P = 0.125), respectively. Notably, the SBE group experienced more post-procedure AEs with significant differences in the rates of post-ERCP cholangitis (0.4% vs 3.6%, P = 0.025) and post-ERCP cholecystitis (0.0% vs 2.4%, P = 0.040). Length of hospital stay was comparable between the two groups [median (interquartile range) 5.0 (1.0-9.0) days for DBE vs 5.0 (3.0-7.0) days for SBE, P = 0.054].
| Variable | DBE (n = 247) | SBE (n = 247) | P value |
| Overall technical success | 218 (88.3) | 229 (92.7) | 0.125 |
| Technical success in 1st session | 217 (87.9) | 226 (91.5) | 0.237 |
| Total adverse events | 26 (10.5) | 36 (14.6) | 0.222 |
| Sedation related AE | 2 (0.8) | 3 (1.2) | 1.000 |
| Post-procedure pancreatitis | 12 (4.9) | 21 (8.5) | 0.149 |
| Mild | 12 (4.9) | 16 (6.5) | 0.125 |
| Moderately severe | 0 (0.0) | 4 (1.6) | |
| Severe | 0 (0.0) | 1 (0.4) | |
| Pneumoperitoneum | 5 (2.0) | 1 (0.4) | 0.218 |
| Perforation | 2 (0.8) | 0 (0.0) | 0.479 |
| Significant bleeding | 4 (1.6) | 1 (0.4) | 0.369 |
| Post-ERCP cholecystitis | 0 (0.0) | 6 (2.4) | 0.040 |
| Post-ERCP cholangitis | 1 (0.4) | 9 (3.6) | 0.025 |
| Length of hospital stay, days, median (interquartile range) | 5.0 (1.0-9.0) | 5.0 (3.0-7.0) | 0.054 |
| Repeated ERCP within 30 days | 33 (13.4) | 26 (10.5) | 0.405 |
Table 4 evaluates the risk factors for post-procedure AEs using univariable and multivariable analyses. The presence of a preserved gastric anatomy significantly reduced the risk of post-procedure AEs [odds ratio (OR) = 0.03, 95% confidence interval (CI): 0.01-0.34, P = 0.003], whereas difficult cannulation significantly increased the risk (OR = 2.21, 95%CI: 1.12-4.32, P = 0.021). Table 5 presents the results of the univariable and multivariable analyses used to identify the risk factors for intubation failure. In the multivariable analysis, preserved gastric anatomy and Roux-en-Y reconstruction than Billroth II anastomosis as the type of reconstruction were found to be significant factors. Patients with a preserved gastric anatomy had a higher likelihood of intubation failure (OR = 3.18, 95%CI: 1.30-8.31, P = 0.013), and patients who had undergone Roux-en-Y reconstruction had a significantly higher risk than those who had undergone Billroth II anasto
| Variable | Univariable analysis | Multivariable analysis | ||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| SBE (vs DBE) | 1.74 (1.00-3.10) | 0.052 | 1.62 (0.82-3.23) | 0.164 |
| Age > 65 years | 1.01 (0.58-1.77) | 0.984 | ||
| Male sex | 1.05 (0.60-1.68) | 0.876 | ||
| History of acute pancreatitis | 0.42 (0.07-1.44) | 0.245 | ||
| Acute cholangitis on admission | 1.38 (0.79-2.39) | 0.256 | ||
| PTBD prior ERCP | 2.16 (0.83-5.00) | 0.087 | 1.79 (0.66-4.38) | 0.221 |
| PTGBD prior ERCP | 1.86 (0.60-4.80) | 0.230 | ||
| Resection | ||||
| PD (vs BDR) | 0.68 (0.22-2.20) | 0.510 | 0.36 (0.07-1.68) | 0.198 |
| STG (vs BDR) | 2.17 (0.93-5.97) | 0.096 | 0.04 (0.00-0.54) | 0.012 |
| TG (vs BDR) | 1.70 (0.62-5.11) | 0.314 | 0.04 (0.00-0.53) | 0.012 |
| Reconstruction | ||||
| B-II Braun (vs B-II) | 0.48 (0.21-1.02) | 0.063 | 0.60 (0.24-1.40) | 0.245 |
| R-Y (vs B-II) | 0.64 (0.34-1.19) | 0.154 | 0.49 (0.19-1.18) | 0.126 |
| Preserved gastric anatomy | 0.33 (0.16-0.62) | 0.001 | 0.03 (0.00-0.34) | 0.003 |
