Published online Oct 7, 2025. doi: 10.3748/wjg.v31.i37.110942
Revised: July 23, 2025
Accepted: August 25, 2025
Published online: October 7, 2025
Processing time: 96 Days and 2.3 Hours
Since Japanese national insurance coverage was expanded to include Helicobacter pylori (H. pylori) gastritis in 2013, approximately 1.5 million patients have received eradication therapy annually. However, the prevalence and clinical features of uninvestigated dyspepsia in the post-eradication era remain unclear.
To evaluate the prevalence of dyspepsia and related endoscopic findings in the general population.
We analyzed data from a gastric cancer screening program using esophagogas
Among 23250 participants, overall dyspepsia prevalence was 28.0%. It was 28.7% in the non-infected and post-eradication cohorts, and lower (25.8%, P < 0.05) in the currently infected or naturally eradicated cohort. In addition, 23.1% of participants reported heartburn. The following were independently associated with dyspepsia: Age < 60 years, female sex, gastric ulcers, duodenal ulcers, erosive esophagitis, a history of gastric surgery, and successful H. pylori eradication. Gastric or esophageal cancer showed no association.
Uninvestigated dyspepsia remains common even after successful H. pylori eradication. Dyspepsia was not con
Core Tip: We analyzed over 23000 adults undergoing endoscopic gastric cancer screening in Japan to assess dyspepsia prevalence across Helicobacter pylori infection statuses. Dyspepsia was most prevalent (28.7%) in the post-eradication and non-infected groups, compared to 25.8% in the currently infected group. Younger age, female sex, peptic ulcers, erosive esophagitis, and post-eradication status were independently associated with dyspepsia. Despite extensive endoscopic evaluation, over 90% of cases had no organic findings. These results highlight the evolving nature of dyspepsia and its persistence in the post-Helicobacter pylori era.
- Citation: Suzuki S, Kanno T, Koike T, Chiba T, Asanuma K, Kato K, Hatayama Y, Ogata Y, Saito M, Hatta W, Uno K, Imatani A, Masamune A. Epidemiology of dyspepsia and esophagogastroduodenoscopic findings in the era of Helicobacter pylori eradication. World J Gastroenterol 2025; 31(37): 110942
- URL: https://www.wjgnet.com/1007-9327/full/v31/i37/110942.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i37.110942
Dyspepsia, a prevalent gastrointestinal disorder, is characterized by abdominal pain, indigestion, epigastric discomfort, bloating, and nausea[1,2]. Patients with this condition usually experience impaired quality of life, highlighting its clinical and economic significance. Previous systematic reviews have shown that approximately 10%-20% of individuals undergoing health checkups in Japan experience chronic epigastric symptoms[3-5]. Similarly, the pooled global prevalence of dyspepsia is 20%[6]. Dyspepsia occurs in association with organic diseases, such as peptic ulcers, and in cases where no organic cause is identified. Notably, 85% of patients with dyspepsia who undergo upper gastrointestinal endoscopy have normal endoscopic findings[2,7-9]. Even in cases of functional dyspepsia without organic diseases, patients incur substantial costs, and work productivity is impaired owing to dyspeptic symptoms[10-12]. The annual direct cost to patients is 699 dollars, with an estimated 1.4 hours of work lost per week owing to functional dyspepsia symptoms[13]. Helicobacter pylori (H. pylori) infection is associated with dyspepsia, and symptom improvement is observed in some patients after eradication[14]. However, the prevalence of dyspeptic symptoms in patients after successful H. pylori eradication remains partially studied.
In Japan, clinical practice guidelines for dyspepsia recommend considering eradication therapy as the first-line treatment for all H. pylori-positive cases[15,16]. Furthermore, Japan introduced national insurance coverage for eradication therapy for all patients with H. pylori infections in 2013. This policy was implemented to support gastric cancer prevention and address the historically high infection rate. Moreover, approximately 1.5 million patients undergo eradication therapy annually[17]. Thus, substantial societal changes have led to a growing post-eradication population. Despite this shift, no large-scale epidemiological studies have been conducted in Japan over the past two decades to assess the prevalence of undiagnosed dyspepsia, associated endoscopic findings, or H. pylori infection status. Owing to the historically high incidence of gastric cancer in Japan, national screening programs have been long established. A gradual shift from radiography-based to endoscopic screening has been observed recently. The population of Sendai city is approximately 1060000, with 500000 residents aged ≥ 49 years[18]. Within this framework, the Sendai city endoscopic gastric cancer screening project, initiated in 2019, targets this population. Eligible individuals are encouraged to undergo screening every 2 years. We aim to clarify the epidemiology of dyspepsia in the general population, considering the H. pylori infection status and esophagogastroduodenoscopic (EGD) findings.
This study was conducted according to the principles of the Declaration of Helsinki (as revised in Brazil in 2013), STROBE reporting guidelines, and approved by the Ethics Committees of the Miyagi Cancer Society (Approval No. 3-2206). Written informed consent was not obtained, as the study involved the secondary use of anonymized data collected through a municipal gastric cancer screening program. Personal identifiers were removed before analysis. The study information was made publicly available on the institutional website, and an opt-out option was provided to protect participants’ rights.
In this cross-sectional study, we used data from the municipal gastric cancer screening program in Sendai city, targeting residents aged ≥ 49 years, conducted between June 27, 2019 and February 27, 2021. A total of 23250 participants were included, with no duplicate cases during the 2 years. Eligible participants selected one of the registered medical institutions for EGD and underwent the procedure after completing a medical questionnaire.
As part of the health screening program, participants completed a medical questionnaire before undergoing EGDs. The questionnaire included information on H. pylori eradication, screening tests for H. pylori, use of antithrombotic agents, and gastrointestinal symptoms, such as heartburn, upper abdominal pain, and bloating. Additionally, data on sex and age were obtained. Information on H. pylori eradication history was collected via a self-reported questionnaire, including the timing of eradication, the presence or absence of eradication confirmation, and the medical facility where the test was performed. These data were subjected to a double-check by public health nurses and trained nurses to ensure accuracy. All data were anonymized, and each participant was assigned an independent study number before data collection. Dyspepsia was defined as the presence of upper abdominal pain, bloating, or both. Incomplete responses on the questionnaires were considered missing values.
Only pre-registered endoscopists were authorized to perform EGD for the gastric cancer screening program. First, a preliminary report was prepared by a local endoscopist, and biopsies were performed at the physician’s discretion. Histopathological results, preliminary reports, and EGD images were submitted to the relevant cancer society. A secondary review was conducted by an independent expert endoscopist, who evaluated the EGD images and histopathological results of the biopsies in reference to the preliminary reports, to provide a final diagnostic evaluation. Gastric atrophy was