| Difficult cannulation | 2.42 (1.31-4.34) | 0.004 | 2.21 (1.12-4.32) | 0.021 |
| EPBD | 1.19 (0.68-2.07) | 0.530 | ||
| EST | 1.74 (0.86-3.34) | 0.106 | 0.89 (0.38-1.97) | 0.775 |
| Biliary stent placement | 1.03 (0.56-1.83) | 0.921 | ||
| Pancreatic stent placement | 0.87 (0.32-1.99) | 0.762 | ||
| Variable | Univariable analysis | Multivariable analysis | ||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| SBE (vs DBE) | 0.63 (0.26-1.46) | 0.289 | ||
| Age > 65 years | 1.11 (0.48-2.71) | 0.813 | ||
| Male sex | 0.99 (0.42-2.42) | 0.979 | ||
| Acute cholangitis on admission | 1.18 (0.49-2.73) | 0.703 | ||
| PTBD prior ERCP | 2.21 (0.50-6.90) | 0.222 | ||
| Resection | ||||
| PD (vs BDR) | 0.50 (0.17-1.45) | 0.197 | ||
| STG (vs BDR) | 0.16 (0.04-0.54) | 0.004 | ||
| TG (vs BDR) | 0.38 (0.10-1.24) | 0.122 | ||
| Reconstruction | ||||
| B-II Braun (vs B-II) | 7.34 (1.28-138.32) | 0.064 | 5.13 (0.87-97.60) | 0.132 |
| R-Y (vs B-II) | 8.69 (1.73-158.02) | 0.037 | 8.65 (1.71-157.60) | 0.038 |
| Preserved gastric anatomy | 3.09 (1.31-7.80) | 0.012 | 3.18 (1.30-8.31) | 0.013 |
This study represents the largest cohort to date comparing the clinical outcomes of ERCP using DBE and SBE in patients with SAA. The success rates of enteroscope intubation, biliary cannulation, and completion of the intended ERCP procedure were comparable between the DBE and SBE groups, irrespective of the anatomical subtype (Supplementary Tables 1 and 2). Preserved gastric anatomy and Roux-en-Y reconstruction were identified as significant risk factors for intubation failure, whereas the type of enteroscope (DBE vs SBE) did not significantly influence intubation success rate. These findings suggest that, beyond device selection, operator proficiency with each enteroscope type and patient-specific anatomical variations are key determinants of successful intubation in patients with SAA.
In this study, the intubation time was significantly shorter in the DBE group than in the SBE group across most anatomical subtypes. Although the balloon inflation and deflation process inherently prolong the procedure, the enhanced stability provided by the inflated balloon may have minimized unintentional backward endoscope slippage during overtube advancement. This, in turn, may have facilitated loop reduction in conjunction with the overtube balloon, ultimately contributing to shorter intubation duration. However, in patients with the most complex anatomy such as bilioenteric diversion with Roux-en-Y reconstruction (BDR), the DBE group exhibited a higher rate of intubation failure than the SBE group (12.8% vs 8.6%), although the difference was not statistically significant. These findings suggest potential confounding factors affecting intubation time, including inter-operator variability in insertion techniques and differences in the length of the reconstructed biliopancreatic limb, which may vary according to the surgical practices at individual centers. According to this difference, the longer procedure time in the SBE group may be attributed to prolonged intubation time and a higher prevalence of bile duct stones, which typically necessitate more time-consuming therapeutic interventions.