evaluated according to the Kimura-Takemoto classification, with atrophy defined as extension to C-2 or beyond, based on the endoscopic findings. Malignancy was defined according to histopathological diagnosis rather than endoscopic appearance. For this study, anonymized data from the final reports, identified by research-specific study identification numbers, were used. Terminologies within the reports were standardized to ensure the consistent documentation of gastric atrophy and history of gastric surgery.
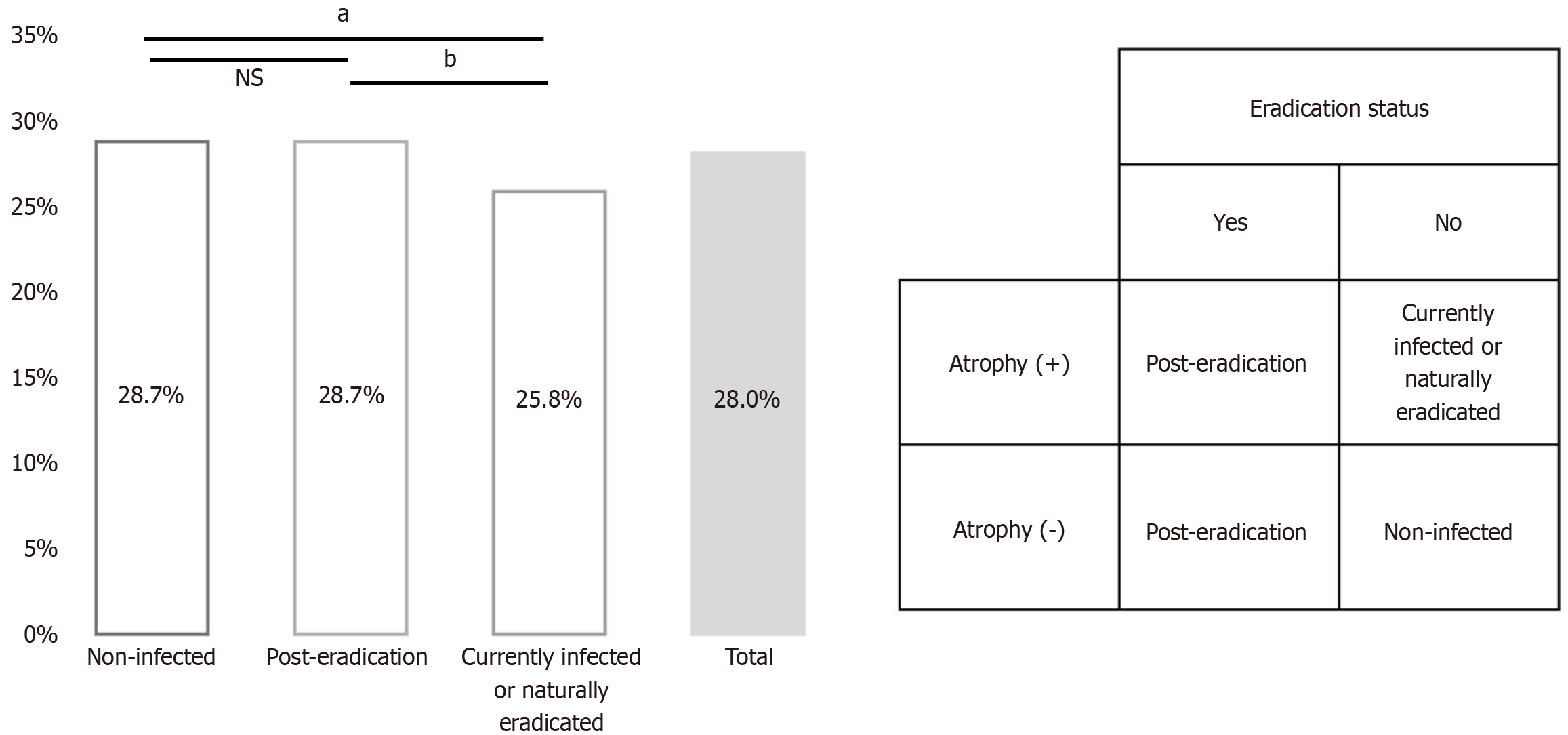
Participants were categorized into three cohorts based on their self-reported H. pylori eradication history and the presence or absence of endoscopic gastric atrophy. Those with a history of successful eradication were assigned to the post-eradication cohort. Participants without a history of eradication or endoscopic evidence of atrophy were classified as non-infected. Furthermore, participants without a history of eradication but with endoscopic evidence of gastric atrophy were classified as currently infected or having had H. pylori naturally eradicated.
Data have been presented as numbers and percentages. Nominal variables were analyzed using Fisher’s exact test. The Kruskal-Wallis test was applied to compare ≥ three groups of sample data. To identify factors correlated with dyspepsia, we compared the demographic and clinical characteristics of participants with and without the condition. Variables with potential correlations were subsequently included in a multivariate logistic regression model to determine independent factors. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (R Foundation for Statistical Computing, Vienna, Austria). EZR is a modified version of R Commander (Department of Informatics, Yokohama National University, Yokohama, Japan) enhanced to incorporate statistical functions frequently used in biostatistics[19]. Statistical significance was set at P < 0.05.
A total of 23250 participants participated in the screening, including 9562 males (41.1%) and 13688 females (58.9%), with a mean age of 69.1 ± 8.5 years. Regarding self-reported upper gastrointestinal symptoms, 4810 (20.7%), 2580 (11.1%), and 5380 (23.1%) participants reported heartburn, upper abdominal pain, and bloating, respectively. Based on symptom re
| Variable | Category number (n = 23250) |
| Sex | |
| Male | 9562 (41.1) |
| Female | 13688 (58.9) |
| Age (years) | |
| < 60 | 3483 (15.0) |
| 60-69 | 7443 (32.0) |
| 70-79 | 10035 (43.2) |
| ≥ 80 | 2289 (9.8) |
| Antithrombotic drug use | |
| Yes | 2152 (9.3) |
| No | 21071 (90.6) |
| Unknown | 27 (0.1) |
| Past history of Helicobacter pylori eradication | |
| Success | 6934 (29.8) |
| Failure or none | 15747 (67.7) |
| Unknown | 569 (2.4) |
| Symptoms | |
| Heartburn | 4810 (20.7) |
| Upper abdominal pain | 2580 (11.1) |
| Bloating | 5380 (23.1) |
| Dyspepsia1 | 6499 (28.0) |
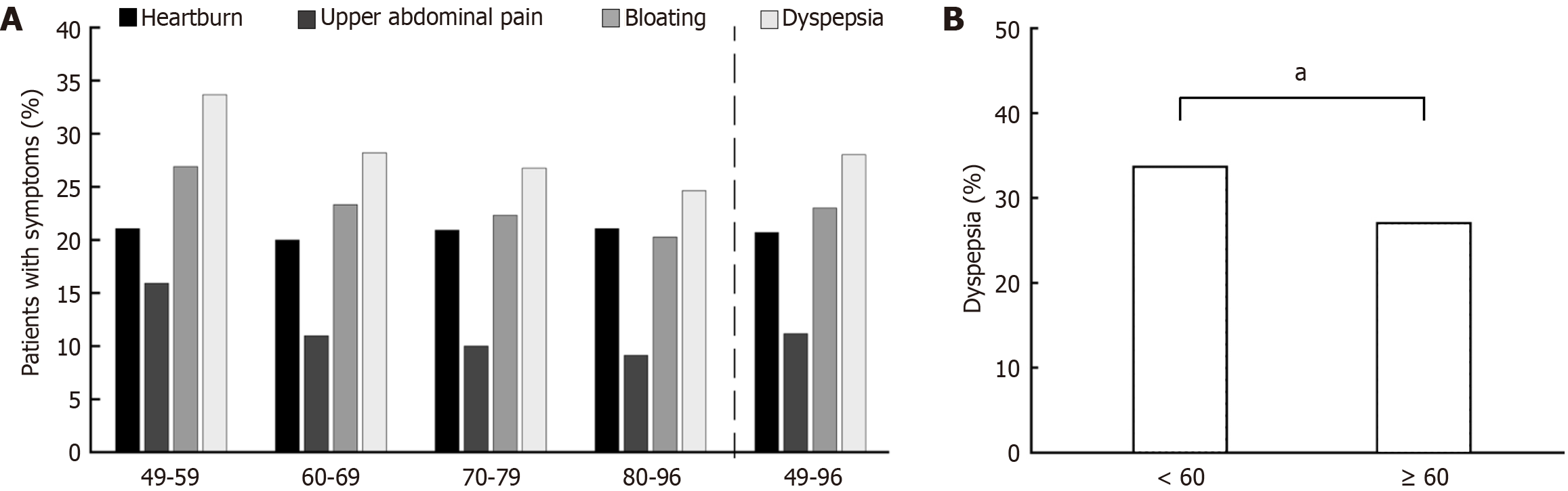
Figure 1 presents the prevalence of upper gastrointestinal symptoms by age cohort. The prevalence of heartburn remained relatively stable at approximately 20% across all age cohorts. In contrast, the prevalence of upper abdominal pain declined markedly after the age of 60 years, decreasing from 15.9% in participants aged 49-59 years to 10.9% in those aged 60-69 years. Similarly, the prevalence of bloating decreased progressively with age, from 26.9% in participants aged < 60 years to 20.3% in those aged ≥ 80 years. These trends imply that the overall prevalence of dyspepsia was higher among participants aged < 60 years (33.5%) than among those aged ≥ 60 years (27.0%, P < 0.001).
Of the 23250 participants who underwent EGD, 91 (0.4%), 29 (0.1%), and 1240 (5.3%) were diagnosed with gastric ulcers, duodenal ulcers, or reflux esophagitis (Los Angeles classification grade A or more severe), respectively. Moreover, esophageal cancer, gastric cancer, or a history of gastric surgery were identified in 27 (0.1%), 180 (0.8%), and 277 (1.2%) participants, respectively. Overall, 92.3% of participants had no organic findings on EGD (Table 2). The gastric atrophy status was assessed based on a combination of endoscopic findings and a history of H. pylori eradication. Among the participants, 31.9% had non-eradicated atrophic gastritis, 29.5% exhibited atrophic changes post-eradication, and 38.6% showed no atrophic changes.
| n (%) | |
| Organic EGD findings | |
| Gastric ulcer | 91 (0.4) |
| Duodenal ulcer | 29 (0.1) |
| Reflux esophagitis (≥ Los A) | 1240 (5.3) |
| Esophageal cancer | 27 (0.1) |
| Gastric cancer | 180 (0.8) |
| History of gastric surgery | 277 (1.2) |
| Gastric atrophy | |
| Non-eradicated atrophic gastritis | 7407 (31.9) |
| Atrophic changes post-eradication | 6868 (29.5) |
| No atrophic changes observed | 8977 (38.6) |
The prevalence of dyspepsia was compared across three cohorts, defined by H. pylori eradication history and the endoscopic atrophic status (Figure 2). Dyspepsia prevalence was 28.7% in the non-infected and post-eradication cohorts, with no notable differences between the two cohorts. In contrast, the currently infected/naturally eradicated cohort had a lower prevalence (25.8%) than did the other two cohorts (P < 0.01 and P < 0.05, respectively).