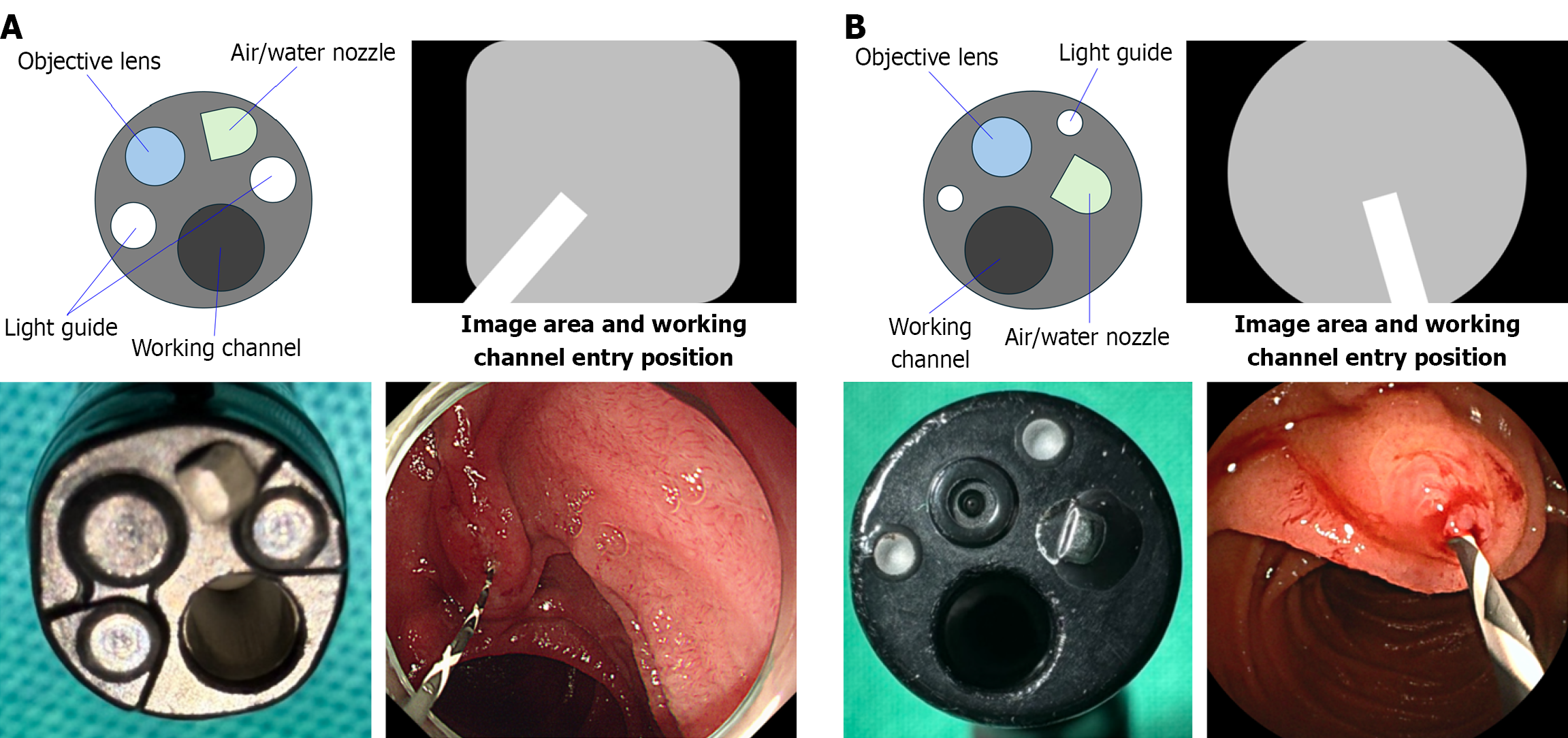
Selective cannulation failed in 10.5% and 6.5% of cases in the DBE and SBE groups, respectively; however, this difference was not statistically significant (P = 0.147). Nevertheless, the numerically lower failure rate observed in the SBE group may reflect the mechanical or procedural advantages under specific anatomical conditions. In patients with a native papilla, such as those who have undergone Roux-en-Y or Billroth II gastrectomy, the papilla typically appears inverted on the endoscopic screen, usually oriented between the 11 and 12 o’clock positions[15]. In this anatomical orientation, SBE offers an advantage, as the catheter exits from the 8 o’clock position, which is more closely aligned with the biliary axis[16]. In contrast, biliary cannulation using DBE, featuring a working channel directed at approximately the 5:30 position, requires repositioning of the papilla to the 6 o’clock orientation (Figure 3)[17]. This need for papillary repositioning, in accordance with the working channel axis, may have contributed to the subtle difference in cannulation success rates between the two groups, although this has not been systematically investigated. Furthermore, differences in the types of catheters and guidewires used for cannulation, as well as variations in individual techniques, may have influenced the observed outcomes.