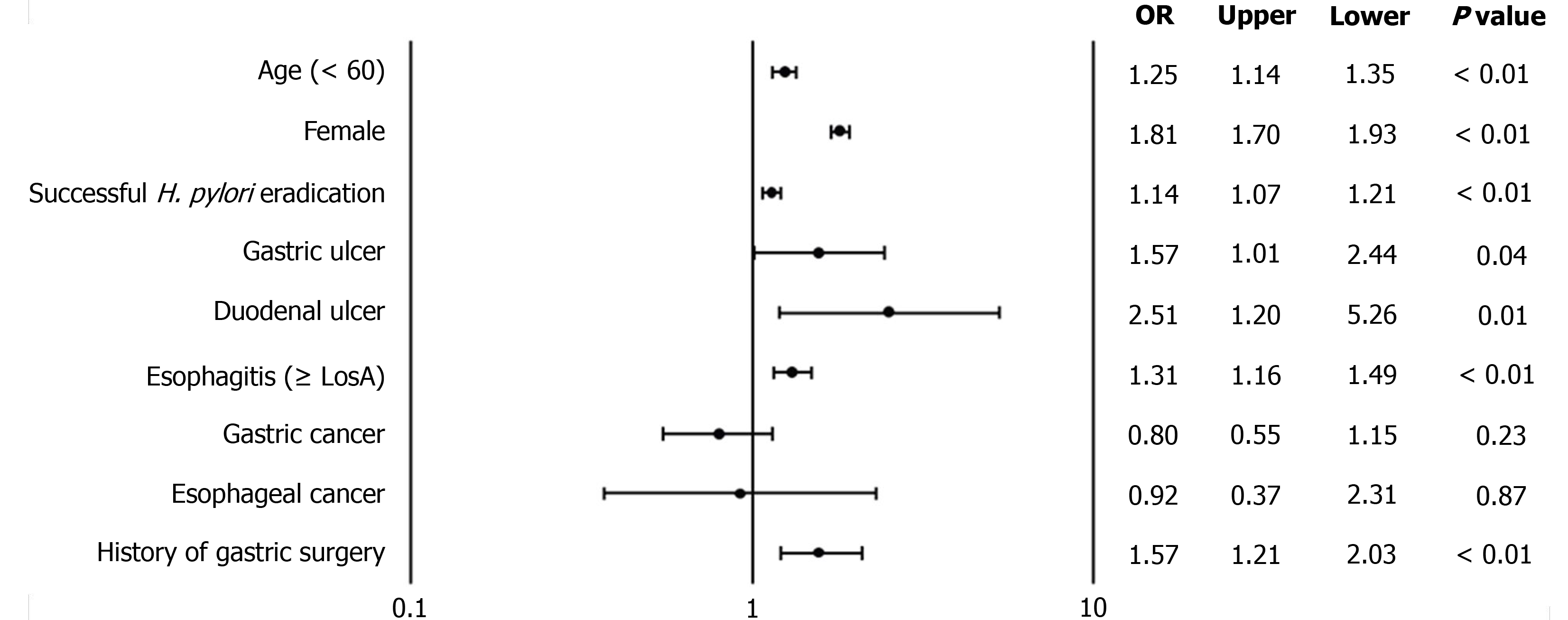
Baseline characteristics were compared between participants with and without dyspepsia (Table 3). Statistically significant differences were observed in age, sex, and the prevalence of duodenal ulcer, reflux esophagitis, gastric cancer, and non-eradicated atrophic gastritis between these two sub-cohorts. Based on these variables, a multivariate logistic regression analysis was conducted to identify the independent factors correlated with dyspepsia (Figure 3). The analysis revealed that the following factors were independently correlated with dyspepsia: Age < 60 years [odds ratio (OR) = 1.25; 95% confidence interval (CI): 1.15-1.35], female sex (OR = 1.81; 95%CI: 1.70-1.93), successful H. pylori eradication (OR = 1.14; 95%CI: 1.07-1.21), gastric ulcer (OR = 1.57; 95%CI: 1.01-2.44), duodenal ulcer (OR = 2.51; 95%CI: 1.20-5.26), reflux esophagitis (OR = 1.31; 95%CI: 1.16-1.49), and a history of gastric surgery (OR = 1.57; 95%CI: 1.21-2.03). Conversely, no notable correlations were found for gastric or esophageal cancer.
| Variable | Dyspepsia1 | P value | |
| Positive (n = 6499) | Negative (n = 16732) | ||
| Age (< 60 years) | 1167 (18.0) | 2314 (13.8) | < 0.01 |
| Female sex | 4471 (68.8) | 9209 (55.0) | < 0.01 |
| Past history of H. pylori eradication | 1994 (30.7) | 4934 (29.5) | 0.08 |
| Gastric ulcer | 31 (0.5) | 60 (0.4) | 0.20 |
| Duodenal ulcer | 14 (0.2) | 15 (0.1) | 0.02 |
| Reflux esophagitis (≥ Los A) | 378 (5.8) | 860 (5.1) | 0.04 |
| Esophageal cancer | 5 (0.1) | 22 (0.1) | 0.39 |
| Gastric cancer | 36 (0.6) | 144 (0.9) | 0.02 |
| History of gastric surgery | 88 (1.4) | 188 (1.1) | 0.16 |
| No organic EGD findings | 5952 (91.6) | 15455 (92.4) | 0.05 |
| No atrophic changes observed | 2576 (39.6) | 6395 (38.2) | 0.048 |
This study provides epidemiological insights into uninvestigated dyspepsia and upper gastrointestinal symptoms in the general population through the data derived from a large-scale endoscopic gastric cancer screening program. Previous epidemiological studies have consistently demonstrated that the prevalence of dyspepsia differs markedly between the general and hospital-based populations, with clinical populations typically exhibiting higher prevalence rates[3-5]. Thus, this large population-based study of over 23000 adults aged ≥ 49 years offers valuable epidemiological insights that differ from those obtained from clinical settings. A major strength of this study is the integration of detailed endoscopic findings with the H. pylori eradication status. This approach offers a multifaceted perspective on the prevalence and clinical significance of dyspeptic symptoms in contemporary Japan, where a substantial proportion of the population has undergone successful eradication.
First, we observed a dyspepsia prevalence of 28% in the general population, substantially higher than the previously reported range of 11%-17% in a similar population two decades ago[3-5,20]. Importantly, this study investigated the prevalence and background of uninvestigated dyspepsia, encompassing individuals with organic diseases, rather than functional dyspepsia as defined by Rome IV criteria[21]. Owing to Japan’s ethnic homogeneity and relatively stable sociocultural conditions, this increase in uninvestigated dyspepsia may reflect physiological changes within the population. One possible explanation is the increasing proportion of individuals with normal gastric acid secretion. This includes individuals who are H. pylori-negative and those who experience post-eradication recovery of acid secretion. Iijima et al[22] have observed an increase in gastric acid secretion in Japan over recent decades, primarily attributed to the declining prevalence of H. pylori infection. In this study, approximately 68% of participants showed no endoscopic evidence of gastric atrophy or had a history of successful eradication therapy. Regarding the correlation between the H. pylori infection status and dyspepsia, symptom prevalence was identical (28.7%) in the non-infected and post-eradication cohorts. This was notably higher than that in participants presumed to be currently infected or who had undergone natural eradication (25.8%). While eradication therapy for H. pylori infection improves dyspeptic symptoms, meta-analyses have indicated that the number needed for treatment remains modest: 9 (95%CI: 7-17) for partial symptom improvement and 14 (95%CI: 11-21) for complete symptom resolution[12]. Despite these benefits, the prevalence of dyspepsia in post-eradication populations remains partially studied. These findings offer significant new insights into the substantial proportion of patients who continue to experience dyspepsia despite successful eradication therapy. Additionally, while approximately 20% of the participants reported heartburn, only 5% exhibited endoscopic evidence of reflux esophagitis. This discrepancy highlights the epidemiological gap between reflux symptoms and organic diseases in the general Japanese population.
Second, our findings confirmed that most participants with dyspepsia (92.3%) had no clinically significant organic findings on EGD. This outcome aligns with the results of previous studies indicating that approximately 85% of patients with dyspepsia have negative endoscopic findings[2]. Multivariate logistic regression analysis revealed younger age, female sex, the presence of gastric or duodenal ulcers or erosive esophagitis, and a history of gastric surgery as independent factors correlated with dyspepsia, consistent with previous findings[23,24]. Conversely, gastric and esophageal cancers were not considerably correlated with dyspeptic symptoms. Advanced cancers may present with prominent symptoms, such as obstruction, bleeding, or nutritional deficiencies, which could contribute to dyspeptic complaints. However, such findings are uncommon in population-based health screenings. In this context, malignancies are frequently detected at an early stage, which may explain the lack of correlation with symptoms. This observation aligns with those of previous epidemiological studies in the general population, which have shown a limited association between dyspepsia and gastrointestinal malignancies[7]. These findings validate the limited utility of dyspepsia as a predictor of malignancy.
This study had some limitations. Firstly, H. pylori infection status was primarily determined using a self-reported questionnaire rather than systematic chemical or histopathological tests. While this approach is common in large-scale epidemiological studies, it inherently posed a limitation regarding precise diagnostic confirmation. However, we considered the self-reported data in our cohort to possess a considerable degree of reliability. A recent report demonstrated high reliability of such questionnaires for epidemiological investigations of H. pylori eradication, showing substantial agreement with medical records[25]. Furthermore, as detailed in the methods section, the self-reported eradication information in this study was meticulously verified through a double-check process conducted by public health nurses and trained nurses. Despite these efforts to enhance reliability, it was not possible to precisely identify individuals with active infection within the group showing endoscopic atrophy but no reported eradication history. This cohort likely included a majority of actively infected individuals, but may also have encompassed a subset with spontaneously cleared infection or unintended eradication due to prior antibiotic use. This inherent characteristic of the dataset should be considered when interpreting our findings. According to a meta-analysis, the rate of reinfection after the successful eradication of H. pylori is approximately 19% in regions with underdeveloped water and sanitation systems[26]. In contrast, Japan, with its nearly universal tap water infrastructure and reduced use of well water, reported a reinfection rate of only 0.2% in a 2012 study population of over 1600 participants, indicating a low likelihood of reinfection[27]. Second, our questionnaire did not fully encompass all symptoms defined by international diagnostic criteria for functional dyspepsia, such as postprandial fullness and early satiety[21]. This simplification might have led to an underestimation of the true prevalence of dyspepsia. While this symptom-based approach was pragmatic for a large-scale health screening and aligned with our objective of broadly understanding epidemiological trends without imposing strict clinical background limitations, we acknowledge that our analysis focused solely on self-reported upper abdominal symptoms and did not differentiate potential underlying non-gastrointestinal causes of abdominal pain, such as biliary or pancreatic diseases. Thus, some reported symptoms may have originated from sources beyond the gastrointestinal tract, which should be considered when interpreting the overall prevalence of dyspepsia. Finally, the questionnaire did not collect data on the use of medications known to influence gastrointestinal symptoms, including acid suppressive agents and nonsteroidal anti-inflammatory drugs. The absence of these variables limited our ability to control for important confounders in the multivariate analysis, and their use could have influenced the observed prevalence and associations of dyspepsia and EGD findings.