Compared to the success rates reported in a previous systematic review[18], our findings were comparable or slightly higher. They reported technical success rates of 96% in patients with Billroth II reconstruction, 80% in those with Roux-en-Y anatomy, and 85% in patients who had undergone PD or hepaticojejunostomy[18]. In our study, intubation success rates in patients with TG and STG were high, ranging from 95.7% in both groups. Among patients with BDR, the success rates were 91.4% and 87.2% in the SBE and DBE groups, respectively. In patients who underwent PD, the technical success rates were 97.1% for SBE and 93.3% for DBE. When comparing SBE and DBE, a similar trend was observed in the first-session technical success rate, with a slightly higher rate in the SBE group (91.5%) than in the DBE group (87.9%), although the difference was not statistically significant. The DBE group included a higher proportion of patients with malignant biliary strictures following PD, which are associated with more severe anatomical distortion and fibrosis than benign strictures. These factors may have contributed to the lower success rates observed in the DBE group, particularly in cases involving high-grade hepaticojejunostomy strictures, despite the significantly shorter intubation time in this group.
Regarding AEs, most procedures in the SBE group were performed for stone removal, whereas in the DBE group, the primary indication was biliary drainage for malignant or benign strictures. As most cases in the DBE group involved stent placement for stricture management, the lower incidence of post-ERCP cholangitis observed in this group may be attributed to the routine drainage. In contrast, prophylactic stent placement was not performed following stone extraction in the SBE group, potentially contributing to the higher rate of post-ERCP cholangitis. Additionally, 36% of the patients in the DBE group underwent PD with concurrent cholecystectomy, compared to only 13.7% in the SBE group. This discrepancy may also contribute to the higher risk of post-ERCP cholecystitis in the SBE group. Interestingly, a preserved gastric anatomy was associated with a lower incidence of AEs (Table 4). This may be attributed to the fact that patients with prior PD or BDR, who typically have a preserved gastric anatomy, rarely require interventions through the native papilla, thus minimizing the risk of post-procedure pancreatitis. This protective effect may have outweighed the negative impact of increased intubation failure and prolonged procedure times, ultimately rendering the absence of gastrectomy a favorable factor in reducing AEs. In addition, difficult cannulation emerged as an independent predictor of AEs. This finding is consistent with previous studies[19-21] indicating that prolonged or repeated cannulation attempts increase the risk of papillary trauma and subsequent ductal inflammation.
Post-procedure pancreatitis was reported less frequently in the DBE group. This may be attributed to the higher proportion of patients with PD or BDR anatomy in this group, in which the separation of the biliary and pancreatic ducts reduces the likelihood of inadvertent pancreatic duct manipulation. Moreover, the majority of DBE-ERCP cases were performed for hepaticojejunostomy strictures requiring biliary stent placement, further minimizing pancreatic inter
Multivariable analysis identified Roux-en-Y and preserved gastric anatomy as significant risk factors for intubation failure. This aligns with previous findings and may reflect the increased difficulty in navigating the long and angulated afferent limb in Roux-en-Y anatomy, as well as loop formation in patients with preserved gastric anatomy[24]. In particular, gastric redundancy and instability in the proximal duodenum can result in the formation of complex S-shaped bowel loops, which create mechanical discordance between the shaft and tip of the enteroscope, thereby hindering smooth scope advancement[25]. Furthermore, the within-group comparison by surgical resection type (Supplementary Table 1) revealed that certain anatomies, particularly BDR, were consistently associated with longer intubation times and higher intubation failure rates. These findings suggest that procedural complexity is not solely dependent on the type of enteroscope but is also significantly influenced by the underlying surgical reconstruction, underscoring the importance of anatomy-specific procedural strategies.
This study has several limitations. First, its retrospective design may have introduced inherent selection and informa
Both DBE and SBE demonstrated comparable clinical success and safety profiles in ERCP for patients with SAA. However, DBE was associated with significantly shorter intubation and total procedure times than SBE. These findings suggest that DBE’s shorter procedure time could be of practical importance in complex or lengthy procedures, although further prospective validation is warranted.
| 1. | ASGE Standards of Practice Committee; Pawa S, Marya NB, Thiruvengadam NR, Ngamruengphong S, Baron TH, Bun Teoh AY, Bent CK, Abidi W, Alipour O, Amateau SK, Desai M, Chalhoub JM, Coelho-Prabhu N, Cosgrove N, Elhanafi SE, Forbes N, Fujii-Lau LL, Kohli DR, Machicado JD, Navaneethan U, Ruan W, Sheth SG, Thosani NC, Qumseya BJ; (ASGE Standards of Practice Committee Chair). American Society for Gastrointestinal Endoscopy guideline on the role of therapeutic EUS in the management of biliary tract disorders: summary and recommendations. Gastrointest Endosc. 2024;100:967-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 31] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 2. | Moreels TG. History of endoscopic devices for the exploration of the small bowel. Acta Gastroenterol Belg. 2009;72:335-337. [PubMed] |
| 3. | Sunada K, Yamamoto H. Double-balloon endoscopy: past, present, and future. J Gastroenterol. 2009;44:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Katanuma A, Isayama H. Current status of endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy in Japan: questionnaire survey and important discussion points at Endoscopic Forum Japan 2013. Dig Endosc. 2014;26 Suppl 2:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | De Koning M, Moreels TG. Comparison of double-balloon and single-balloon enteroscope for therapeutic endoscopic retrograde cholangiography after Roux-en-Y small bowel surgery. BMC Gastroenterol. 2016;16:98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Shah RJ, Smolkin M, Yen R, Ross A, Kozarek RA, Howell DA, Bakis G, Jonnalagadda SS, Al-Lehibi AA, Hardy A, Morgan DR, Sethi A, Stevens PD, Akerman PA, Thakkar SJ, Brauer BC. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc. 2013;77:593-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 207] [Article Influence: 15.9] [Reference Citation Analysis (1)] |
| 7. | Itokawa F, Itoi T, Ishii K, Sofuni A, Moriyasu F. Single- and double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y plus hepaticojejunostomy anastomosis and Whipple resection. Dig Endosc. 2014;26 Suppl 2:136-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Iwai T, Kida M, Yamauchi H, Imaizumi H, Koizumi W. Short-type and conventional single-balloon enteroscopes for endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: single-center experience. Dig Endosc. 2014;26 Suppl 2:156-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Tanisaka Y, Ryozawa S, Itoi T, Yamauchi H, Katanuma A, Okabe Y, Irisawa A, Nakahara K, Iwasaki E, Ishii K, Kin T, Terabe H, Izawa N, Morita R, Minami K, Araki R, Fujita A, Ogawa T, Mizuide M, Kida M. Efficacy and factors affecting procedure results of short-type single-balloon enteroscopy-assisted ERCP for altered anatomy: a multicenter cohort in Japan. Gastrointest Endosc. 2022;95:310-318.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 52] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 10. | Shimatani M, Hatanaka H, Kogure H, Tsutsumi K, Kawashima H, Hanada K, Matsuda T, Fujita T, Takaoka M, Yano T, Yamada A, Kato H, Okazaki K, Yamamoto H, Ishikawa H, Sugano K; Japanese DB-ERC Study Group. Diagnostic and Therapeutic Endoscopic Retrograde Cholangiography Using a Short-Type Double-Balloon Endoscope in Patients With Altered Gastrointestinal Anatomy: A Multicenter Prospective Study in Japan. Am J Gastroenterol. 2016;111:1750-1758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 134] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 11. | Shimatani M, Mitsuyama T, Tokuhara M, Masuda M, Miyamoto S, Ito T, Nakamaru K, Ikeura T, Takaoka M, Naganuma M, Okazaki K. Recent advances of endoscopic retrograde cholangiopancreatography using balloon assisted endoscopy for pancreaticobiliary diseases in patients with surgically altered anatomy: Therapeutic strategy and management of difficult cases. Dig Endosc. 2021;33:912-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1238] [Cited by in RCA: 2022] [Article Influence: 126.4] [Reference Citation Analysis (1)] |