Dyspepsia was prevalent in 28.0% of the adult Japanese population. The post-eradication cohort reported a dyspepsia prevalence of 28.7%, the same as in the non-infected group. Similarly, dyspepsia was correlated with age, the female sex, successful H. pylori eradication, erosive esophagitis, gastric and duodenal ulcers, and a history of gastric surgery.
| 1. | Ford AC, Mahadeva S, Carbone MF, Lacy BE, Talley NJ. Functional dyspepsia. Lancet. 2020;396:1689-1702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 334] [Article Influence: 55.7] [Reference Citation Analysis (0)] |
| 2. | Nasseri-Moghaddam S, Mousavian AH, Kasaeian A, Kanno T, Yuan Y, Ford AC, Moayyedi P. What is the Prevalence of Clinically Significant Endoscopic Findings in Subjects With Dyspepsia? Updated Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2023;21:1739-1749.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Hirakawa K, Adachi K, Amano K, Katsube T, Ishihara S, Fukuda R, Yamashita Y, Shiozawa S, Watanabe M, Kinoshita Y. Prevalence of non-ulcer dyspepsia in the Japanese population. J Gastroenterol Hepatol. 1999;14:1083-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Kawamura A, Adachi K, Takashima T, Murao M, Katsube T, Yuki M, Watanabe M, Kinoshita Y. Prevalence of functional dyspepsia and its relationship with Helicobacter pylori infection in a Japanese population. J Gastroenterol Hepatol. 2001;16:384-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Kaji M, Fujiwara Y, Shiba M, Kohata Y, Yamagami H, Tanigawa T, Watanabe K, Watanabe T, Tominaga K, Arakawa T. Prevalence of overlaps between GERD, FD and IBS and impact on health-related quality of life. J Gastroenterol Hepatol. 2010;25:1151-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 185] [Article Influence: 11.6] [Reference Citation Analysis (3)] |
| 6. | Ford AC, Marwaha A, Sood R, Moayyedi P. Global prevalence of, and risk factors for, uninvestigated dyspepsia: a meta-analysis. Gut. 2015;64:1049-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 337] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 7. | Beaton DR, Sharp L, Lu L, Trudgill NJ, Thoufeeq M, Nicholson BD, Rogers P, Docherty J, Jenkins A, Morris AJ, Rösch T, Rutter MD. Diagnostic yield from symptomatic gastroscopy in the UK: British Society of Gastroenterology analysis using data from the National Endoscopy Database. Gut. 2024;73:1421-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Aziz Q, Fass R, Gyawali CP, Miwa H, Pandolfino JE, Zerbib F. Functional Esophageal Disorders. Gastroenterology. 2016;S0016-5085(16)00178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 384] [Cited by in RCA: 395] [Article Influence: 39.5] [Reference Citation Analysis (0)] |
| 9. | Zhao Y, Zou D, Wang R, Ma X, Yan X, Man X, Gao L, Fang J, Yan H, Kang X, Yin P, Hao Y, Li Q, Dent J, Sung J, Halling K, Wernersson B, Johansson S, He J. Dyspepsia and irritable bowel syndrome in China: a population-based endoscopy study of prevalence and impact. Aliment Pharmacol Ther. 2010;32:562-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 10. | Talley NJ, Locke GR, Saito YA, Almazar AE, Bouras EP, Howden CW, Lacy BE, DiBaise JK, Prather CM, Abraham BP, El-Serag HB, Moayyedi P, Herrick LM, Szarka LA, Camilleri M, Hamilton FA, Schleck CD, Tilkes KE, Zinsmeister AR. Effect of Amitriptyline and Escitalopram on Functional Dyspepsia: A Multicenter, Randomized Controlled Study. Gastroenterology. 2015;149:340-349.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 247] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 11. | Sperber AD, Freud T, Aziz I, Palsson OS, Drossman DA, Dumitrascu DL, Fang X, Fukudo S, Ghoshal UC, Kellow J, Khatun R, Okeke E, Quigley EMM, Schmulson M, Simren M, Tack J, Whitehead WE, Whorwell P, Bangdiwala SI. Greater Overlap of Rome IV Disorders of Gut-Brain Interactions Leads to Increased Disease Severity and Poorer Quality of Life. Clin Gastroenterol Hepatol. 2022;20:e945-e956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 85] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 12. | Brook RA, Kleinman NL, Choung RS, Melkonian AK, Smeeding JE, Talley NJ. Functional dyspepsia impacts absenteeism and direct and indirect costs. Clin Gastroenterol Hepatol. 