| 13. | Park CH, Park SW, Hyun B, Lee J, Kae SH, Jang HJ, Koh DH, Choi MH. Efficacy and safety of etomidate-based sedation compared with propofol-based sedation during ERCP in low-risk patients: a double-blind, randomized, noninferiority trial. Gastrointest Endosc. 2018;87:174-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Itoi T, Ishii K, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Tsuji S, Ikeuchi N, Moriyasu F, Sakai Y. Ultrathin endoscope-assisted ERCP for inaccessible peridiverticular papilla by a single-balloon enteroscope in a patient with Roux-en-Y anastomosis. Dig Endosc. 2010;22:334-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Tanisaka Y, Mizuide M, Fujita A, Shiomi R, Shin T, Sugimoto K, Ryozawa S. Single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: a technical review. Clin Endosc. 2023;56:716-725. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Tanisaka Y, Mizuide M, Fujita A, Jinushi R, Shiomi R, Shin T, Hirata D, Terada R, Tashima T, Mashimo Y, Ryozawa S. Can endoscopic retrograde cholangiopancreatography-related procedures for resolving acute cholangitis be effectively and safely performed in patients with surgically altered anatomy? Comparison study to evaluate the timing of short-type single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography. Dig Endosc. 2023;35:361-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Shimatani M, Tokuhara M, Kato K, Miyamoto S, Masuda M, Sakao M, Fukata N, Miyoshi H, Ikeura T, Takaoka M, Okazaki K. Utility of newly developed short-type double-balloon endoscopy for endoscopic retrograde cholangiography in postoperative patients. J Gastroenterol Hepatol. 2017;32:1348-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Skinner M, Popa D, Neumann H, Wilcox CM, Mönkemüller K. ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 2014;46:560-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 161] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 19. | Lee KJ, Cho E, Park DH, Cha HW, Koh DH, Lee J, Park CH, Park SW. Identification of risk factors associated with post-ERCP pancreatitis in patients with easy cannulation: a prospective multicenter observational study (with videos). Gastrointest Endosc. 2025;101:988-996.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna GS, Shaw MJ, Snady HW, Erickson RV, Moore JP, Roel JP. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 852] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 21. | Testoni PA, Mariani A, Giussani A, Vailati C, Masci E, Macarri G, Ghezzo L, Familiari L, Giardullo N, Mutignani M, Lombardi G, Talamini G, Spadaccini A, Briglia R, Piazzi L; SEIFRED Group. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol. 2010;105:1753-1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 210] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 22. | Wu CCH, Lim SJM, Khor CJL. Endoscopic retrograde cholangiopancreatography-related complications: risk stratification, prevention, and management. Clin Endosc. 2023;56:433-445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 23. | Kopacova M, Tacheci I, Rejchrt S, Bartova J, Bures J. Double balloon enteroscopy and acute pancreatitis. World J Gastroenterol. 2010;16:2331-2340. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Abu Dayyeh B. Single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy: getting there. Gastrointest Endosc. 2015;82:20-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Yang MJ, Cho W, Hwang JC, Yoo BM, Kim SS, Kim JH, Shin EJ. Mechanistic loop-resolution strategies for short-type single-balloon enteroscopy-assisted ERCP in patients post Roux-en-Y hepaticojejunostomy with a preserved stomach and duodenum. Endoscopy. 2025;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/