2010;8:498-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 144] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 13. | Lacy BE, Weiser KT, Kennedy AT, Crowell MD, Talley NJ. Functional dyspepsia: the economic impact to patients. Aliment Pharmacol Ther. 2013;38:170-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 234] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 14. | Ford AC, Tsipotis E, Yuan Y, Leontiadis GI, Moayyedi P. Efficacy of Helicobacter pylori eradication therapy for functional dyspepsia: updated systematic review and meta-analysis. Gut. 2022;gutjnl-2021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 15. | Miwa H, Nagahara A, Asakawa A, Arai M, Oshima T, Kasugai K, Kamada K, Suzuki H, Tanaka F, Tominaga K, Futagami S, Hojo M, Mihara H, Higuchi K, Kusano M, Arisawa T, Kato M, Joh T, Mochida S, Enomoto N, Shimosegawa T, Koike K. Evidence-based clinical practice guidelines for functional dyspepsia 2021. J Gastroenterol. 2022;57:47-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 80] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 16. | Iwata E, Sugimoto M, Murata M, Morino Y, Akimoto Y, Hamada M, Niikura R, Nagata N, Kawai T. Improvement of dyspeptic symptoms after Helicobacter pylori eradication therapy in Japanese patients. JGH Open. 2023;7:855-862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Tsuda M, Asaka M, Kato M, Matsushima R, Fujimori K, Akino K, Kikuchi S, Lin Y, Sakamoto N. Effect on Helicobacter pylori eradication therapy against gastric cancer in Japan. Helicobacter. 2017;22:e12415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 102] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 18. | Sendai City. Japanese age-specific basic resident registration system. [cited 1 June 2025]. Available from: https://www.city.sendai.jp/chosatoke/shise/toke/jinko/jyuuki.html. |
| 19. | Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48:452-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9275] [Cited by in RCA: 14528] [Article Influence: 1117.5] [Reference Citation Analysis (0)] |
| 20. | Yamagishi H, Koike T, Ohara S, Kobayashi S, Ariizumi K, Abe Y, Iijima K, Imatani A, Inomata Y, Kato K, Shibuya D, Aida S, Shimosegawa T. Prevalence of gastroesophageal reflux symptoms in a large unselected general population in Japan. World J Gastroenterol. 2008;14:1358-1364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 21. | Stanghellini V, Chan FK, Hasler WL, Malagelada JR, Suzuki H, Tack J, Talley NJ. Gastroduodenal Disorders. Gastroenterology. 2016;150:1380-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 818] [Cited by in RCA: 1039] [Article Influence: 103.9] [Reference Citation Analysis (0)] |
| 22. | Iijima K, Koike T, Abe Y, Ohara S, Nakaya N, Shimosegawa T. Time series analysis of gastric acid secretion over a 20-year period in normal Japanese men. J Gastroenterol. 2015;50:853-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Kim SE, Kim N, Lee JY, Park KS, Shin JE, Nam K, Kim HJ, Song HJ, Joo YE, Myung DS, Seo JH, Jo HJ, Kim SM, Lim SH, Kim HJ, Baik GH, Choi SH, Choi SC. Prevalence and Risk Factors of Functional Dyspepsia in Health Check-up Population: A Nationwide Multicenter Prospective Study. J Neurogastroenterol Motil. 2018;24:603-613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Rahman MM, Ghoshal UC, Kibria MG, Sultana N, Yusuf MA, Nahar S, Ahmed F, Rowshon A, Hasan M. Functional Dyspepsia, Peptic Ulcer, and Helicobacter pylori Infection in a Rural Community of South Asia: An Endoscopy-Assisted Household Survey. Clin Transl Gastroenterol. 2021;12:e00334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Sasaki Y, Abe Y, Shoji M, Mizumoto N, Takeda H, Oizumi H, Yaoita T, Sawada N, Yamagishi K, Saito E, Watanabe M, Ishizawa K, Konta T, Kayama T, Tsugane S, Ueno Y, Inoue M. Reliability of self-reported questionnaire for epidemiological investigation of Helicobacter pylori eradication in a population-based cohort study. Sci Rep. 2021;11:15605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Xu L, Li XT, Ur-Rahman I, Zhang C, Qi YB, Hu RB, Li K, Awadh AM, Ma J, Xiao W, Gao SJ, Yang PL, Wang Y, Peng QS, Wang T, Zheng QM, Ding SZ. Global H. pylori recurrence, recrudescence, and re-infection status after successful eradication in pediatric patients: a systematic review and meta-analysis. J Gastroenterol. 2024;59:668-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 27. | Take S, Mizuno M, Ishiki K, Imada T, Okuno T, Yoshida T, Yokota K, Oguma K, Kita M, Okada H, Yamamoto K. Reinfection rate of Helicobacter pylori after eradication treatment: a long-term prospective study in Japan. J Gastroenterol. 2012;47:641-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/